Abstract
Background
In the context of decreasing external and limited Ukrainian governmental funding for opioid agonist treatments (OAT) for opioid dependent people who inject drugs in Ukraine, information on sustainable financial models is needed.
Methods
Data on 855 opioid dependent people who inject drugs (PWID) were drawn from a cross-sectional nationwide survey of 1,613 PWID. They comprised 434 participants who were receiving OAT and 421 who were not at point of survey but who had done so in the past or were interested in receiving the treatment. Multivariate logistic regression was used to examine factors associated with willingness-to-pay (WTP) for OAT, stratified by OAT experience. Variation in the price which respondents were willing to pay for OAT and its effect on their monthly income among PWID with different OAT experience were assessed as a continuous variable using one-way ANOVA and Kruskal–Wallis test.
Results
Overall, 378 (44%) expressed WTP for OAT. Factors independently associated with WTP differed by OAT experience. Among those using OAT, independent predictors of WTP included: city (Dnipro – aOR=1.9; 95%CI=1.1–4.8 and Lviv – (aOR=2.2; 95%CI=1.1–4.8) compared to those elsewhere in Ukraine), higher income (aOR=1.8; 95%CI=1.2–2.7) and receiving psychosocial counseling (aOR=1.8; 95%CI=1.2–2.7). Among those who had previously been on OAT, positive attitude towards OAT (aOR=1.3; 95%CI=1.1–1.6) and family support of OAT (aOR=2.5; 95%CI=1.1–5.7) were independently associated with WTP. Among PWID who had never been on OAT, being male (aOR=2.2; 95%CI=1.1–4.2), younger age (aOR=1.9; 95%CI=1.2–3.2), higher income (aOR=2.0; 95%CI=1.2–3.4) and previous unsuccessful attempts to enter OAT (aOR=2.3; 95%CI=1.1–4.7) were independently associated with WTP. PWID were willing to commit a large percentage of their monthly income for OAT, which, however, varied significantly based on OAT experience: current OAT: 37% of monthly income, previous OAT: 53%, and never OAT: 60% (p-value=0.0009).
Conclusions
WTP for OAT was substantial among PWID in Ukraine, supporting the implementation of self-pay or co-payment programs. Such strategies, however, must remain affordable, provide better access to OAT, and consider specific needs of PWID.
Keywords: willingness to pay, opioid agonist therapy, methadone, buprenorphine, Ukraine
1. Introduction
Eastern Europe and Central Asia remain the only regions where HIV incidence and mortality continue to increase, with Ukraine having the highest HIV prevalence among adults in the region (Joint United Nations Programme on HIV/AIDS (UNAIDS) 2016). Opioid agonist therapies (OAT) are both an effective and the most cost-effective strategy for preventing HIV in PWID-driven epidemics like the one in Ukraine (Alistar et al. 2011). OAT also markedly reduces many social, medical and legal harms associated with drug injection (Nolan et al. 2015; Tran et al. 2012; Van Den Berg et al. 2007; Wong et al. 2003; World Health Organization 2004). Numerous studies have shown that OAT reduced opioid use, HIV-related risk behaviors (Avants et al. 2004; Magura et al. 1998), and criminal activity (Sun et al. 2015), improved ART (Tran & Nguyen 2013) and tuberculosis treatment adherence (Morozova et al. 2013) and quality of life in PWID, including those living with HIV (Altice et al. 2006; Nosyk et al. 2010). Consequently, it is in society’s interest to ensure access to effective and high-quality care for PWID.
Sustaining HIV prevention programs requires adequate resources, yet budget constraints are becoming increasingly challenging due to recent global economic slowdown and political and economic turmoil in Ukraine resulting from the ongoing conflict in Crimea and Eastern regions. National governments must therefore balance resources and priorities to fund multiple competing social and health issues (Hecht et al. 2009). Moreover, resources for HIV services mainly involve funding from international donors, a source that is rapidly decreasing in Ukraine, despite it being a lower-middle-income country. Anticipated loss of international donor funding in Ukraine by 2017 has created a sense of urgency to strengthen the healthcare system and ensure the sustainability of interventions for the control of HIV infection.
Ukraine successfully introduced OAT with buprenorphine in 2004 (Bruce et al. 2007) with the number of PWID enrolled in treatment restricted to approximately 800. Though more OAT slots were added with the introduction of methadone in 2008 (Lawrinson et al. 2008; Schaub et al. 2010), scale-up to achieve the 2015 target of 20,000 PWID on treatment has remained elusive. Currently, only 2.9% (N= 9,214) of the estimated 310,000 opioid-dependent PWID in Ukraine are receiving OAT (Ukrainian Centers for Disease Control (UCDC) 2015). A variety of individual and structural factors influence OAT entry and retention in Ukraine (Bojko et al. 2013; Bojko et al. 2015; Bojko et al. 2016; Kutsa et al. 2016; Makarenko et al. 2016; Mazhnaya et al. 2016). Before 2017, the OAT program, including drug procurement and management, and additional payments to program staff, was supported by international donors. From 2014, international donors instituted a transition plan to enable the Ukrainian government to take over payment for OAT, with anticipated full financing by 2017. Despite the Government having made commitments to support OAT for 20,892 PWID by 2018 (Verkhovna Rada of Ukraine 2014), it will provide financial support only for 7300 patients on OAT with methadone (Ministry of Finance of Ukraine 2016). Consequently, there is an increasing concern about sustaining HIV prevention and addiction treatment services, especially in the context of political and financial turmoil.
In this context, planning for, and development of, innovative financing for OAT delivery is urgently needed, including options that ensure continued free OAT combined with partial and complete self-pay strategies. Regulatory changes in March 2016 allow for OAT to be prescribed and dispensed in pharmacies, but few patients receive it because it is not widely available except as part of pilot projects. Assessing the willingness of PWID to pay for OAT will help guide government and private providers to develop alternative financing mechanisms to promote sustainability of OAT services in Ukraine. Additionally, alternative models of OAT provision will allow individuals the freedom to choose between governmental, private or possibly mixed health care system that would meet the needs and values of PWID and give them opportunity to benefit from the treatment.
Measurement of willingness-to-pay (WTP) in health services studies could be facilitated using direct or indirect, also known as revealed- or stated-preference methods. Most prior studies used contingent valuation, indirect, technique to assess WTP for drug misuse treatment (Bishai et al. 2008; Borisova & Goodman 2003; Tang et al. 2007; Tran 2013; Zarkin et al. 2000). Since our study was not originally designed to measure WTP for OAT, we used direct (reveled-preference) method to measure WTP and assessed factors associated with WTP for OAT among groups of PWID in Ukraine with different prior OAT experience. Additionally, we measured the price that PWID were willing to pay for OAT, expressed as a ratio of PWID’s monthly income.
Methods
Survey design and sampling
This study emerged from research seeking to understand the barriers and facilitators to medication-assisted treatment entry and retention in Ukraine. A cross-sectional survey of 1,613 PWID was conducted from February 2014 to February 2015 in Kyiv, Odesa, Mykolaiv, Dnipro, and Lviv. A detailed description of the survey design and instruments is presented elsewhere (Makarenko et al. 2016). Briefly, local, opioid dependent PWID who were 18 years or older were recruited randomly from addiction treatment clinic records of current and previous OAT clients. Additionally, PWID who had never been on OAT were recruited through respondent-driven sampling, using standard procedures (Heckathorn 1997). Three groups of PWID were included in the study, based on their OAT experience: 1) current (N=434); 2) previous (N=279); and 3) never on OAT (N=900).
Measures
WTP, the primary outcome, was assessed from the survey question: “If you had the opportunity to pay for OAT legally, would you be willing to pay for your OAT treatment?” among those PWID who expressed willingness to enroll in OAT. For the subset of PWID expressing WTP for OAT, they were additionally asked about the maximum daily price they would pay for OAT. The list of potential covariates of WTP included in the bivariate analysis was based on the results of the preceding qualitative research that assessed barriers of access and retention in OAT (Bojko et al. 2015; Bojko et al. 2016) and previous studies that measured WTP. Age was included as a continuous variable. Employment was categorized as full- or part-time, versus seasonal and not employed. Income was defined as money received monthly from legal and illegal sources and stratified by the minimum wage in Ukraine in 2014. Years of drug injection was categorized as >5 or ≤5 years. Frequent injectors were defined as those who injected drugs for ≥20 days in the last 30 days. An alcohol use disorder was assessed by AUDIT with scores ≥8 for men and ≥4 for women (Babor et al. 2001; Caviness et al. 2009). Standardized cutoffs for moderate to severe depression were categorized for CES-D scores ≥10 (Andresen et al. 1994; Zhang et al. 2012). Two composite variables about attitudes toward OAT were created. The positive attitude variable was generated from 10 questions (5 each about buprenorphine and methadone) related to benefits of OAT that included OAT: a) is a very good way to treat opioid addiction; b) improves your quality of life; c) helps you stay out of prison; d) reduces the injection of drugs; and e) is less stressful than using other narcotics. The negative attitude variable included 6 questions (3 each about buprenorphine and methadone) related to negative myths and beliefs that OAT is: a) only replacing one addiction for another; b) bad for a person’s health; and c) people should try to get off OAT as soon as they can. Additionally, OAT-related characteristics were analyzed for current and previous OAT patients. OAT type was defined as methadone versus buprenorphine. Duration on OAT measured by month was included as a continuous variable. Receiving psychosocial or medical services while being on OAT was defined as using at least one of services available on OAT site. Satisfaction with OAT dosage and experience of short interruptions in treatment (<10 days) were also assessed for those who were currently or had previously been on OAT. For PWID who had never been on OAT, variables reflecting registration at Narcology service and unsuccessful treatment entry attempts were analyzed. To assess a price that PWID were willing to pay for OAT, we created a ratio variable: percentage of amount willing to pay for OAT to PWID’s monthly income.
Statistical analysis
Among the 1,613 PWID in the national survey, 758 were excluded because they expressed no interest in being prescribed OAT, leaving 855 (currently on OAT – N=434, previously on OAT – N=108, never on OAT – N=313) in the final analytical sample. The data on respondents who were not interested in receiving OAT have been published elsewhere (Makarenko et al. 2016). All analyses of WTP for OAT were stratified by OAT experience. This was based on an assumption that program-related factors relevant only for PWID with current or previous OAT experience or characteristics related to persons who have never been on OAT, could be associated with WTP for OAT. Chi-square and Fisher’s exact tests for categorical data and Mann-Whitney test for median comparisons of not normally distributed continuous variables were used to examine differences in characteristics associated with WTP for OAT, stratified by the three OAT experience groups. Multivariate logistic regression was conducted separately for each OAT group. In multivariate analysis, determinants of respondents’ WTP were assessed using socio-demographic characteristics, risk behaviors, and for current and previous OAT clients, characteristics related to their participation in OAT. In addition, we examined if registry as a drug user at a Narcology service and unsuccessful attempts to enter OAT were associated with WTP among PWID who have never been on OAT. For the final multivariate regression model, a p-value of 0.1 was used to enter a model, and the reduced model was constructed using a combination of backward elimination and forward selection strategies, with variables retained in the model if they were independently associated with the outcome at p<0.05. Additionally, to examine potential clustering by region, final models were assessed for effect modification by city of survey using interaction term and likelihood ratio test. The average prices which respondents were willing to pay per day for OAT for PWID with different OAT experience were assessed as a continuous variable. This was done using one-way ANOVA analysis for comparison of means in more than two groups and Kruskal–Wallis test where there were more than two groups for median comparisons of not normally distributed continuous variables, and as a dichotomous variable stratified by median price (30 UAH) using a chi-square. All statistical analysis was performed using SAS 9.3 (SAS Institute Inc., Cary, NC, USA).
Ethical approval
Institutional review boards at Yale University, New Haven, USA (approval number – 1112009437) and the Gromashevskiy Institute at the National Academy of Medical Sciences in Ukraine approved the study protocol.
Results
Of the 855 PWID, 434 (50.8%) were currently using OAT, 108 (12.6%) had previously used OAT and 313 (36.6%) had never used it. The proportion of PWID willing to pay for OAT varied by their experience with OAT and by type of OAT (methadone or buprenorphine or both) that they would be willing to pay for, adjusting for previous or current OAT type (Figure 1). Those who had prior OAT experience, i.e. were previously or currently on OAT, reported WTP significantly more frequently compared to PWID who had never been on OAT (51% and 49% vs. 36%; p<0.001). PWID currently receiving methadone were significantly more likely to be willing to pay for methadone (60%) or both methadone and buprenorphine (33%), whereas the majority of those on buprenorphine reported WTP for buprenorphine (72%). Among those previously on OAT, there were no significant differences between WTP for methadone or buprenorphine and the type of OAT they had received previously.
Figure 1. Willingness to Pay for different OAT type, stratified by current and previous OAT experience adjusting for type of OAT treatment (N=266).
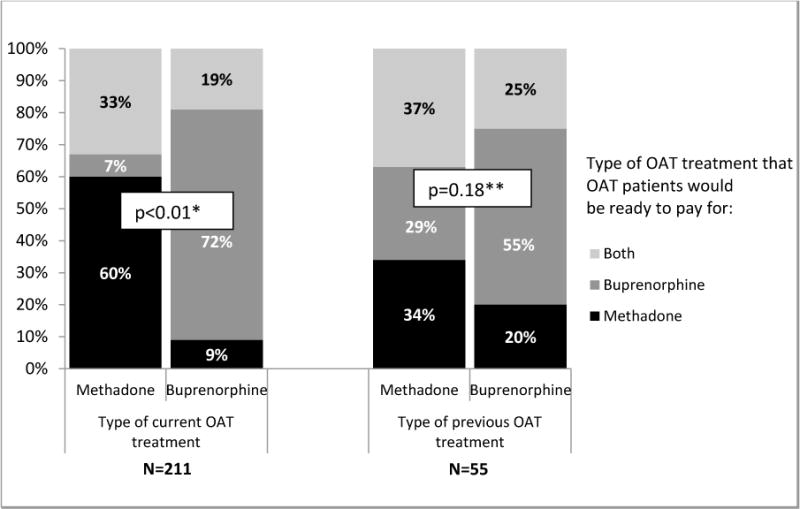
Legend: OAT: opioid agonist treatment.
*P-value for Chi-square test.
**P-value for Fisher’s exact test.
Table 1 describes characteristics of study participants by WTP, stratified by their experience with OAT. Among those currently on OAT, WTP for OAT showed geographic variation with higher rates in PWID in Lviv and Dnipro. Among PWID currently on OAT, WTP was higher for those who were in continuous employment as opposed to intermittent or no employment (53% vs. 15% and 31% respectively, p=0.03); who had higher incomes (66% vs. 55%, p=0.01); lower negative attitudes score towards OAT (median=2, inter-quartile range (IQR)=1–4 vs. 3 (2–5), p<0.001); had family members or friends who supported their participation in OAT (69% vs. 59%, p=0.04); and who had received psychological counseling (70% vs. 58%, p=0.01) and medical services (45% vs. 34%, p=0.01). Among those previously on OAT, WTP was significantly higher among those with more positive attitude towards OAT (median=9 (7–10) vs. median=7 (4–9), p<0.001) and whose family or friends supported OAT (62% vs. 38%, p=0.02), although reporting short interruptions in OAT was more frequent among PWID willing to pay and those who had previously been on OAT (35% vs. 19%, p=0.07). Among PWID who had never been on OAT, WTP was more common for men (88% vs. 75%, p<0.01); for younger PWID (median age=32 (27–38) vs. median age=35 (30–40), p-value=0.02); for higher monthly income (76% vs. 61%, p<0.01); those who had been unable to access OAT previously (17% vs. 9%, p=0.04) and who were HIV-negative (45% vs. 37%, p<0.05).
Table 1.
Characteristics of study participants by their willingness to pay for opioid agonist treatment, stratified by experience (N=855)
| Willing to pay for OAT | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Currently on OAT (N=434) | Previously on OAT (N=108) | Never on OAT (N=313) | |||||||
|
| |||||||||
| Yes N=211 |
No N=223 |
P-value | Yes N=55 |
No N=53 |
P-value | Yes N=112 |
No N=201 |
P-value | |
|
| |||||||||
| Sex (Male) | 167 (79.2) | 173 (77.6) | 0.6918 | 40 (72.7) | 39 (73.6) | 0.9199 | 98 (87.5) | 151 (75.1) | 0.0088 |
|
| |||||||||
| Age – median (IQR) | 37 (32–43) | 36 (32–43) | 0.2023 | 36 (31–43) | 38 (31–46) | 0.9094 | 32 (27–38) | 35 (30–40) | 0.0177 |
|
| |||||||||
| City | 0.0088 | 0.1579 | 0.2772 | ||||||
| Kyiv | 61 (28.9) | 79 (35.4) | 19 (34.6) | 16 (30.2) | 39 (34.8) | 68 (33.8) | |||
| Odesa | 25 (11.8) | 22 (9.9) | 6 (10.9) | 4 (7.6) | 10 (8.9) | 26 (12.9) | |||
| Mykolaiv | 41 (19.4) | 64 (28.7) | 11 (20.0) | 21 (39.6) | 5 (4.6) | 19 (9.5) | |||
| Dnipro | 57 (27.0) | 45 (20.2) | 12 (21.8) | 10 (18.8) | 20 (17.9) | 37 (18.4) | |||
| Lviv | 27 (12.8) | 13 (5.8) | 7 (12.7) | 2 (3.8) | 38 (33.9) | 51 (25.4) | |||
|
| |||||||||
| Employment | 0.0275 | 0.4169 | 0.1556 | ||||||
| Full time/Part time | 113 (53.5) | 91 (40.8) | 30 (54.6) | 23 (43.4) | 54 (48.2) | 75 (37.3) | |||
| Temporary/Seasonal/Day laborer | 31 (14.7) | 39 (17.5) | 8 (14.5) | 7 (13.2) | 18 (16.1) | 35 (17.4) | |||
| Not employed | 67 (31.8) | 93 (41.7) | 17 (30.9) | 23 (43.4) | 40 (35.7) | 91 (45.3) | |||
|
| |||||||||
| Monthly Income (>1200 UAH) | 140 (66.4) | 122 (54.7) | 0.0132 | 38 (69.1) | 37 (69.8) | 1.0000 | 85 (75.9) | 123 (61.2) | 0.0083 |
|
| |||||||||
| Injection drug use duration (>5 years) | 208 (98.6) | 220 (98.7) | 1.0000 | 54 (98.2) | 53 (100.0) | 1.0000 | 98 (87.5) | 172 (85.6) | 0.7329 |
|
| |||||||||
| Injected drugs in the last 30 days | 45 (21.3) | 55 (24.7) | 0.4093 | 46 (83.6) | 46 (86.8) | 0.7880 | 108 (96.4) | 196 (97.5) | 0.7264 |
|
| |||||||||
| Frequent drug injecting (>20 days in the last 30 days) | 8 (3.8) | 15 (6.7) | 0.2018 | 19 (34.6) | 18 (34.0) | 0.9491 | 76 (67.9) | 131 (65.2) | 0.6307 |
|
| |||||||||
| Alcohol use disorder | 48 (22.8) | 67 (30.0) | 0.0852 | 22 (40.0) | 15 (28.3) | 0.2280 | 58 (51.8) | 106 (52.7) | 0.8718 |
|
| |||||||||
| Moderate to severe depression | 86 (40.8) | 110 (49.3) | 0.0730 | 37 (67.3) | 34 (64.2) | 0.8398 | 69 (61.6) | 131 (65.2) | 0.5288 |
|
| |||||||||
| Positive attitude towards OAT – median (IQR) | 9 (8–10) | 9 (7–10) | 0.0370 | 9 (7–10) | 7 (4–9) | 0.0002 | 8 (6–9) | 7 (4–9) | 0.4111 |
|
| |||||||||
| Negative attitude towards OAT – median (IQR) | 2 (1–4) | 3 (2–5) | 0.0008 | 3 (2–5) | 3 (2–5) | 0.7248 | 4 (2–5) | 3 (2–5) | 0.1250 |
|
| |||||||||
| Family/friends support participation in OAT | 145 (68.7) | 132 (59.2) | 0.0390 | 34 (61.8) | 20 (37.7) | 0.0205 | 46 (41.1) | 84 (41.8) | 0.9014 |
|
| |||||||||
| HIV status (self-reported) | 0.9592 | 0.3495 | 0.0498 | ||||||
| Positive | 96 (45.5) | 98 (43.9) | 27 (49.1) | 19 (35.9) | 20 (17.9) | 61 (30.4) | |||
| Negative | 105 (49.8) | 114 (51.2) | 24 (43.6) | 27 (50.9) | 51 (45.5) | 75 (37.3) | |||
| Unknown | 10 (4.7) | 11 (4.9) | 4 (7.3) | 7 (13.2) | 41 (36.6) | 65 (32.3) | |||
|
| |||||||||
| Registration at Narcology service | – | – | – | – | – | – | 41 (36.6) | 74 (36.8) | 0.9707 |
|
| |||||||||
| Tried to enter OAT but failed | – | – | – | – | – | – | 19 (17.0) | 18 (9.0) | 0.0443 |
|
| |||||||||
| OAT type (Methadone) | 165 (78.2) | 179 (80.3) | 0.5950 | 35 (63.6) | 39 (73.6) | 0.3043 | – | – | – |
|
| |||||||||
| Duration on OAT (months) – median (IQR) | 33.5 (13.1–61.3) | 37.4 (19.8–62.1) | 0.2496 | 4.0 (0.1–7.0) | 3.0 (0.1–8.1) | 0.9826 | – | – | – |
|
| |||||||||
| Received psychological counseling on OAT site | 148 (70.1) | 130 (58.3) | 0.0102 | 23 (41.8) | 28 (52.8) | 0.3352 | – | – | – |
|
| |||||||||
| Received medical services on OAT site | 96 (45.3) | 75 (33.6) | 0.0115 | 12 (21.8) | 11 (20.7) | 0.8926 | – | – | – |
|
| |||||||||
| Satisfied with dosage | 177 (83.9) | 187 (83.9) | 0.9933 | 48 (87.3) | 47 (88.7) | 0.8223 | – | – | – |
|
| |||||||||
| Experienced short interruptions in treatment | 42 (19.9) | 46 (20.6) | 0.8516 | 19 (34.6) | 10 (18.9) | 0.0661 | – | – | – |
|
| |||||||||
| Legend: OAT : opioid agonist treatment. | |||||||||
|
| |||||||||
| Currency exchange: US$1 = 8UAH | |||||||||
Table 2 presents findings from multivariate models used to determine factors independently associated with WTP, stratified by OAT experience. Among PWID on OAT, independent predictors of WTP included: location (Lviv vs. Kyiv: aOR=2.2, 95% CI=1.1–4.8, Dnipro vs. Kyiv: aOR=1.9, 95% CI=1.1–3.2); higher monthly income (aOR=1.8, 95% CI=1.2–2.7); and receipt of psychological counseling at OAT site (aOR=1.8, 95% CI=1.2–2.7), while negative attitudes toward OAT (aOR=0.8, 0.8–0.9) was negatively associated with WTP. Among PWID previously on OAT, only positive attitudes towards OAT (aOR=1.3, 95% CI=1.1–1.6) and support from family/friends (aOR=2.5, 95% CI=1.1–5.7) were significant predictors of WTP. Among PWID who had never been on OAT, factors independently associated with WTP included: being male (aOR=2.2, 95% CI=1.1–4.2), younger age (aOR=2.2, 95% CI=1.2–3.2), higher monthly income (aOR=2.0, 95% CI=1.2–3.4), and unsuccessful previous attempts to enter OAT (aOR=2.3, 95% CI=1.1–4.7).
Table 2.
Multivariable regression models of willingness to pay for opioid agonist treatment, experience
| Currently on OAT | Previously on OAT | Never on OAT | |
|---|---|---|---|
|
|
|||
| Variable | AOR (95% CI) | AOR (95% CI) | AOR (95% CI) |
|
| |||
| Sex | |||
| Female | – | Ref. | |
| Male | – | 2.2 (1.1–4.2) | |
|
| |||
| Age, years | |||
| ≥34 years | – | – | Ref. |
| <34 years | 1.9 (1.2–3.2) | ||
|
| |||
| City | |||
| Kyiv | Ref. | ||
| Odesa | 1.7 (0.9–3.5) | – | |
| Mykolaiv | 0.8 (0.5–1.4) | – | |
| Dnipro | 1.9 (1.1–3.2) | ||
| Lviv | 2.2 (1.1–4.8) | ||
|
| |||
| Median Income | |||
| ≤1200 UAH | Ref. | – | Ref. |
| >1200 UAH | 1.8 (1.2–2.7) | 2.0 (1.2–3.4) | |
|
| |||
| Received psychological counseling | |||
| No | Ref. | – | – |
| Yes | 1.8 (1.2–2.7) | ||
|
| |||
| Negative attitudes toward OAT | 0.8 (0.8–0.9) | – | – |
|
| |||
| Positive attitudes toward OAT | – | 1.3 (1.1–1.6) | – |
|
| |||
| Family/friend support OAT | – | ||
| No | Ref. | – | |
| Yes | 2.5 (1.1–5.7) | ||
|
| |||
| Previous unsuccessful attempt to enter OAT | – | – | Ref. |
| No | 2.3 (1.1–4.7) | ||
| Yes | |||
Legend: OAT: opioid agonist treatment; AOR: adjusted odds ratio; CI: confidence interval; Ref: referent.
Currency exchange: US$1= 8UAH
Table 3 and Figure 2 describe differences in the amount of money that PWID were willing to pay per day for OAT. The median daily price was higher among those who had never received OAT. Proportions of those who were ready to pay >30 UAH (US$1= 8UAH) per day were significantly higher among those never or previously on OAT compared to current OAT users (64% and 46% respectively vs. 31%, p<0.0001). The ratio of the amount willing to pay for OAT to monthly income also differed by OAT experience (37% among those currently on OAT, 53% among those previously on OAT, and 60% among those on OAT).
Table 3.
Ratio of amount in UAH which PWID are willing to pay for OAT to monthly income
| Experience with OAT | ||||
|---|---|---|---|---|
| Current N=211 |
Previous N=55 |
Never N=112 |
P-value | |
| Amount willing to pay for a day of OAT (UAH) | ||||
| Mean (SD) | 86 (365) | 77 (156) | 76 (150) | 0.9645* |
| Median (IQR) | 20 (10–50) | 30 (20–50) | 50 (22–100) | <0.0001** |
| Monthly income (UAH) | ||||
| Mean (SD) | 2330 (2705) | 2505 (2153) | 2911 (2678) | 0.4341* |
| Median (IQR) | 2000 (1000–3000) | 2000 (1049–3000) | 2500 (1500–4000) | 0.0724** |
| Ratio: Amount willing to pay per month for OAT/Monthly income | ||||
| Mean (SD) | 0.46 (0.31) | 0.54 (0.27) | 0.59 (0.29) | 0.0009* |
| Median (IQR) | 0.37 (0.20–0.77) | 0.53 (0.30–0.75) | 0.60 (0.30–0.80) | 0.0014** |
Legend: OAT: opioid agonist treatment; WTP: willingness-to-pay; SD: standard deviation; IQR: inter-quartile range.
P-value for one-way ANOVA.
P-value for Kruskal-Wallis test.
Figure 2. Ratio of amount in UAH which PWID are ready to pay for OAT to their monthly income*.
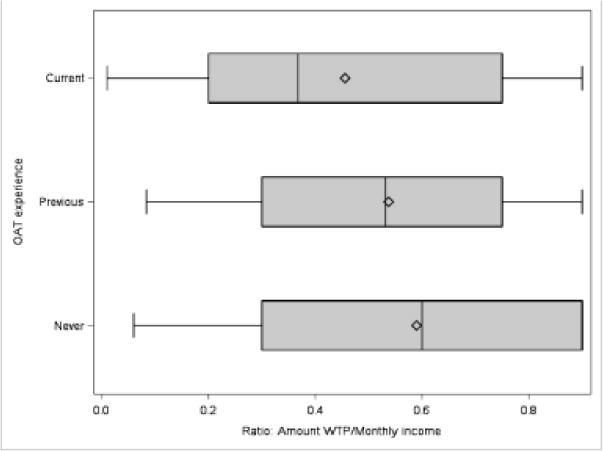
Legend: OAT: opioid agonist treatment; WTP: willingness-to-pay.
*The never on OAT group was willing to pay for OAT significantly more for OAT compared to both other groups (p<0.0014).
Discussion
There have been substantial debates among policy makers, medical professionals, researchers and OAT clients regarding the future of OAT in Ukraine. Given suboptimal OAT coverage and the financial crisis in Ukraine resulting from the ongoing conflict in Crimea and the Donbas region, new financial models for expanding HIV prevention in Ukraine are urgently needed. Recent legislation has relaxed controls over OAT prescription and delivery, allowing OAT with methadone by prescription, while only buprenorphine has been prescribed until recently. Despite relaxation in OAT regulations, less than 1% of all patients on OAT self-pay for it and buprenorphine is the only OAT medication currently purchased. Findings from this study suggest that development of alternative optimal financial models of OAT provision might help to increase the number of individuals who seek treatment with more co-payment being drawn from patients of OAT programs.
In a setting where OAT has been restricted to government supervised settings and provided free of charge since its inception, now over half (53%) of PWID interested in receiving OAT expressed a willingness to pay. Strikingly, patients were willing to commit a large percentage of their monthly income to pay for OAT (up to ~60%). While this may not be associated with truly committing out-of-pocket payment, compared to the lowest cost of opioids injected per day (~70UAH or ~9USD), this would represent a cost-savings to the user. Reducing the out-of-pocket expenses of purchasing OAT rather than spending money on illicit drugs is likely to decrease the financial burden on PWID and their families, as well as ultimately reducing costs of crime and incarceration for society (Sun et al. 2015).
Interestingly, those who were either currently or previously on OAT were significantly more likely to be willing to pay for it than those who had never been on OAT, suggesting that they valued its use. This could also be related to the finding that PWID who previously attempted to access OAT, but were unable to do so, were willing to pay for OAT. Factors previously associated with inability to access OAT have been described elsewhere: requirement to be officially registered as a drug user at a Narcology service (Bojko et al. 2015), which limits employment opportunities and increases risk for police harassment (Kutsa et al. 2016; Makarenko et al. 2016; Mazhnaya et al. 2016), frustrating and time-consuming process that often restricts access to PWID who have full-time jobs or health problems (Bojko et al. 2015), and lack of available OAT slots in governmental programs in some cities (Ukrainian Centers for Disease Control (UCDC) 2015). This suggests that the highly regulated and restricted access to OAT has limited treatment expansion and makes room for alternative methods for entering OAT.
Income emerged as a consistent theme for WTP, especially among those currently and never on OAT. It is unclear, however, why income did not emerge as a key factor in those previously on OAT. This might be related to the characteristics of those who transitioned off OAT for employment reasons; a common complaint about the operating hours at OAT sites was that they were inflexible and interfered with ability to find and keep employment (Bojko et al. 2016). Geographical diversity in WTP was observed among PWID currently on OAT. Previous studies have found geographical variability in prevalence and severity of drug injection, HIV prevalence among PWID and OAT coverage in Ukraine (Polonsky et al. 2015; Zaller et al. 2015). This makes clearer the importance of local experiences of OAT and how these may influence interest in OAT (Makarenko et al. 2016), but also the willingness to pay for it. However, further research is needed to investigate local differences in OAT provision in Ukraine.
Over half were willing to pay for OAT but the cost was also important, especially for PWID who had never been on OAT who were willing to pay more, even when controlling for income. In Ukraine, the costs for buprenorphine are markedly higher than for methadone, but having it prescribed in pharmacies without daily dispensing costs may reduce the overall costs for treatment programs and patients alike. Studies elsewhere have demonstrated that transitioning from OAT to non-specialty treatment settings not only increases the number of patients on treatment, but also can be done safely without significantly jeopardizing public and individual health (Bachireddy et al. 2015). As OAT becomes increasingly available for purchase in pharmacies, it will be crucial to regulate costs, to ensure that patients receive medication that is acceptable to them. An important contribution here, unlike the WTP study in Vietnam, is the finding that a positive attitude towards OAT is significantly associated with WTP among PWID who have never been on OAT. This supports findings that better knowledge about the benefits of OAT will increase willingness to receive and pay for it (Makarenko et al. 2016; Polonsky et al. 2016; Tang et al. 2007). Among those who are currently prescribed OAT, receiving onsite psychological counseling at OAT sites appeared to be an important factor related to WTP. These findings are consistent with results elsewhere showing that clients would pay more for ancillary services like case management during their addiction treatment (Bishai et al. 2008).
This study is the first to examine WTP for OAT in Ukraine where HIV is concentrated in PWID and where healthcare financing reforms are anticipated due to the ongoing political and economic conflict combined with the impending loss of external funding for HIV prevention and treatment. Despite study strengths, including its timeliness and novelty in Ukraine, it is not without limitations, some of which are inherent to observational studies and sampling. Though participants with OAT experience were sampled randomly, RDS was used to enroll PWID who had never been on OAT and, therefore, generated estimates could be imprecise since covariates from this group were unweighted. (Gile & Handcock 2010; Goel & Salganik 2010). The sample size of PWID previously on OAT was small and may have limited ability to detect important differences within this group. Furthermore, future studies should deploy other methods to explore WTP and include patient preferences, payment thresholds and patient segmentation profiles, often explored using conjoint analysis and contingent valuation.
Conclusions
These findings have several implications. First, is the potential for OAT services to be funded or co-funded by patients themselves to ensure the sustainability of OAT programs and improve HIV prevention in Ukraine. Second, such strategies that prioritize private over public funding for OAT should consider household income to ensure that patients can continue OAT. Third, findings here suggest that the strategy for considering self-pay or co-payments for OAT should also include educational campaigns to improve knowledge about treatment benefits and eliminate myths and believe about OAT for both PWID and health providers. Finally, it is crucial to improve access to private programs by relaxing requirements for treatment entry, and structuring of OAT programs according to the specific needs of patients by implementing gender-specific services and psychological counseling, arranging flexible operating hours at OAT sites and expanding OAT by prescription for eligible patients.
Acknowledgments
The authors would like to acknowledge the National Institute on Drug Abuse for funding for research (R01 DA029910 and R01 DA033679) and career development (K24 DA017072) and the Global Health Equity Scholars Program funded by the Fogarty International Center and the National Institute of Allergy and Infectious Diseases (Research Training Grant R25 TW009338) as well as New York State International Training and Research Program through in-country training grant funded by the Fogarty International Center (D43TW000233).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
We have no conflict of interest to declare.
References
- Alistar SS, Owens DK, Brandeau ML. Effectiveness and cost effectiveness of expanding harm reduction and antiretroviral therapy in a mixed HIV epidemic: a modeling analysis for Ukraine. PLoS Med. 2011;8:e1000423. doi: 10.1371/journal.pmed.1000423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altice FL, Sullivan LE, Smith-Rohrber D, Basu S, Stancliff S, Eldred L. The potential role of buprenorphine in the treatment of opioid dependence in HIV-infected individuals and in HIV infection prevention. Clin Infect Dis. 2006;43(Suppl 4):S178–83. doi: 10.1086/508181. [DOI] [PubMed] [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- Avants SK, Margolin A, Usubiaga MH, Doebrick C. Targeting HIV-related outcomes with intravenous drug users maintained on methadone: a randomized clinical trial of a harm reduction group therapy. J Subst Abuse Treat. 2004;26:67–78. doi: 10.1016/S0740-5472(03)00159-4. [DOI] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders Identification test (AUDIT) World Health Organization, Department of Mental Health and Substance Dependence; 2001. [Google Scholar]
- Bachireddy C, Weisberg DF, Altice FL. Balancing access and safety in prescribing opioid agonist therapy to prevent HIV transmission. Addiction. 2015;110:1869–71. doi: 10.1111/add.13055. [DOI] [PubMed] [Google Scholar]
- Bishai D, Sindelar J, Ricketts EP, Huettner S, Cornelius L, Lloyd JJ, Havens JR, Latkin CA, Strathdee SA. Willingness to pay for drug rehabilitation: implications for cost recovery. J Health Econ. 2008;27:959–72. doi: 10.1016/j.jhealeco.2007.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bojko MJ, Dvoriak S, Altice FL. At the crossroads: HIV prevention and treatment for people who inject drugs in Ukraine. Addiction. 2013;108:1697–9. doi: 10.1111/add.12243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bojko MJ, Mazhnaya A, Makarenko I, Marcus R, Dvoriak S, Islam Z, Altice FL. “Bureaucracy & Beliefs”: Assessing the barriers to accessing opioid substitution therapy by people who inject drugs in Ukraine. Drugs: Education prevention and policy. 2015 doi: 10.3109/09687637.2015.1016397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bojko MJ, Mazhnaya A, Marcus R, Makarenko I, Islam Z, Filippovych S, Dvoriak S, Altice FL. The Future of Opioid Agonist Therapies in Ukraine: A Qualitative Assessment of Multilevel Barriers and Ways Forward to Promote Retention in Treatment. J Subst Abuse Treat. 2016;66:37–47. doi: 10.1016/j.jsat.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borisova NN, Goodman AC. Measuring the value of time for methadone maintenance clients: willingness to pay, willingness to accept, and the wage rate. Health Econ. 2003;12:323–34. doi: 10.1002/hec.738. [DOI] [PubMed] [Google Scholar]
- Bruce RD, Dvoryak S, Sylla L, Altice FL. HIV treatment access and scale-up for delivery of opiate substitution therapy with buprenorphine for IDUs in Ukraine–programme description and policy implications. Int J Drug Policy. 2007;18:326–8. doi: 10.1016/j.drugpo.2006.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caviness CM, Hatgis C, Anderson BJ, Rosengard C, Kiene SM, Friedmann PD, Stein MD. Three brief alcohol screens for detecting hazardous drinking in incarcerated women. J Stud Alcohol Drugs. 2009;70:50–4. doi: 10.15288/jsad.2009.70.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gile KJ, Handcock MS. Respondent-Driven Sampling: An Assessment of Current Methodology. Sociol Methodol. 2010;40:285–327. doi: 10.1111/j.1467-9531.2010.01223.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goel S, Salganik MJ. Assessing respondent-driven sampling. Proc Natl Acad Sci U S A. 2010;107:6743–7. doi: 10.1073/pnas.1000261107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hecht R, Bollinger L, Stover J, McGreevey W, Muhib F, Madavo CE, de Ferranti D. Critical choices in financing the response to the global HIV/AIDS pandemic. Health Aff (Millwood) 2009;28:1591–605. doi: 10.1377/hlthaff.28.6.1591. [DOI] [PubMed] [Google Scholar]
- Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Social Problems. 1997;44:174–99. [Google Scholar]
- Joint United Nations Programme on HIV/AIDS (UNAIDS) Global AIDS Update 2016. Geneva, Switzerland: 2016. [Google Scholar]
- Kutsa O, Marcus R, Bojko MJ, Zelenev A, Mazhnaya A, Dvoriak S, Filippovych S, Altice FL. Factors Associated with Physical and Sexual Violence by Police among People who Inject Drugs in Ukraine: Implications for Retention on Opioid Agonist Therapy. Journal of the International AIDS Society. 2016 doi: 10.7448/IAS.19.4.20897. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrinson P, Ali R, Buavirat A, Altice FL, Chiamwongpaet S, Dvoryak S, Habrat B, Jie S, Mardiati R, Mokri A, Moskalewicz J, Newcombe D, Poznyak V, Subata E, Uchtenhagen A, Utami DS, Vial R, Zhao C. Key findings from the WHO collaborative study on substitution therapy for opioid dependence and HIV/AIDS. Addiction. 2008;103:1484–92. doi: 10.1111/j.1360-0443.2008.02249.x. [DOI] [PubMed] [Google Scholar]
- Magura S, Rosenblum A, Rodriguez EM. Changes in HIV risk behaviors among cocaine-using methadone patients. J Addict Dis. 1998;17:71–90. doi: 10.1300/J069v17n04_07. [DOI] [PubMed] [Google Scholar]
- Makarenko I, Mazhnaya A, Polonsky M, Marcus R, Bojko MJ, Filippovych S, Springer S, Dvoriak S, Altice FL. Determinants of willingness to enroll in opioid agonist treatment among opioid dependent people who inject drugs in Ukraine. Drug Alcohol Depend. 2016;165:213–20. doi: 10.1016/j.drugalcdep.2016.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazhnaya A, Bojko MJ, Makarenko I, Marcus R, Filippovych S, Islam Z, Dvoriak S, Altice FL. In their own voices: Breaking the vicious cycle of addiction, treatment and criminal justice among people who inject drugs in Ukraine. DEPP Drugs: education, prevention and policy. 2016;23:163–75. doi: 10.3109/09687637.2015.1127327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- V.R.o. Ukraine, editor. Ministry of Finance of Ukraine. Ukrainian State Budget for 2017. 2016. [Google Scholar]
- Morozova O, Dvoryak S, Altice FL. Methadone treatment improves tuberculosis treatment among hospitalized opioid dependent patients in Ukraine. Int J Drug Policy. 2013;24:e91–8. doi: 10.1016/j.drugpo.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolan S, Hayashi K, Milloy MJ, Kerr T, Dong H, Lima VD, Lappalainen L, Montaner J, Wood E. The impact of low-threshold methadone maintenance treatment on mortality in a Canadian setting. Drug Alcohol Depend. 2015;156:57–61. doi: 10.1016/j.drugalcdep.2015.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosyk B, Marsh DC, Sun H, Schechter MT, Anis AH. Trends in methadone maintenance treatment participation, retention, and compliance to dosing guidelines in British Columbia, Canada: 1996–2006. J Subst Abuse Treat. 2010;39:22–31. doi: 10.1016/j.jsat.2010.03.008. [DOI] [PubMed] [Google Scholar]
- Polonsky M, Azbel L, Wickersham JA, Taxman FS, Grishaev E, Dvoryak S, Altice FL. Challenges to implementing opioid substitution therapy in Ukrainian prisons: Personnel attitudes toward addiction, treatment, and people with HIV/AIDS. Drug Alcohol Depend. 2015;148:47–55. doi: 10.1016/j.drugalcdep.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polonsky M, Rozanova J, Azbel L, Bachireddy C, Izenberg J, Kiriazova T, Dvoryak S, Altice FL. Attitudes Toward Addiction, Methadone Treatment, and Recovery Among HIV-Infected Ukrainian Prisoners Who Inject Drugs: Incarceration Effects and Exploration of Mediators. AIDS Behav. 2016 doi: 10.1007/s10461-016-1375-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaub M, Chtenguelov V, Subata E, Weiler G, Uchtenhagen A. Feasibility of buprenorphine and methadone maintenance programmes among users of home made opioids in Ukraine. Int J Drug Policy. 2010;21:229–33. doi: 10.1016/j.drugpo.2009.10.005. [DOI] [PubMed] [Google Scholar]
- Sun HM, Li XY, Chow EP, Li T, Xian Y, Lu YH, Tian T, Zhuang X, Zhang L. Methadone maintenance treatment programme reduces criminal activity and improves social well-being of drug users in China: a systematic review and meta-analysis. BMJ Open. 2015;5:e005997. doi: 10.1136/bmjopen-2014-005997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang CH, Liu JT, Chang CW, Chang WY. Willingness to pay for drug abuse treatment: results from a contingent valuation study in Taiwan. Health Policy. 2007;82:251–62. doi: 10.1016/j.healthpol.2006.09.007. [DOI] [PubMed] [Google Scholar]
- Tran BX. Willingness to pay for methadone maintenance treatment in Vietnamese epicentres of injection-drug-driven HIV infection. Bull World Health Organ. 2013;91:475–82. doi: 10.2471/BLT.12.115147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran BX, Nguyen LT. Impact of methadone maintenance on health utility, health care utilization and expenditure in drug users with HIV/AIDS. Int J Drug Policy. 2013;24:e105–10. doi: 10.1016/j.drugpo.2013.07.007. [DOI] [PubMed] [Google Scholar]
- Tran BX, Ohinmaa A, Duong AT, Nguyen LT, Vu PX, Mills S, Houston S, Jacobs P. Cost-effectiveness of integrating methadone maintenance and antiretroviral treatment for HIV-positive drug users in Vietnam’s injection-driven HIV epidemics. Drug Alcohol Depend. 2012;125:260–6. doi: 10.1016/j.drugalcdep.2012.02.021. [DOI] [PubMed] [Google Scholar]
- Ukrainian Centers for Disease Control (UCDC) Opioid Substitution Therapy Statistics. Ukrainian Center for Disease Control; 2015. [Google Scholar]
- Van Den Berg C, Smit C, Van Brussel G, Coutinho R, Prins M. Full participation in harm reduction programmes is associated with decreased risk for human immunodeficiency virus and hepatitis C virus: evidence from the Amsterdam Cohort Studies among drug users. Addiction. 2007;102:1454–62. doi: 10.1111/j.1360-0443.2007.01912.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verkhovna Rada of Ukraine. State Budget of Ukraine for 2014. Verkhovna Rada of Ukraine; 2014. [Google Scholar]
- Wong KH, Lee SS, Lim WL, Low HK. Adherence to methadone is associated with a lower level of HIV-related risk behaviors in drug users. J Subst Abuse Treat. 2003;24:233–9. doi: 10.1016/s0740-5472(03)00029-1. [DOI] [PubMed] [Google Scholar]
- World Health Organization. WHO/UNODC/UNAIDS Position Paper Substitution maintenance therapy in the management of opioid dependence and HIV/AIDS prevention 2004 [Google Scholar]
- Zaller N, Mazhnaya A, Larney S, Islam Z, Shost A, Prokhorova T, Rybak N, Flanigan T. Geographic variability in HIV and injection drug use in Ukraine: implications for integration and expansion of drug treatment and HIV care. Int J Drug Policy. 2015;26:37–42. doi: 10.1016/j.drugpo.2014.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarkin GA, Cates SC, Bala MV. Estimating the willingness to pay for drug abuse treatment: a pilot study. J Subst Abuse Treat. 2000;18:149–59. doi: 10.1016/s0740-5472(99)00030-6. [DOI] [PubMed] [Google Scholar]
- Zhang W, O’Brien N, Forrest JI, Salters KA, Patterson TL, Montaner JS, Hogg RS, Lima VD. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PLoS One. 2012;7:e40793. doi: 10.1371/journal.pone.0040793. [DOI] [PMC free article] [PubMed] [Google Scholar]


