Abstract
The embodied experience of nursing practice is rarely studied. Drawing on data from an internationally relevant larger study conducted in 2013–14, here we explore the sensory dimension of the embodied experiences of nursing staff working on two acute NHS hospital wards before and after a move to all-single room inpatient accommodation. We undertook a secondary analysis of 25 interviews with nursing staff (12 before and 13 after the move with half [13/25] using photographs taken by participants) from a mixed-method before-and-after study. This analysis focused on the sensory dimensions of nursing staff's experiences of their working practices and the effect of the built environment upon these. Drawing on Pallasmaa's theoretocal insights, we report how the all-single room ward design prioritises ‘focused vision’ and hinders peripheral perception, whilst the open ward environment is rich in contextual and preconscious information. We suggest all-single room accommodation may offer staff an impoverished experience of caring for patients and of working with each other.
Keywords: Healthcare design, Nursing work, Embodiment, Staff experience, Patient experience
Highlights
-
•
Differences in seeing/hearing patients and staff in open/single room environments (82).
-
•
The open ward environment is rich in contextual and preconscious information (76).
-
•
Staff in single rooms prioritise focused vision; peripheral perception is hindered (82).
-
•
Single room design hinders support, situation awareness and care prioritisation (80).
-
•
Teamwork can be undermined in single rooms; this may be detrimental for patient care (84).
1. Background
The importance of ‘rediscovering’ embodiment in nursing ‘if we are to “re-humanize” care and promote and protect high standards of person-centred nursing practice’ was recently advocated by Draper (2014, p. 2236), who suggests empirical investigation of embodiment in nursing has remained relatively neglected. The human experience of the built environment is exquisitely embodied and multi-sensorial (Pallasmaa, 2012) but rarely a central concern of nursing and healthcare research. Embodiment is the experience of living through our bodies, conducting our daily business in and through our bodies (Draper, 2014), and thus our bodies are in the margin of all our perceptions (Priest, 2000). The limited examination to date of the physical spaces in which clinical care takes place suggests a potentially rich source of understanding of the links and influences between space and professional practice, including working conditions, interprofessional and professional-patient relationships, and patients’ experiences of care (Andrews and Shaw, 2008, Halford and Leonard, 2003, Malone, 2003). Furthermore research evidence suggests positive staff experiences support good patient outcomes (Rafferty et al., 2007) and good patient experiences of care (Maben et al., 2012a, Maben et al., 2012b).
Internationally the case is being made for more single room accommodation in new hospital designs and some researchers argue for the abolition of all shared accommodation (Pennington and Isles, 2013). Much evidence derives from studies in the USA and Scandinavia (Ulrich et al., 2008, West et al., 2010). Claimed advantages of single room patient accommodation for staff include: potential for more personalised patient contact, potentially fewer interruptions and, with medical storage in rooms and less distraction, a decreased chance of prescribing errors (Ulrich et al., 2008). Disadvantages include increased staff travel distances, the potential need for an increase in staffing levels as a result of more single room occupancy and/or adjustments to staff skill mix (Young and Yarandipour, 2007). Clearly, the situation is complex and trade-offs may be necessary (Stichler, 2001).
We conducted an earlier study which examined the impact on healthcare staff and patients of the built environment before and after the move in terms of patient safety outcomes (on which the new build 100% single room environment had no significant impact), costs, and staff and patient preferences (on balance, patients preferred single rooms, staff preferred a mix of single rooms and multi-bedded bays – Maben et al., 2015a, Maben et al., 2015b). The aim of the secondary analysis of staff interviews from this earlier study, as presented here, is to focus specifically on the sensory dimensions of nursing staff's embodied experiences of working on hospital wards before and after a move from open plan ward arrangements to a new build, all-single room patient accommodation hospital site.
Tunbridge Wells Hospital, where the study took place, was the first district general hospital in England with 100% single room inpatient accommodation (Maben et al., 2015a, Maben et al., 2015b). The planning of such new in-patient accommodation is guided by Health Building Note 4 (HBN 04), which - on the basis of rising patient expectations (particularly in relation to privacy and dignity), movement toward greater patient choice, and the imperative of improving prevention of hospital acquired infections - recommends that a minimum of 50% of in-patient beds should be in single rooms in new hospital builds. At Tunbridge Wells Hospital the 100% single room design was championed by the National Patient Safety Agency (NPSA) on grounds of patient safety, as a means to improve infection control and reduce patient falls, stress caused by noise and sleep deprivation, and length of stay. Single rooms were also seen as means of facilitating improved staff to patient communication, patient confidentiality and privacy, family support, and patient satisfaction. The Trust board approved the 100% single room design primarily with a view to building a patient-centred and safe environment (see also Maben et al., 2012c).
In the book The eyes of the skin: architecture and the senses, Finnish architect and theorist Juhan Pallasmaa critiques the hegemony of vision in architecture, explaining how ocularcentrism can lead to forms of the built environment which neglect the integration of all senses in the human experience of space (2012). In the preface to the 2012 edition of his book, Pallasmaa refers to the distinction between ‘focused’ and ‘peripheral’ vision:
The role of peripheral and unfocused vision in our lived experience of the world, as well as in our experience of interiority in the spaces we inhabit, has also evoked my interest. […] The very essence of the lived experience is moulded by unconscious haptic imagery and unfocused peripheral vision. Focused vision confronts us with the world, whereas peripheral vision envelops us in the flesh of the world. (p.14)
Pallasmaa (2012, p.14) is concerned with the extent to which architectural theories and practices pay attention to the ‘collaboration of the various sensory realms’ and the ‘preconscious perceptual realm, which is experienced outside the sphere of focused vision’ (2012, p. 14). The distinction he operates helps us understand nursing staff's perceptions of the space they work in and the ways in which this space may affect their sensory experiences at work.
Our examination here of nursing staff's’ experiences of working in a medical admission unit and a general surgical ward before and after the move to all-single room accommodation has two main aims: 1) to explore how ward design affected the sensory dimension of nursing staff's experience of their working practices, and 2) examine the implications of this for staff-patient and staff-staff relationships on the wards. We use Pallasmaa's distinction between ‘focused’ and ‘peripheral’ visual perception to draw a parallel with the modes of seeing/being seen and hearing/being heard described by nursing staff in reference to caring for patients in the open-plan and all-single room ward environment. Paying attention to the experiences of seeing and hearing that are made possible, constrained, and/or transformed in/by different ward environments, illuminates the types of interactions that different ward designs make possible and the power dynamics these designs either reinforce or challenge.
2. Methods
In our original study (Maben et al., 2015a, Maben et al., 2015b, Simon et al., 2016), four case study adult in-patient wards were selected on the basis of variation in patient populations and length of stay (acute assessment unit [AAU]; general surgery; medical [older people]; and maternity). The aim of the our original study was to explore the impact of the move to a newly built acute hospital with all single rooms on care delivery, working practices, staff and patient experience, safety outcomes and costs. We undertook a mixed-methods study to inform a pre-/post-‘move’ comparison within a single hospital, a quasi-experimental study in two control hospitals and analysis of capital and operational costs associated with single rooms.
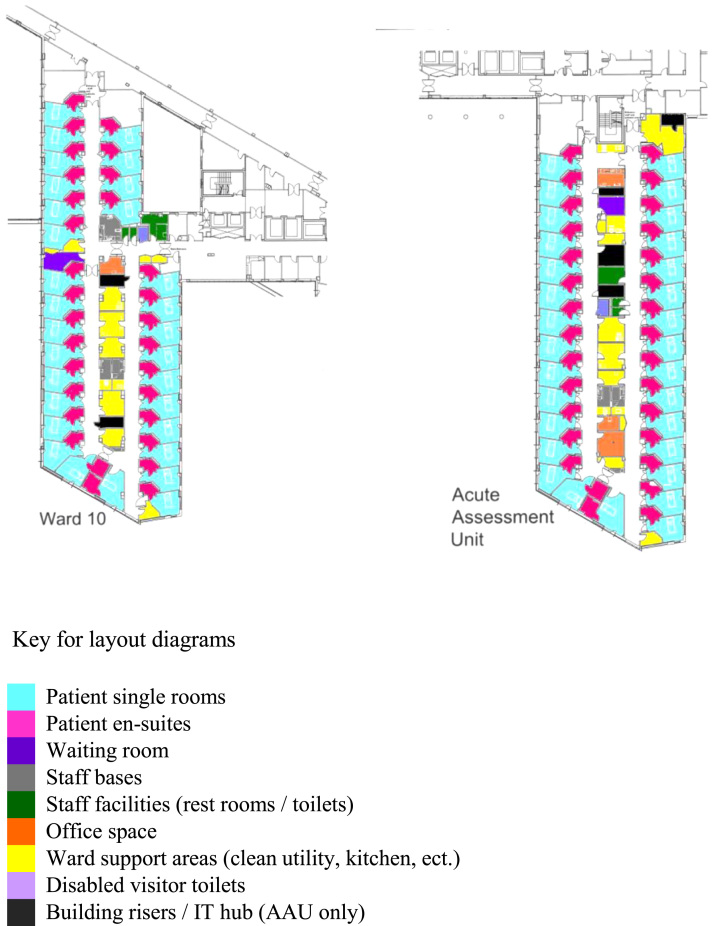
For this paper we carried out a secondary analysis of 25 one-to-one interviews (12 before and 13 after the move to 100% single rooms) with nursing staff from two of the original four ward case studies: the Acute Assessment Unit (AAU) and the general surgical ward (see Table 1 for details). As part of the original study these interviews explored staff experiences of working differently/new ways of working, ward layout (including layout of single rooms and en-suites), staff communication and teamwork, and perceptions of patient experience. These two settings were selected because they present similarities as well as differences: both are general units and have comparable patient dependency with high dependency patients requiring frequent monitoring; and both have similar ward design, although the AAU does not have a double handed corridor (with rooms on both sides) (see Fig. 1). However, they differ in terms of patient turnover (which is, at least in principle, faster in the AAU at 48 hours) and organisation and management of work practices, allowing for a wider range of experiences of nursing practice. The other two wards examined in our original study – a postnatal unit and a care of the elderly ward – were excluded as they presented peculiarities in terms of surveillance needs and organisation of work (care of the elderly environments requiring enhanced surveillance and postnatal wards dealing largely with the care of women who are not ill) that might emphasise aspects of working practices which translate less well to other contexts.
Table 1.
Staff interviews pre and post move.
| Staff group | Phase |
Staff interviews |
Total interviews | |
|---|---|---|---|---|
|
(photo elicitation in brackets) | ||||
| AAU | Surgical | |||
| Nurses | Pre | 5 | 4 | 9 |
| (3) | (2) | (5) | ||
| Post | 5 | 6 | 11 | |
| (3) | (3) | (6) | ||
| Healthcare assistants | Pre | 1 | 2 | 3 |
| (0) | (1) | (1) | ||
| Post | 1 | 1 | 2 | |
| (0) | (1) | (1) | ||
| Total interviews | All | 12 | 13 | 25 |
Fig. 1.
General surgical ward (Ward 10) (left) and AAU (right) layouts, post-move. Reproduced with kind permission from Stantec and Laing O′Rourke (colours added by the authors). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
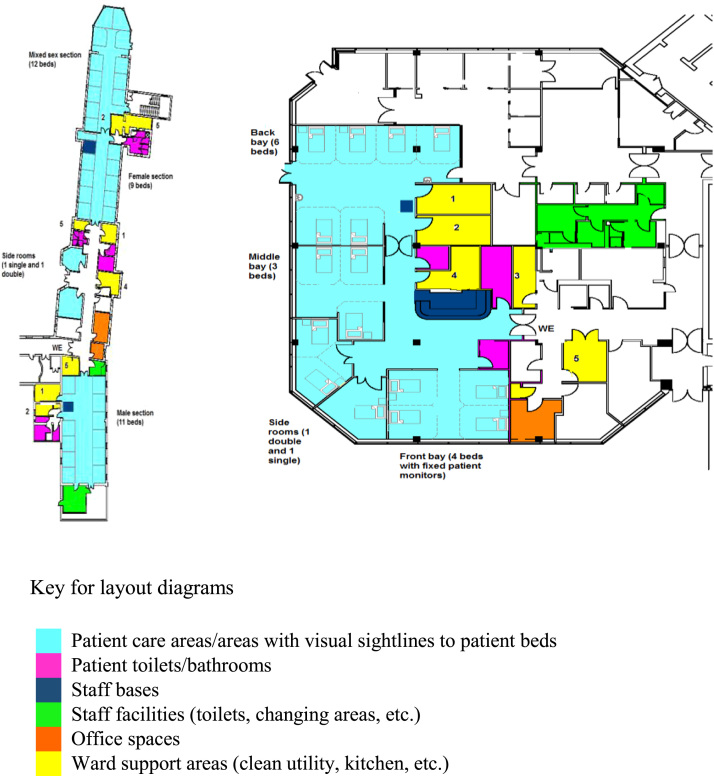
For both the AAU and the general surgical ward examined, the old accommodation was open plan with bays (AAU) and Nightingale style wards (large room without subdivisions with 9–12 beds arranged along the sides of the ward) (see Fig. 2 for plans of the wards before the move). Between October 2010 and September 2011, twelve interviews (6 on each ward) were undertaken on these wards before the move; and 13 interviews were undertaken after the move to the new all-single room hospital building (6 on AAU and 7 on the surgical ward) between September 2012 and June 2013. Staff participation was voluntary. Participants were recruited via the ward managers and by the researcher while conducting observation on the wards. Interviews were conducted on the wards in a private room or quiet area, and lasted between 30 and 60 minutes. The study included the use of photography to aid participants’ reflection upon and discussion of working practices. Half of participants were asked to take photographs of their work environment and were provided with a disposable camera and an information/guidance sheet, and asked to take a minimum of five photographs of aspects of the ward environment they considered important. These photographs were then used alongside the interview topic guide to aid discussion during the interview. The topic guide covered staff experiences of ways of working; ward layout; staff communication and teamwork and perceptions of patient experience. Interviews were audio-recorded and transcribed verbatim. Ethical and local NHS approval was received prior to study commencement.
Fig. 2.
General surgical ward (left) and AAU (right) layouts, pre-move. Reproduced with kind permission from Stantec and Laing O′Rourke (colours added by the authors). (For interpretation of the references to color in this figure legend, the reader is referred to the web version of this article.)
For this paper, the subset of 25 transcripts was analysed thematically with a coding approach informed by grounded theory principles (Charmaz, 2014). Emerging themes (e.g. ‘communication on wards’, ‘visibility of nurses’, ‘visibility of patients’) were discussed and the conceptual tool of Pallasmaa's distinction between ‘focused’ and ‘peripheral’ vision identified as relevant and useful to their interpretation. Thirteen of the interviews presented here (6 pre-move and 7 post-move) were accompanied by photographs. We examined all the photographs in relation to the transcripts they accompanied in terms of subject photographed, context, and interviewee's comments relating to the photograph. We use a selection in this paper to illustrate examples of pre- and post-move experiences of nursing work.
3. Findings
Three key dimensions of nursing staff's sensory experience stood out as dramatically affected by the change of ward design: 1) the ways in which nursing staff were able to see and hear patients on their ward; 2) the extent to which nursing staff were aware of colleagues’ presence and workload on the ward; 3) the extent to which nursing staff could be seen and heard by patients. These dimensions are presented separately but there is inevitably some degree of overlap.
3.1. Nursing work and the senses: seeing and hearing patients
When asked about the space in which they worked, both before and after the move to the new hospital, nursing staff talked at length about being able to see and hear what was going on – both with patients and with other members of the team (see below). One of the prominent anxieties expressed by staff prior to moving to the new hospital as well as after the move concerned the surveillance and monitoring of patients - especially those at risk of falling - as the design of the new single room wards was felt to limit nurses’ ability to monitor several patients at a glance. This inability to ‘eyeball’ patients went hand in hand with nursing staff's reduced ability to see and hear one another and thus to work effectively as a team (see theme 2 below).
The impossibility of ‘keeping an eye’ on several patients at once was a source of anxiety and/or dissatisfaction for the vast majority of participating staff. The interview extract below captures the challenge of the single room ward design for surveillance and monitoring, a theme that was prominent across interviews and ward environments.
When we were on an open ward I could walk on the ward and I could view everybody. And when you knew your patient you could see [if they didn’t look well]. Whereas now I can walk up and down the rooms, but as soon as I’m in a room I’m away from everybody. […] That time has gone where you could just stand and have a quick chat with a patient while you were still keeping an eye on everybody else. (Surgical ward; post-move)
Staff's main concerns were about safeguarding patients and protecting them from falling. However, there were other advantages to being able to see and hear patients (and be seen and heard by them, see theme 3 below) on an open ward or a multi-bedded bay. Being able to prioritise calls for help, whilst providing reassurance to those patients asked to wait, was perceived as important. Patients were also aware that others needed attention so were felt to be more understanding and patient (see below). Practical ways in which nursing staff were able to prioritise - and organise between them - the calls they attended to and/or communicate unavoidable delays to patients requiring assistance in the pre-move, open ward environments are illustrated in the following exemplar quotations:
…we’ve got confused patients. They’re all constantly shouting out. And where we are now, we can shout over ‘I’ll be with you in a minute.’ When you’re in your rooms, you’re not going to know who's shouting, so I think it's going to be challenging in that kind of way, not knowing where to go, how to prioritise yourself really. Whereas here you can look out and see, ‘Well, I’ll go to her first’ or say to someone ‘If I go to her, will you go to her?’ (AAU, pre-move)If you are in with somebody else, the majority of our bays, they can see the nurses' station, so if I'm busy with somebody they know I'm going to be a few minutes but they can still press their buzzer and call the attention of somebody else… […] Or if I'm with somebody and I am going to be a while, I'll say, 'Well, I'm with somebody, I'm going to be at least five minutes, can you press your bell and one of the other nurses will come.' And it's an immediate reassurance and you're not going to get that in the new hospital. (AAU, pre-move)
The examples above illustrate how communication that aims to ensure the needs of patients are met is enabled by a space that allows wide-angle visibility and easy transfer of sound/voice. This corresponds to what Pallasmaa describes as ‘peripheral’, or context-rich, vision in his study of architectural forms (Pallasmaa, 2012). Fig. 3 provides a sense of the view nursing staff had of inpatient beds in the open-plan surgical ward of the old hospital building. The nurse who took this photograph (Fig. 3) said she could sit at the desk (particularly on night duty) and could see all 8–10 patients including those out of this particular shot. By contrast, Fig. 4 illustrates the single room corridor in the new building, with in-board bathrooms highlighting staff's inability to see and thus check on more than one patient at a time (an in-board bathroom is located at the room's entrance and has walls protruding into the corridor, whereas in an out-board layout the bathroom is placed on the room's exterior wall). The new hospital design drew on the healing environment literature and prioritised patient views of the wooded valley surrounding the hospital. As a consequence, in-board bathrooms obscured nursing staff's sight lines along the length of the corridor, and thus apart from a short double handed corridor (i.e. a corridor where patient rooms are directly opposite each other on either side of the corridor rather than opposite ward support areas such as treatment rooms or storage rooms) on the surgical ward (which nurses preferred)- see Fig. 1- nursing staff could only see into one room at a time.
Fig. 3.
Surgical ward pre-move.
Fig. 4.
Surgical ward, post-move.
Greater awareness of a larger number of patients in the pre-move, open ward environment, further augmented by patients and visitors acting as extra ‘eyes’ could sometimes also help with, and prevent or reduce risk:
…on an open plan ward obviously you’re always looking at the patients as you walk up and down the ward to get something, or even when going to another patient you sort of like flash your eyes across everybody else. And also if one person has got a problem, somebody in the next bed - if they can’t find their buzzer for instance or they’re not compos mentis to press the buzzer - then there is always somebody there that knows that patient needs a nurse or he or she is climbing out of bed. So you’ve got a sort of extra pair of eyes. (Surgical ward, pre-move)
The context-rich perspective of the open ward also aided other forms of risk awareness, which – as one member of staff described – had become impossible in the all single room setting:
Yeah, staff not being able to see. Things like, a jug they (patient) knocked over on the floor, and the water making the floor slippery, you can't see that incident, you can't hear it like you used to be able to hear it, so you're just not aware of it as soon as you would have been in the old place. So things like that. (Surgical ward, post-move)
In participants’ comments the visual and auditory dimensions of their sense of ‘having the pulse’ of the ward environment - which we would recognise as situation awareness - were closely intertwined. This integrated visual and auditory perception made possible by the open-plan space enabled staff to safeguard and monitor patients in a way that they perceived as more effective, but it also helped them to ask for support from colleagues and offer it when required.
3.2. Being aware of colleagues presence and workload: teamwork and mutual support
For nursing staff being able to call for help, having an immediate visual perception of what help is available, and being able to tell whether a colleague is struggling and may need help were central to teamwork on the wards. An experienced nurse on the surgical ward explained the advantages of the open-plan ward in terms of staff being able to work more efficiently by having an ‘at-a-glance’ sense of what needed to be done and who was available:
One benefit of having this kind of Nightingale ward is that you can see if somebody's making a bed, you would just go up and help them make the bed because it's quicker to make a bed with two and you can chat while you’re making the bed. You can just see what needs to be done at a glance and if you need something you can just pop your head out the curtain and just say, ‘Will somebody get me …’ save you taking all your apron off and that just happens all the time. (Surgical ward, pre-move)
It was important, especially for nurses in supervisory roles, to be able to tell when colleagues might need help or were under strain. This very much depended on the ability to see and hear each other during a shift, which, as the quotes below exemplify, was much more of a challenge in the all-single room setting:
It's just nice that we all work so much as a team because we can visibly see each other all the time. And if somebody's looking a bit tired or a bit, you know, I’m talking about staff now because if you’ve had a really long day you think, ‘Oh poor thing, I’ll do this for you, you go and do something that's less …’ But we do, we’re very nurturing I think, very nurturing of each other. You can see if somebody is flagging or you can see if somebody's not doing perhaps as much as they could do and you say, ‘Oh could you just come and help me do this?’ (Surgical ward, pre-move)
…So how some of the junior nurses are coping with that kind of pressure… and that is a direct result of the [single room] environment, really because you can’t eyeball nurses enough to know that they’re drowning and they need help. (AAU, post-move)
Being able to help and support each other depended on being able to see but also, and sometimes more importantly, to hear one another. Nursing staff working in the new hospital commented positively on how single rooms were more conducive to having difficult or sensitive conversations with patients enabling them to open up more to staff, and how they significantly reduced noise disturbing people's sleep/rest. However, they also affected the extent to which staff could call for help. Prior to the move, a participant from the surgical ward commented:
If you’re in a (single) room and need a hand quite quickly, you can buzz your buzzer whereas here [on the open-plan ward] we buzz the buzzer but we shout as well, we just say ‘I need a hand’. But they might not hear you when you’re in a side room. (Surgical ward, pre-move)
Once in the new hospital building, staff found that such broader interactions with colleagues had decreased. The informal conversations that staff could have on an open ward did not take place unless people went on breaks together, which was rarely possible, or if they established friendships that continued outside the workplace. A staff nurse comments before the move:
We have… not unprofessionally, but we have a laugh to keep our spirits up for a twelve and a half hour shift, we have to keep each other happy. And I think that works really well where we are because we’re a good group and we do work well as a team. But we do keep each other really happy. We have a laugh and stuff whilst we work, so it's quite nice, when you do to about eight o′clock and everyone's feeling really tired and maybe this person tells a little joke and it just uplifts and then you’re ready to go for the next half an hour. So yes, we do work as a good team I think. (AAU, pre-move)
Research evidence shows that this informal interaction matters; it contributes to keeping up morale and helps keep stress under control, it is also often used to communicate information about patients (Adams et al., 2013). In the open plan environment, nursing staff had opportunities to integrate clinical information about patients through informal catching up with colleagues which was much more difficult in the single room environment.
The design of the physical space post move also contributed to a loss of informal learning because staff could no longer see colleagues care delivery or hear colleagues’ interactions with patients when conversations were confined to the privacy of single rooms:
You overhear someone working behind a curtain and you pick up and you think ‘That was a really nice thing they did for that patient. Maybe I’ll try that’. I think that's definitely missing, picking up on things from each other that way. Because you don’t hear people because they’re in a room, or it's not as easy to hear how they interact with people, you have to follow them. (AAU, post-move)
A space that allows staff to watch and listen to more experienced colleagues at work can also enable modelling of good practice and effective communication. These highlight that a ward design that concerns itself primarily with facilitating one-to-one staff-patient communication also needs to pay attention to the forms of communications it may inadvertently obstruct. The following section on the less desirable effects of patients’ reduced awareness of nursing work on the ward further supports this argument.
3.3. Being seen and heard by patients: Invisible nursing work
Just as there is a significant change to what nursing staff can see and hear resulting from the changed ward design, there is a corresponding change in what patients are able to witness. Nursing work, and especially the care of other patients, becomes largely invisible to patients. They can neither see nor hear care happening. This has important implications for nursing staff's experiences of working in an acute hospital setting. Nurses and clinical support workers in our study had concerns regarding patients’ isolation and possible loneliness in the all-single room environment. Overall they felt that in open plan environments, patients were more likely to talk to one another and socialise and this was considered an important factor for recovery (an example of this was documented in one of the pictures taken by staff, see Fig. 5). The ‘day rooms’ of the new single room wards were seen as inadequate and uninviting by staff who felt that patient socialisation was definitely hindered in the new environment. Patients reported not being orientated to the whole ward and described a lack of information from staff about day room facilities or other communal areas (although AAU did not have a dayroom) and reported not knowing if they were able to leave their rooms and meet others (Maben et al., 2015a).
Fig. 5.
Surgical ward, pre-move.
In the pre-move open-plan setting, different forms of collaboration seemed to take place, both between patients and between patients and staff:
…on the open ward if they [patients] are aware that you’re short-staffed I think people that are up and about will help the other patients a bit more as well, because they know that you’re short-staffed, whereas in a room they can’t tell that you are short-staffed. And also they can see what's going on – patients can see what's going on. So if you’re busy with something then they won’t ask you to do something until you’ve finished with that, although not all the time. (Surgical ward, pre-move)
The physical barriers to socialisation for patients in the new hospital meant reduced opportunities for patients to help and support each other when staff were not immediately available. Following the move to the new hospital building, a nurse from the surgical ward commented:
…before, people were very caring towards each other, I think, because most people do like to help other people don’t they, and support other people? And I think even when people are in, being sick, they still get huge benefits from being supportive to people around them. So, there's been a lot of changes in that respect. (Surgical ward, post-move)
But another, perhaps even more prominent issue, was the extent to which interactions between staff and patients were affected by the ward layout. In the new hospital layout, nursing staff noticed that patients seemed to be less aware of how busy staff were on the ward.
…people think because they haven’t seen you you’re not working. Whereas in the six-bedded bay even if you just walked into that bay and walked back out again they’ve seen you, they know you’re busy. (AAU, post-move)
…if you’ve got a very poorly patient going on, taking one to two of your nurses up, you’ve still got relatives coming in, wanting to speak to doctors, and they don’t see that, they don’t see that busy bit, because it's in a room shut away. (AAU, post-move)
Patients being less aware of what nursing staff were occupied with had several implications. First and foremost it meant patients might occasionally feel neglected. It also meant that, combined with the reduced interaction among patients (see above), each individual interaction would often be more time-consuming, patients wanted to prolong the interaction due to the relative infrequency (compared to the open ward) of seeing other people (patients and staff). An AAU nurse commented on how simply introducing herself was now taking up a lot of time:
…now I have to go into each and every room and keep repeating myself. I do find the patients are more chatty because I think sometimes if they haven’t got that much family coming to see them they keep you for a little bit longer… (AAU, post-move)
In open wards staff could easily greet a group of people and patients felt less isolated because they were regularly seeing staff even if those staff were not directly caring for them. More strikingly, after the move to single rooms patients’ reduced awareness of nurses’ work meant some members of staff felt patients had unrealistic expectations of care. Some participants commented that the new layout meant patients were more “demanding”, and that they seemed to confuse the hospital with a hotel, as the interview extracts below illustrate:
I think it's lonely, and I think patients are much more difficult now, I think that's what's come with the single rooms. They do believe they’re in a hotel, I’m sure! Because it is very posh, very smart, very high spec, and as I say to you I think, really, they don’t realise there's 29 other rooms. And they’re not really interested that there's 29 other rooms.(Surgical ward, post-move)
Somebody has actually said, 'Oh, I think I'll stay another night in this hotel,' and they have compared it to a hotel and somebody has turned around and said, 'It's not a hotel, it's a hospital.' But they're treating it a bit like it is a hotel because they've got everything there, haven't they? They've got the TV and the en-suite. […] I think because they are behind a closed door, they don’t see what we’re doing and how busy we are and you get some people that are just buzzing for you to go in just because they want to see somebody and they will make some little excuse – ‘Oh can you pass me that?’ where it's in front of them and they can get it themselves. (Surgical ward, post-move)
Patients on open plan wards, especially male patients, also noted the importance of having others to distract them and stop them worrying about themselves and their own illnesses (Maben et al., 2015a, Maben et al., 2015b). Undoubtedly single rooms allow for different forms of interaction compared to open ward settings. Discreet and uninterrupted one-to-one communication and interaction are possible and this is an important aspect of person-centred care. Patients opened up more to staff due to enhanced privacy and confidentiality (Maben et al., 2015a) and nursing staff can dedicate their full attention to each patient individually, without being distracted by the busy environment of the open ward. Staff suggested this was a welcome change but that it also meant a lot more time spent talking to some patients, and the staff worried they were neglecting others as a result.
Well, if somebody calls you once you get into the side room, you’re really oblivious, aren’t you, to everything else? I mean, that's lovely in lots of ways, because you can really concentrate on your patient and you can have good communication with your patient without any distraction, but you probably are in there for maybe a lot longer, well certainly you would be in there for a lot longer with them, than you would have been if they’d been on an open ward. Because they would have heard you being called, or they would have seen there was a need elsewhere. And people do keep you in there for quite a long time. (Surgical ward, post-move)
Finally, the micro-environment of the single room was found to create conditions that affected the power dynamics of the ward dramatically; the single room was more like the patients’ space or their home. One participant explained how she felt uncomfortable going into a room where a patient had many family relatives/visitors:
I think as well, when relatives come in – this is another thing with the single rooms- when they come in and they’re with their relative, or with the patient, and especially if you have a big family come in, you feel a bit like you’re intruding […] You feel a bit like you’re on a show. (Surgical ward, post-move)
We would not define challenges to traditional power dynamics in healthcare, which often see health professionals define the modes and boundaries of interaction, as an undesirable outcome of design innovation. However, as we argue in the discussion below, such potential challenges need to be considered carefully and discussed with staff to prepare them for these changes and create ways to counter the negative impacts.
Finally, in terms of differences between the two wards and Pallasmaa's distinctions, staff on the surgical ward felt more enabled visually and aurally - in terms of seeing and hearing staff and patients - by the presence of the double handed corridor (not present in the AAU) due to the perceived enhanced geographical proximity of the rooms (with rooms being opposite each other rather than in linear arrangement). Staff could position themselves equidistant from the entrance of three to four patient rooms as opposed to only two in the linear/single handed corridor arrangement of rooms. On the surgical ward, patients with dementia and/or at high risk of falling, would be deliberately allocated (or moved as soon as possible) to a room on the double-handed corridor to enhance surveillance (an option not open to AAU staff). On the AAU, falls-risk patients were regularly observed sitting outside the room (on what was essentially a long dark corridor) so staff could ‘keep an eye’ on them. Interestingly, since completion of the study the hospital has converted a Board Room and offices into a new 38 bedded ward which is not 100% single rooms and comprises nine 4-bedded bays and two side rooms.
The general adult wards in the new hospital (including the surgical ward considered here) were designed with a view to ‘decentralised’ nursing teams (usually three staff members) looking after ‘clusters’ of 10 patient rooms. So, for example, a ward team of 10 members of staff would be split into three ‘decentralised’ teams working at their own ‘local’ base next to the rooms for which they are responsible. Unlike the general adult wards, AAU had a unique layout that staff found difficult to adapt to and which did not enable staff to work in decentralised teams caring for patients in 10 single rooms as easily as on the surgical ward. The unique layout of AAU created an additional challenge whereby one ‘area’ had its 10 rooms located round the U at the end of the ward finger – meaning that staff could only see/hear some of their call bells as the central ward support acted as a visual and aural barrier to that ‘area’. The priority for the AAU was finding a configuration of decentralised nursing teams that enabled staff to work effectively in the nonstandard ward layout. This was a protracted process that was described by staff as stressful and disruptive. The surgical ward, with its established leadership and teamwork (Maben et al., 2015a), focussed on supporting the team to deliver good care overall rather than prioritising one particular challenge. In terms of maintaining situation awareness, the surgical ward deliberately retained a central handover of all staff every morning, which the ward manager felt was important for communication, maintaining ward identity and counteracting the segregation caused by decentralised working.
The AAU faced more challenges than the surgical ward, with changes in size of the ward, increased acuity of patients and decreased level of staffing (initially) with a legacy of staffing difficulties (high turnover, high reliance on agency staff) that remained unresolved and meant a lack of continuity for the team overall. Both wards had the same leader pre and post move, however, the surgical ward appeared to have the more favourable context for the move with fewest concurrent changes, a small reduction in beds and a strong leader, who emphasised communication and mutual support for staff. Staff in the AAU reported transition difficulties, taking more than 6 months to settle in, whereas on the surgical ward the team reported adapting fairly rapidly. Whilst these comparisons have highlighted a number of differences in design and adaptation to differing built environments, it is also important not to examine design implications in isolation as differing contextual factors also shape how design influences teamwork, safety and patient experiences of care delivery. Thus apparently common sense changes in design require rich and substantial evaluation to illuminate fully the consequences of such changes (Ramsay and Fulop, 2015).
4. Discussion
Informed by the distinction drawn by Pallasmaa between ‘focused’ and ‘peripheral’ vision which we illustrated in our Background section, our interpretation of staff experiences explores the extent to which ‘focused’ perception is prioritised or predominates and the extent to which ‘peripheral’ – or ‘contextual’ – perception is facilitated or hindered in different built environments. We begin to see that different forms of attention are encouraged by the two different ward designs examined here. Our choice of theoretical lens is very specific and aims to keep us focused on sensory aspects of nursing work. Other theoretical lenses would have lent themselves to analysing the experiences of nursing staff in the pre- and post-move environments – for example Foucault's readings of surveillance and the panopticon (Foucault, 1973, Foucault, 1977) or Goffman's stage metaphors (Goffman, 1959); however, we were interested in drawing upon scholarly work from architectural theory with a view to emphasising the contribution that this work can make to understanding nursing work. In its original formulation, Pallasmaa's distinction between focussed and peripheral vision aimed to support the author's passionate argument that the world of architecture too often prioritises vision over other sensory forms of experiences. In our analysis, we were cautious not to extend this argument to our analysis, but to draw on the distinction itself as a tool to interpret our data.
With Pallasmaa's distinction in mind, the open plan space of the Nightingale ward or the multi-bedded bay is rich in contextual and preconscious information. Nursing staff can direct their focus to individual patients and remain aware – at least to some extent- of the needs of other patients and colleagues in the room as well as to the broader environment more generally. Single rooms, on the other hand, largely prioritise what, to follow Pallasmaa's distinction, we could call ‘focused vision’ in the sense of focused one-to-one interaction, away from possible sources of distraction and interruption. We suggest that, by prioritising a ‘focused vision’ type of interaction between nursing staff and patients aimed at enhanced patient-centredness, an all-single room ward design may be neglecting the importance of context-rich interactions on staff's working practices and wellbeing at work.
The analysis presented in this paper speaks to two broader academic fields. Drawing upon architectural theory, it aims to contribute to the body of social scientific work focusing on the role of the spatial in the constitution and shaping of social worlds. Despite recurring calls over the last two decades for more attention to space and place in the sociology of organisations (e.g. Halford, 2008) and a dedicated sociology of place (e.g. Gieryn, 2000), to date the role of architecture and buildings remains largely overlooked by sociologists and left to geographers (Martin et al., 2015). As Löw (2016, p.ix) puts it: “It seems that the predominant impression is that specialists are supposed to attend to spatial phenomena (e.g. sociology of architecture or urban sociology) but that society, or, to put it in terms less charged with presuppositions, the social can be largely understood without a theory of space” (2016, p. ix). We also aim to feed into the more established tradition of nursing research by taking a distinctive space-sensitive approach to the study of professional practices and relationships (e.g. Andrews, 2016; Andrews and Shaw, 2008; Conradson, 2003).
Although the all-single room design may be underpinned by principles of egalitarianism (all patients admitted to the ward are entitled to the privacy and dignity that single rooms afford) and patient-centredness (patients are attended individually, cared for in the privacy of the single rooms, with enhanced confidentiality and minimal disruption), it seems to place significant demands on staff's abilities to adapt to a work environment which offers fewer opportunities for mutual support, situation awareness, effective prioritisation of care, and collective reassurance of patients. We suggest that this work environment, although conducive to privacy and dignity of care, also has the potential to impoverish – rather than enhance – other aspects of patient experience of caring as well as for staff working there.
Crucial though it is, patient experience cannot be separated from staff experience of care and it is known that more positive staff experiences are an antecedent to more positive patient experiences (Maben et al., 2012a, Maben et al., 2012b) and support good patient outcomes (Rafferty et al., 2007). The all-single room ward environment fosters predominantly – if not exclusively – forms of interactions that are context-poor and therefore limit staff's abilities to draw on valuable ‘peripheral’ information, both in their caring for patients and in their supporting each other as a team. Our data illustrate how in the new hospital, in most circumstances, the only opportunity for staff to catch up about patients was when they were undertaking tasks together and at planned meetings and these opportunities were fewer than in the previous open-wards of the old hospitals. Important issues of privacy and confidentiality make dedicated meetings optimal for discussing clinical information concerning patients, however, informal information exchange and catching up that were more likely in the open plan environment were deemed important for teamwork and patient monitoring, confirming existing evidence (Adams et al., 2013). The potential of the all-single room design to undermine effective staff teamwork (including collaboration between staff and patients) can ultimately prove detrimental for patient-centred care. Also, in open wards, where sight and hearing are less obstructed, we have seen that there can be instances in which patients help each other and support nursing work by alerting nurses to situations that need immediate attention.
These forms of collaboration seem important to us in that they disrupt the ‘us-and-them’ boundaries that too often are drawn between health professionals and patients. This is particularly interesting when considered alongside the potential for inversion of power relations that the enclosed space of the single room seems to engender at times. Our findings highlight how some nursing staff felt they now had to ‘enter’ the patient's bounded space of the single room, could feel ‘intrusive’ in doing so, and felt less able to exercise some degree of control on the agendas and duration of their interactions with patients. We suggest that without careful consideration of wider cultural and contextual experiences all-single room ward design risks hindering collaborative forms of communication between patients and nursing staff whilst also altering power dynamics in a way which rather than empowering patients has the potential to disempower all parties involved.
5. Conclusion
Changes in ward design result in complex changes in staff's and patient's experiences of care, well beyond the immediate implications for safety, privacy and dignity. By privileging ‘focused’ – i.e. context-poor – visual and auditory forms of perceptions, all-single room hospital accommodation may be offering staff an impoverished experience of caring for patients. Although aspiring to enhanced patient-centredness – in the sense of safeguarding patient dignity and privacy and creating the condition for one-to-one communication and listening, - it may actually prove disempowering for both staff and patients. Paying attention to the sensory experiences of the built environment of all social actors in a healthcare setting permits the illumination of how changes in the dimensions of spatial experience translate into intended as well as unintended changes in the social relationships of nursing care.
Funding source
This work was supported by the Department of Health, National Institute for Health Research (NIHR), Health Services and Delivery Research Programme (HS&DR, grant number 10/1013/42).
Disclaimer
The views and opinions as expressed herein are those of the authors and do not necessarily reflect those of the HS&DR Programme, NIHR, NHS or Department of Health.
Ethical approval
King's College London Psychiatry, Nursing and Midwifery Research Ethics Committee (PNM/09/10-30).
Contributor Information
S. Donetto, Email: sara.donetto@kcl.ac.uk.
C. Penfold, Email: cp10008@medschl.cam.ac.uk.
J. Anderson, Email: janet.anderson@kcl.ac.uk.
G. Robert, Email: glenn.robert@kcl.ac.uk.
J. Maben, Email: jill.maben@kcl.ac.uk.
References
- Andrews G.J. Geographical thinking in nursing inquiry, part one: locations, contents, meanings. Nurs. Philos. 2016;17(4):262–281. doi: 10.1111/nup.12133. [DOI] [PubMed] [Google Scholar]
- Andrews G.J., Shaw D. Clinical geography: nursing practice and the (re) making of institutional space. J. Nurs. Manag. 2008;16(4):463–473. doi: 10.1111/j.1365-2834.2008.00866.x. [DOI] [PubMed] [Google Scholar]
- Adams M., Robert G., Maben J. “Catching up”: the significance of occupational communities for the delivery of high quality home care by community nurses. Health. 2013;17(4):422–438. doi: 10.1177/1363459312460703. [DOI] [PubMed] [Google Scholar]
- Charmaz K. Sage; London: 2014. Constructing grounded theory. [Google Scholar]
- Conradson D. Geographies of care: spaces, practices, experiences. Social. Cult. Geogr. 2003;4(4):451–454. [Google Scholar]
- Draper J. Embodied practice: rediscovering the ‘heart’of nursing. J. Adv. Nurs. 2014;70(10):2235–2244. doi: 10.1111/jan.12406. [DOI] [PubMed] [Google Scholar]
- Foucault M. Pantheon; New York: 1977. Discipline and Punish. [Google Scholar]
- Foucault M. Tavistock; London: 1973. The Birth of the Clinic. [Google Scholar]
- Gieryn T.F. A space for place in sociology. Annu. Rev. Sociol. 2000;26(1):463–496. [Google Scholar]
- Goffman E. Doubleday Anchor; New York: 1959. The Presentation of Self in Everyday Life, [Google Scholar]
- Halford S. Sociologies of space, work and organisation: from fragments to spatial theory. Sociol. Compass. 2008;2(3):925–943. [Google Scholar]
- Halford S., Leonard P. Space and place in the construction and performance of gendered nursing identities. J. Adv. Nurs. 2003;42:201–208. doi: 10.1046/j.1365-2648.2003.02601.x. [DOI] [PubMed] [Google Scholar]
- Löw M. Palgrave; New York: 2016. The Sociology of Space: Materialities, Social Structures, and Action. [Google Scholar]
- Maben J., Adams M., Peccei R., Murrells T., Robert G. ‘Poppets and parcels': the links between staff experience of work and acutely ill older peoples' experience of hospital care. Int. J. older People Nurs. 2012;7(2):83–94. doi: 10.1111/j.1748-3743.2012.00326.x. [DOI] [PubMed] [Google Scholar]
- Maben J., Peccei R., Adams M., Robert G., Richardson A., Murrells T., Morrow E. NIHR Service Delivery and Organization Programme; Southampton: 2012. Exploring the Relationship Between Patients' Experiences of Care And the Influence of Staff Motivation, Affect and Wellbeing. Final report. [Google Scholar]
- Maben, J., Penfold, P., Glenn, R., Griffiths, P., 2012c. Evaluating a major innovation in hospital design: Workforce implications and impact on patient and staff experiences of all single room hospital accommodation. Report of phase 1 findings for HaCIRIC2012. https://www.kcl.ac.uk/nursing/research/nnru/publications/Reports/Single-Room-Hospital-Accomodation---HaCIRIC-Phase-1-Report---June-2012.pdf. [PubMed]
- Maben J., Griffiths P., Penfold C., Simon M., Pizzo E., Anderson J., Barlow J. Evaluating a major innovation in hospital design: workforce implications and impact on patient and staff experiences of all single room hospital accommodation. Health Serv. Delivery Res. 2015;3(3) [PubMed] [Google Scholar]
- Maben J., Griffiths P., Penfold C., Simon M., Anderson J.E., Robert G., Barlow J. One size fits all? Mixed methods evaluation of the impact of 100% single-room accommodation on staff and patient experience, safety and costs. BMJ Qual. Saf. 2015;22:241–256. doi: 10.1136/bmjqs-2015-004265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malone R.E. Distal nursing. Soc. Sci. Med. 2003;56(11):2317–2326. doi: 10.1016/s0277-9536(02)00230-7. [DOI] [PubMed] [Google Scholar]
- Martin D., Nettleton S., Buse C., Prior L., Twigg J. Architecture and health care: a place for sociology. Sociol. Health Illn. 2015;37(7):1007–1022. doi: 10.1111/1467-9566.12284. [DOI] [PubMed] [Google Scholar]
- Pallasmaa J. John Wiley & Sons; Chichester: 2012. The Eyes of the Skin: Architecture and the Senses. [Google Scholar]
- Pennington H., Isles C. Should hospitals provide all patients with single rooms? Br. Med. J. 2013;347:18–19. doi: 10.1136/bmj.f5695. [DOI] [PubMed] [Google Scholar]
- Priest S. Merleau-Ponty's concept of the body-subject. Nurs. Philos. 2000;1:173–174. [Google Scholar]
- Rafferty A.M., Clarke S.P., Coles J., Ball J., James P., McKee M., Aiken L.H. Outcomes of variation in hospital nurse staffing in English hospitals: cross-sectional analysis of survey data and discharge records. Int. J. Nurs. Stud. 2007;2007(2):175–182. doi: 10.1016/j.ijnurstu.2006.08.003. (Epub 2006 Oct 24) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsay A.I., Fulop N.J. Why evaluate ‘common sense’quality and safety interventions? BMJ Qual. Saf. 2015;25:224–225. doi: 10.1136/bmjqs-2015-004755. [DOI] [PubMed] [Google Scholar]
- Simon M., Murrells T., Griffiths P., Maben J. Is single room hospital accommodation associated with differences in health care associated infection, falls, pressure ulcers or medication errors? A natural experiment with non-equivalent controls. J. Health Serv. Res. Policy. 2016 doi: 10.1177/1355819615625700. (1355819615625700. Published online before print January 24, 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stichler J.F. Creating a healing environment in critical care units. Crit. Care Nurs. Q. 2001;24(3):1–20. doi: 10.1097/00002727-200111000-00002. [DOI] [PubMed] [Google Scholar]
- Ulrich, R.S., Zimring, C., Zhu, X., DuBose, J., Seo, H.-B., Choi, Y-.S., et al., 2008. A review of the research literature on evidence-based healthcare design. Healthcare Leadership: White paper series: The Center for Health Design. 〈https://www.healthdesign.org/sites/default/files/LitReviewWP_FINAL.pdf〉 (Accessed 24 January 2017).
- West P., McDonagh S., Burke M., Trueman P. Department of Health; London: 2010. Evaluation of Hillingdon Hospital Single Rooms Pilot Site - Part 1: final Literature Review and Final Report.〈http://webarchive.nationalarchives.gov.uk/20130314154404/https:/publications.spaceforhealth.nhs.uk/stream.php?id=7z7gspo38a6dr=4=rp3nqsso8p45q8sp844p7r11〉 (Accessed 24 January 2017) [Google Scholar]
- Young P., Yarandipour R. Examining the case for single rooms. Health Estate J. 2007;61(8):85–86. [PubMed] [Google Scholar]