Abstract
Objective
To examine trajectories of internalizing and externalizing behavior problems of preterm children between 16 months and 6 years of age and predictors of trajectories, including gestational age, child dysregulation, maternal depression, socioeconomic status, and parenting.
Study design
This longitudinal study followed 148 children and their mothers from Neonatal Intensive Care Unit (NICU) discharge until age 6. Gestational ages ranged from 23–36 weeks. The study included assessment of maternal-reported behavior problems, maternal depression, neonatal and socioeconomic characteristics, and observations of dysregulated behavior and parenting. Trajectories were identified with a semi-parametric group-based analytic method, and multinomial logistic regression was used to identify significant risk factors.
Results
Three distinct trajectories for preterm children were found for both internalizing and externalizing behavior problems. For the two groups with greater behavior problems (Groups 1 and 2), trajectories reached their peak between 24–36 months of age, then leveled off or decreased. Group 3 showed a stable low level of externalizing behaviors, and a low, but slightly increasing level of internalizing behaviors. Maternal depression, child dysregulation, gestational age, and socioeconomic challenges were identified as risk factors that predicted less optimal behavior problem trajectories.
Conclusions
Children born prematurely followed one of three distinct developmental trajectories for both internalizing and externalizing behavior problems. The most severe behavior problems started early in development and were associated with increased child dysregulation, maternal depression, and lower socioeconomic status. These findings have implications for screening and monitoring preterm children.
Keywords: Behavior Problems, Longitudinal, Maternal Depression, Parenting, Prematurity, Dysregulation, Parent-Child Interactions
Prematurity (birth at <37 weeks of gestation) and admission to a Neonatal Intensive Care Unit (NICU) are associated with medical complications1, increased rates of intellectual disability, attention difficulties, and language and motor problems2–5, but links to child behavior problems have been less consistent. Externalizing behavior problems are marked by aggression and disruptive behavior, while internalizing behaviors include withdrawal, depression, and anxiety6–8. Three reviews indicate that preterm children have increased rates of externalizing and internalizing behaviors compared with children born at full term2,3,9 but reviews comparing very preterm children (VPT; <32 weeks) and full term children have not always found these differences10. These findings may reflect a “paradox of prematurity”11 wherein late preterm children (LPT; 34–36 weeks) may be at higher risk for some problems than VPT children11,12. Studies at single time points may limit our understanding, while examining trajectories may allow for earlier identification of at-risk children13–18.
Multiple factors have emerged as potential predictors of behavior problems. Dysregulated emotions (i.e. impulsivity, emotional lability) may be important precursors for children who are developmentally compromised19,20. Preterm infants are also at risk for experiencing more dyadic interactional difficulties, including more intrusive parenting, than full term children21. In prior studies of preterm children, negative, insensitive mothering has predicted greater externalizing behaviors at 2 and 6 years12,22. Mothers of preterm infants are at risk for depression23, and these elevated depressive symptoms predict less optimal parenting24 and more child behavior problems4. The current study examined trajectories of internalizing and externalizing behavior problems between 16 months and 6 years of age in preterm children admitted to an NICU and how those trajectories were affected by early child and family factors. By identifying factors predictive of suboptimal behavioral trajectories, pediatricians may be able to better monitor and screen preterm children for preventive intervention, as well as provide anticipatory guidance to families.
Methods
181 preterm infants and their mothers were recruited from three NICUs. Infants were born at <37 weeks of gestation, had no congenital malformations, prenatal drug exposures, or significant neurological findings, and had mothers ≥17 years of age who read English. For multiple births, 1 child was randomly selected to participate. Of the 181 participants, 3 were excluded due to later identification of a grade IV intraventricular hemorrhage, 4 were excluded as the children were born at full term, and 25 were excluded as they did not have Child Behavior Checklists (CBCLs) completed at two time points, the minimum number suggested for the group-based analyses,25 for a total sample of 148 dyads.
Families were enrolled following IRB approval. Prior to NICU discharge, mothers completed questionnaires and medical records were reviewed by nurses. Gestational age was collected from the medical records. At 16, 24, and 36 months of age (corrected for prematurity), mothers completed questionnaires, the child was assessed, and dyads were videotaped playing in the lab. Visits were scheduled within 2 weeks of corrected age. At 6 years of age, mothers completed a 20–25 minute phone interview and questionnaires.
Measures
Child behavior problems
Mothers completed the Preschool CBCL (1.5 to 5 years)6 at 16, 24, and 36 months and the School-Age CBCL (6–18 years)7 at 6 years. The CBCL has been widely used and validated with preterm samples9. Although the CBCL was collected at 16 months corrected for gestational age, the average chronological age of children was 18.1 months (Range=16.4–21.5 months), and the gestational age was unrelated to CBCL score at any time point The t-scores for Internalizing and Externalizing Problem scales were used due to differences in number of items between the preschool (99 items) and school-age versions (113 items)7.
Parent-child interactions
Interactions at 16 months were coded using 3 established subscales from the Parent Child Early Relational Assessment (PCERA)26–28. The PCERA assesses the frequency, duration, and intensity of affect and behaviors of parent-infant dyads during 5 minutes of play. Each variable is coded from 1 (negative quality) to 5 (positive quality). Higher scores indicate more positive parenting, less negative parenting and less dysregulation. Positive Parenting includes tone of voice, positive affect, enjoyment, and quality of verbalizations, (11 items; α=.90). Negative Parenting includes angry, hostile tone and mood, negative affect, and displeasure (5 items; α=.90). Child Dysregulation includes negative affect, irritable mood, and emotional lability (6 items; α=.88). Ten percent of the sample at each time point was independently coded by 4 trained research assistants. Inter-rater reliability ranged from .83 to .97 across codes (M=.88). Kappa coefficients for individual codes ranged from .60 to 1.0 (M=.83).
Maternal depression
Maternal depressive symptoms were measured at 16 months using The Center for Epidemiologic Studies Depression Scale (CES-D)29, a 20 item self-report questionnaire on a 4-point scale (M=7.83 SD=7.16, Range=0–40, α=.89).
Child cognitive skills
Cognitive skills at 16 months were assessed with the Mental Developmental Index (MDI) score from the Bayley Scales of Infant Development, 2nd Edition30 (M=100, SD=15, α=.91). In this sample, the average MDI score was 88.39 (SD=11.75, Range=50–122), with no significant outliers.
Maternal socioeconomic status (SES)
Mothers completed a demographic questionnaire at NICU discharge. Family income was initially skewed because one family reported income of $500,000; it was top-coded to the next highest family income (i.e. $210,000). The SES index was created by standardizing and averaging maternal education and family income (α=.74).31
Results
A semi-parametric group-based method25,32 was used to identify distinct trajectories of internalizing and externalizing behavior by identifying clusters of individuals with similar developmental pathways. Since the analytic sample was selected based on at least two data time points on the CBCL, there were no missing data for predictors. Behavior problems were modeled as a function of child age in months using the PROC TRAJ procedure in SAS.32 Since behavior problems were approximately normally distributed, censored normal models were estimated. First, unconditional models were fitted for internalizing and externalizing behaviors to identify the number and shape of trajectory groups for each outcome. The Bayesian Information Criterion (BIC) was used to identify the best fitting model, with the lowest BIC score indicating better fit25. Posterior probabilities of group membership were evaluated, with a posterior probability of .70 or higher for individuals assigned to a given group considered evidence of acceptable model fit25.
Next, multinomial logistic regression was used to examine predictors of trajectory group membership. The likelihood of membership in each trajectory group was compared with the likelihood of membership in the trajectory group with the highest level of symptoms over time (Group 1: High), predicted by SES, child gestational age, child cognitive skills, maternal depression, and parent-child interactions during play (positive parenting, negative parenting, child dysregulation). Group 1 was chosen as the initial reference group so that all analyses indicate contrast with the highest risk group, indicating factors that increase the likelihood of greater resilience and fewer behavior problems. Differences between Groups 2 (Medium) and 3 (Low) are also noted within the text. Separate models were run for internalizing and externalizing behaviors, weighting all analyses by posterior probability so that more prototypical cases for each trajectory group were more heavily weighted. This approach accounts in part for the uncertainty in assigning cases to trajectory groups.
One hundred forty eight mother-child dyads were included. Ten mothers completed CBCLs at 2 time points, 38 at 3 time points, and 100 at all 4 time points. At 6 years, 106 mothers participated (71.6%). Families were more likely lost to attrition when mothers were younger, single, had less education, and were not Caucasian, but were comparable on other variables (Table I). Descriptive statistics are displayed in Table II. Of note, 13.8% of women reported CESD scores in the clinical range (≥16; n = 20). In addition, although positive and negative parenting were weakly correlated (r = .28, p =.001), child dysregulation was unrelated to either positive (r = .07, p =.451) or negative parenting (r = −.02, p =.850).
Table 1.
Demographic and Neonatal Characteristics at NICU discharge (N=148)
| Variable | Range or Frequency (%) |
M | SD |
|---|---|---|---|
| Maternal Age | 17–42 | 30.08 | 6.21 |
| Maternal Education (years) | 8–21 | 14.49 | 2.68 |
| Family Income per Year ($) | 4,320–210,000 | 59,739 | 40,423 |
| Sex of Child (Male) | 74 (50.0%) | ||
| Child MDI Score at 16 months | 50–122 | 88.39 | 11.75 |
| Infant Race | |||
| African American | 17 (11.5%) | ||
| Asian | 1 (0.7%) | ||
| Caucasian | 102 (68.9%) | ||
| Latino | 2 (1.4%) | ||
| Middle Eastern | 2 (1.4%) | ||
| Multiracial | 24 (16.2%) | ||
| Marital Status (Married or Cohabitating) | 121 (81.8%) | ||
| Infant Gestational Age (in weeks) | 23.71–36 | 31.48 | 3.04 |
| Late Preterm (34–36 weeks) | 45 (30.4%) | ||
| Moderate Preterm (32–33 6/7 weeks) | 36 (24.3%) | ||
| Very Preterm (28–31 6/7 weeks) | 43 (29.1%) | ||
| Extremely Preterm (<28 weeks) | 24 (16.2%) | ||
| Infant Birth Weight | 490–3328 | 1748.17 | 579.48 |
| Extremely Low (<1,000 g) | 22 (14.9%) | ||
| Very Low (<1,500 g) | 29 (19.6%) | ||
| Low (<2,500 g) | 84 (56.8%) | ||
| Normal (≥2,500 g) | 13 (8.7%) | ||
| Days Hospitalized | 2–136 | 32.42 | 28.49 |
| Multiple Birth | 28 (18.9%) | ||
| Medical Concerns | |||
| Apnea | 99 (66.9%) | ||
| Respiratory Distress Syndrome | 76 (51.4%) | ||
| Chronic Lung Disease | 14 (9.5%) | ||
| Gastroesophageal Reflux | 14 (9.5%) | ||
| Retinopathy of Prematurity | 2 (1.4%) | ||
| Sepsis and Other Infections | 18 (12.2%) |
Table 2.
Descriptive Statistics
| Mean | SD | Min. | Max. | % Borderlinea |
% Clinically significantb |
|
|---|---|---|---|---|---|---|
| Internalizing behaviors (CBCL) | ||||||
| T score 16 months | 45.65 | (8.82) | 29 | 70 | 4% | 2% |
| 24 months | 49.46 | (9.53) | 29 | 71 | 8% | 5% |
| 36 months | 50.82 | (10.50) | 29 | 72 | 7% | 15% |
| 72 months | 49.37 | (9.90) | 33 | 72 | 5% | 7% |
| Externalizing behaviors (CBCL) | ||||||
| T score 16 months | 47.81 | (8.75) | 28 | 68 | 1% | 5% |
| 24 months | 51.78 | (10.12) | 28 | 76 | 10% | 14% |
| 36 months | 51.82 | (9.53) | 28 | 70 | 7% | 13% |
| 72 months | 50.18 | (9.93) | 33 | 72 | 6% | 8% |
| Mat. Depression (CES-D) | 7.83 | 7.16 | 0.00 | 40.00 | 14%c | |
| PCERAd | ||||||
| Positive parenting | 39.88 | 6.46 | 22.00 | 52.00 | ||
| Negative parenting | 21.50 | 2.83 | 12.00 | 25.00 | ||
| Child dysregulation | 27.26 | 3.07 | 16.00 | 30.00 | ||
CBCL T score 60–63 equal borderline clinical range,
T score 63 or greater equal clinical range of behavior
Scores ≥16 indicate risk for clinical depression.
The Parent-Child Early Relational Assessment (PCERA) does not contain a standard criteria for clinical significance.
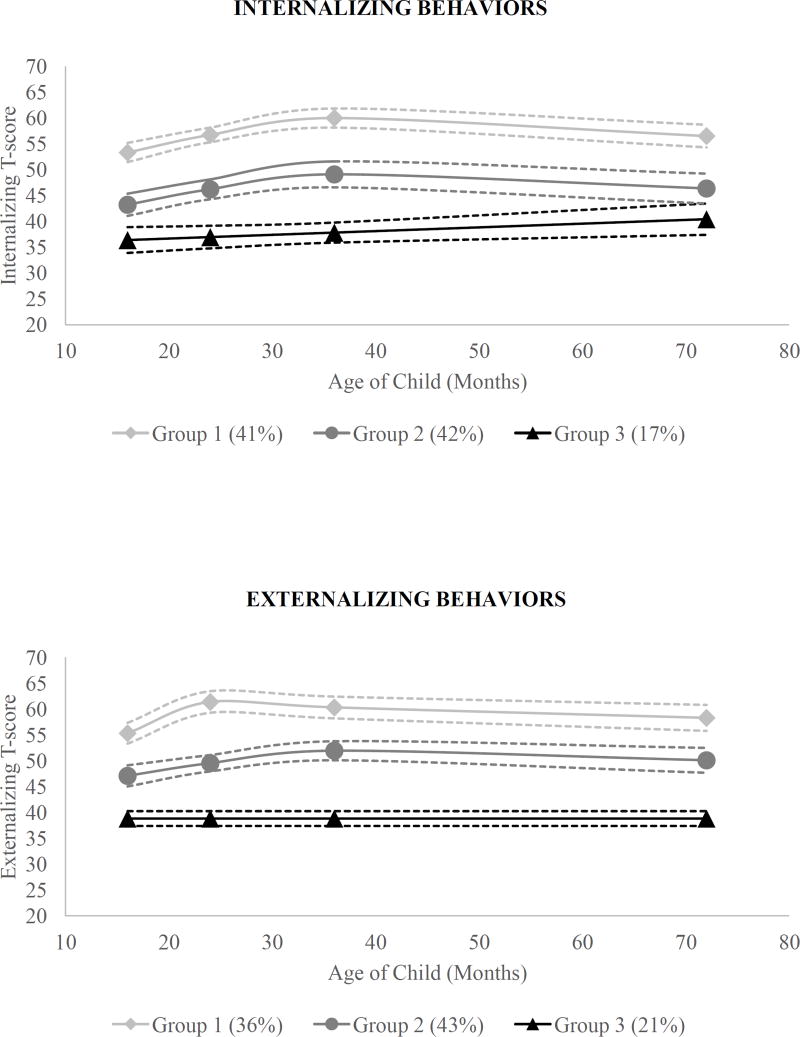
Internalizing Behavior
For internalizing behaviors, a three group model minimized BIC scores (BIC scores: 1 group=−1984.46; 2 groups=−1899.10; 3 groups=−1895.46; 4 groups=−1900.98). As seen in the Figure, 41% of the sample displayed the highest level of internalizing behavior across time (Group 1: High). For the High group, internalizing behavior increased from 16 through 36 months, then gradually declined through 72 months. An additional 42% of the sample displayed a similar pattern over time, at lower levels (Group 2: Medium). The remaining 17% showed the lowest level of internalizing symptoms over time (Group 3: Low). Symptoms gradually increased for this group. Children were assigned to each group with 89% confidence (average posterior probabilities were .93, .83, and .92 for Groups 1, 2, and 3, respectively). Group trajectory was unrelated to the number of time points when CBCLs were collected.
Figure 1.
Predicted Trajectories (with 95% Confidence Intervals) of Internalizing and Externalizing Behaviors
Table III presents the results of the multinomial analyses, using likelihood of membership in Group 1 (High) as the comparison group. Compared with Group 1 (High), the likelihood of membership in Group 2 (Medium) or Group 3 (Low) was increased by higher SES, fewer maternal depressive symptoms, and less child dysregulation. In other words, the risk of being in Group 1 was increased by lower SES, greater maternal depressive symptoms and greater child dysregulation. With each additional point on the CES-D scale, the risk of a child following the Group 1 (High) trajectory increased by 27%. More positive parenting decreased the likelihood of Group 2 (Medium) membership, while the likelihood of membership in Group 3 (Low; lowest trajectory of internalizing behaviors over time) was decreased by higher gestational age. With each additional week of gestation, the likelihood of belonging to Group 3 (Low) decreased by 21%. The risk of being in Group 1 was increased by less positive parenting and later gestational age.
Table 3.
Multinomial Logistic Regression Predicting Trajectory Membership
| Group | Internalizing Symptoms | Externalizing Symptoms | |||||
|---|---|---|---|---|---|---|---|
| O.R. | 95% CI | 95% CI | O.R. | 95% CI | 95% CI | ||
| Lower | Upper | Lower | Upper | ||||
| Group 1 | Reference group | Reference group | |||||
| Group 2 | Maternal SES | 1.96* | 1.03 | 3.75 | 2.07* | 1.06 | 4.01 |
| Child gestational age | 0.94 | 0.81 | 1.09 | 0.94 | 0.81 | 1.10 | |
| Child cognitive skills | 0.99 | 0.95 | 1.03 | 0.97 | 0.93 | 1.02 | |
| Maternal depressive symptoms | 0.92* | 0.85 | 0.98 | 0.92* | 0.86 | 0.98 | |
| PCERAa | |||||||
| Positive parenting | 0.92* | 0.85 | 0.99 | 0.94 | 0.87 | 1.01 | |
| Negative parenting | 0.96 | 0.81 | 1.14 | 0.99 | 0.84 | 1.16 | |
| Child dysregulation | 1.22** | 1.06 | 1.42 | 1.19* | 1.03 | 1.37 | |
| Group 3 | Maternal SES | 2.46* | 1.06 | 5.69 | 1.79 | 0.79 | 4.05 |
| Child gestational age | 0.79* | 0.65 | 0.95 | 0.84 | 0.70 | 1.01 | |
| Child cognitive skills | 0.96 | 0.91 | 1.01 | 0.97 | 0.92 | 1.02 | |
| Maternal depressive symptoms | 0.79** | 0.68 | 0.91 | 0.81** | 0.71 | 0.91 | |
| PCERAa | |||||||
| Positive parenting | 0.99 | 0.88 | 1.10 | 0.98 | 0.89 | 1.08 | |
| Negative parenting | 0.84 | 0.66 | 1.08 | 1.10 | 0.88 | 1.37 | |
| Child dysregulation | 1.26* | 1.03 | 1.54 | 1.14 | 0.96 | 1.35 | |
The Parent-Child Early Relational Assessment (PCERA) does not contain a standard criteria for clinical significance. Higher scores on the PCERA indicate more positive parenting, less negative parenting and less dysregulation, whereas lower scores indicate more negative parenting and greater dysregulation.
p <.05,
p< .01
Follow-up analyses were conducted using multinomial regression but with Group 2 (Medium) as the comparison group to further distinguish predictors of trajectory group membership. Compared with the likelihood of membership in Group 2 (Medium), the likelihood of membership in Group 3 (Low) was decreased by higher gestational age (OR=0.83, p=.04, CI [0.70, 0.99]) and higher maternal depressive symptoms (O.R.=0.86, p=.03, CI [0.75, 0.98]). Comparisons of Group 2 (Medium) to Group 1 (High) are represented in Table III.
Externalizing Behavior
A three group model also yielded the best fit for externalizing behaviors, minimizing BIC scores (BIC scores: 1 group=−1978.20; 2 groups=−1896.90; 3 groups=−1875.17; 4 groups=− 1881.20). Group 1 (36% of children; High) displayed the highest level of externalizing behavior over time (Figure). Group 1 (High) displayed increases in externalizing behaviors from 16 to 24 months, then gradual declines through 72 months. Unlike Group 1 (High), Group 2 (Medium) did not display a peak at 24 months, but showed an increase from 16 to 36 months, followed by a gradual decrease through 72 months. Group 2 (Medium) was the largest group, accounting for 43% of children. The remaining 21% showed a steady pattern of few externalizing behaviors over time (Group 3: Low). Children were assigned to each group with 91% confidence (average posterior probabilities were .93, .89, and .90 for Groups 1, 2, and 3, respectively). Group trajectory was unrelated to the number of time points when CBCLs were collected.
Next, predictors of trajectory group membership were examined. Compared with Group 1 (High), the likelihood of membership in Group 2 (Medium) was increased by higher SES, lower depressive symptoms, and less child dysregulation, while the likelihood of membership in Group 3 (Low) was increased by lower depressive symptoms. In other words, the risk of being in Group 1 (High) was increased by lower SES, greater depressive symptoms and greater child dysregulation. Children of mothers with levels of maternal education and income one standard deviation below the mean were over twice as likely to belong in trajectory Group 1 (High), as compared with Group 2 (Medium). Compared with Group 3 (Low), the likelihood of membership in Group 1 (High) was increased by 24% with each additional point on the CES-D. Follow-up analyses were again conducted to further distinguish predictors of trajectory groups. Higher maternal depression symptoms decreased the likelihood of children following the Group 3 (Low) trajectory compared with Group 2 (Medium) (O.R.=0.88, p=.03, CI [0.78, 0.98]).
Discussion
This prospective longitudinal study examined patterns of behavior problem trajectories in preterm children admitted to the NICU and identified individual, familial, and contextual risk factors for such trajectories. These findings have implications for primary care pediatricians that care for preterm infants and children. Three distinct trajectories were identified for both internalizing and externalizing behavior problems, consistent with prior research in children born at term gestation.13,16 Similar patterns emerged in both the externalizing and internalizing models. For the groups with more behavior problems (High and Medium), trajectories reached their peaks between 24–36 months, then leveled off or decreased. These patterns are consistent with behavior problems in term children (i.e. the “terrible twos and threes”) and may reflect normative developmental progressions.16,33 Temper tantrums and separation anxiety are common occurrences during toddlerhood and typically decrease after children have more language, executive function and regulatory skills33. Thus, pediatricians may be able to reassure parents of preterm toddlers that this increase is normative and behavior is expected to improve over time.
Group 3 (Low), in contrast, showed a stable low level of externalizing behaviors, and low, but slightly increasing internalizing behaviors. Given that even at their height, the internalizing behaviors were far below clinical levels, the slow increase over time may reflect a regression to the mean, or a reflection of children’s verbalization of fears and worries34.
In our sample, 51.3% of children were in the High risk group for either internalizing or externalizing trajectories, which is concerning. Yet, only 14–15% of children experienced clinically significant levels of behavior problems at any given time point, and 96% of these children were in the high risk trajectory group. These findings suggest that Group 1 (High) trajectory may identify children who need particular attention and repeated screening by pediatricians, as they may experience more difficulty in school and home settings. It is important for pediatricians to monitor these trajectories over time, as early trajectory membership predicts later psychiatric problems, attentional difficulties, poor school achievement, or substance use18,35. Preterm children are already at increased risk for many of the above outcomes, so identifying early patterns may assist in prioritizing intervention. These findings also indicate that important data can be gained by assessing behavior at one point in time during early childhood for preterm children. Assessing child behavior at a two-or three-year check-up, for example, may be helpful in analyzing children’s long-term risk.
However, the majority of children did not have clinically significant levels of either internalizing or externalizing problems and were functioning well from a behavioral perspective. This may be reassuring information for families to receive from pediatricians. Further, although the bottom two groups were labeled as Medium and Low for clarification purposes, there is no indication that those in Group 2 (Medium) are at any greater risk for clinically significant behavior problems than those in Group 3 (Low). They are different patterns of development with slightly different predictors, but both appear to be normative patterns of development.
In addition to identifying trajectories, we examined early contributors to trajectory membership. Maternal depression, parent-child interactions, child dysregulation, and socioeconomic challenges are risk factors that have long been viewed as critical to children’s development within preterm populations4,36. Although one would expect observations of expressed negative affect, emotional lability, irritability, and impulsivity to relate to externalizing behavior, dysregulation was also associated with trajectories of internalizing behaviors, suggesting that children in Group 1 (High) for either trajectory may experience more generalized underlying difficulties in regulation and emotional control, and that such difficulties are evident early in life. Further, dysregulation was measured at 16 months, while behavior problems peaked later in development, suggesting interventions to improve regulatory skills could begin before a child develops more severe symptomatology.
Although unmeasured in this study, dysregulation may be associated with specific aspects of the child’s temperament in preterm and term samples, including negative affect, irritability, distress to limitations and intensity of mood37,38. Future studies should examine whether temperament also may be a predictor of trajectories. Temperament can be assessed via questionnaire by pediatricians even earlier in development, at a 3 month, or 6 month visit, and may provide opportunities for targeted surveillance of children at risk.
With regards to familial factors, maternal depression was strongly associated with trajectory membership. The American Academy of Pediatrics recommends assessing postpartum depression in mothers, and there have been other suggestions to assess depression in mothers of preterm children39. These findings add to the evidence that maternal depression is detrimental to children’s development40,41 and that pediatricians should attend to the well-being of parents to provide preventive interventions.
Contrary to expectations, parenting quality during play was largely unrelated to trajectory membership, with one exception. Parent-child interactions have generally been associated with children’s behavior12,33,42,43, so this finding was surprising. Given the neurodevelopmental vulnerabilities associated with prematurity, other factors, such as synchrony or vagal tone, may be more critical21,24,44. It also may be that interactions that stress the relationship (i.e., clean-up tasks, difficult puzzle tasks) may be better at measuring the parenting attributes that more directly impact behavior problems than the free play measurement used in this study. SES emerged as a fairly consistent predictor of both internalizing and externalizing trajectory membership, highlighting the importance of economic hardship early in development, particularly as preterm children admitted to the NICU are disproportionally from lower income households45. We measured household income and parental education, two important indicators, but these are also a proxy for a number of other factors, including neighborhood resources, access to services and early prenatal care.
Gestational age was unrelated to externalizing problems. Given that prior research has found heightened risk for children across gestational age9, this finding is somewhat unsurprising. There may be other factors during pregnancy or delivery that are differentially important to children’s behavior, and any level of prematurity can present challenges to the child and family. We chose to use gestational age as a continuous variable, rather than by subgroup categories, due to issues of power.
For internalizing disorders, children in the more resilient group were more premature than those in the most at-risk group. Although this may be initially surprising, emerging research suggests that LPT children have heightened levels of reported behavior problems36. Children born earlier may be more likely to receive early intervention services that address behavioral concerns46, although we were unable to assess this reason. In addition, parents of children born LPT may expect that their children will be developmentally typical, given the fewer medical complications compared with those born VPT1,5. Parents may then not attribute emerging children worries or withdrawal to prematurity, and thus rate the behaviors as more concerning. Future research should contrast parent-reports of internalizing behavior with clinical assessments in order to parse out the impact of parental reporting biases.
There are limitations that must be mentioned. This study examined trajectories of preterm children, but there was no comparison group of term children. Thus, we cannot directly compare predictors and trajectories across preterm and full term populations. Second, mothers completed all reported measurements. Although maternal reports of the CBCL are the most common assessment of children’s behavior problems7, other multi-informant data would be ideal, and teachers, fathers, or clinical assessments could provide additional information. Further, our findings indicated similar rates of externalizing and internalizing behavior problems, although other research has shown higher rates of internalizing behaviors in preterm children47. This may be due to the age of measurement and the use of maternal report alone. The CBCL was measured first at 16 months (corrected for prematurity), although it is designed to start at 18 months. However, children were 18 months (average uncorrected for prematurity) during the assessment and internal consistency and variability were appropriate. There was attrition in the study, but it was not associated with any study variables. Finally, child dysregulation and parenting were measured during the same play interaction. We were limited by either choosing to measure child and parent behavior at two separate time points or using the same interaction.
Beginning at 16 months corrected age, preterm children who had been admitted to an NICU followed one of three distinct developmental trajectories for behavior problems, including one at higher risk for later behavioral problems. These trajectories were identified before two years of age. Early behavioral dysregulation, maternal depression, and lower SES were factors increasing the likelihood of membership in a high-risk trajectory. Our study suggests that pediatricians should monitor children with these risk factors closely, and refer them to early treatment prior to the onset of more severe behavioral issues.
Acknowledgments
Supported by the National Institutes of Health (R01 HD44163, T32 HD07489, and P30 HD03352) and the University of Wisconsin.
Abbreviations
- NICU
Neonatal Intensive Care Unit
- LPT
Late Preterm
- VPT
Very Preterm
- SES
Socioeconomic Status
- CBCL
Child Behavior Checklist
- PCERA
Parent Child Early Relational Assessment
- CESD
Center for Epidemiological Studies Depression Scale
- BIC
Bayesian Information Criterion
- MDI
Mental Developmental Index.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors declare no conflicts of interest.
References
- 1.McCormick MC, Litt JS, Smith VC, Zupancic JA. Prematurity: an overview and public health implications. Annu. Rev. Public Health. 2011;32:367–79. doi: 10.1146/annurev-publhealth-090810-182459. [DOI] [PubMed] [Google Scholar]
- 2.Bhutta AT, Cleves MA, Casey PH, Cradock MM, Anand K. Cognitive and behavioral outcomes of school-aged children who were born preterm. J. Am. Med. Assoc. 2002;288:728–37. doi: 10.1001/jama.288.6.728. [DOI] [PubMed] [Google Scholar]
- 3.De Jong M, Verhoeven M, van Baar AL. School outcome, cognitive functioning, and behaviour problems in moderate and late preterm children and adults: A review. Semin. Fetal. Neonatal Med. 2012;17:163–69. doi: 10.1016/j.siny.2012.02.003. [DOI] [PubMed] [Google Scholar]
- 4.Gray RF, Indurkhya A, McCormick MC. Prevalence, stability, and predictors of clinically significant behavior problems in low birth weight children at 3, 5, and 8 years of age. Pediatrics. 2004;114:736–43. doi: 10.1542/peds.2003-1150-L. [DOI] [PubMed] [Google Scholar]
- 5.Marlow N, Wolke D, Bracewell MA, Samara M. Neurologic and developmental disability at six years of age after extremely preterm birth. N. Engl. J. Med. 2005;352:9–19. doi: 10.1056/NEJMoa041367. [DOI] [PubMed] [Google Scholar]
- 6.Achenbach TM, Rescorla LA. ASEBA preschool forms & profiles: An integrated system of multi-informant assessment. Burlington, VT: ASEBA; 2000. [Google Scholar]
- 7.Achenbach TM, Rescorla LA. ASEBA school age forms and profiles. Burlington, VT: ASEBA; 2001. [Google Scholar]
- 8.Achenbach TM, Edelbrock CS. The classification of child psychopathology: a review and analysis of empirical efforts. Psychol. Bull. 1978;85:1275–1301. [PubMed] [Google Scholar]
- 9.Arpi E, Ferrari F. Preterm birth and behaviour problems in infants and preschool-age children: a review of the recent literature. Dev. Med. Child Neurol. 2013;55:788–96. doi: 10.1111/dmcn.12142. [DOI] [PubMed] [Google Scholar]
- 10.Aarnoudse-Moens CSH, Weisglas-Kuperus N, van Goudoever JB, Oosterlaan J. Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics. 2009;124:717–28. doi: 10.1542/peds.2008-2816. [DOI] [PubMed] [Google Scholar]
- 11.Shah PE, Robbins N, Coelho RB, Poehlmann J. The paradox of prematurity: The behavioral vulnerability of late preterm infants and the cognitive susceptibility of very preterm infants at 36 months post-term. Infant Behav. Dev. 2013;36:50–62. doi: 10.1016/j.infbeh.2012.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gerstein ED, Poehlmann-Tynan J. Transactional processes in children born preterm: Influences of mother–child interactions and parenting stress. J. Fam. Psychol. 2015;29:777–87. doi: 10.1037/fam0000119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Feng X, Shaw DS, Silk JS. Developmental trajectories of anxiety symptoms among boys across early and middle childhood. J. Abnorm. Psychol. 2008;117:32–47. doi: 10.1037/0021-843X.117.1.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fanti KA, Henrich CC. Trajectories of pure and co-occurring internalizing and externalizing problems from age 2 to age 12: findings from the National Institute of Child Health and Human Development Study of Early Child Care. Dev. Psychol. 2010;46:1159–75. doi: 10.1037/a0020659. [DOI] [PubMed] [Google Scholar]
- 15.Campbell SB, Shaw DS, Gilliom M. Early externalizing behavior problems: Toddlers and preschoolers at risk for later adjustment. Dev. Psychopathol. 2000;12:467–88. doi: 10.1017/s0954579400003114. [DOI] [PubMed] [Google Scholar]
- 16.Hill AL, Degnan KA, Calkins SD, Keane SP. Profiles of externalizing behavior problems for boys and girls across preschool: the roles of emotion regulation and inattention. Dev. Psychol. 2006;42:913–28. doi: 10.1037/0012-1649.42.5.913. [DOI] [PubMed] [Google Scholar]
- 17.Shaw DS, Gilliom M, Ingoldsby EM, Nagin DS. Trajectories leading to school-age conduct problems. Dev. Psychol. 2003;39:189–200. doi: 10.1037//0012-1649.39.2.189. [DOI] [PubMed] [Google Scholar]
- 18.Nagin D, Tremblay RE. Trajectories of boys’ physical aggression, opposition, and hyperactivity on the path to physically violent and nonviolent juvenile delinquency. Child Dev. 1999;70:1181–96. doi: 10.1111/1467-8624.00086. [DOI] [PubMed] [Google Scholar]
- 19.Gerstein ED, Pedersen y Arbona A, Crnic KA, Ryu E, Baker BL, Blacher J. Developmental risk and young children’s regulatory strategies: Predicting behavior problems at age five. J. Abnorm. Child Psychol. 2010;39:351–64. doi: 10.1007/s10802-010-9471-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cole PM, Michel MK, O’Donnell Teti L. The development of emotion regulation and dysregulation: A clinical perspective. Monogr. Soc. Res. Child. Dev. 1994;59:73–100. [PubMed] [Google Scholar]
- 21.Feldman R. Parent-infant synchrony and the construction of shared timing; physiological precursors, developmental outcomes, and risk conditions. J. Child Psychol. Psychiatry. 2007;48:329–54. doi: 10.1111/j.1469-7610.2006.01701.x. [DOI] [PubMed] [Google Scholar]
- 22.Poehlmann J, Burnson C, Weymouth LA. Early parenting, represented family relationships, and externalizing behavior problems in children born preterm. Attach. Hum. Dev. 2014;16:271–91. doi: 10.1080/14616734.2014.884610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vigod SN, Villegas L, Dennis C, Ross LE. Prevalence and risk factors for postpartum depression among women with preterm and low- birth- weight infants: a systematic review. BJOG Int. J. Obstet. Gynaecol. 2010;117:540–50. doi: 10.1111/j.1471-0528.2009.02493.x. [DOI] [PubMed] [Google Scholar]
- 24.Poehlmann J, Schwichtenberg AJ, Bolt DM, Hane A, Burnson C, Winters J. Infant physiological regulation and maternal risks as predictors of dyadic interaction trajectories in families with a preterm infant. Dev. Psychol. 2011;47:91–105. doi: 10.1037/a0020719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nagin DS. Group-based modeling of development. Cambridge: Harvard University Press; 2005. [Google Scholar]
- 26.Clark R. The Parent-Child Early Relational Assessment Instrument and Manual. Madison, WI: Department of Psychiatry, University of Wisconsin Medical School; 2010. [Google Scholar]
- 27.Clark R. The parent-child early relational assessment: A factorial validity study. Educ. Psychol. Meas. 1999;59:821–46. [Google Scholar]
- 28.Clark R. The Parent-Child Early Relational Assessment Instrument and Manual. Madison, WI: Department of Psychiatry, University of Wisconsin Medical School; 1985. [Google Scholar]
- 29.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl. Psychol. Meas. 1977;1:385–401. [Google Scholar]
- 30.Bayley N. Bayley Scales of Infant Development. San Antonio: Psychological Corporation; 1993. [Google Scholar]
- 31.Davis-Kean PE. The influence of parent education and family income on child achievement: the indirect role of parental expectations and the home environment. J. Fam. Psychol. 2005;19:294–304. doi: 10.1037/0893-3200.19.2.294. [DOI] [PubMed] [Google Scholar]
- 32.Jones BL, Nagin DS, Roeder KA. SAS procedure based on mixture models for estimating developmental trajectories. Sociol. Methods Res. 2001;29:374–93. [Google Scholar]
- 33.Campbell SB. Behavior problems in preschool children: A review of recent research. J. Child Psychol. Psychiatry. 2006;36:113–49. doi: 10.1111/j.1469-7610.1995.tb01657.x. [DOI] [PubMed] [Google Scholar]
- 34.Bongers IL, Koot HM, Van der Ende J, Verhulst FC. The normative development of child and adolescent problem behavior. J. Abnorm. Psychol. 2003;112:179–92. doi: 10.1037/0021-843x.112.2.179. [DOI] [PubMed] [Google Scholar]
- 35.Broidy LM, Nagin DS, Tremblay RE, Bates JE, Brame B, Dodge KA, et al. Developmental trajectories of childhood disruptive behaviors and adolescent delinquency: a six-site, cross-national study. Dev. Psychol. 2003;39:222–45. doi: 10.1037//0012-1649.39.2.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Poehlmann-Tynan J, Gerstein ED, Burnson C, Weymouth L, Bolt D, Maleck S, et al. Risk and resilience in preterm children at age 6. Dev. Psychopathol. 2015;27:843–58. doi: 10.1017/S095457941400087X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rothbart MK, Sheese BE. Temperament and emotion regulation. In: Gross JJ, editor. Handbook of emotion regulation. New York: Guilford Press; 2007. pp. 331–50. [Google Scholar]
- 38.Poehlmann J, Schwichtenberg AJ, Shlafer RJ, Hahn E, Bianchi JP, Warner R. Emerging self-regulation in toddlers born preterm or low birth weight: differential susceptibility to parenting? Dev. Psychopathol. 2011;23:177–93. doi: 10.1017/S0954579410000726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Beck CT. Recognizing and screening for postpartum depression in mothers of NICU infants. Adv. Neonatal Care. 2003;3:37–46. doi: 10.1053/adnc.2003.50013. [DOI] [PubMed] [Google Scholar]
- 40.Goodman SH, Rouse MH, Connell AM, Broth MR, Hall CM, Heyward D. Maternal depression and child psychopathology: A meta-analytic review. Clin. Child Fam. Psychol. Rev. 2011;14:1–27. doi: 10.1007/s10567-010-0080-1. [DOI] [PubMed] [Google Scholar]
- 41.Lovejoy MC, Graczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clin. Psychol. Rev. 2000;20:561–92. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- 42.Forcada-Guex M, Pierrehumbert B, Borghini A, Moessinger A, Muller-Nix C. Early dyadic patterns of mother–infant interactions and outcomes of prematurity at 18 months. Pediatrics. 2006;118:107–14. doi: 10.1542/peds.2005-1145. [DOI] [PubMed] [Google Scholar]
- 43.Treyvaud K, Doyle LW, Lee KJ, Roberts G, Cheong JLY, Inder TE, et al. Family functioning, burden and parenting stress 2 years after very preterm birth. Early Hum. Dev. 2011;87:427–31. doi: 10.1016/j.earlhumdev.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 44.Feldman R, Eidelman AI. Biological and environmental initial conditions shape the trajectories of cognitive and social-emotional development across the first years of life. Dev. Sci. 2009;12:194–200. doi: 10.1111/j.1467-7687.2008.00761.x. [DOI] [PubMed] [Google Scholar]
- 45.Kramer MS, Seguin L, Lydon J, Goulet L. Socio- economic disparities in pregnancy outcome: why do the poor fare so poorly? Paediatr. Perinat. Epidemiol. 2000;14:194–210. doi: 10.1046/j.1365-3016.2000.00266.x. [DOI] [PubMed] [Google Scholar]
- 46.Hill JL, Brooks-Gunn J, Waldfogel J. Sustained effects of high participation in an early intervention for low-birth-weight premature infants. Dev. Psychol. 2003;39:730–44. doi: 10.1037/0012-1649.39.4.730. [DOI] [PubMed] [Google Scholar]
- 47.Treyvaud K, Ure A, Doyle LW, Lee KJ, Rogers CE, Kidokoro H, et al. Psychiatric outcomes at age seven for very preterm children: rates and predictors. J. Child Psychol. Psychiatry. 2013;54:772–9. doi: 10.1111/jcpp.12040. [DOI] [PMC free article] [PubMed] [Google Scholar]