Abstract
Introduction
Behavioral economic measurement of the relative value of tobacco (Cigarette Purchase Task; CPT) is used to examine individual differences in motivation for tobacco under certain contexts. Smokers with psychopathology, relative to those without, may demonstrate stronger demand for tobacco following a period of smoking deprivation, which could account for disparate rates of smoking and cessation among this subgroup.
Method
Participants (n = 111) were community-recruited adult daily smokers who completed the CPT after a deprivation period of approximately 60 minutes. Presence of psychopathology was assessed via clinical interview; 40.5% (n = 45) of the sample met criteria for past-year psychological diagnosis. Specifically, 31.5% (n = 35) had an emotional disorder (anxiety/depressive disorder), 17.1% (n = 19) had a substance use disorder, and 19.1% of the sample had more than one disorder.
Results
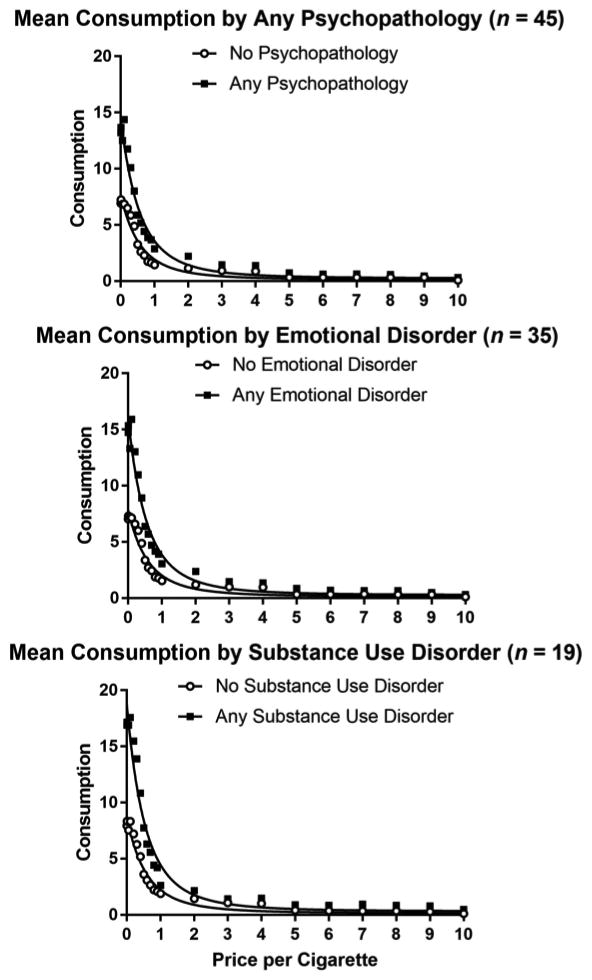
Smokers with any psychopathology showed significantly higher intensity (demand at unrestricted cost; $0) and Omax (peak expenditure for a drug) relative to smokers with no psychopathology. Intensity was significantly higher among smokers with an emotional disorder compared to those without. Smokers with a substance use disorder showed significantly higher intensity and Omax, and lower elasticity, reflecting greater insensitivity to price increases. Having ≥ 2 disorders was associated with higher intensity relative to having 1 or no disorders.
Discussion
Findings suggest that presence of psychopathology may be associated with greater and more persistent motivation to smoke. Future work is needed to explore the mechanism linking psychopathology to tobacco demand.
Keywords: cigarette purchase task, behavioral economics, psychopathology, tobacco, relative value, comorbidity
1. Introduction
Although population-based smoking rates have declined over the past several decades (US Department of Health and Human Services [USDHHS], 2014), cigarette use remains high among those with psychopathology relative to those without (34.3% vs. 16.7%; Centers for Disease Control and Prevention [CDCP], 2013; Morris et al., 2014). It is estimated that 30.9% of all cigarettes smoked by adults between 2009 and 2011 were by individuals with a history of a psychiatric disorder (CDCP, 2013). Smokers with a history of psychopathology are also significantly less likely to quit smoking successfully relative to those with no such history (34.7% vs. 53.4% quit rate; CDCP, 2013). Various psychiatric disorders are linked to poor smoking cessation outcomes, including depressive disorders (Hitsman et al., 2003; Zvolensky et al., 2015), schizophrenia (Lasser et al., 2000), anxiety disorders (Piper et al., 2010, 2011), posttraumatic stress disorder (Beckham et al., 2013; Zvolensky et al., 2008), and co-morbid substance use problems (Goodwin et al., 2014; Humfleet et al., 1999). Additionally, the prevalence of several anxiety disorders and dysthymia among current smokers appears to have increased over the past decade (Goodwin et al., 2014). Therefore, understanding smoking maintenance factors among individuals with psychopathology is a pressing public health priority (Aubin et al., 2012).
Behavioral economic theories and principles provide a useful framework for examining the appeal of a given substance, or the relative value, despite negative consequences of use (Bickel et al., 2014). The relative reinforcing value of, or demand for, a given drug has been assessed via self-reported hypothetical purchase tasks wherein participants indicate how much of a drug they would purchase at a range of prices (MacKillop et al., 2008; Murphy and MacKillop, 2006). These tasks yield data indicating the strength of motivation to obtain the drug, and can provide meaningful information about individual differences in motivational salience for drugs (i.e., the extent to which an individual values a drug under certain contexts). Five key behavioral economic indices of substance demand can be obtained from assessment of purchase task performance: intensity (amount of drug consumed at zero cost), Pmax (price at maximum expenditure for a drug), Omax (peak expenditure for a drug), breakpoint (cost whereby drug consumption is suppressed to zero), and elasticity of demand (the degree to which consumption decreases with increasing price). Purchase tasks have been used successfully to assess demand for several substances including tobacco (Acker and MacKillop, 2013; MacKillop, Brown, et al., 2012; MacKillop et al., 2008; MacKillop, Few, et al., 2012; MacKillop and Tidey, 2011), alcohol (Amlung et al., 2012; Mackillop et al., 2014; MacKillop et al., 2010; MacKillop and Murphy, 2007; Murphy et al., 2013; Murphy and MacKillop, 2006), and marijuana (Aston et al., 2015; Collins et al., 2014; Metrik et al., 2016). Data generally indicate that purchase behavior reflects an inverted U-shaped curve, such that expenditures for hypothetical substances are low when price value is low, increased with moderate prices, and is suppressed at high prices (Hursh and Silberberg, 2008; Jacobs and Bickel, 1999; Murphy et al., 2011). Specific to the cigarette purchase task, tobacco demand indices generally tend to be associated with indicators of nicotine dependence and smoking rate (MacKillop et al., 2008; Murphy et al., 2011) and are sensitive to nicotine deprivation and cue-induced craving (MacKillop et al., 2012), and certain demand indices are associated with lower motivation for smoking cessation (Murphy et al., 2011).
Limited work to date has examined tobacco demand as a function of psychopathology. Theoretically, smokers with emotional disorders (e.g., anxiety and mood disorders, posttraumatic stress disorder), which are largely characterized by high levels of negative affect, dysregulated mood states, and avoidance, may expect a reduction in distress states following consumption of cigarettes (McCarthy et al., 2010). Negative reinforcement smoking may, in turn, increase demand for tobacco for these individuals. For example, one study found that among trauma-exposed heavy drinkers, more severe posttraumatic stress symptoms were associated with demand intensity, greater peak expenditure for alcohol, (Omax), and lower sensitivity to increasing price of alcohol (elasticity; Murphy et al., 2013). Moreover, intensity and elasticity of alcohol demand explained, in part, the link between posttraumatic stress symptoms and consequences related to drinking (Tripp et al., 2015). Laboratory-based studies have also found that regular drinkers respond with greater alcohol demand (intensity, Omax, Pmax) following acute stress induction (Amlung and MacKillop, 2013), a finding also observed among heavy drinkers (Owens et al., 2015).
It is also possible that smokers with comorbid substance use disorders, relative to those without, may demonstrate stronger and more persistent motivation to consume cigarettes. One study of heavy drinking college students found cigarette smokers, relative to non-smokers, reported greater intensity, Omax, Pmax, and lower sensitivity to increasing price of alcohol (Yurasek et al., 2013). Impulsivity, a dispositional individual difference factor associated with behavioral externalizing behavior and disorders, has also been associated with greater alcohol demand among college student drinkers (Amlung et al., 2013) and cigarette smokers who also reported past-year alcohol use (Gray and MacKillop, 2013).
The bulk of the existing data to date on psychopathology and substance demand has been specific to alcohol, as reviewed above (e.g., Murphy et al., 2013; Tripp et al., 2015). We are aware of only one existing published study of psychopathology and tobacco demand, which found that smokers with schizophrenia, relative to healthy controls, had higher intensity of demand (MacKillop and Tidey, 2011). This work has not yet been extended to broader forms of psychopathology which is important given (a) heterogeneity in psychopathology and (b) differences in smoking lapse behavior across different disorder groups (e.g., anxiety versus substance use disorders; Piper et al., 2010). Additionally, given that comorbid psychopathology is associated with poorer smoking cessation outcomes (Cougle et al., 2010; Piper et al., 2010), it is important to understand how tobacco demand may differ as a function of number of diagnoses.
Thus, the current study examined the association between various forms of psychopathology and situational tobacco demand in a sample of community-recruited daily smokers. We examined the effect of having any past-year, relative to not, in terms of tobacco demand, as indexed via performance on a state-version of the Cigarette Purchase Task (CPT; MacKillop et al., 2008) following approximately 60 minutes of smoking deprivation. This assessment window allowed for the onset of tobacco craving, which can occur within 30 minutes of not smoking (Hendricks et al., 2006). Additionally, we tested the unique patterning of effects of having an emotional disorder (anxiety/depressive disorder), comorbid (non-tobacco) substance use disorder, and the number of psychological diagnoses in terms of CPT performance. It was hypothesized that smokers with any psychopathology, relative to none, would demonstrate greater tobacco demand following deprivation, and that these differences would be present in smokers with emotional disorders and those with substance use disorders. It was also hypothesized that smokers with more disorders (having two or more diagnoses) would demonstrate greater tobacco demand relative to individuals with one or no diagnosis.
2. Material and methods
2.1 Participants
Non-treatment seeking adult daily smokers were recruited for an experimental study on anxiety and smoking behavior (Farris and Zvolensky, 2016). Community-recruited individuals who were between 18-65 years of age, reported smoking 10 or more cigarettes per day for at least one year, and smoked within the first 30 minutes of waking in the morning, were invited for a baseline assessment to determine eligibility for the experimental study (described in Farris and Zvolensky, 2016). Participants were excluded from participation during an initial telephone screen if they reported heavy/frequent drinking (≥ 9 standard drinks/week), illicit drug use (≥ 3 days/week), unstable medical conditions, or current psychotic symptoms. The current study is a secondary analysis of data from participants who completed the baseline assessment including the CPT (n = 126), regardless of whether or not they were deemed eligible for the experimental phase of the study. Several cases (n = 11) showed evidence of inconsistent responding across prices (i.e., had ≥3 reversals), and 4 cases exhibited constant demand, suggesting low effort during this task; these cases were excluded from subsequent analysis.
Participants (n = 111; Mage = 43.8; SD = 9.8; 55.8% male) identified race as Black/African-American (59.5%), white (33.3%), American Indian/Alaska Native (1.8%), Asian (1.0%), or other (4.5%), and 5.4% of participants identified ethnicity as Hispanic. Approximately half of the sample completed at least some college (57.5%). Participants were single (47.7%), divorced/separated (35.1%), married/co-habituating (12.6%), and widowed (4.5%). Employment status was reported as unemployed (38.7%), employed full time (24.3%), employed part time (23.3%), student (3.6%), disabled (7.2%), retired (1.8%), and homemaker (0.9%). Of those who reported income (n = 46), 63.0% of participants reported annual household income < $25,000.
2.2 Measures
The Financial Strain Questionnaire (FSQ; Pearlin et al., 1981), which was adapted from an economic strain measure, was used as a proxy for income due to missing data on annual household income for 58.6% of the sample. The FSQ, is an 8-item self-reported measure that assesses perceived difficulty affording clothes, leisure activities, car, furniture, and other necessities (i.e., medical care, housing). Items that are rated on a scale from 1 to 3 (e.g., “I have enough money”, “I have somewhat enough money”, “I don’t have enough money”). Monetary status at the end of the month is also assessed using a similar scaling (1 = some money left over, 3 = no money left over). Items are summed to derive a total financial strain index, with higher scores indicating greater strain.
The Smoking History Questionnaire (SHQ; Brown et al., 2002), a 30-item self-report measure, was used to gather information about smoking history in order to establish pattern of cigarette use per eligibility criteria (e.g., daily use). A Carbon Monoxide (CO) Analysis, using the Vitalograph Breath Co carbon monoxide monitor, was conducted to measure the amount of CO (in parts per million [ppm]) in an expired breath sample. The Timeline Follow-Back Interview (TLFB; Sobell and Sobell, 1992) is a calendar-based assessment of substance use, which was used to document frequency, quantity, and patterns of tobacco, alcohol, and illicit drug use in the past 30 days. The Fagerström Test for Nicotine Dependence (FTND; Heatherton et al., 1991), a 6-item scale that assesses gradations in tobacco dependence, was used to assess the level of physiological dependence on tobacco (range 0-10, with higher scores reflecting higher levels of dependence). The FTND has adequate internal consistency, positive relations with key smoking variables (e.g., saliva cotinine), and high test-retest reliability (Heatherton et al., 1991; Pomerleau et al., 1994). Internal consistency of FTND items was low in the current sample (α = .42), likely based on low item count.
The Structured Clinical Interview for DSM-IV Disorders-Non-Patient Version (SCID-I/NP; First et al., 2007), a clinician-administered semi-structured diagnostic assessment, was used to assess the presence of past-year psychopathology based on the DSM-IV-TR diagnostic guidelines. Diagnostic assessments were conducted by highly-trained post-baccalaureate research assistants. In the current study, all diagnostic assessments were audio-recorded and 100% of cases were supervised by the first author for diagnostic accuracy. A random 20% of recordings were subjected to blinded inter-rater reliability review by a doctoral-level clinical psychology graduate student. No cases of diagnostic disagreement were noted. Of note, despite telephone screening for frequent substance use, many participants met criteria for current (past-year) substance use disorder. See results section for details.
The Cigarette Purchase Task (CPT; MacKillop et al., 2008) was used to assess the relative value of tobacco. The CPT is based on progressive-ratio operant schedules wherein participants self-report their cigarette consumption under various levels of price, which has been validated in several studies (e.g., Mackillop et al., 2008; Murphy et al., 2011). A state version of the CPT (Hitsman et al., 2008) was used in the current study. Participants were provided with the following task instructions: “Imagine that you could smoke RIGHT NOW. The following questions ask how many cigarettes you would consume if they cost various amounts of money. Assume the available cigarettes are your favorite brand. Assume that you have the same income/savings that you have now and NO ACCESS to any cigarettes or nicotine products other than those offered at these prices. In addition, assume that you would consume cigarettes that you request at this time. You cannot save or stockpile cigarettes for a later date. Be sure to consider each price increment carefully.” The CPT was completed approximately 60 minutes post-smoking, and was administered on the computer where each of the 22 questions/prices were presented one at a time, and read: “How many cigarettes would you smoke RIGHT NOW if they were: Free [$0/pack], 1¢ each [20¢/pack], 5¢ each [$1/pack], 10¢ each [$2/pack], 20¢ each [$4/pack], 30¢ each [$6/pack], 40¢ each [$8/pack], 50¢ each [$10/pack], 60¢ each [$12/pack], 70¢ each [$14/pack], 80¢ each [$16/pack], 90¢ each [$18/pack], $1 each [$20/pack], $2 each [$40/pack], $3 each [$60/pack], $4 each [$80/pack], $5 each [$100/pack], $6 each [$120/pack], $7 each [$140/pack], $8 each [$160/pack], $9 each [$180/pack], $10 each [$200/pack] ?”
2.3 Procedure
Participants completed an initial telephone assessment to determine potential eligibility. Potentially eligible individuals were scheduled for an in-person appointment and instructed to bring their usual brand of cigarettes to the appointment. All participants provided written, informed consent prior to initiation of any study procedures, and this study protocol was approved by the Institutional Review Board where the data were collected. Upon arrival, participants completed a diagnostic assessment (per the SCID-I/NP), smoking history measures, and provided a carbon monoxide sample of expired breath to verify smoking status. At a standardized point during the baseline assessment, participants were told they could have a ‘smoke break’. The experimenter accompanied the participant outdoors, alongside the laboratory, and informed the participant that he/she had the opportunity to smoke one cigarette (all participants smoked). The participants were told to smoke as usual, and were given as much time as desired. Next, the participants returned inside the laboratory and completed approximately 60 minutes of computerized self-report assessments, which were broken up by two scheduled snack/water breaks (no smoking or caffeine was permitted). The CPT was the last measure completed during the assessment period. All participants were compensated $25 for completing the baseline assessment.
2.4 Data Analytic Procedures
Calculations of demand indices were obtained using the following methods. Price elasticity values were generated by fitting individual curves in GraphPad Prism using the Koffarnus exponentiated demand equation (Koffarnus et al., 2015), Q = Q0 × 10k(e-aQ0C-1), where Q = quantity consumed, Q0 = derived intensity, k = a constant across individuals that denotes the range of the dependent variable (tobacco cigarettes), C = the cost of the commodity, and α = elasticity or the rate constant determining the rate of decline in consumption based on increases in price (i.e., essential value). This is a modification to the Hursh and Silberberg (2008) exponential demand equation that does not require eliminating or substituting for consumption values of zero. The appropriate k value was determined by subtracting the log10-transformed average consumption at the highest price ($10.00) from the log10-transformed average consumption at the lowest price used in curve fitting ($0.01). The k value used in analyses was 1.757. An R2 value was generated to reflect percentage of variance accounted for by the demand equation (i.e., the adequacy of the fit of the model to the data).
Raw CPT data were examined for outliers using standard scores, with a criterion of Z = 3.29 to retain maximum data. A small number of outliers were detected (1.3%). The outliers were determined to be legitimate high-magnitude values and were recoded as one unit higher than the next lowest non-outlying value (Tabachnick and Fidell, 2000). Five metrics of tobacco demand were obtained from the CPT: (a) intensity of demand (i.e., the amount of drug consumed at zero cost), (b) Omax (i.e., peak expenditure for a drug), (c) Pmax (i.e., price at maximum expenditure), (d) breakpoint (i.e., cost at which consumption is suppressed to zero), and (e) elasticity of demand (i.e., the sensitivity of tobacco consumption to increases in cost). Observed values for intensity, Omax, Pmax, and breakpoint were estimated by directly examining CPT performance. Elasticity of demand was empirically derived using values generated from a modified exponential demand equation (Koffarnus et al., 2015). Next, all data were examined for distribution normality using histograms. All tobacco demand variables were non-normally distributed. A square root transformation was used for intensity, log10 transformation was used for Omax, and cube root transformation was used for Pmax, breakpoint, and elasticity of demand; all transformations improved the distribution substantially.
The sample was split according to the presence or absence of any psychopathology, emotional disorders, and substance use disorders and examined in terms mean differences in each of the five smoking demand indices. A trichotomously coded variable (0 = no disorder, 1 = presence of one disorder, 2 = presence of two or more disorders) was utilized to examine differences in demand indices by presence of comorbid disorders. Analysis of covariance (ANCOVA) was utilized to examine group differences after adjusting for participant gender, age, race (white/non-white), and financial strain.
3. Results
3.1 Sample Characteristics
The sample averaged smoking 16.8 (SD = 8.61) cigarettes per day, initiated smoking at age 16.0 (SD = 6.5) years, and smoked for an average of 23.6 years (SD = 11.1). Moderate levels of tobacco dependence were reported per the FTND (M = 4.7; SD = 1.5), 55.0% of participants reported smoking their first cigarette of the day within 5 minutes of waking, and average expired CO levels at baseline were 23.3 ppm (SD = 11.6). Slightly more than half of the sample reported smoking menthol cigarettes (59.5%).
Regarding past-year (12-month) psychopathology, 40.5% (n = 45) of the sample To. Approximately one-third of the sample had past-year emotional disorder (31.5%) and 17.1% met criteria for a substance use disorder. Of those with a diagnosis, 48.9% had more than one diagnosis (range 1-4). See Table 1. Smokers with any past-year psychopathology, relative to those without, did not significantly differ in terms of age, gender, race, average number of cigarettes per day, level of tobacco dependence, smoking within 5 minutes of waking, use of menthol cigarettes, or perceived health. Financial strain was significantly higher among smokers with psychopathology (M = 18.4, SD = 4.9) relative to those without psychopathology (M = 16.1, SD = 5.1; t[109] = -2.43, p = .017).
Table 1. Psychopathology in sample.
| Past-Year (12-Month) Diagnosis | Full Sample (n = 111) | With Diagnosis (n = 45) |
|---|---|---|
| Emotional Disorder | 31.5% | 77.8% |
| Major depressive disorder, single episode | 2.7% | 6.7% |
| Major depressive disorder, recurrent | 6.3% | 15.6% |
| Bipolar Disorder I | 1.8% | 4.4% |
| Bipolar Disorder II | 1.8% | 4.4% |
| Dysthymic Disorder | 4.5% | 11.1% |
| Panic Disorder w/ Agoraphobia | 2.7% | 6.7% |
| Panic Disorder w/o Agoraphobia | 1.8% | 4.4% |
| Social anxiety disorder | 6.3% | 15.6% |
| Specific phobia | 8.1% | 20.0% |
| Obsessive-compulsive disorder | 0.9% | 2.2% |
| Posttraumatic stress disorder | 11.7% | 28.9% |
| Generalized anxiety disorder | 1.8% | 4.4% |
| Substance Use Disorder | 17.1% | 42.2% |
| Alcohol Abuse | 0.9% | 2.2% |
| Alcohol Dependence | 5.4% | 13.3% |
| Cannabis Abuse | 1.8% | 4.4% |
| Cannabis Dependence | 1.8% | 4.4% |
| Cocaine Abuse | 0.9% | 2.2% |
| Cocaine Dependence | 1.8% | 4.4% |
| Opioid Abuse | 0.9% | 2.2% |
| Opioid Dependence | 3.6% | 8.9% |
| Sedative, Hypnotic, Anxiolytic Dependence | 0.9% | 2.2% |
| Other Substance Dependence | 0.9% | 2.2% |
| Other Disorder | 4.5% | 11.1% |
| Psychotic Disorder NOS | 1.8% | 4.4% |
| Bulimia Nervosa | 0.9% | 2.2% |
| Eating Disorder NOS | 1.8% | 4.4% |
Note: NOS = Not otherwise specified
3.2 Tobacco Demand Results
3.2.1 Overview
As expected, cigarette consumption decreased as a function of increasing price. Figure 2 depicts the expenditure associated with each price. The modified exponential demand equation (Koffarnus et al., 2015) provided an excellent fit to the overall demand data (R2 = .969) and a good fit to the individual data (median R2 = .851, interquartile range = .763 - .905). The untransformed indices of tobacco demand for the total sample are presented in Table 2 in addition to the inter-correlations between demand indices and other sample characteristics. None of the demand indices were significantly associated with age, gender, race (white/non-white), financial strain, or perceived health. Tobacco dependence per the FTND and average cigarettes per day were significantly correlated with intensity and Omax. Of note, while not displayed in Table 2, use of menthol cigarettes relative to non-menthol, was not associated with any difference in demand indices (consistent with O’Connor et al., 2012).
Table 2. Correlations among demand indices and sample characteristics.
| Variable | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. Intensity | -- | .65** | .17 | .31** | -.34** | -.05 | .03 | .08 | .10 | .39** |
| 2. Omax | .68** | .73** | -.70** | -.01 | -.08 | .14 | .04 | .21* | ||
| 3. Pmax | .84** | -.47** | -.07 | -.12 | .04 | -.08 | -.05 | |||
| 4. Breakpoint | -.57** | -.18 | -.03 | .08 | .06 | .02 | ||||
| 5. Elasticity | .01 | .14 | -.20* | .02 | -.07 | |||||
| 6. Age | -.21* | -.01 | -.10 | -.04 | ||||||
| 7. Gender (female) | -.10 | .25** | -.01 | |||||||
| 8. Race (non-white) | -.05 | -.13 | ||||||||
| 9. Financial Strain | .13 | |||||||||
| 10. FTND | ||||||||||
| Mean | 9.47 | 7.98 | 1.75 | 2.42 | 0.41 | 43.83 | n=49 | n=74 | 17.06 | 4.73 |
| SD / SEMa | 1.17 | 1.60 | 0.25 | 0.28 | 0.11 | 9.84 | 44.1% | 66.7% | 5.05 | 1.48 |
Note: Gender (coded 0=male, 1=female); Race (coded 0=white; 1=non-white); Financial Strain (Financial Strain Questionnaire); Perceived Health per the Short Form Health Survey-12 (SH-12); FTND (Fagerström Test for Nicotine Dependence)
SEM is presented for demand indices, SD is presented for all other descriptive variables
p < .05,
p < .01,
p < .001
3.2.2. Psychological Diagnoses
See Table 3 for the adjusted means, standard error of measurement and significance tests reflecting group differences in demand indices by psychopathology status. Smokers with any psychopathology, relative to those without, purchased more cigarettes at zero cost (higher intensity of demand) and displayed higher peak expenditure for cigarettes (Omax). Similarly, smokers with an emotional disorder specifically, relative to those without, displayed significantly higher intensity of demand. Among smokers with an alcohol/substance use disorder, CPT performance showed significantly higher intensity of demand, higher peak expenditure for cigarettes (Omax), and more inelastic demand (insensitivity to price increase), relative to smokers without a substance use disorder. See Figure 1 for depiction of demand curves by psychopathology status.
Table 3. Demand indices by presence of psychopathology.
| Any Psychopathology | Emotional Disorder | Substance Use Disorder | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | Yes | No | Yes | No | Yes | |||||||||||||
| (n = 66) | (n = 45) | (n = 76) | (n = 35) | (n = 92) | (n = 19) | |||||||||||||
| Metric | Mean | SEM | Mean | SEM | F | p | Mean | SEM | Mean | SEM | F | p | Mean | SEM | Mean | SEM | F | p |
| Intensity | 7.25 | 1.39 | 12.72 | 1.70 | 6.62 | .012 | 7.50 | 1.30 | 13.75 | 1.94 | 5.81 | .018 | 8.09 | 1.16 | 16.17 | 2.62 | 9.78 | .002 |
| Omax | 5.79 | 2.08 | 11.18 | 2.54 | 4.08 | .036 | 6.52 | 1.95 | 11.14 | 2.92 | 1.55 | .216 | 7.31 | 1.77 | 11.18 | 3.97 | 3.97 | .049 |
| Pmax | 1.50 | 0.33 | 2.19 | 0.40 | 0.99 | .332 | 1.78 | 0.31 | 1.69 | 0.46 | 0.05 | .832 | 1.55 | 0.27 | 2.75 | 0.61 | 2.06 | .155 |
| Breakpoint | 2.34 | 0.37 | 2.56 | 0.45 | 0.37 | .543 | 2.40 | 0.35 | 2.50 | 0.52 | 0.05 | .824 | 2.37 | 0.31 | 2.72 | 0.70 | 0.57 | .453 |
| Elasticity | 0.42 | 0.14 | 0.42 | 0.17 | 0.70 | .403 | 0.48 | 1.28 | 0.42 | 1.13 | 1.09 | .300 | 0.48 | 0.12 | 0.12 | 0.27 | 4.05 | .047 |
Note: Mean/SEM are non-transformed values; Means are adjusted for covariates (Gender, age, race, FTND, Economic strain).
Figure 1. Hypothetical consumption by psychopathology status.
3.2.3. Psychiatric Comorbidity
Tobacco demand was examined as a function of psychiatric comorbidity: no diagnosis (n = 66), 1 diagnosis (n = 23), ≥ 2 diagnoses (n = 22). See Table 4 for CPT metrics stratified by number of diagnoses. The ANCOVA results indicated group differences in terms of intensity of demand. Post-hoc comparisons indicated that smokers with ≥ 2 diagnoses purchased significantly more cigarettes at zero cost relative to smokers with no diagnoses or 1 diagnosis (p = .022). There were no other significant differences in demand indices across the groups.
Table 4. Demand indices by number of diagnoses.
| Number of Diagnoses | ||||||||
|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2+ | ||||||
| (n = 66) | (n = 23) | (n = 22) | ||||||
| Metric | Mean | SEM | Mean | SEM | Mean | SEM | F | p |
| Intensity | 7.15 | 1.39 | 10.70 | 2.38 | 15.13 | 2.61 | 4.46 | .014 |
| Omax | 5.78 | 2.09 | 10.96 | 3.57 | 11.45 | 3.92 | 2.07 | .132 |
| Pmax | 1.52 | 0.33 | 2.48 | 0.56 | 1.69 | 0.61 | 0.80 | .451 |
| Breakpoint | 2.35 | 0.37 | 2.82 | 0.64 | 2.26 | 0.70 | 0.33 | .720 |
| Elasticity | 0.42 | 0.14 | 0.51 | 0.25 | 0.31 | 0.27 | 0.47 | .627 |
Note: Mean and SEM are non-transformed values; Means are adjusted for covariates (Gender, age, race, FTND, Economic strain)
4. Discussion
Assessment of tobacco demand provides insight into the motivation for tobacco use under certain contexts. In the current sample of non-treatment seeking community smokers, individuals with any past-year psychopathology, relative to those without, demonstrated significantly higher intensity and Omax, following approximately a 60-minute period of smoking deprivation. Specifically, smokers with psychopathology, versus those without, reported they would smoke almost twice as many cigarettes when they were free ($0; M = 12.7 versus M = 7.3 cigarettes). Smokers with past-year psychopathology were also willing to spend a significantly higher amount on cigarettes ($11.18) after approximately 60 minutes of smoking deprivation relative to smokers with no past-year psychiatric history ($5.79). These data suggest that psychological symptoms and/or disorders are related to a higher demand for tobacco. The current pattern of results and magnitude of effects are broadly consistent with a prior study of general tobacco demand among smokers with schizophrenia relative to healthy controls (MacKillop and Tidey, 2011). Collectively, psychopathology appears to most consistently relate to amplitude of demand (i.e., how many cigarettes an individual would consume and how much would be spent; MacKillop et al., 2009) in the context of acute craving. In contrast, tobacco demand over the course of escalating price (i.e., persistence of demand) does not appear to be influenced by general psychopathology (non-disorder specific). That is, smokers with psychopathology (a) demonstrate volumetric differences in demand, which may demarcate heavy use, especially in response to deprivation/craving, and (b) do not differ in terms of sensitivity to price of cigarettes, which tends to represent likelihood of changing patterns of drug use (e.g., MacKillop and Murphy, 2007). It is worth noting that, like other studies, tobacco dependence (per the FTND) was significantly associated with tobacco demand indices (MacKillop et al., 2008; Murphy et al., 2011), in particular indices that reflect volumetric consumption (e.g., intensity, Omax).
Smoking intensity was significantly higher among those with an emotional disorder (anxiety, depressive) compared to those without an emotional disorder (M = 13.8 versus M = 7.5 cigarettes purchased). These results complement existing data from the alcohol demand literature, which has found that posttraumatic stress symptoms and laboratory-induced stress are associated with greater trait alcohol demand (Amlung and MacKillop, 2013; Murphy et al., 2013; Owens et al., 2015; Tripp et al., 2015). The magnitude of our observed effects in tobacco demand intensity observed in this study is larger than mean values reported in changes in alcohol demand following laboratory-induced stress (Amlung and MacKillop, 2013). These findings uniquely indicate that in the context of rising craving/smoking deprivation, smokers with emotional disorders (relative to those without) appear to view tobacco as particularly incentivizing.
Additionally, unique differences in tobacco demand indices emerged among smokers with substance use disorders. Here, smokers with a comorbid substance use disorder (relative to those without) had significantly higher intensity of demand when cost was unrestricted (M = 16.2 versus M = 8.1 cigarettes purchased) and higher Omax, which corresponded to an average peak expenditure of $11.18 versus $7.31 for cigarettes. The magnitude of these effects is larger than previously reported differences in alcohol demand among those with and without comorbid tobacco use (Yurasek et al., 2013) and impulsivity’s effect on alcohol demand (Amlung et al., 2013; Grey and MacKillop, 2014), even after adjusting for relative factors including tobacco dependence. Moreover, smokers with comorbid substance use disorders also had significantly lower elasticity, reflecting greater insensitivity to price increases. It is worth noting that inelastic tobacco demand was unique to smokers with substance use disorder, but not emotional disorders. Accordingly, smokers with substance use disorders may be at high risk for persistent tobacco demand during smoking deprivation, which could contribute to poorer smoking cessation outcomes (Rohsenow et al., 2015). This unique set of findings warrants replication and further examination, however preliminarily suggests that there may be unique motivational processes underlying persistent smoking that distinguish between externalizing (substance use) and internalizing (emotional) disorders.
Finally, the number of comorbid disorders appears to be related to the intensity of tobacco demand. Specifically, smokers with ≥ 2 diagnoses demonstrated the highest tobacco demand when price was unrestricted (M = 15.1 cigarettes purchased), relative to smokers with only 1 diagnosis (M = 10.7 cigarettes) and those with no diagnosis (M = 7.2 cigarettes). Thus, the motivation for tobacco during smoking deprivation appears to be higher among smokers with comorbid disorders, relative to those without, which may in part contribute to poor smoking cessation outcomes in this subgroup of smokers (Piper et al., 2010).
It is worth noting that the patterning of observed effects by psychopathology status remained significant after adjusting for common demographic factors (age, gender, race), economic strain, and level of tobacco dependence. Thus, psychopathology appears to be incrementally related to tobacco demand. Explicit reasons for higher demand among smokers with psychopathology were not tested here, although there are several potential explanations which may or may not be unique to specific forms of psychopathology. For example, smokers with psychopathology may rely on nicotine for stress dampening properties (whether perceived or actual; Kassel et al., 2003). Environmental factors, including stressful/unstable living conditions, or lack of access to cessation treatments (e.g., Fagerström and Aubin, 2009; Schroeder and Morris, 2010), or neurobiological factors (e.g., antipsychotic-like and dopamine-releasing effects; Dome et al., 2010) could also account for, or contribute to, elevated tobacco demand. Among smokers with emotional disorders, some of the most consistent evidence indicates that cognitive-affective vulnerabilities related to negative-reinforcement (e.g., sensitivity to and intolerance of psychological/ physiological distress states) and positive-reinforcement (e.g., anhedonia) underlie the link between emotional disorders and smoking (Leventhal and Zvolensky, 2015). Elevated demand for tobacco among smokers with comorbid alcohol/substance use disorders may be potentially related to cross-tolerance or enhanced drug effects (Clark et al., 2001; Kouri et al., 2004), or psychological vulnerability factors associated with behavioral disinhibition (e.g., greater impulsivity, sensation-seeking; Amlung et al., 2014; Gray and MacKillop, 2013) especially in the context of increasing craving. Low tolerance of nicotine withdrawal symptoms among smokers with comorbid substance use disorders is linked to poorer smoking cessation outcomes (Rohsenow et al., 2015), and may also maintain high tobacco demand through negative-reinforcement motivational processes (i.e., avoidance of withdrawal distress regardless of increasing cigarette cost). These and other mechanisms that may explain higher motivation for tobacco use among psychologically-vulnerable smokers should be explored in future investigations.
There are several study limitations that are important to address. First, the study is cross-sectional in nature, thus inferences about causal associations between psychopathology and situational tobacco demand cannot be made. Second, past (lifetime) psychopathology that was successfully treated or remitted was not included in the categorization of past-year psychopathology. It is also possible that by assessing psychopathology in the past-year, some smokers may have remitted or partially-remitted disorders (i.e., that are not present in the past-month). Naturally remitting psychopathology or lifetime psychopathology (versus current) might differentially affect aspects of smoking and cessation likelihood (Piper et al., 2010). Third, the presence of comorbid substance use disorders was low in the current sample, based on the exclusion of individuals who self-reported frequent drinking (≥ 9 standard drinks/week) and/or illicit drug use (≥ 3 days/week) during an initial telephone pre-screening. Additionally, callers who reported active psychotic symptoms during the telephone screening were also excluded, thus the presence of psychotic-spectrum psychopathology among the sample of smokers who completed the in-person assessment was low, as designed (n = 2; 1.8%) Thus, it is important to consider the extent to which these findings generalize to all forms of psychopathology, including serious mental illness. Fourth, the sample size did not permit examination of the associations between tobacco demand and specific forms of psychopathology, which may limit the specificity of the current findings based on the heterogeneity of psychological disorders. Fifth, while menthol cigarette use was not associated with CPT performance, a large percentage of the sample reported use of mentholated cigarettes (59.5%), which may not be representative of the general population of smokers (8.2%; SAMHSA, 2011). Sixth, with respect to the CPT, the instructions used in the current investigation prompted the participants to assume that the cigarettes for purchase were their “favorite brand.” However, this brand may vary from what they typically smoke, due to availability/price. Thus, if individuals believed that the available cigarettes to purchase during the CPT were of higher quality than their typical brand, this could have resulted in increased tobacco demand, as has been shown with marijuana (e.g., Collins et al., 2016). Seventh, baseline (trait) CPT performance was not assessed in the current investigation. Thus, although we assessed state tobacco demand following acute deprivation (60 minutes post-smoking), we are unable to make conclusions about situational factors that exacerbate tobacco demand. Finally, a typical pattern of responding on the CPT is evidenced by decreasing purchase of cigarettes as cost increases. Therefore, we excluded data from cases where participants displayed ≥ 3 reversals (n = 11), potentially reflecting invalid responding. Reversals may have occurred from misunderstanding directions or limited cognitive ability (e.g., MacKillop and Tidey, 2011), or could have been an artifact of how the CPT items were administered -- items were presented one at a time on a screen rather than all at once, thus upcoming prices were unknown.
The current study offers novel information about differences in tobacco demand among smokers with and without psychopathology. Based on elevated volumetric demand in smokers with psychopathology, this subgroup of smokers may require more intensive and multi-faceted smoking cessation treatment to adequately address high motivation for tobacco, even after only a short period of deprivation. This may be particularly important for smokers with multiple psychiatric diagnoses and smokers with substance use disorders. More work is needed to understand aspects of tobacco demand across various forms of specific forms of psychopathology.
Acknowledgments
Author Disclosures: This work was funded by a pre-doctoral National Research Service Award from the National Institute of Drug Abuse (F31-DA035564) awarded to the first author. The research described in this paper was also supported in part by a grant to the first author from the American Psychological Association. The first author is currently supported by a training grant from the National Health, Lung, and Blood Institute (T32-HL076134-11). Data analysis and manuscript preparation was supported in part by a grant from the National Institute on Drug Abuse to the second author (K01-DA039311).
Footnotes
Contributors: Drs. Farris and Zvolensky developed the parent study, and Drs. Farris, Aston, and Metrik designed the current secondary investigation. Drs. Farris and Aston managed the literature searches and summaries of previous related work and completed statistical analyses. All authors contributed to and have approved the final manuscript.
Conflict of Interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Acker J, MacKillop J. Behavioral economic analysis of cue-elicited craving for tobacco: a virtual reality study. Nicotine Tob Res. 2013;15:1409–16. doi: 10.1093/ntr/nts341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlung M, Few LR, Howland J, Rohsenow DJ, Metrik J, MacKillop J. Impulsivity and alcohol demand in relation to combined alcohol and caffeine use. Exp Clin Psychopharmacol. 2013;21:467–74. doi: 10.1037/a0034214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlung M, MacKillop J. Understanding the effects of stress and alcohol cues on motivation for alcohol via behavioral economics. Alcohol Clin Exp Res. 2014;38:1780–9. doi: 10.1111/acer.12423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlung MT, Acker J, Stojek MK, Murphy JG, MacKillop J. Is talk “cheap”? An initial investigation of the equivalence of alcohol purchase task performance for hypothetical and actual rewards. Alcohol Clin Exp Res. 2012;36:716–24. doi: 10.1111/j.1530-0277.2011.01656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aston ER, Metrik J, MacKillop J. Further validation of a marijuana purchase task. Drug Alcohol Depend. 2015;152:32–38. doi: 10.1016/j.drugalcdep.2015.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aubin HJ, Rollema H, Svensson TH, Winterer G. Smoking, quitting, and psychiatric disease: A review. Neurosci Biobehav Rev. 2012;36:271–284. doi: 10.1016/j.neubiorev.2011.06.007. [DOI] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, Murphy JG. The behavioral economics of substance use disorders: reinforcement pathologies and their repair. Annu Rev Clin Psychol. 2014;10:641–77. doi: 10.1146/annurev-clinpsy-032813-153724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Lejuez CW, Kahler CW, Strong DR. Distress tolerance and duration of past smoking cessation attempts. J Abnorm Psychol. 2002;111:180–5. [PubMed] [Google Scholar]
- Center for Disease Control and Prevention. Vital signs: Current cigarette smoking among adults aged ≥18 years with mental illness — United States, 2009-2011. Morb Mortal Wkly Rep. 2013;62:77–80. [PMC free article] [PubMed] [Google Scholar]
- Clark A, Lindgren S, Brooks SP, Watson WP, Little HJ. Chronic infusion of nicotine can increase operant self-administration of alcohol. Neuropharmacology. 2001;41:108–17. doi: 10.1016/s0028-3908(01)00037-5. [DOI] [PubMed] [Google Scholar]
- Collins RL, Vincent PC, Yu J, Liu L, Epstein LH. A behavioral economic approach to assessing demand for marijuana. Exp Clin Psychopharmacol. 2014;22:211–21. doi: 10.1037/a0035318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins RL, Vincent PC, Earleywine M, Liu L, Yu J, de Leo J. Poster presented at Marijuana and Cannabinoids: A Neuroscience Research Summit. NIH Campus: Bethesda, MD; Mar, 2016. The effects of perceived quality on demand for marijuana: Policy implications of a web-based behavioral economic experiment with young-adult marijuana users. [Google Scholar]
- Dome P, Lazary J, Kalapos MP, Rihmer Z. Smoking, nicotine and neuropsychiatric disorders. Neurosci Biobehav Rev. 2010;34:295–342. doi: 10.1016/j.neubiorev.2009.07.013. [DOI] [PubMed] [Google Scholar]
- Fagerström K, Aubin HJ. Management of smoking cessation in patients with psychiatric disorders. Curr Med Res Opin. 2009;25:511–518. doi: 10.1185/03007990802707568. [DOI] [PubMed] [Google Scholar]
- Farris SG, Zvolensky MJ. An experimental test of the effect of acute anxious arousal and anxiety sensitivity on negative reinforcement smoking. J Psychopharmacol. 2016;30 doi: 10.1177/0269881116642880. [DOI] [PubMed] [Google Scholar]
- Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz N, Curry SJ. Clinical practice guidelines. U.S. Department of Health and Human Services, Public Health Service; Rockville, MD: 2008. Treating tobacco use and dependence: 2008 update. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, non-patient edition. Biometrics Research, New York State Psychiatric Institute; New York, NY: 2007. [Google Scholar]
- Goodwin RD, Sheffer CE, Chartrand H, Bhaskaran J, Hart CL, Sareen J, Bolton J. Drug use, abuse, and dependence and the persistence of nicotine dependence. Nicotine Tob Res. 2014;16:1606–1612. doi: 10.1093/ntr/ntu115. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Wall MM, Choo T, Galea S, Horowitz J, Nomura Y, Zvolensky MJ, Hasin DS. Changes in the prevalence of mood and anxiety disorders among male and female current smokers in the United States: 1990-2001. Ann Epidemiol. 2014;24:493–7. doi: 10.1016/j.annepidem.2014.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray JC, MacKillop J. Interrelationships among individual differences in alcohol demand, impulsivity, and alcohol misuse. Psychol Addict Behav. 2014;28:282–7. doi: 10.1037/a0032766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. Br J Addict. 1991;86:1119–27. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hendricks PS, Ditre JW, Drobes DJ, Brandon TH. The early time course of smoking withdrawal effects. Psychopharmacology (Berl) 2006;187:385–396. doi: 10.1007/s00213-006-0429-9. [DOI] [PubMed] [Google Scholar]
- Hitsman B, Borrelli B, McChargue DE, Spring B, Niaura R. History of depression and smoking cessation outcome: A meta-analysis. J Consult Clin Psychol. 2003;71:657–63. doi: 10.1037/0022-006x.71.4.657. [DOI] [PubMed] [Google Scholar]
- Hitsman B, MacKillop J, Lingford-Hughes A, Williams TM, Ahmad F, Adams S, Nutt DJ, Munafò MR. Effects of acute tyrosine/phenylalanine depletion on the selective processing of smoking-related cues and the relative value of cigarettes in smokers. Psychopharmacology (Berl) 2008;196:611–21. doi: 10.1007/s00213-007-0995-5. [DOI] [PubMed] [Google Scholar]
- Humfleet G, Muñoz R, Sees K, Reus V, Hall S. History of alcohol or drug problems, current use of alcohol or marijuana, and success in quitting smoking. Addict Behav. 1999;24:149–54. doi: 10.1016/s0306-4603(98)00057-4. [DOI] [PubMed] [Google Scholar]
- Hursh SR, Silberberg A. Economic demand and essential value. Psychol Rev. 2008;115:186–198. doi: 10.1037/0033-295X.115.1.186. [DOI] [PubMed] [Google Scholar]
- Jacobs EA, Bickel WK. Modeling drug consumption in the clinic using simulation procedures: Demand for heroin and cigarettes in opioid-dependent outpatients. Exp Clin Psychopharmacol. 1999;7:412–26. doi: 10.1037//1064-1297.7.4.412. [DOI] [PubMed] [Google Scholar]
- Kassel JD, Stroud LR, Paronis CA. Smoking, stress, and negative affect: correlation, causation, and context across stages of smoking. Psychol Bull. 2003;129:270–304. doi: 10.1037/0033-2909.129.2.270. [DOI] [PubMed] [Google Scholar]
- Koffarnus MN, Franck CT, Stein JS, Bickel WK. A modified exponential behavioral economic demand model to better describe consumption data. Exp Clin Psychopharmacol. 2015;23:504–12. doi: 10.1037/pha0000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kouri EM, McCarthy EM, Faust AH, Lukas SE. Pretreatment with transdermal nicotine enhances some of ethanol’s acute effects in men. Drug Alcohol Depend. 2004;75:55–65. doi: 10.1016/j.drugalcdep.2004.01.011. [DOI] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness: A population-based prevalence study. JAMA. 2000;284:2606–10. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Amlung MT, Acker J, Gray JC, Brown CL, Murphy JG, Ray LA, Sweet LH. The neuroeconomics of alcohol demand: an initial investigation of the neural correlates of alcohol cost-benefit decision making in heavy drinking men. Neuropsychopharmacology. 2014;39:1988–95. doi: 10.1038/npp.2014.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Amlung MT, Acker J, Stojek M. Further validation of an Alcohol Purchase Task: Equivalence of versions for hypothetical and actual rewards. Alcohol Clin Exp Res. 2010;34:48A–48A. doi: 10.1111/j.1530-0277.2011.01656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Brown CL, Stojek MK, Murphy CM, Sweet L, Niaura RS. Behavioral economic analysis of withdrawal- and cue-elicited craving for tobacco: An initial investigation. Nicotine Tob Res. 2012a;14:1426–34. doi: 10.1093/ntr/nts006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Few LR, Murphy JG, Wier LM, Acker J, Murphy C, Stojek M, Carrigan M, Chaloupka F. High-resolution behavioral economic analysis of cigarette demand to inform tax policy. Addiction. 2012b;107:2191–200. doi: 10.1111/j.1360-0443.2012.03991.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Murphy JG. A behavioral economic measure of demand for alcohol predicts brief intervention outcomes. Drug Alcohol Depend. 2007;89:227–33. doi: 10.1016/j.drugalcdep.2007.01.002. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Murphy JG, Ray LA, Eisenberg DTA, Lisman SA, Lum JK, Wilson DS. Further validation of a cigarette purchase task for assessing the relative reinforcing efficacy of nicotine in college smokers. Exp Clin Psychopharmacol. 2008;16:57–65. doi: 10.1037/1064-1297.16.1.57. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Murphy JG, Tidey JW, Kahler CW, Ray LA, Bickel WK. Latent structure of facets of alcohol reinforcement from a behavioral economic demand curve. Psychopharmacology (Berl) 2009;203:33–40. doi: 10.1007/s00213-008-1367-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Tidey JW. Cigarette demand and delayed reward discounting in nicotine-dependent individuals with schizophrenia and controls: An initial study. Psychopharmacology (Berl) 2011;216:91–9. doi: 10.1007/s00213-011-2185-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Aston ER, Kahler CW, Rohsenow DJ, McGeary JE, Knopik VS, MacKillop J. Cue-elicited increases in incentive salience for marijuana: Craving, demand, and attentional bias. Drug Alcohol Depend. 2016;167:82–8. doi: 10.1016/j.drugalcdep.2016.07.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, MacKillop J. Relative reinforcing efficacy of alcohol among college student drinkers. Exp Clin Psychopharmacol. 2006;14:219–227. doi: 10.1037/1064-1297.14.2.219. [DOI] [PubMed] [Google Scholar]
- Murphy JG, MacKillop J, Tidey JW, Brazil LA, Colby SM. Validity of a demand curve measure of nicotine reinforcement with adolescent smokers. Drug Alcohol Depend. 2011;113:207–14. doi: 10.1016/j.drugalcdep.2010.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Yurasek AM, Dennhardt AA, Skidmore JR, McDevitt-Murphy ME, MacKillop J, Martens MP. Symptoms of depression and PTSD are associated with elevated alcohol demand. Drug Alcohol Depend. 2013;127:129–36. doi: 10.1016/j.drugalcdep.2012.06.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Connor RJ, Bansal-Travers M, Carter LP, Cummings KM. What would menthol smokers do if menthol in cigarettes were banned? Behavioral intentions and simulated demand Addiction. 2012;107:1330–8. doi: 10.1111/j.1360-0443.2012.03822.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owens MM, Murphy CM, MacKillop J. Initial Development of a Brief Behavioral Economic Assessment of Alcohol Demand. Psychol Conscious. 2015;2:144–152. doi: 10.1037/cns0000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, Cook JW, Schlam TR, Jorenby DE, Baker TB. Anxiety diagnoses in smokers seeking cessation treatment: Relations with tobacco dependence, withdrawal, outcome and response to treatment. Addiction. 2011;106:418–427. doi: 10.1111/j.1360-0443.2010.03173.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, Smith SS, Schlam TR, Fleming MF, Bittrich AA, Brown JL, Leitzke CJ, Zehner ME, Fiore MC, Baker TB. Psychiatric disorders in smokers seeking treatment for tobacco dependence: Relations with tobacco dependence and cessation. J Consult Clin Psychol. 2010;78:13–23. doi: 10.1037/a0018065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomerleau CS, Tate JC, Lumley MA, Pomerleau OF. Gender differences in prospectively versus retrospectively assessed smoking withdrawal symptoms. J Subst Abuse. 1994;6:433–40. doi: 10.1016/s0899-3289(94)90376-x. [DOI] [PubMed] [Google Scholar]
- Rohsenow DJ, Tidey JW, Kahler CW, Martin RA, Colby SM, Sirota AD. Intolerance for withdrawal discomfort and motivation predict voucher-based smoking treatment outcomes for smokers with substance use disorders. Addict Behav. 2015;43:18–24. doi: 10.1016/j.addbeh.2014.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeder SA, Morris CD. Confronting a neglected epidemic: Tobacco cessation for persons with mental illnesses and substance abuse problems. Annu Rev Public Health. 2010;31:297–314. doi: 10.1146/annurev.publhealth.012809.103701. 1p following 314. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, Litten RZ, Allen JP, editors. Measuring alcohol consumption: Psychosocial and biochemical methods. Humana Press; Totowa, NJ: 1992. pp. 41–72. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Center for Behavioral Health Statistics and Quality. The NSDUH Report: Recent Trends in Menthol Cigarette Use; Rockville, MD: Nov 18, 2011. [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4th. Allyn and Bacon; Boston, MA: 2000. [Google Scholar]
- Tripp JC, Meshesha LZ, Teeters JB, Pickover AM, McDevitt-Murphy ME, Murphy JG. Alcohol craving and demand mediate the relation between posttraumatic stress symptoms and alcohol-related consequences. Exp Clin Psychopharmacol. 2015;23:324–31. doi: 10.1037/pha0000040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US Department of Health and Human Services. The health consequences of smoking— 50 years of progress: A report of the Surgeon General. Atlanta, GA: 2014. [Google Scholar]
- Yurasek AM, Murphy JG, Clawson AH, Dennhardt AA, MacKillop J. Smokers report greater demand for alcohol on a behavioral economic purchase task. J Stud Alcohol Drugs. 2013;74:626–34. doi: 10.15288/jsad.2013.74.626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziedonis D, Hitsman B, Beckham J, Zvolensky M, Adler L, udrain-McGovern J, Breslau N, Brown R, George T, Williams J, Calhoun P, Riley W. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine Tob Res. 2008;10:1691–1715. doi: 10.1080/14622200802443569. doi:905756217 [pii]\r10.1080/14622200802443569. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bakhshaie J, Sheffer C, Perez A, Goodwin RD. Major depressive disorder and smoking relapse among adults in the United States: a 10-year, prospective investigation. Psychiatry Res. 2015;226:73–7. doi: 10.1016/j.psychres.2014.11.064. [DOI] [PMC free article] [PubMed] [Google Scholar]


