Abstract
Background
The prevalence of sway back posture (SBP) is very high among elite gymnasts. This posture may be partly due to the improper function of lumbar multifidus muscles (LMM) as lumbar stabilizers muscles.
Purpose
The aim of this study was to compare the thicknesses of LMM measured at rest and during the contraction elicited during an arm lift between elite gymnasts with SBP and normal posture.
Study Design
Observational, descriptive, comparative
Methods
The participants consist of twenty gymnasts between the ages of 17 and 30 who had trained in gymnastics for more than ten years. They were assigned to two groups: SBP (n=10) and control (n=10). Posture analysis with grid paper and plumb line was performed for all subjects. The thickness of LMM on dominant side of spinal column was measured by a real-time ultrasound at five lumbar levels. The thickness of the LMM was measured both at rest and during the contraction elicited during an arm lift. The variation between the LMM thickness between the muscle at rest and muscle at the peak of contraction was regarded as LMM muscle function.
Result
The thickness of LMM was less in SBP group than the control group at all lumbar segments. The variation in LMM thickness between the state of rest and muscle contraction was significantly less in athletes with SBP than controls when compared at all levels of the lumbar spine (p < 0.05).
Conclusion
The function of LMM may be disturbed in athletes with SBP as demonstrated by decreased thicknesses of LMM found in gymnasts with SBP. Additionally, the thickness of the LMM as a strong antigravity and stabilizing muscle group was decreased during arm raising in gymnasts with SBP.
Level of Evidence
3a
Keywords: Gymnastics, lumbar multifidus, sway-back posture, ultrasound imaging
Introduction
Posture, which is the relative disposition of the body at any one moment, is composite of the different positions of the joints at that time.1 A “well balanced posture” is the result of an interaction between the musculoskeletal system, nervous system and contextual effects.2 On the other hand, the faulty posture is result of an imperfect relationship among various skeletal structures of body. In such an example, the body is balanced less efficiently over its base of support. Therefore, any limitation, imbalance, or misalignment of musculoskeletal structures will have a significant effect on the efficiency of movements.
Sway-Back Posture (SBP) is the most common deviation or faulty posture of sagittal alignment1,3 characterized by anterior translation of the pelvis and hip joints, beyond the center of gravity line, a flatted curve in the lumbar region and overextended hip and knee joints.2 In one study, it has been reported that 35% of young girls may be affected by sway back posture.4 In a study that specifically included gymnasts, 80% of female gymnasts demonstrated SBP, which suggests that this postural fault is highly prevalent in this population.5
Gymnastics is a competitive sport that involves a series of maneuvers requiring strength, flexibility, balance and high levels of motor control. It consists of many different styles including artistic, rhythmic, trampoline, tumbling, and aerobic gymnastics. Artistic gymnastics is the best-known style, which includes different events for men and women. Women’s events include the vault, the uneven bars, the balance beam and the floor exercises. In gymnastics, there are six basic maneuvers including the hollow, arch, tuck, straddle, pike, and lunge, which are the basis for many skills used in by artistic gymnasts. In gymnastics, SBP may be induced as a result of competition or training programs.6 In some case, this posture may improve the gymnasts’ ability at different levels of the competition. However, this posture may also predispose the gymnasts to an imbalance in spinal musculature, which when carried into performance may induce pain and disability. Low back pain is the most common complaint reported by 50% of young artistic gymnasts (11-19 years old), occurring as a result of curve changes in lumbar region.6
A significant correlation between SBP and low back pain has been reported by O’Sullivan et al.7 The authors revealed that lumbar multifidus activity decreased while subjects were in sway standing. The lumbar multifidus muscles (LMM) are important muscles that function to stabilize the lumbar vertebrae and pelvis. Researchers have suggested that the size and activity of LMM decreased in people with low back pain.8,9 Smaller size of LMM and loss of stability has been observed in the lumbar spine of patients with LBP.5,10,11
The multifidi are the deepest spinal extensors that serve to produce tension and contract to stabilize against external loads. According to different authors, it has been shown that actions like arm lift or straight leg raising, increase the load on the spinal column and result in the contraction of the spinal stabilizer muscles including the lumbar multifidus.5,28 Moseley et al30 indicated that activation of different elements of LMM occur concurrently with voluntary arm lift. Therefore, arm lift was chosen as a functional and dynamic task for use in this study to examine the contraction of the lumbar multifidi.
Ultrasound imaging (USI) is a painless, noninvasive, and real-time technique that can be used to examine muscle features like size, thickness, and cross section area (CSA). This technique can be utilized either at rest or during dynamic movements and it has been reported Real-time ultrasonography is a relatively simple and inexpensive method of accurately measuring muscle thickness.14 Hodges et al24 noted that LMM thickness changes in response to other muscles contracting. This change in muscle thickness between rest and contracted conditions is one measure of contraction ability. It has been shown that USI is able to image both superficial and deep muscles such as the abdominal, lumbar multifidus, and pelvis floor muscles with high reliability and validity.12,13,14,15 The USI method for imaging the lumbar multifidus muscles (LMM) can be conducted in both prone and side-lying positions and without any adverse effects on the results.16 Further, it has been confirmed that USI is a reliable and non-invasive method for recording activity and thickness changes of lumbar multifidus (MF) in low load range of dynamic functions.17
The aim of this study was to compare the thicknesses of LMM measured at rest and during the contraction elicited during an arm lift between elite gymnasts with SBP and normal posture. It was hypothesized that thickness changes (between relaxed and active conditions) of lumbar multifidus muscles may be different between gymnasts with sway-back posture and gymnasts without sway-back posture.
Materials and Methods
Sample
Twenty female gymnasts between the ages of 17-30 were recruited. They all competed in artistic gymnastics at the Iranian national championship level and were recruited from Iranian Gymnastics Federation. They were assigned to two groups: gymnasts with SBP (n=10) and gymnasts with normal posture (n=10). Age, duration of activity at an elite level, time spent training per week, and history of surgery/pain in lower back and pelvis were self-reported by all athletes.
To be included in the SBP group the subjects could not be performing exercise therapy or training for daily activities (such as correcting standing posture or doing exercises in order to correct the SBP). The exclusion criteria were: 1) any history of surgery of the spine, lower extremity or pelvis, and 2) musculoskeletal disorders like spasm, tendonitis, sprain and strain, fracture or dislocation of the spine or pelvis. Prior to involvement in the study, the study protocol was explained to all participants and it was their option to participate in this study. After acceptance, they were given a questionnaire to fill out. Height and weight was measured and the values were used to obtain their BMI. Consequently, the two groups were matched by means of age, time training and anthropometric variables such as weight, height and body mass index (BMI= weight / squared height) (Table 1).
Table 1.
Characteristic of the sway-back posture and control groups expressed as mean and standard deviation (SD) and range (significance level p < 0.05)
| Sway-Back Posture (n=10) | Normal Posture (n=10) | P Value | |
|---|---|---|---|
| Age (year) | 22.30±4.44 | 22.50±4.76 | 0.924 |
| Range | 17−30 | 16−30 | |
| Weight (kg) | 52.27±8.00 | 56.95±4.47 | 0.124 |
| Range | 36.90−69.00 | 48.30−64.00 | |
| Height (cm) | 160.80±0.06 | 161.20±0.05 | 0.881 |
| Range | 151−172 | 153−168 | |
| BMI (kg/m²) | 20.11±2.13 | 21.94±1.89 | 0.058 |
| Range | 16.18−23.32 | 19.10−24.43 | |
| Time Training (h/week) | 27.30±4.07 | 25.90±3.73 | 0.143 |
| Range | 22−35 | 20−32 |
Posture analysis
In order to evaluate posture, a plumb line and grid paper was used according to the methods described by Kendall.2 A similar technique was used by Mulhearn5 and Dolphens19 in their studies examining posture. The distance between the grid paper on the wall and plumb line that hung from the roof was 45 centimeters. The researchers adjusted the plumb line to be parallel to with one of lines on the grid paper. Markers were placed on the seventh cervical spinous process, the middle of greater trochanter and the middle of lateral malleolus. Then the gymnasts were asked to stand between the grid paper and plumb line so that the plumb line passed the middle of the lateral malleolus marker. Their feet were in the natural toe out position with 15cm distance between 1st metatarsals for all subjects. Then they were asked to put equal weight on both feet. They held this position for three minutes (this is necessary to allow enough time for them to achieve their habitual posture). To standardize the head posture, the ear meatus was aligned with the marker and the gymnasts were asked to look at a marker that was placed on the wall. The researchers then observed their final posture and checked the plumb line. If C7 and the greater trochanter were behind the plumb line, the gymnast was placed in the sway-back posture group, all others were placed in the normal posture group.19
Lumbar lordosis measuring protocol
In the current study, a flexible ruler (Intra-tester reliability of 0.92, Inter-tester reliability of 0.82 and validity of 0.91 when compared to X-ray)20 was used to measure the angle of lumbar lordosis. At first, the lumbar vertebrae were identified using iliac crest as a landmark. The angle was measured after three minutes to reach to their typical posture. The flexible ruler was placed on the middle of the lumbar region, conforming to the spinal posture of the athlete (Figure 1). The spinous processes of L1 and S2 vertebrae were marked on the ruler. Then without altering the shape of the flexible ruler, the convex side of the ruler was drawn on a paper and L1 and S2 were delineated on the paper. To evaluate the lumbar lordosis two points of L1 and S2 were connected to each other and identified as “L” then from the middle of the line “L”, another line perpendicular to the curve was added and labeled it as “H”. The following formula was then used to compute the degree of lumbar lordosis (D).
Figure 1.
Lumbar lordosis measurement using flexible ruler. The spinous processes of L1 and S2 was marked on the ruler. (L1: first lumbar vertebrae, S2: second sacrum vertebrae).
Pelvic tilt measurement
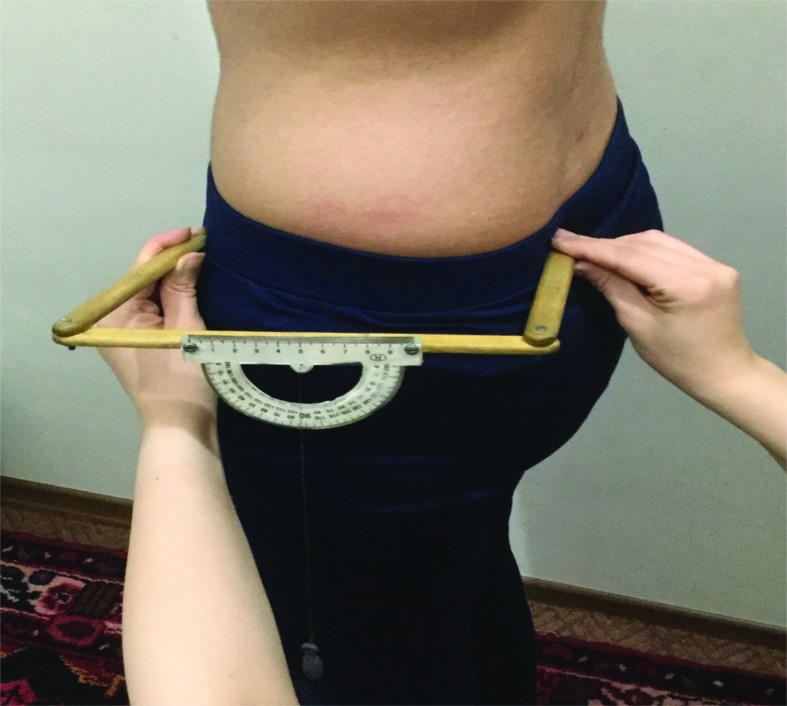
Pelvic tilt was measured with inclinometer. Arms of inclinometer were placed on the ASIS and PSIS landmarks. Then the inclination of the pelvic directly was read from protractor (Figure 2). To evaluate posterior or anterior pelvic tilt, vertical lines from anterior superior iliac spine (ASIS) and posterior superior iliac spine (PSIS) were drawn to grid paper. These two points were attached to each other with a line. The distance between the middle of line and plumb line was measured with a ruler.20 Intraclass correlation coefficient for repeated measures, Intra-tester and Intra-tester reliability were indicated 0.99.29
Figure 2.
Pelvic tilt was measured with inclinometer. Arms of inclinometer were placed on the ASIS and PSIS landmarks. (ASIS: anterior superior iliac spine, PSIS: posterior superior iliac spine).
Ultrasound imaging protocol
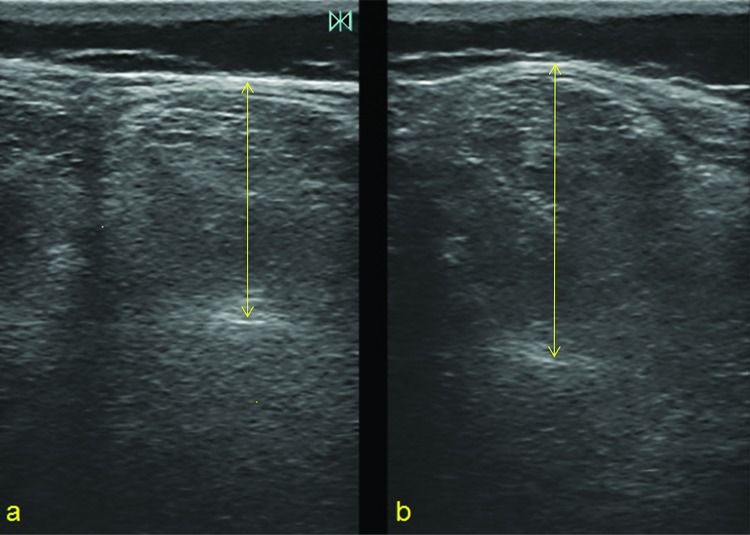
The technique was performed using a B-Mode ultrasonography device (Honda 2100, Honda Co., Japan) with a frequency of 7.5 M Hz and a linear array probe. The athletes were placed in prone position with a pillow under their abdominal region to flatten their lordosis. They were asked to relax in order to prevent any muscle contraction. The researchers used the iliac crest as a landmark to find lumbar vertebrae, and the top of the crest at the spine was identified as L4. Palpation was then used to identify other lumbar vertebrae, which were delineated by marks on the skin. By putting the probe longitudinally, the spinous processes of the vertebrae were seen on screen. Once each vertebra was found, the probe was turned to a transverse alignment. In this view, the spinous process and both transverse processes of one vertebra were identifiable. The echogenic transverse process of the dominant side of the spine was used as a landmark. Dominance was defined by asking the subject which hand she would use to write. The distance between the transverse process and the subcutaneous fascia was used as lumbar multifidus muscle thickness while the subjects were at rest. Athletes were asked to elevate their dominant arm up to the level of their ear in order to induce a contraction of the LMM. At the end of the movement, the muscle thickness was measured (Figure 3). These subsequent steps and measurements were repeated at each vertebral level from L1-L5. A total of 10 measurements were taken per gymnast to view each vertebral segment from L1-L5 while at rest and during contraction of the LMM.
Figure 3.
(a) Ultrasound image of lumbar multifidus muscle at the fifth level of vertebra with measurement of the muscle thickness at rest. (b) Ultrasound image of the lumbar multifidus contraction consequent to arm lift.
The thicknesses of lumbar multifidus muscles were measured on the display of the ultrasound device, then the thickness variation between the state of rest and contraction was computed as a measure of muscle contractility.
Reliability
The reliability of the LMM thickness, the degree of lumbar lordosis and the pelvis tilt measurement was evaluated for ten randomly selected individuals (five from SBP group and five from control group). The measurements were repeated three times with an interval of one hour within one day. The first measurement was performed as mentioned, and for subsequent measurements all markers were removed after each testing session. For all subsequent measures, bony landmarks were re-identified and markers were replaced as mentioned in the methods section. The level of ICC (3,1) for the intra-testers reliability was excellent for LMM thickness measurement in both states of rest [ICC = 0.98 (95% CI = 0.92-0.99)] and contraction [ICC = 0.96 (95% CI = 0.88-0.98)]. Excellent values were also found for the flexible ruler [ICC = 0.99 (95% CI = 0.97-.099)]; and inclinometer [ICC = 0.97 (95% CI = 0.88-0.99)].
Statistical analysis
The Shapiro-Wilk test was used to assess for normal distribution and the Levene test was used to assess the equality of variances.
An ANCOVA was used to assess outcomes using the covariate variables such as age, weight, height and BMI. Data analysis was then rendered using SPSS (version 23). Statistical significance was established as p < 0.05.
RESULTS
The measurement of lumbar lordosis was significantly less in gymnasts with SBP than the control group (p ≤ 0.008) demonstrating decreased lordosis in this posture. However, the pelvic tilt difference between the two groups was not statically significant different.
The thicknesses of the lumbar multifidus muscles were less in the SBP group compared to the control group in all lumbar segments from L1-L5 at rest, but these differences were not statistically significant. However, the thickness during contraction as induced by the action of arm lift was significantly different (p ≤ 0.031) at the level of fifth lumbar vertebra (Tables 2 and 3).
Table 2.
Thickness of lumbar multifidus muscle in all lumbar segments from L1-L5 in rest in the sway-back and control groups expressed as mean and standard deviation (SD) and range (significance level p < 0.05)
| Sway-Back Posture Group | Control Group | |||||
|---|---|---|---|---|---|---|
| Level | Mean±SD | Range | Mean±SD | Range | P Value | |
| Lumbar Multifidus?Thickness In Rest | L1 | 20.94±3.59 | 16.60−27.10 | 22.49±3.20 | 15.60−26.50 | 0.323 |
| L2 | 21.07±3.80 | 15.70−27.40 | 24.14±5.02 | 17.65−35.73 | 0.141 | |
| L3 | 22.53±3.95 | 16.10−31.35 | 24.15±3.19 | 20.00−29.40 | 0.326 | |
| L4 | 24.23±3.96 | 18.50−33.10 | 24.90±3.53 | 21.40−33.15 | 0.694 | |
| L5 | 25.16±3.12 | 20.05−29.95 | 26.47±4.54 | 21.25−35.85 | 0.460 |
L1: First lumbar vertebrae, L2: Second lumbar vertebrae, L4: Fourth lumbar vertebrae, L5: Fifth lumbar vertebrae
Table 3.
Thickness of lumbar multifidus muscle in all lumbar segments from L1-L5 in contraction consequent to arm lift in the sway-back and control groups expressed as mean and standard deviation (SD) and range (significance level p < 0.05)
| Sway-Back Posture Group | Control Group | |||||
|---|---|---|---|---|---|---|
| Level | Mean±SD | Range | Mean±SD | Range | p Value | |
| Lumbar Multifidus?Thickness In Contraction | L1 | 24.21±4.22 | 18.40−31.70 | 27.20±3.45 | 20.50−31.70 | 0.100 |
| L2 | 24.45±4.23 | 19.50−33.15 | 29.32±4.71 | 23.25−40.25 | 0.062 | |
| L3 | 26.49±4.48 | 20.15−35.15 | 29.96±2.89 | 25.45−34.65 | 0.055 | |
| L4 | 28.12±3.59 | 23.65−36.75 | 30.37±2.93 | 27.90−35.30 | 0.143 | |
| L5 | 28.63±3.28 | 23.70−32.10 | 32.41±3.10 | 27.40−41.00 | 0.031* |
Significant difference (p < 0.05) between sway-back posture group and control group
L1: First lumbar vertebrae, L2: Second lumbar vertebrae, L4: Fourth lumbar vertebrae, L5: Fifth lumbar vertebrae
The LMM thicknesses during contraction minus the LMM thicknesses at rest indicated that the thickness variation was significantly less in gymnasts with SBP when compared to the control group at all five segments (L1-L4, p < 0.05 and L5, p value < 0.001) (Table 4). The measurement of lumbar lordosis (measured with a flexible ruler) was significantly less in gymnasts with SBP than the control group (p ≤ 0.008) demonstrating decreased lordosis in this posture. However, the pelvic tilt difference between the two groups was not statistically significantly different.
Table 4.
Thickness changes of lumbar multifidus muscle between rest and contraction in response of dominant arm lifting in dominant side of spine column in all lumbar segments from L1-L5 in the sway-back and control groups expressed as mean and standard deviation (SD) and range (significance level p < 0.05)
| Sway-Back Posture Group | Control Group | |||||
|---|---|---|---|---|---|---|
| Level | Mean±SD | Range | Mean±SD | Range | p Value | |
| Thickness Variation of Lumbar Multifidus | L1 | 3.18±1.02 | 1.25−4.60 | 4.71±1.43 | 2.35−7.90 | 0.014* |
| L2 | 3.38±1.24 | 1.96−5.75 | 5.18±1.20 | 3.15−7.00 | 0.004* | |
| L3 | 3.96±1.45 | 2.15−6.50 | 5.80±1.43 | 3.70−7.60 | 0.011* | |
| L4 | 3.76±1.11 | 1.65−5.25 | 5.46±1.90 | 2.15−8.35 | 0.025* | |
| L5 | 3.47±1.33 | 1.30−6.00 | 5.93±1.49 | 3.50−8.00 | 0.001** | |
| Pelvic Tilt | 7.60±3.38 | 2.00−13.50 | 9.25±1.77 | 6.75−12.50 | 0.189 | |
| Lumbar Lordosis | 37.62±6.39 | 28.62−46.05 | 45.74±5.72 | 30.04−55.26 | 0.008* |
Significant difference (P < 0.05) between sway-back posture group and control group
Significant difference (P < 0.01) between sway-back posture group and control group
L1: First lumbar vertebrae, L2: Second lumbar vertebrae, L4: Fourth lumbar vertebrae, L5: Fifth lumbar vertebrae
DISCUSSION
In this study, USI was used to evaluate the LMM in gymnastic athletes with and without SBP. The thickness of LMM was measured in states of both rest and contraction. The variations of thickness between the two states are considered a measurement of LMM function. Sway-back posture is an adaptation of spine that occurs over time with a lot of potential side effects. It is not considered an acute injury such as those that include sprains, fractures, dislocations, muscle strains and contusions.21 Many different variables contribute to development of SBP, including the method of coaching and type of exercises, as well as growth and development.
Postural adaptations and gymnast preference appear to be important factors among gymnastic athletes that develop SBP. Training volume is another important factor and it has been shown that training more than 400 hours/year may decrease or increase the degree of lumbar lordosis,22 hovever, there was no clear difference between gymnasts volume of training between those with SBP and those without. In the current study, the athletes with SBP focused more on the vault events which requires the straight straddle and tuck positions. Furthermore, they also performed exercises like handstand flat back and handstand backward rolling in order to be successful on the vault. Therefore, while focusing on these, it is possible that differences in evolution of spinal column posture may have occurred as a result of spinal muscles imbalances, that may have happened between agonist and antagonist or synergistic spinal muscles.
Group comparison
Variation in muscle size as measured by USI has been regarded as a sign of muscle efficacy, tension and contractility.23,24 Muscle size, has been reported to significantly correlate with electromyography activities of the same muscle.24 Muscle thickness is a factor to determine the level of contractility generated by an individual muscle’s contraction.23,24 In paraspinal muscle ultrasonography, the thickness of semispinalis capitis muscle significantly increased as the force of the neck extensor muscles were increased from 0% to 100% of maximum voluntary contraction.23
In the current study, the thickness variation between state of rest and contraction (consequent to dominant arm flexion) was used as a measure of LMM function. The authors’ main goal was to determine whether these thickness changes were different between gymnasts with SBP and gymnasts with normal posture.
To find the activity or contractility of muscles by USI, difference of thickness between rest and contraction is important. Less difference of measured muscle thickness between rest and contraction indicates less activity of the LMM23,24 because the LMM are enabled to stabilize the spinal column in a correct alignment during dynamic movements. Ultrasound imaging of LMM at all five segments demonstrated significant differences in their thickness variations (obtained from the LMM thicknesses during contraction induced by the action of arm lift minus the LMM thicknesses at rest) between the SBP group and control group. Significantly greater thickness variation of LMM between two groups at the level of fifth lumbar vertebra indicates that muscles at this level were influenced by SBP. This finding was in accordance with that found by Pezoloto et al25 who documented greater fat infiltration in lumbar multifidus and other erector spine muscles at the levels of fourth and fifth lumbar vertebrae in subjects with SBP. This measurement was used to confirm greater atrophy of muscle due to the presence of more fat and may be it is because of anatomical and biomechanical properties that the greatest volume of LMM is at the L5/S1 level. Findings in the current study indicate that during contraction, the LMM thickness in SBP group was significantly less than the control group.
The amount of lumbar lordosis was significantly less in SBP subjects than the control group, which could be due to the stabilizer role of LMM. The LMM are important for maintenance of the lumbar lordosis and activity of the LMM contributes to efficient alignment of spinal column and pelvis, and those athletes with SBP had decreased activity during arm raise of the LMM. However, anterior pelvic tilt was not significantly different between the SBP subjects and the controls. Anterior pelvic tilt has been described as an important abnormality in SBP, which causes anterior shift of trunk to the line of gravity as the athlete tends to extend the trunk, with a corresponding decrease in the involvement of LMM and paraspinal muscles.25,26,27 On the other hand, the abdominal muscles such as rectus abdominis increase their work to attempt to impede the extension of lumbar vertebrae.28 These muscle imbalances have been reported in a variety of different studies.3,15,29 However, in those studies, the athletes were asked to actively recreate different postures such as sway standing or sway sitting, whereas in the current study the gymnasts were asked to demonstrate their normal, habitual posture. This difference may explain the lack of significant difference in anterior pelvic tilt found between groups in the current study
LIMITATIONS & RECOMMENDATIONS
Only athletes who were in artistic gymnastic competition were evaluated and hence more general biomechanical tests were not performed. The current results may not apply to all gymnasts. There are other limitations like sample size, lack of blinding and only the female gender being represented. The examiner was not blinded to the either groups. The authors recommend investigating the biomechanical properties of the type of exercises and training programs, which may influence the development of SBP among gymnasts which could be beneficial for education for coaches and to guide treatment for physical therapists.
CONCLUSION
In this study, ultrasound imaging was used to evaluate the LMM in gymnastic athletes with SBP. The thickness of LMM was measured in both states of rest and contraction. The variations of thickness between the two states are considered a measurement of LMM contractility. The contractility of LMM was decreased in athletes with SBP in comparison with athletes with normal posture. This may affect the normal lumbar curvature or stabilization during activity as a result of insufficient LMM contraction. The authors recommend this method to assess and evaluate the function of LMM and spinal column posture in individuals with SBP.
REFERENCES
- 1.Magee DJ. Orthopedic physical assessment. 5th edition. Saunders, Philadelphia, PA; 2007. [Google Scholar]
- 2.Kendall FP McCreary EK Provance PG, et al. Muscles: Testing and Function. 5th edition. Lippincott Williams & Wilkins, Baltimore, MD; 2005. [Google Scholar]
- 3.Smith A O'Sullivan PB Straker L. Classification of sagittal thoraco-lumbo-pelvic alignment of the adolescent spine in standing and its relationship to low back pain. Spine. 2008;33:2101-2107. [DOI] [PubMed] [Google Scholar]
- 4.Simorgh L Kheirkhah M Khakhali-Zavieh M. Investigation of sway back posture prevalence and alignment of spine and lower limb joints in this deformity. Rehabilitation J. 2006;7(2):31-37. [Google Scholar]
- 5.Mulhearn S George K. Abdominal muscle endurance and its association with posture and low back pain: An initial investigation in male and female elite gymnasts. Physiotherapy J. 1999; 85(4)210-216. [Google Scholar]
- 6.Purcell L Micheli L. Low Back Pain in Young Athletes. Sports Health. 2009; 1(3): 212-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mitchell T, O'Sullivan PB Burnett AF, et al. Regional differences in lumbar spinal posture and the influence of low back pain. BMC Musculoskel Disord. 2008;18(9):152-163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hodges PW Moseley GL. Pain and motor control of the lumbopelvic region:Effect and possible mechanisms. J Electromyog KineS. 2003;13(4):361-370. [DOI] [PubMed] [Google Scholar]
- 9.Lee SW Chan CK Lam C, et al. Relationship between law back pain and lumbar multifidus size at different postures. Spine. 2006; 31(19): 2258-2262. [DOI] [PubMed] [Google Scholar]
- 10.Dickx N Cagnie B Achten E, et al. Differentiation between deep and superficial fibers of the lumbar multifidus by magnetic resonance imaging. European Spine J. 2010; 19(1):122-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pavlova V Meakin JR Cooper K, et al. The lumbar spine has an intrinsic shape specific to each individual that remain a characteristic throughout flexion and extension. Eur Spine J. 2014; 23(1): 26-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee JP Tseng WY Shau YW, et al. Measurement of segmental cervical multifidus contraction by ultrasonography in asymptomatic adults. Manual Therapy J. 2007; 12(3): 286-94. [DOI] [PubMed] [Google Scholar]
- 13.Kristjansson E. Reliability of ultrasonography for the cervical multifidus muscle in asymptomatic and symptomatic subjects. Man Ther. 2004; 9(2): 83-8. [DOI] [PubMed] [Google Scholar]
- 14.Dupount AC Sauerberi EE Fenton PV, et al. Real time sonography to estimate muscle thickness: comparison with MRI and CT. J Clin Ultrasound. 2001;29(4):230-38. [DOI] [PubMed] [Google Scholar]
- 15.Lee JC Cha JG Kim Y, et al. Quantitative analysis of back muscle degeneration in the patients with the degenerative lumbar flat back using a digital image analysis: comparison with the normal control. Spine. 2008; 33(3): 318-325. [DOI] [PubMed] [Google Scholar]
- 16.Coldron Y Stokes M Cook K. Lumbar multifidus muscle size dose not differ whether ultrasound imaging is performed in prone or side lying. Man Ther. 2003;8(3):161-165. [DOI] [PubMed] [Google Scholar]
- 17.Kiesel KB Uhl TL Underwood FB. Measurement of lumbar multifidus muscle contraction with rehabilative ultrasound imaging. Man Ther. 2007; 2(2):161-166. [DOI] [PubMed] [Google Scholar]
- 18.McDonnell MK Sahrmann SA Van Dillen A specific exercise program and modification of postural alignment for treatment of cervicogenic headache: a case report. J Ortthop Sports Phys Ther. 2005;35(1):3-15. [DOI] [PubMed] [Google Scholar]
- 19.Dolphens M Cagnie B Vleeming A. A clinical postural model of sagittal alignment in young adolescents before age at peak height velocity. Eur Spine J. 2012; 21(11): 2188-2197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rajabi R Seidi F Mohamadi F. Which method is accurate when using the flexible ruler to measure the lumbar curvature angle deep point or midpoint of arch. World Appl Sci. 2008;4(6):849-852. [Google Scholar]
- 21.Fettorne FA Ricciardelli E. Gymnastic injuries: the Virginia experience 1982-1983. Am J Sports Med. 1987;15(1):59-62. [DOI] [PubMed] [Google Scholar]
- 22.Jose M. Muyor Pedro A. Lopez-Minarro, Fernando Alacid. Spinal posture of thorasic and lumbar spine and pelvic tilt in highly trained cyclists. J Sports Sci Med. 2011;10(2):355-361. [PMC free article] [PubMed] [Google Scholar]
- 23.Rezasoltani A Ylinen J Vihko V. Isometric cervical extension force and dimension of semispinalis capitis muscle. J Rehab Res and Dev. 2002;39(3):423-428. [PubMed] [Google Scholar]
- 24.Hodges PW Pengel LHM Herbert RD Gandevia SC. Measurement of muscle contraction with ultrasound imaging. Muscle & Nerve. 2003;27(6):682-692. [DOI] [PubMed] [Google Scholar]
- 25.Pezolato A de Vasconcelos E Defino HLA Nogueira-Barbosa MH. Fat infiltration in the lumbar multifidus and erector spine muscles in subjects with sway-back posture. Eur Spine J. 2012;21(11):2158–2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O'Sullivan PB Grahamslaw M Kendell M, et al. The effects of different standing and sitting postures on trunk muscle activity in a pain-free population. Spine. 2002;27(11):1238–1244. [DOI] [PubMed] [Google Scholar]
- 27.Sahrmann SA. Diagnosis and treatment of movement impairment syndromes. 1st edition. Mosby, St. Louis, MO; 2002. [Google Scholar]
- 28.Bogduk N. Clinical anatomy of the lumbar spine and sacrum, 4th edition. Elsevier, Philadelphia, PA; 2005. [Google Scholar]
- 29.Claus AP Hides J Mosley GL, et al. Different way to balance the spine: subtle changes in sagittal spinal curves affect regional muscle activity. Spine. 2009;34(6):208-14. [DOI] [PubMed] [Google Scholar]
- 30.Moseley GL Hodges PW Gandevia SC. Deep and superficial fibers of the lumbar multifidus muscle are differentialy active during voluntary arm movements. Spine. 2002; 27(2): E29-3. [DOI] [PubMed] [Google Scholar]
- 31.Chowdhury Salian Sh Yardi S. Intertester and Intratester Reliability and Validity of Measures of Innominate Bone Inclination in Standing Using Pelvin. Int J Innovations Sci Engineer Tech. 2015; 7(4): 5068-77. [Google Scholar]