Abstract
Purpose
The aim of this study is to evaluate the effect of a novel bovine cumulus oocyte complex (COC) shipping media designed to arrest meiotic resumption during transport on meiotic arrest, as well as meiotic resumption, subsequent embryonic development, and embryo quality.
Methods
Bovine cumulus oocyte complexes were transported overnight from the collection facility to the laboratory. COCs were placed in control in vitro maturation (IVM) or in shipping arrest medium (SAM) containing multiple meiotic inhibitors, and then shipped to our laboratory. Upon arrival, meiotic status was assessed, control COCs were inseminated, and arrested COCs were matured and inseminated the next day. Embryonic development and quality were analyzed.
Results
When bovine COC arrived at the laboratory after overnight shipment (21 h) in SAM, the majority of oocytes remained at the GV stage (75.6 ± 2.9% GV). Arrested oocytes successfully resumed and completed meiosis during IVM after removal from SAM (96.8 ± 0.5% metaphase II compared to control 88.3 ± 5.0%). Moreover, the development of blastocysts per COC was not different from control (22.3 ± 2.4% for control and 18.7 ± 2.1% for SAM), nor was any difference detected in blastocyst quality as determined by cell number and allocation.
Conclusions
Our study demonstrates that a physiological system incorporating cyclic adenosine monophosphate and cyclic guanosine monophosphate modulators can be used to maintain meiotic arrest followed by successful nuclear maturation and pre-implantation embryo development equal to control IVM-derived embryos. Our results offer promising insights for the development of pre-IVM media that may improve oocyte developmental competence in vitro.
Keywords: In vitro maturation, Oocyte competence, Meiosis, Transport
Introduction
In 1935, Pincus and Enzmann described in vitro maturation (IVM) of mammalian oocytes for the first time, and showed that spontaneous meiotic resumption occurs as soon as the oocyte is removed from its follicular niche [1]. Since that time, IVM has not become a routine technique in mammalian assisted reproductive technology (ART) outside of the research laboratory, due to reduced embryo development and pregnancy outcomes following IVF of IVM oocytes [2–4]. In bovine, one of the reasons that may explain low developmental competence of in vitro matured oocytes is the use of a heterogeneous population of oocytes collected from antral follicles at different stages of their growth [5]. Another factor contributing to poor results following IVM may be the use of inadequate in vitro maturation conditions that do not support oocyte competence [6, 7]. However, human IVM could be a beneficial alternative to conventional IVF. It reduces the adverse effects of exogenous hormones used to stimulate follicle growth, and is time and cost-effective compared to standard IVF procedures [4, 8, 9].
Because of its potential benefit to infertility patients in human clinic ART, as well as agricultural and biomedical applications, much research has gone into the development of protocols and culture systems to improve IVM efficiency, reviewed in [10, 11]. Although IVM promotes nuclear maturation, it fails to support cytoplasmic maturation and thus subsequent fertilization, embryo development, implantation, and pregnancy are compromised [6, 12, 13]. Unfortunately, cytoplasmic maturation remains poorly understood. In bovine, one approach to improve oocyte competence has been to utilize conditions that arrest or delay spontaneous meiotic resumption during a short period, prior to IVM, to potentially synchronize nuclear and cytoplasmic maturation and improve oocyte competence [14–24]. A short period of meiotic arrest prior to IVM using IBMX (a broad phosphodiesterase (PDE) inhibitor) and forskolin (FSK; a broad adenylate cyclase activator), called “SPOM” (simulated physiological oocyte maturation), has been shown to improve developmental competence of bovine oocytes [14]. However, these results have been inconsistent [25], due in part to discrepancies in the SPOM protocol across laboratories [26]. In bovine cumulus oocyte complex (COC), pre-IVM treatment with cyclic adenosine monophosphate (cAMP) activator/modulator (FSK + IBMX) enhances the cumulus cell contribution to oocyte antioxidant defense and improves oocyte quality via gap junction communication [27]. Recently, inhibition of meiotic resumption in the presence of physiologically relevant reagents (C-type natriuretic peptide (CNP), estradiol) instead of synthetic reagents like forskolin and broad PDE inhibitors has been shown to better enable normal functions of the rat COC in vitro [28], maintaining gap junction activity and supporting key gene expression critical for oocyte maturation.
The objective of our experiments was to develop a shipping medium for bovine COC in which nuclear maturation of the oocyte would be arrested using a physiological approach. We hypothesized that considering the reported beneficial effect of short pre-IVM systems, arresting meiosis during shipment of COC may improve oocyte developmental competence.
Materials and methods
Both oocyte collection and shipping medium contain an inhibitor of cAMP degradation (a PDE3 specific inhibitor: cilostamide) and an inhibitor of cyclic guanosine monophosphate (cGMP) degradation (a PDE5 specific inhibitor: sildenafil) as well as CNP and estradiol. CNP stimulates the production of cGMP and estradiol help maintains CNP receptors on cumulus cells in many species [29, 30]. After collection and selection, COCs were placed into a defined (no follicular fluid or serum) shipping medium in the presence of CNP, estradiol, BMP15, and a low concentration of FSH. Estradiol has been shown to maintain CNP receptors on cumulus/granulosa cells in different species; CNP stimulates the production of cGMP; and BMP15 and low concentration of FSH help keep gap junctions open [29–32], which is critical to promote transfer of molecules that prevent meiotic resumption (reviewed in [33]). Cilostamide, sildenafil, and hypoxanthine (a naturally occurring cAMP-phosphodiesterase inhibitor [21, 34, 35]) were also included.
Unless specified otherwise, all chemicals were purchased from Sigma-Aldrich (St. Louis, MO, USA). Bovine COC were cultured in 5% CO2 in air during pre-IVM shipment, and 7.5% CO2 in air for subsequent IVF followed by 7.5% CO2 and 6.5% O2 for embryo culture. The gas concentrations used for embryo culture (7.5% CO2 and 6.5% O2) are increased to compensate for the elevation of our laboratory (1830 m above sea level) and are equivalent to 6% CO2 and 5% O2 at sea level. All incubations were conducted 38.5 °C.
COC shipment and maturation
Bovine COCs were recovered from 2 to 8 mm follicles on abattoir derived ovaries (DeSoto Biosciences, Inc.; Seymour, TN). Control COCs were selected and washed in HEPES-buffered medium. Fifty COCs were placed in 2 ml of equilibrated IVM medium (Table 1) in 2.5-ml glass tubes. Tubes were sealed with parafilm and placed into a temperature controlled (38.5 °C) shipping container (Minitube International®) for overnight shipment. For meiotic arrest, COCs were collected, selected, and washed in HEPES-buffered medium in the presence of inhibitors of meiotic resumption (100 μM cilostamide, 100 μM sildenafil, 100 nM estradiol, 100 nM CNP). Fifty COCs were then placed into 2 ml of equilibrated shipping arrest medium (SAM) in 2.5 ml tubes, and shipped overnight with control COC. SAM is a modified version of the bovine IVM medium including meiotic inhibitors (100 μM hypoxanthine, 100 nM CNP, 100 μM cilostamide, 100 μM sildenafil, 100 nM estradiol, 100 ng/ml BMP15; 1 × 10–5 IU/ml rh-FSH) and without EGF. After 24 h of maturation, control COCs were fertilized in vitro. After 21 h of arrest, COCs in SAM were placed into IVM medium (5 COC/50 μl drops under oil) for 24 h in the laboratory, and fertilized the next day. Composition of IVM, IVF, in vitro culture (IVC) 1, and IVC 2 medium is presented in Table 1.
Table 1.
Composition of media used for bovine maturation, fertilization, and embryo culture
| Reagent | Concentrations (mM) | |||
|---|---|---|---|---|
| IVM | IVF | IVC 1 | IVC 2 | |
| NaCl | 100 | 100 | 100 | 100 |
| KCl | 5 | 5 | 5 | 5 |
| KH2PO4 | 0.5 | 0.5 | 0.5 | 0.5 |
| CaCl2·2H2O | 1.7 | 1.7 | 1.7 | 1.7 |
| MgSO4 | 1.2 | 0.2 | 1.2 | 1.2 |
| Bicarbonate | 25 | 25 | 25 | 25 |
| Glucose | 5 | 0.5 | 0.5 | – |
| Fructose | – | – | – | 3 |
| Pyruvate | 0.4 | 0.4 | 0.3 | 0.1 |
| l-Lactate | 6 | 6 | 6 | 6 |
| Ala-Gln | 1 | 1 | 1 | 1 |
| Citrate | 0.5 | – | 0.25 | 0.5 |
| Cysteamine | 0.5 | – | – | – |
| Cysteine | 0.6 | – | – | – |
| Taurine | 5 | 0.1 | 0.1 | 0.1 |
| Glycine | 2.0 | – | – | 2 |
| MEM-NEAA | 1× | 1× | 0.25× | 1× |
| MEM-EAA | 0.5× | – | 0.25× | 0.5× |
| MEM vitamins | 1× | – | – | 1× |
| EDTA | – | – | 5 μM | – |
| Insulin, transferrin, selenium (ITS) | (0.5 μg/ml I, 0.275 μg/ml T, 0.25 ng/ml S) | – | (0.5 μg/ml I, 0.275 μg/ml T, 0.25 ng/ml S) | (0.5 μg/ml I, 0.275 μg/ml T, 0.25 ng/ml S) |
| myo-Inositol | – | – | – | 0.075 |
| rh-FSHa | 0.1 IU/ml | – | – | – |
| rm-EGFb | 50 ng/ml | – | – | – |
| Caffeine | – | 2 | – | – |
| Heparin | – | 7.5 μg/ml | – | – |
| Hyaluronan | 0.25 mg/ml | – | 0.125 mg/ml | 0.125 mg/ml |
| rHSAc | 2.5 mg/ml | – | – | – |
| FAF BSA | – | 8 mg/ml | 8 mg/ml | 8 mg/ml |
| Gentamicin | 50 μg/ml | 50 μg/ml | 25 μg/ml | 25 μg/ml |
aRecombinant human FSH
bRecombinant mouse epidermal growth factor
cRecombinant human serum albumin
Oocyte nuclear maturation
To determine nuclear status, oocytes were fixed and stained using aceto-orcein as previously described [36]. Oocytes were classified into three groups: germinal vesicle (GV)-stage oocytes, corresponding to oocytes that did not mature; germinal vesicle breakdown (GVBD)/metaphase I (MI) stage oocytes (GVBD/MI stage), corresponding to oocytes that did resume meiosis but did not complete nuclear maturation; and metaphase II (MII) stage oocytes, corresponding to oocytes that matured successfully. A total of 148 oocytes in control IVM, 157 in SAM 21 h, and 131 in SAM 21 h followed by 24 h IVM were studied in 3 replicates.
Bovine IVF and embryo culture
Cryopreserved bull spermatozoa were thawed and separated on a 45/90% discontinuous gradient (PureSperm®100; Nidacon). Spermatozoa were washed, counted, and diluted to a final concentration in the fertilization drop of 2 × 106 spermatozoa/ml. Ten COCs were added to the 50 μl drop of fertilization medium (Table 1) under oil and coincubated with spermatozoa for 22 h.
After fertilization, COC were denuded by vortexing and cultured in IVC 1 medium (10 zygotes per 20 μl drop). Ninety-six hours post insemination, zygotes were checked for cleavage. Embryos with more than four cells were moved to IVC 2 medium (5 embryos/20 μl). After 7 days of culture (D7; 174 h), development to the blastocyst stage was assessed and hatching/hatched blastocysts were fixed for subsequent determination of cell number and allocation. A total of 263 COCs in control and 362 COCs in SAM 21 h were studied in 3 replicates. The total number of blastocyst produced in the control treatment was 80 and in SAM 116. The total number of hatching/hatched blastocysts produced in the control treatment was 39 and in SAM was 48.
Embryo quality
Quantification of inner cell mass (ICM) and trophectoderm (TE) cells was performed on hatching or fully hatched blastocysts at D7 of development. Blastocysts were fixed in 4% paraformaldehyde. Antibodies against SRY (sex determining region Y)-box 2 (SOX2; AN579; Biogenex, Fremont, CA, USA) to detect ICM cells and CDX2 (caudal type homeobox 2) (MU392A-UC; Biogenex) to detect trophectoderm cells were used, as described previously [37]. Stained embryos were analyzed using an Olympus BX52 microscope and MetaMorph Microscopy Automation and Image Analysis Software. A total of 83 blastocysts for control IVM and 40 for SAM 21 h were used in 3 replicates.
Statistical analysis
Data were analyzed using NCSS software (Number Cruncher Statistical System, Kaysville UT, USA). For maturation, blastocyst development and cell number, a one-way ANOVA was performed with treatment as a fixed factor. A Bonferroni multiple comparison test was used. Differences were determined to be significant when p < 0.05.
Results
Meiotic arrest
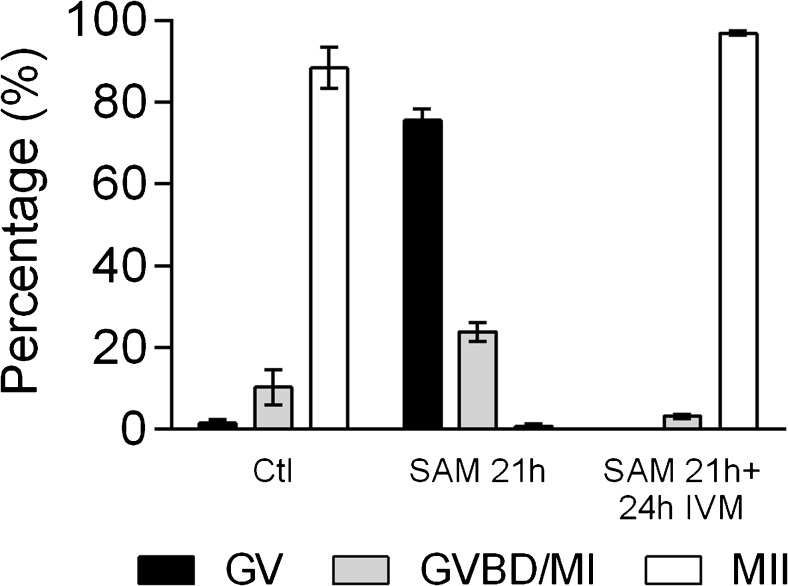
When bovine COCs were shipped overnight (21 h) from the collection facility to the laboratory in SAM, most but not all of the oocytes remained at the GV stage (75.6 ± 2.9% GV versus 1.4 ± 0.9% for control; Fig. 1). When matured in control IVM medium after shipment in SAM, arrested oocytes successfully resumed and completed meiosis (96.8 ± 0.5% MII compared to control 88.3 ± 5%; Fig. 1).
Fig. 1.
Analysis of bovine oocyte nuclear maturation after shipment in IVM medium or in shipping arrest medium (SAM) followed by 24 h IVM (control IVM (n = 148); 21 h SAM (n = 157); 21 h SAM + 24 h IVM (n = 131); three replicates). Data are presented as mean ± S.E.M.
Embryo development and quality
Cleavage was not different from control (59 ± 1.7% for control and 64 ± 2.9% for SAM). Development of bovine blastocysts on D7 of culture following meiotic arrest for 21 h in SAM and IVM/IVF was not different than development of control embryos produced following IVM during shipment (18.7 ± 2.1 and 22.4 ± 2.4% blastocyst per COC; 13.2 ± 0.9 and 14.5 ± 2.8% hatching/hatched blastocyst per COC, respectively) (Fig. 2a). Development per cleaved oocyte was also not different (30.3 ± 2.9 for control and 25.9 ± 2.1 for SAM; Fig. 2b).
Fig. 2.
Effect of meiotic arrest in shipping arrest medium (SAM), followed by IVM, IVF, and IVC on subsequent bovine embryo development, compared to control embryos matured during shipment. Development is reported per COC entered into SAM or control IVM (a) and per cleaved embryo (b). Data is presented as mean ± S.E.M (SAM, n = 362 COC; Ctl, n = 263 COC; three replicates). No differences were detected between treatments
To assess the quality of embryos produced after meiotic arrest, cell number and allocation were determined in D7 hatching/hatched blastocysts (Fig. 3a). There was no difference in blastocyst TE (CDX2 positive) or ICM (SOX2 positive) cell number between blastocysts derived from arrested or control oocytes (Fig. 3b). The proportion of ICM cells was also not significantly different between treatments (18.95 ± 1.2 versus 21.15 ± 1.4%, respectively; Fig. 3c).
Fig. 3.
Cell number and allocation in D7 hatched/hatching bovine blastocysts produced after 21 h meiotic arrest in SAM followed by IVM, IVF, and IVC, compared to those produced from control IVM oocytes matured during shipment. Embryos were stained for SOX2 (ICM cells, green) and CDX2 (TE cells, red) using specific antibodies (a). The number of ICM and TE cells was determined (b), and the percentage of SOX2 positive (ICM) cells was calculated (c). Data are expressed as mean ± SEM (n = 83 for control and 40 for SAM; three replicates)
Discussion
Here, we described for the first time the impact of a shipping medium arresting oocyte meiotic resumption that targets cumulus cells, cAMP/cGMP signaling, and gap junctions on developmental competence of bovine oocytes. We show that the shipping arrest medium maintained meiotic arrest during overnight shipment without negatively affecting developmental competence. Our results will facilitate shipment of COC between production facilities and research laboratories as well as offer insights for the development of maturation systems that can improve oocyte developmental competence in vitro.
Modulation of cAMP concentrations within mammalian COC during maturation modestly improves oocyte developmental competence in several species [14, 17, 19, 24, 27, 38–47]. Modulation of cAMP before IVM, in a short pre-IVM period of meiotic arrest, also improves developmental competence [14, 20, 24, 27], although the mechanisms involved are unclear. To date, the use of pre-IVM culture systems to improve developmental competence has yielded inconsistent results, and this technology is not yet used routinely [25, 26]. In addition to the cAMP pathway, the CNP/cGMP pathway is a major player in the regulation of meiosis [31, 48–52]. Addition of physiologically relevant granulosa cell-derived reagents like CNP and estradiol, rather than supplementation with pharmaceutical chemicals such as forskolin and PDE inhibitors, better enables normal physiological functions of the COC during meiotic arrest in vitro [28].
The arresting shipping system we developed is composed of both an HEPES-buffered medium for collection and selection of COC and a pre-equilibrated bicarbonate-buffered medium for shipment. The HEPES-buffered medium used to collect and select COC has been designed to maintain cAMP at high levels within the oocyte, taking advantage of the role of cGMP in this process, using PDE3 and PDE5 specific inhibitors (cilostamide and sildenafil), as well as preserve the signaling that maintains meiotic arrest with CNP and estradiol. In the shipping arrest medium (SAM), meiotic resumption was prevented by physiological signaling molecules that maintain meiotic arrest via gap junction-mediated communication between the cumulus cells and the oocyte (CNP and estradiol with low concentrations of FSH and BMP15). In addition to these physiological arresting molecules, low concentrations of cilostamide, hypoxanthine, and sildenafil were also included in the shipping medium, as our preliminary studies found that multiple inhibitors were required to efficiently and consistently maintain arrest and preserve developmental competence in bovine COC. It is interesting to note that cAMP activators like Forskolin are not needed to maintain meiotic arrest in our system. Because the presence of high levels of cAMP in the oocyte are necessary to keep the oocyte in meiotic arrest [53–55], and most of the oocytes in our study were arrested after 21 h, this suggests that cAMP is maintained at elevated levels in oocytes during collection and shipment. The oocytes that did not maintain meiotic arrest may have been collected from follicles that were regressing or atretic, due to the heterogeneous population of follicles present on abattoir ovaries in the bovine. These COCs would have likely already lost gap junction communication between the cumulus cells and the oocyte, resulting in a decrease of cGMP/cAMP and initiating germinal vesicle breakdown prior to collection that could not have been reversed [43, 44].
To our knowledge, this is the first report using a pre-IVM medium incorporating physiological ligand/receptor molecules in the context of shipping COC. Our results demonstrate that oocytes can be maintained for 21 h in meiotic arrest during shipment without compromising oocyte quality. We specifically targeted PDE5 and PDE3 using the inhibitors cilostamide and sildenafil. In the bovine, PDE8 participates in cAMP regulation; however, the commercially available PDE8 inhibitor dipyridamole inhibits multiple other PDEs including PDEs 6, 7, 10, and 11. Moreover, in our system, dipyridamole was not able to consistently maintain meiotic arrest (data not shown).
In the SAM medium we have developed, the majority of bovine oocytes remain arrested for 21 h. We did observe that bovine oocyte arrest is exquisitely sensitive to perturbations in temperature and pH; improvements in the percentage of arrested oocytes in this medium were possible when these parameters were more carefully maintained in a steady state (data not shown). Although not an end point, we examined that arresting medium can impact chromatin condensation. Keeping the gap junctions open helps to maintain chromatin in a de-condensed state [56, 57], which may help promote developmental competence of the oocyte. In this system, developmental competence of the oocyte is maintained, although it was not improved. Because these oocytes were obtained from abattoir derived ovaries and likely come from a heterogeneous population of follicles, it would be of interest to explore whether use of the SAM system in oocytes derived from known follicles by OPU would be more effective at maintaining meiotic arrest and/or improving oocyte quality. The ability to arrest oocytes from genetically valuable females during transportation from the farm to the laboratory is of particular interest for the bovine industry, even without quality enhancement. Also, because about 25% of the oocytes were not arrested in GV after shipment, it is possible that these oocytes undergo in vitro aging prior to IVF, and in that sense do not participate or participate poorly in the development of blastocysts [58]. If these non-arrested oocytes are numerically excluded from the analysis (about 25% of the oocytes) and only arrested oocytes considered, the shipping arrest medium may indeed be beneficial for development of the arrested oocytes following IVF. Further studies examining the effects, if any, of SAM on epigenetic modifications and fetal development are warranted as characterization and use of this approach increases.
In conclusion, our study demonstrates that a physiological system incorporating cAMP and cGMP modulators can be used to maintain meiotic arrest during bovine oocyte shipment followed by successful nuclear maturation and pre-implantation embryo development equal to control IVM-derived embryos. Our results offer promising insights for the development of shipping media that may improve oocyte developmental competence in vitro, as well as suggesting a physiological approach to pre-IVM systems in general that could be applied to laboratory and agricultural species, as well as human ART.
References
- 1.Pincus G, Enzmann EV. The comparative behavior of mammalian eggs in vivo and in vitro: I. The activation of ovarian eggs. J Exp Med. 1935;62(5):665–675. doi: 10.1084/jem.62.5.665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.ASRM In vitro maturation: a committee opinion. Fertil Steril. 2013;99(3):663–666. doi: 10.1016/j.fertnstert.2012.12.031. [DOI] [PubMed] [Google Scholar]
- 3.Gremeau AS, Andreadis N, Fatum M, Craig J, Turner K, McVeigh E, et al. In vitro maturation or in vitro fertilization for women with polycystic ovaries? A case-control study of 194 treatment cycles. Fertil Steril. 2012;98(2):355–360. doi: 10.1016/j.fertnstert.2012.04.046. [DOI] [PubMed] [Google Scholar]
- 4.Wrenzycki C, Stinshoff H. Maturation environment and impact on subsequent developmental competence of bovine oocytes. Reproduction in domestic animals = Zuchthygiene. 2013;48(Suppl 1):38–43. doi: 10.1111/rda.12204. [DOI] [PubMed] [Google Scholar]
- 5.Gilchrist RB, Thompson JG. Oocyte maturation: emerging concepts and technologies to improve developmental potential in vitro. Theriogenology. 2007;67(1):6–15. doi: 10.1016/j.theriogenology.2006.09.027. [DOI] [PubMed] [Google Scholar]
- 6.Eppig JJ, O’Brien MJ, Wigglesworth K, Nicholson A, Zhang W, King BA. Effect of in vitro maturation of mouse oocytes on the health and lifespan of adult offspring. Hum Reprod. 2009;24(4):922–928. doi: 10.1093/humrep/den466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gilchrist RB. Recent insights into oocyte-follicle cell interactions provide opportunities for the development of new approaches to in vitro maturation. Reprod Fertil Dev. 2011;23(1):23–31. doi: 10.1071/RD10225. [DOI] [PubMed] [Google Scholar]
- 8.Edwards RG. Are minimal stimulation IVF and IVM set to replace routine IVF? Reprod BioMed Online. 2007;14(2):267–270. doi: 10.1016/S1472-6483(10)60797-3. [DOI] [PubMed] [Google Scholar]
- 9.Rose BI, Laky D, Miller B. The case for in vitro maturation lower cost and more patient friendly. J Reprod Med. 2014;59(11–12):571–578. [PubMed] [Google Scholar]
- 10.Smitz JE, Thompson JG, Gilchrist RB. The promise of in vitro maturation in assisted reproduction and fertility preservation. Semin Reprod Med. 2011;29(1):24–37. doi: 10.1055/s-0030-1268701. [DOI] [PubMed] [Google Scholar]
- 11.Walls M, Junk S, Ryan JP, Hart R. IVF versus ICSI for the fertilization of in-vitro matured human oocytes. Reprod BioMed Online. 2012;25(6):603–607. doi: 10.1016/j.rbmo.2012.08.001. [DOI] [PubMed] [Google Scholar]
- 12.Coticchio G, Dal Canto M, Mignini Renzini M, Guglielmo MC, Brambillasca F, Turchi D, et al. Oocyte maturation: gamete-somatic cells interactions, meiotic resumption, cytoskeletal dynamics and cytoplasmic reorganization. Hum Reprod Update. 2015;21(4):427–454. doi: 10.1093/humupd/dmv011. [DOI] [PubMed] [Google Scholar]
- 13.Li R, Albertini DF. The road to maturation: somatic cell interaction and self-organization of the mammalian oocyte. Nat Rev Mol Cell Biol. 2013;14(3):141–152. doi: 10.1038/nrm3531. [DOI] [PubMed] [Google Scholar]
- 14.Albuz FK, Sasseville M, Lane M, Armstrong DT, Thompson JG, Gilchrist RB. Simulated physiological oocyte maturation (SPOM): a novel in vitro maturation system that substantially improves embryo yield and pregnancy outcomes. Hum Reprod. 2010;25(12):2999–3011. doi: 10.1093/humrep/deq246. [DOI] [PubMed] [Google Scholar]
- 15.Downs SM, Schroeder AC, Eppig JJ. Developmental capacity of mouse oocytes following maintenance of meiotic arrest in vitro. Gamete research. 1986;15(4):305–316. doi: 10.1002/mrd.1120150404. [DOI] [Google Scholar]
- 16.Lonergan P, Khatir H, Carolan C, Mermillod P. Bovine blastocyst production in vitro after inhibition of oocyte meiotic resumption for 24 h. J Reprod Fertil. 1997;109(2):355–365. doi: 10.1530/jrf.0.1090355. [DOI] [PubMed] [Google Scholar]
- 17.Luciano AM, Pocar P, Milanesi E, Modina S, Rieger D, Lauria A, et al. Effect of different levels of intracellular cAMP on the in vitro maturation of cattle oocytes and their subsequent development following in vitro fertilization. Mol Reprod Dev. 1999;54(1):86–91. doi: 10.1002/(SICI)1098-2795(199909)54:1<86::AID-MRD13>3.0.CO;2-C. [DOI] [PubMed] [Google Scholar]
- 18.Mermillod P, Tomanek M, Marchal R, Meijer L. High developmental competence of cattle oocytes maintained at the germinal vesicle stage for 24 hours in culture by specific inhibition of MPF kinase activity. Mol Reprod Dev. 2000;55(1):89–95. doi: 10.1002/(SICI)1098-2795(200001)55:1<89::AID-MRD12>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 19.Nogueira D, Ron-El R, Friedler S, Schachter M, Raziel A, Cortvrindt R, et al. Meiotic arrest in vitro by phosphodiesterase 3-inhibitor enhances maturation capacity of human oocytes and allows subsequent embryonic development. Biol Reprod. 2006;74(1):177–184. doi: 10.1095/biolreprod.105.040485. [DOI] [PubMed] [Google Scholar]
- 20.Richani D, Wang X, Zeng HT, Smitz J, Thompson JG, Gilchrist RB. Pre-maturation with cAMP modulators in conjunction with EGF-like peptides during in vitro maturation enhances mouse oocyte developmental competence. Mol Reprod Dev. 2014;81(5):422–435. doi: 10.1002/mrd.22307. [DOI] [PubMed] [Google Scholar]
- 21.Sirard MA, First NL. In vitro inhibition of oocyte nuclear maturation in the bovine. Biol Reprod. 1988;39(2):229–234. doi: 10.1095/biolreprod39.2.229. [DOI] [PubMed] [Google Scholar]
- 22.Vanhoutte L, De Sutter P, Nogueira D, Gerris J, Dhont M, Van der Elst J. Nuclear and cytoplasmic maturation of in vitro matured human oocytes after temporary nuclear arrest by phosphodiesterase 3-inhibitor. Hum Reprod. 2007;22(5):1239–1246. doi: 10.1093/humrep/dem007. [DOI] [PubMed] [Google Scholar]
- 23.Wu GM, Sun QY, Mao J, Lai L, McCauley TC, Park KW, et al. High developmental competence of pig oocytes after meiotic inhibition with a specific M-phase promoting factor kinase inhibitor, butyrolactone I. Biol Reprod. 2002;67(1):170–177. doi: 10.1095/biolreprod67.1.170. [DOI] [PubMed] [Google Scholar]
- 24.Zeng HT, Richani D, Sutton-McDowall ML, Ren Z, Smitz JE, Stokes Y, et al. Prematuration with cyclic adenosine monophosphate modulators alters cumulus cell and oocyte metabolism and enhances developmental competence of in vitro-matured mouse oocytes. Biol Reprod. 2014;91(2):47. doi: 10.1095/biolreprod.114.118471. [DOI] [PubMed] [Google Scholar]
- 25.Guimaraes AL, Pereira SA, Leme LO, Dode MA. Evaluation of the simulated physiological oocyte maturation system for improving bovine in vitro embryo production. Theriogenology. 2015;83(1):52–57. doi: 10.1016/j.theriogenology.2014.07.042. [DOI] [PubMed] [Google Scholar]
- 26.Gilchrist RB, Zeng HT, Wang X, Richani D, Smitz J, Thompson JG. “Re-evaluation and evolution of the simulated physiological oocyte maturation (SPOM) system.” Theriogenology. 2015;84(4):656–7. [DOI] [PubMed]
- 27.Li HJ, Sutton-McDowall ML, Wang X, Sugimura S, Thompson JG, Gilchrist RB. “Extending prematuration with cAMP modulators enhances the cumulus contribution to oocyte antioxidant defence and oocyte quality via gap junctions.” Hum Reprod. 2016;31(4):810-21. [DOI] [PubMed]
- 28.Campen KA, Clark ZL, Olds MA, McNatty KP, Pitman JL. The in-vitro effects of cAMP and cGMP modulators on inter-cellular dye transfer and gene expression levels in rat cumulus cell-oocyte complexes. Mol Cell Endocrinol. 2015;420:46–56. doi: 10.1016/j.mce.2015.11.025. [DOI] [PubMed] [Google Scholar]
- 29.Zhang J, Wei Q, Cai J, Zhao X, Ma B. Effect of C-type natriuretic peptide on maturation and developmental competence of goat oocytes matured in vitro. PLoS One. 2015;10(7):e0132318. doi: 10.1371/journal.pone.0132318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zhang M, Su YQ, Sugiura K, Wigglesworth K, Xia G, Eppig JJ. Estradiol promotes and maintains cumulus cell expression of natriuretic peptide receptor 2 (NPR2) and meiotic arrest in mouse oocytes in vitro. Endocrinology. 2011;152(11):4377–4385. doi: 10.1210/en.2011-1118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Franciosi F, Coticchio G, Lodde V, Tessaro I, Modina SC, Fadini R, et al. Natriuretic peptide precursor C delays meiotic resumption and sustains gap junction-mediated communication in bovine cumulus-enclosed oocytes. Biol Reprod. 2014;91(3):61. doi: 10.1095/biolreprod.114.118869. [DOI] [PubMed] [Google Scholar]
- 32.Sugimura S, Ritter LJ, Sutton-McDowall ML, Mottershead DG, Thompson JG, Gilchrist RB. Amphiregulin co-operates with bone morphogenetic protein 15 to increase bovine oocyte developmental competence: effects on gap junction-mediated metabolite supply. Mol Hum Reprod. 2014;20(6):499–513. doi: 10.1093/molehr/gau013. [DOI] [PubMed] [Google Scholar]
- 33.Winterhager E, Kidder GM. Gap junction connexins in female reproductive organs: implications for women’s reproductive health. Hum Reprod Update. 2015;21(3):340–352. doi: 10.1093/humupd/dmv007. [DOI] [PubMed] [Google Scholar]
- 34.Downs SM, Coleman DL, Ward-Bailey PF, Eppig JJ. Hypoxanthine is the principal inhibitor of murine oocyte maturation in a low molecular weight fraction of porcine follicular fluid. Proc Natl Acad Sci U S A. 1985;82(2):454–458. doi: 10.1073/pnas.82.2.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Eppig JJ, Ward-Bailey PF, Coleman DL. Hypoxanthine and adenosine in murine ovarian follicular fluid: concentrations and activity in maintaining oocyte meiotic arrest. Biol Reprod. 1985;33(5):1041–1049. doi: 10.1095/biolreprod33.5.1041. [DOI] [PubMed] [Google Scholar]
- 36.Laforest MF, Pouliot E, Gueguen L, Richard FJ. Fundamental significance of specific phosphodiesterases in the control of spontaneous meiotic resumption in porcine oocytes. Mol Reprod Dev. 2005;70(3):361–372. doi: 10.1002/mrd.20203. [DOI] [PubMed] [Google Scholar]
- 37.Bakhtari A, Ross PJ. DPPA3 prevents cytosine hydroxymethylation of the maternal pronucleus and is required for normal development in bovine embryos. Epigenetics. 2014;9(9):1271–1279. doi: 10.4161/epi.32087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Funahashi H, Cantley TC, Day BN. Synchronization of meiosis in porcine oocytes by exposure to dibutyryl cyclic adenosine monophosphate improves developmental competence following in vitro fertilization. Biol Reprod. 1997;57(1):49–53. doi: 10.1095/biolreprod57.1.49. [DOI] [PubMed] [Google Scholar]
- 39.Luciano AM, Modina S, Vassena R, Milanesi E, Lauria A, Gandolfi F. Role of intracellular cyclic adenosine 3′,5′-monophosphate concentration and oocyte-cumulus cells communications on the acquisition of the developmental competence during in vitro maturation of bovine oocyte. Biol Reprod. 2004;70(2):465–472. doi: 10.1095/biolreprod.103.020644. [DOI] [PubMed] [Google Scholar]
- 40.Nogueira D, Albano C, Adriaenssens T, Cortvrindt R, Bourgain C, Devroey P, et al. Human oocytes reversibly arrested in prophase I by phosphodiesterase type 3 inhibitor in vitro. Biol Reprod. 2003;69(3):1042–1052. doi: 10.1095/biolreprod.103.015982. [DOI] [PubMed] [Google Scholar]
- 41.Nogueira D, Cortvrindt R, De Matos DG, Vanhoutte L, Smitz J. Effect of phosphodiesterase type 3 inhibitor on developmental competence of immature mouse oocytes in vitro. Biol Reprod. 2003;69(6):2045–2052. doi: 10.1095/biolreprod.103.021105. [DOI] [PubMed] [Google Scholar]
- 42.Shu YM, Zeng HT, Ren Z, Zhuang GL, Liang XY, Shen HW, et al. Effects of cilostamide and forskolin on the meiotic resumption and embryonic development of immature human oocytes. Hum Reprod. 2008;23(3):504–513. doi: 10.1093/humrep/dem344. [DOI] [PubMed] [Google Scholar]
- 43.Thomas RE, Armstrong DT, Gilchrist RB. Bovine cumulus cell-oocyte gap junctional communication during in vitro maturation in response to manipulation of cell-specific cyclic adenosine 3′,5′-monophosophate levels. Biol Reprod. 2004;70(3):548–556. doi: 10.1095/biolreprod.103.021204. [DOI] [PubMed] [Google Scholar]
- 44.Thomas RE, Thompson JG, Armstrong DT, Gilchrist RB. Effect of specific phosphodiesterase isoenzyme inhibitors during in vitro maturation of bovine oocytes on meiotic and developmental capacity. Biol Reprod. 2004;71(4):1142–1149. doi: 10.1095/biolreprod.103.024828. [DOI] [PubMed] [Google Scholar]
- 45.Vanhoutte L, Nogueira D, De Sutter P. Prematuration of human denuded oocytes in a three-dimensional co-culture system: effects on meiosis progression and developmental competence. Hum Reprod. 2009;24(3):658–669. doi: 10.1093/humrep/den420. [DOI] [PubMed] [Google Scholar]
- 46.Vanhoutte L, Nogueira D, Dumortier F, De Sutter P. Assessment of a new in vitro maturation system for mouse and human cumulus-enclosed oocytes: three-dimensional prematuration culture in the presence of a phosphodiesterase 3-inhibitor. Hum Reprod. 2009;24(8):1946–1959. doi: 10.1093/humrep/dep104. [DOI] [PubMed] [Google Scholar]
- 47.Zeng HT, Ren Z, Guzman L, Wang X, Sutton-McDowall ML, Ritter LJ, et al. Heparin and cAMP modulators interact during pre-in vitro maturation to affect mouse and human oocyte meiosis and developmental competence. Hum Reprod. 2013;28(6):1536–1545. doi: 10.1093/humrep/det086. [DOI] [PubMed] [Google Scholar]
- 48.Kawamura K, Cheng Y, Kawamura N, Takae S, Okada A, Kawagoe Y, et al. Pre-ovulatory LH/hCG surge decreases C-type natriuretic peptide secretion by ovarian granulosa cells to promote meiotic resumption of pre-ovulatory oocytes. Hum Reprod. 2011;26(11):3094–3101. doi: 10.1093/humrep/der282. [DOI] [PubMed] [Google Scholar]
- 49.Kiyosu C, Tsuji T, Yamada K, Kajita S, Kunieda T. NPPC/NPR2 signaling is essential for oocyte meiotic arrest and cumulus oophorus formation during follicular development in the mouse ovary. Reproduction. 2012;144(2):187–193. doi: 10.1530/REP-12-0050. [DOI] [PubMed] [Google Scholar]
- 50.Robinson JW, Zhang M, Shuhaibar LC, Norris RP, Geerts A, Wunder F, et al. Luteinizing hormone reduces the activity of the NPR2 guanylyl cyclase in mouse ovarian follicles, contributing to the cyclic GMP decrease that promotes resumption of meiosis in oocytes. Dev Biol. 2012;366(2):308–316. doi: 10.1016/j.ydbio.2012.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Santiquet N, Papillon-Dion E, Djender N, Guillemette C, Richard FJ. New elements in the C-type natriuretic peptide signaling pathway inhibiting swine in vitro oocyte meiotic resumption. Biol Reprod. 2014;91(1):16. doi: 10.1095/biolreprod.113.114132. [DOI] [PubMed] [Google Scholar]
- 52.Zhang M, Su YQ, Sugiura K, Xia G, Eppig JJ. Granulosa cell ligand NPPC and its receptor NPR2 maintain meiotic arrest in mouse oocytes. Science. 2010;330(6002):366–369. doi: 10.1126/science.1193573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cho WK, Stern S, Biggers JD. Inhibitory effect of dibutyryl cAMP on mouse oocyte maturation in vitro. J Exp Zool. 1974;187(3):383–386. doi: 10.1002/jez.1401870307. [DOI] [PubMed] [Google Scholar]
- 54.Dekel N, Beers WH. Rat oocyte maturation in vitro: relief of cyclic AMP inhibition by gonadotropins. Proc Natl Acad Sci U S A. 1978;75(9):4369–4373. doi: 10.1073/pnas.75.9.4369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schultz RM, Montgomery RR, Belanoff JR. Regulation of mouse oocyte meiotic maturation: implication of a decrease in oocyte cAMP and protein dephosphorylation in commitment to resume meiosis. Dev Biol. 1983;97(2):264–273. doi: 10.1016/0012-1606(83)90085-4. [DOI] [PubMed] [Google Scholar]
- 56.Labrecque R, Lodde V, Dieci C, Tessaro I, Luciano AM, Sirard MA. Chromatin remodelling and histone m RNA accumulation in bovine germinal vesicle oocytes. Mol Reprod Dev. 2015;82(6):450–462. doi: 10.1002/mrd.22494. [DOI] [PubMed] [Google Scholar]
- 57.Lodde V, Franciosi F, Tessaro I, Modina SC, Luciano AM. Role of gap junction-mediated communications in regulating large-scale chromatin configuration remodeling and embryonic developmental competence acquisition in fully grown bovine oocyte. J Assist Reprod Genet. 2013;30(9):1219–1226. doi: 10.1007/s10815-013-0061-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Koyama K, Kang SS, Huang W, Yanagawa Y, Takahashi Y, Nagano M. Aging-related changes in in vitro-matured bovine oocytes: oxidative stress, mitochondrial activity and ATP content after nuclear maturation. J Reprod Dev. 2014;60(2):136–142. doi: 10.1262/jrd.2013-115. [DOI] [PMC free article] [PubMed] [Google Scholar]