Abstract
Proximity to primary healthcare facilities may be a serious barrier to accessing mental health services in resource-limited settings. In this study, we examined whether the distance to the primary healthcare clinic (PHCC) was associated with risk of depression in KwaZulu-Natal (KZN) Province, South Africa. Depressive symptoms and household coordinates data were accessed from the nationally representative South African National Income Dynamics Study (SA-NIDS). Distances between households and their nearest PHCCs were calculated and mixed-effects logistic regression models fitted to the data. Participants residing <6 kms from a PHCC (aOR=0.608, 95% CI:0.42–0.87) or 6–14.9 kms (aOR=0. 612, 95% CI:0.44–0.86) had a lower depression risk compared to those residing ≥15 kms from the nearest PHCC. Distance to the PHCC was independently associated with increased depression risk, even after controlling for key socioeconomic determinants. Minimizing the distance to PHCC through mobile health clinics and technology could improve mental health.
Keywords: primary healthcare clinic, depression, social disconnectedness, GPS, South Africa
Introduction
The importance of proximity to a primary healthcare (PHC) facility has been well-established in resource-limited settings [1–3]. Within the communicable diseases context, for example, distance to clinic and cost of transportation are recognized as major barriers to HIV treatment adherence [4–6]. A growing emphasis on community models of care that integrate mental health treatments into PHC systems [7] has focused attention on the role these barriers may have in the mental health context. Lack of access to, and availability of, mental health services (MHS) for individuals with mental illness, is a major challenge in sub-Saharan Africa [8]. Community-based mental health services (CMHS) are scarce or even absent, and many individuals have to access care at psychiatric (tertiary) hospitals that are located far from their homes.
Major depression represents a growing public health burden across the world. According to a recent systematic review, depressive disorders contribute more to ‘years lived with a disability’ than other mental and behavioral challenges [9]. Depression is a major public health challenge in South Africa [10], where, despite the availability of effective treatments, the need for CMHS is high and the treatment gap considerable. Previous research has shown that 9.8% of all South African adults have experienced a common mental disorder [11], but less than one quarter (22.6%) of those with a major depressive disorder sought care within the past 12 months [12]. It is likely that this substantial mental health treatment gap is partly a consequence of its historic past, where the enforced spatial separation of races created enduring disparities in access to healthcare services that have not been overcome. Black South Africans were particularly disadvantaged by being legally excluded from urban areas and forcibly moved into ethnically based undeveloped rural ‘homelands’. In post-apartheid South Africa, disparities in access to health services remain an enduring challenge [13], and many black South Africans remain socially disconnected from government-funded PHC services due to financial constraints [14,15].
Within many developing countries, mental health services receive a disproportionately small proportion of state funding, and the scarcity of mental health resources in these contexts has serious implications for access to effective care [8]. This is particularly evident in KwaZulu-Natal (KZN) Province in South Africa, where inadequate funding and a lack of human resources in mental health services have been reported [16]. Research shows that untreated depressive symptoms at a sub-threshold level can lead to major depression with a longer phase of residual symptoms [17], making timely access to care critical. As the frontline of the public healthcare provision in KZN [18], primary healthcare clinics (PHCC) provide treatment for various medical challenges, and a community-based healthcare model may be the key to realizing better mental health within this population. To date, however, the geospatial barriers to mental health that have planning and policy implications for implementing CMHS in the sub-Saharan African context have not been adequately understood. In the current study, we use data from a nationally representative longitudinal study to assess the association between proximity to the nearest primary healthcare clinic PHCC and the risk of depression within KZN.
Methods
Conceptual framework
The conceptual framework for this analysis is the Behavioral Model of Health Services Use framework [19], which was developed to address concerns related to social inequity in access to healthcare services among families [20], ethnic minorities and individuals from rural areas [21]. The rationale of this framework is that an individual’s decision to access healthcare services is often constrained by his or her position in the social structure, as well as the availability of these services. There are three major components to this framework [19]: predisposing factors (i.e. demographic background, social class, health beliefs); enabling factors (i.e. income, ability to travel, availability of services in the community); and need for care (i.e. perception of health needs). More recently, the model has been modified to account for geographic access (i.e., distance) as a predisposing factor that may constrain individuals from seeking care [22]. The magnitude of social disconnectedness [23], characterized by the experience of living far from the nearest PHCC, may increase and ultimately have a negative impact on individuals at risk of mental health problems, particularly depression.
Study design and sample
We used data from the South African National Income Dynamics Study (SA-NIDS), this being the first nationally representative panel study to contain in-depth information about participants of all ages in South Africa [24]. The SA-NIDS utilized a stratified, two-stage cluster sample design, and approximately 7,300 households were chosen from 400 of Statistics South Africa’s primary sampling units in the first wave. The adult questionnaires were administered to every consenting member aged 15 or older from eligible households. Our study utilized data from three waves: Wave 1 (2008), Wave 2 (2010), and Wave 3 (2012), with the sample limited to adult household members living in KZN. The adult questionnaires were available and administered in the country’s 11 official languages. Permission for the study was obtained from the University of KwaZulu-Natal Biomedical Research Ethics Committee (BE 111/14).
Measurement
The primary outcome of our current investigation was self-reported depressive symptoms obtained from the adult questionnaire (Waves 1–3). SA-NIDS utilizes the 10-item abridged version of the Center for Epidemiologic Studies Depression Scale (CES-D) to assess the severity of depressive symptomatology. Comparable to the original 20-item CES-D [25], the abridged version [26] has been shown to retain psychometric validity [27, 28]. The instrument captures depressive symptoms during the past week using four possible responses: 0 = rarely or none of the time (less than 1 day); 1 = some or little of the time (1–2 days); 2 = occasionally or a moderate amount of time (3–4 days); and 3 = almost or all of the time (5–7 days). Depression symptomatology is based on a total score of 10 items (range from 0–30; Cronbach’s alpha = 0.75), with a cutoff score of ≥ 10 used to indicate significant depressive symptoms (i.e. risk of depression). This cutoff value was derived from the seminal CES-D report by Andresen and colleagues [26].
The main study predictor for depressive symptoms was household proximity to the nearest primary healthcare clinic (PHCC). Proximity was calculated as the ellipsoidal distance between the participant’s household and his/her nearest PHCC. Household GPS coordinates were accessed (with permission) from the DataFirst’s Secure Data Centre at University of Cape Town, while publically available GPS co-ordinates for PHCCs were obtained from the KZN Department of Health [29]. The nearest PHCC was identified using QGIS version 2.12 “Lyon” [30]. The ellipsoidal distance between the households and their nearest PHCC was calculated using the “GEODIST” package [31] in Stata version 14. The ellipsoidal distance is known to be a computationally more intensive and accurate method for calculating the distance between two points along the surface of a mathematical model of the earth [32]. A previous South African study on the relationship between proximity to PHCC and health outcome utilized 5 and 7 km to indicate thresholds of ‘long distance’ [33]. The current study utilized a middle value of 6 km radius as that threshold. Information on age, education attainment, gender, marital status, race/ethnicity, employment status, household income, and geographic typology of residence (i.e. rural) was also obtained from the adult questionnaires (Waves 1–3), and included in the model to adjust for potential confounders.
Analysis
The analysis consisted of two stages. In the first stage we used descriptive statistics to summarize the baseline sociodemographic, clinical and household characteristics of our study cohort. In the second stage we investigated the association between the distance to the nearest PHCC and depressive symptoms using a mixed-effects logistic regression model. We adjusted the analysis for age, education attainment, gender, marital status, race/ethnicity, employment status, household income, geographic typology of residence, as well as the year of the NIDS assessment (for time trend). As SA-NIDS was designed as a complex survey, we further adjusted the analysis using post-stratification weights for the three waves. These weights were based on the age-sex-race distribution for the mid-year population estimates in 2008, 2010 and 2012 using figures obtained from Statistics South Africa [34,35].
Results
The summary of the baseline sociodemographic, household and clinical characteristics of our study cohort (n=4,039), which are presented in Table 1. Over half of study participants were female (60.0%) and aged less than 35 years old (55.9%), with the majority being Black African (78.6%). Most of the participants had completed at least a high school equivalent level of education (86.9%). Approximately half were single (54.7%), and not employed (59.2%), while a third (33.8%) had significant depressive symptoms. The majority of households (84%) were located <6 km from their closest PHCC.
Table 1.
Baseline sociodemographic and clinical characteristics
| n | % | ||
|---|---|---|---|
|
|
|||
| Individual characteristics (n=4,039): | |||
| Gender: | Male | 1,473 | 40.05% |
| Female | 2,566 | 59.95% | |
| Age group: | 15–19 | 828 | 18.50% |
| 20–24 | 581 | 14.47% | |
| 25–29 | 423 | 13.00% | |
| 30–34 | 337 | 9.89% | |
| 35+ | 1,862 | 44.14% | |
| Race/ethnicity: | African | 3,793 | 83.62% |
| Coloured‡ | 49 | 1.86% | |
| Asian/Indian | 150 | 8.66% | |
| White | 47 | 5.86% | |
| Educational attainment: | Less than high school | 798 | 13.12% |
| Completed high school | 2,548 | 62.66% | |
| Beyond high school | 693 | 24.22% | |
| Marital status: | Married/living with partner | 1,144 | 31.01% |
| Divorced/widow/separated | 467 | 10.43% | |
| Single | 2,413 | 58.56% | |
| Employment status: | Not employed | 2,468 | 56.37% |
| Employed | 1,548 | 43.63% | |
| Depression risk: | CES-D<10 | 2,559 | 66.16% |
| CES-D≥10 | 1,462 | 33.84% | |
| Household characteristics (n=1,765): | |||
| Geographic typology: | Rural formal | 261 | 14.39% |
| Tribal authority | 1,121 | 42.53% | |
| Urban formal | 274 | 26.11% | |
| Urban informal | 109 | 16.98% | |
| Income quantiles: | Bottom | 747 | 36.20% |
| Bottom/middle | 460 | 22.46% | |
| Middle | 264 | 14.87% | |
| Middle/high | 168 | 10.40% | |
| High | 126 | 16.07% | |
| Distance to PHC clinic: | < 6 km | 1,360 | 84.51% |
| 6–14.9 km | 363 | 14.50% | |
| ≥15km | 40 | 1.00% | |
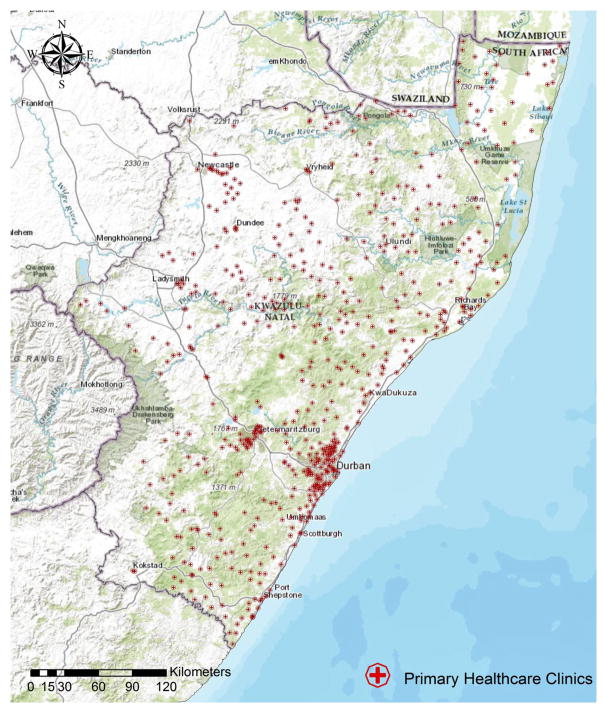
Figure 1 show that the PHCCs in KZN are concentrated predominantly in urban areas (e.g. Durban). Table 2 shows the adjusted mixed effects regression results for the association between the distance to PHCC and risk of depression. In comparison with those participants residing ≥15 km from a PHCC, those residing 6–14.9 kms away (adjusted odds ratio [aOR]=0. 612, 95% confidence interval [CI]: 0.44–0.86) and those residing <6 kms away (aOR=0.608, 95% CI: 0.42–0.87) had a significantly lower odds of depressive symptomatology. In addition, we found that female gender, older age, African/Coloured race/ethnicity, unemployed status, and urban informal residence were significantly associated with depressive symptomatology.
Figure 1.
Location of primary healthcare clinics in KwaZulu-Natal
Table 2.
Relationship between proximity to PHC clinic and depression risk using mixed-effects logistic regression
| aOR | Robust SE | Z | 95% CI: | |||
|---|---|---|---|---|---|---|
|
|
||||||
| Proximity to PHC clinic: | [≥15km] | |||||
| 6–14.9 km | 0.612 | 0.11 | −2.84 | 0.44 | 0.86 | |
| <6 km | 0.608 | 0.11 | −2.70 | 0.42 | 0.87 | |
| Gender: | [Male] | |||||
| Female | 1.20 | 0.08 | 2.66 | 1.05 | 1.38 | |
| Age group: | [15–19] | |||||
| 20–24 | 1.29 | 0.14 | 2.40 | 1.05 | 1.58 | |
| 25–29 | 1.91 | 0.22 | 5.72 | 1.53 | 2.39 | |
| 30–34 | 2.15 | 0.28 | 5.92 | 1.67 | 2.77 | |
| 35+ | 2.63 | 0.27 | 9.32 | 2.15 | 3.23 | |
| Race/ethnicity: | [White] | |||||
| African | 4.31 | 1.92 | 3.29 | 1.81 | 10.30 | |
| Coloured | 3.62 | 1.74 | 2.68 | 1.41 | 9.28 | |
| Asian/Indian | 1.70 | 0.94 | 0.95 | 0.57 | 5.04 | |
| Educational attainment: | [Less than high school] | |||||
| Completed high school | 0.96 | 0.08 | −0.49 | 0.82 | 1.13 | |
| Beyond high school | 0.84 | 0.10 | −1.48 | 0.67 | 1.06 | |
| Marital status: | [Married/living with partner] | |||||
| Divorced/widow/separated | 1.23 | 0.17 | 1.56 | 0.95 | 1.60 | |
| Single | 1.14 | 0.10 | 1.52 | 0.96 | 1.35 | |
| Employment status: | [Not employed] | |||||
| Employed | 0.73 | 0.06 | −3.71 | 0.62 | 0.86 | |
| Geographic typology: | [Urban informal] | |||||
| Rural formal | 0.61 | 0.10 | −2.95 | 0.44 | 0.85 | |
| Tribal authority | 0.71 | 0.06 | −3.92 | 0.59 | 0.84 | |
| Urban formal | 0.90 | 0.10 | −0.92 | 0.72 | 1.13 | |
| Income quantiles: | [Bottom] | |||||
| Bottom/middle | 1.06 | 0.09 | 0.65 | 0.90 | 1.24 | |
| Middle | 0.88 | 0.08 | −1.41 | 0.75 | 1.05 | |
| Middle/high | 0.84 | 0.08 | −1.83 | 0.70 | 1.01 | |
| High | 0.81 | 0.09 | −1.95 | 0.66 | 1.00 | |
| Assessment period: | [2008] | |||||
| 2010 | 0.72 | 0.06 | −4.23 | 0.62 | 0.84 | |
| 2012 | 0.86 | 0.07 | −1.92 | 0.74 | 1.00 | |
Reference category in bracket.
PHC stands for primary healthcare.
Discussion
Residing far from a primary healthcare clinic (PHCC) poses a significant and independent risk for depressive symptoms among KZN adults who participated in the SA-NIDS survey, even after controlling for key socioeconomic determinants of depression. As hypothesized, participants who were physically (and thus we suggest socially) disconnected from the closest PHC facility (by virtue of residing further away) were more likely to be at risk of depression.
Our study results can be explained by the Behavioral Model of Health Services Use framework [19], which provides a conceptual link between the distance to a PHCC and depression symptomatology. Notably, McLaren and colleagues [33] reported that participants residing further from a clinic had a lower likelihood of a health consultation, while a six-nation primary care study (including both developed and developing countries) showed that longer distance was a major obstacle to accessing treatment for depression [36]. Aspects of treatment that are likely influenced by geographic inaccessibility include: having reduced contact with healthcare service providers [37]; limited available psychotherapy [38]; and less access to outpatient treatment [39–40].
We also found, as indicated in Table 2, that certain residential typology (i.e. rural compared to urban informal area) was significantly associated with lower depression risk, warranting further discussion about the role of health and place within the South African context. International findings on urban-rural differences are often contradictory, but most reviews suggest that depression is marginally higher in urban areas [41–47]. A recent South African study confirmed a high prevalence in young individuals residing in an urban informal settlement, with almost 50% of males and almost 60% of females reporting significant depressive symptoms [48]. South Africa has a long history of labor migration, with mining being the bedrock of the country’s economy throughout the 20th century [49]. Out of economic necessity, many individuals, in particular young Black South Africans, left families behind to seek employment outside their rural/traditional home areas [50], resulting in erosion of the traditional way of life and broken family ties [51,52]. Furthermore, Black African migrants often lived in under-resourced ‘townships’ and other urban informal areas on the city outskirts that often lacked urban planning and provided little or no basic services. This living arrangement (e.g. mining hostels) has continued after the advent of democracy [53]. The loss or lack of psychosocial support as result of disconnection from family of origin, as well as poor amenities/services associated with living in urban informal areas, may in part account for the association we have found between urban informal residence and higher risk for depression.
There were several study limitations. First, SA-NIDS is a nationally (rather than provincially) representative sample by design, and our results may therefore not be generalized to the entire KZN. Second, it is acknowledged that the data on mental health services utilization (and level of care provision at PHCC) in SA-NIDS is limited. Assumptions had to be made that PHCCs provide limited mental health services (with little variation across clinics) for patents presenting with depression and/or comorbid medical illness.
Notwithstanding these limitations, the current study is one of only a few within a Sub-Saharan setting that examined the relationship between household proximity to healthcare facility and depression risk. Furthermore, our study has important policy implications for addressing population mental health needs in countries that have limited resources. It is well established that in order to be effective, the optimal treatment for depression as a life-long condition requires both pharmacotherapeutic and psychotherapic approaches [54], the latter in particular requiring frequent contact with a provider [37]. This highlights the need for expanding PHC services that have appropriately integrated mental healthcare interventions. Our results suggest that where primary services are geographically accessible, treatment coverage is likely to be improved in the population; and the burden associated with common mental disorders mitigated to some extent. Importantly, while the rationale for integrating mental health into PHC is evident, research on the feasibility, acceptability, and effectiveness of such care models is warranted in South Africa [55].
Beyond a focus on PHC, we also acknowledge other potential solutions that may reduce inaccessibility to mental health services, such as mobile health clinics and mHealth (mobile health) technologies. Although the latter is at a formative stage of implementation, there are a number of South African studies demonstrating its potential for treating depression [56,57]. Finally, in addition to reaffirming the call for integration of mental health care into community-based primary care in KwaZulu-Natal Province [58], we argue that a geospatial or ‘place-based’ approach [59–61] to mental health care provision is critical to understanding the structural factors contributing to risk for mental disorders within developing country settings.
Acknowledgments
Role of the Funding Source:
AT was supported by SA MRC Flagship grant (MRC-RFAUFSP-01-2013/UKZN HIVEPI) and National Institutes of Health Research Training Grant (R25TW009337), funded by the Fogarty International Center and the National Institute of Mental Health. AV was supported by SA MRC Flagship grant (MRC-RFAUFSP-01-2013/UKZN HIVEPI). FT was supported by South African MRC Flagship (MRC-RFA-UFSP-01–2013/UKZN HIVEPI) and NIH grants (R01HD084233 and R01AI124389) as well as a UK Academy of Medical Sciences Newton Advanced Fellowship (NA150161). The study was also supported by University of KwaZulu-Natal funding to RS. The content is solely the responsibility of the authors and does not necessarily represent the official views of the SA MRC, UK Academy of Medical Sciences or the NIH. All authors declare that they have no conflicts of interest.
Waves 1–3 Data: Southern Africa Labour and Development Research Unit. National Income Dynamics Study. Cape Town: Southern Africa Labour and Development Research Unit [producer], 2015. Cape Town: DataFirst [distributor], 2015. We thank Lynn Woolfrey at DataFirst at the University of Cape Town.
References
- 1.Cooke GS, Tanser FC, Bärnighausen TW, Newell ML. Population uptake of antiretroviral treatment through primary care in rural South Africa. BMC Public Health. 2010;10:1. doi: 10.1186/1471-2458-10-585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Govindasamy D, Ford N, Kranzer K. Risk factors, barriers and facilitators for linkage to antiretroviral therapy care: a systematic review. AIDS. 2012;26:2059–2067. doi: 10.1097/QAD.0b013e3283578b9b. [DOI] [PubMed] [Google Scholar]
- 3.Siedner MJ, Lankowski A, Tsai AC, Muzoora C, Martin JN, Hunt PW, Haberer JE, Bangsberg DR. GPS-measured distance to clinic, but not self-reported transportation factors, are associated with missed HIV clinic visits in rural Uganda. AIDS. 2013;27:1503. doi: 10.1097/QAD.0b013e32835fd873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Weiser S, Wolfe W, Bangsberg D, Thior I, Gilbert P, Makhema J, Kebaabetswe P, Dickenson D, Mompati K, Essex M, Marlink R. Barriers to antiretroviral adherence for patients living with HIV infection and AIDS in Botswana. J Acquir Immune Defic Syndr. 1999;34:281. doi: 10.1097/00126334-200311010-00004. [DOI] [PubMed] [Google Scholar]
- 5.Geng EH, Nash D, Kambugu A, Zhang Y, Braitstein P, Christopoulos KA, Muyindike W, Bwana MB, Yiannoutsos CT, Petersen ML, Martin JN. Retention in care among HIV-infected patients in resource-limited settings: emerging insights and new directions. Curr HIV/AIDS Rep. 2010;7:234–44. doi: 10.1007/s11904-010-0061-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coetzee B, Kagee A, Vermeulen N. Structural barriers to adherence to antiretroviral therapy in a resource-constrained setting: the perspectives of health care providers. AIDS Care. 2011;23:146–51. doi: 10.1080/09540121.2010.498874. [DOI] [PubMed] [Google Scholar]
- 7.Lancet Global Mental Health Group. Scale up services for mental disorders: a call for action. Lancet. 2007;370:1241–1252. doi: 10.1016/S0140-6736(07)61242-2. [DOI] [PubMed] [Google Scholar]
- 8.Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370:878–89. doi: 10.1016/S0140-6736(07)61239-2. [DOI] [PubMed] [Google Scholar]
- 9.Murray CJ, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2010;380:2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 10.Lund C, Kleintjes S, Kakuma R, Flisher AJ MHaPP Research Programme Consortium. Public sector mental health systems in South Africa: inter-provincial comparisons and policy implications. Soc Psychiatry Psychiatr Epidemiol. 2010;45:393–404. doi: 10.1007/s00127-009-0078-5. [DOI] [PubMed] [Google Scholar]
- 11.Herman AA, Stein DJ, Seedat S, Heeringa SG, Moomal H, Williams DR. The South African Stress and Health (SASH) study: 12-month and lifetime prevalence of common mental disorders. S Afr Med J. 2009;99:339–44. [PMC free article] [PubMed] [Google Scholar]
- 12.Seedat S, Williams DR, Herman AA, Moomal H, Williams SL, Jackson PB, Myer L, Stein DJ. Mental health service use among South Africans for mood, anxiety and substance use disorders. S Afr Med J. 2009;99:346–5. [PMC free article] [PubMed] [Google Scholar]
- 13.Hassim A, Heywood M, Berger J. Health and democracy: A guide to human rights, health law and policy in postapartheid South Africa. Cape Town: SiberInk; 2007. [Google Scholar]
- 14.Goudge J, Gilson L, Russell S, Gumede T, Mills A. Affordability, availability and acceptability barriers to health care for the chronically ill: longitudinal case studies from South Africa. BMC Health Serv Res. 2009;9:1. doi: 10.1186/1472-6963-9-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Maillacheruvu P, McDuff E. South Africa’s return to primary care: The struggles and strides of the primary health care system. J Glob Health. 2014 Accessed from: http://www.ghjournal.org/south-africas-return-to-primary-care-the-struggles-and-strides-of-the-primary-health-care-system/
- 16.Burns JK. Mental health services funding and development in KwaZulu-Natal: a tale of inequity and neglect. S Afr Med J. 2010;100:662–666. doi: 10.7196/samj.4100. [DOI] [PubMed] [Google Scholar]
- 17.Iacoviello BM, Alloy LB, Abramson LY, Choi JY. The early course of depression: a longitudinal investigation of prodromal symptoms and their relation to the symptomatic course of depressive episodes. J Abnorm Psychol. 2010;119:459. doi: 10.1037/a0020114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.KwaZulu-Natal Department of Health. New mobile clinics to enhance the School Health Programme and access for people in informal settlements and rural communities. 2012 Accessed from: http://www.kznhealth.gov.za/comms/mobileclinics15.3.2012.htm.
- 19.Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? J Health Soc Behav. 1995;36:1–10. [PubMed] [Google Scholar]
- 20.Andersen R. A behavioral model of families’ use of health services. Chicago, IL: University of Chicago; 1968. [Google Scholar]
- 21.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. Milbank Mem Fund Q. 1973;51:95–124. [PubMed] [Google Scholar]
- 22.Arcury TA, Gesler WM, Preisser JS, Sherman J, Spencer J, Perin J. The effects of geography and spatial behavior on health care utilization among the residents of a rural region. Health Serv Res. 2005;40:135–56. doi: 10.1111/j.1475-6773.2005.00346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cornwell EY, Waite LJ. Social disconnectedness, perceived isolation, and health among older adults. J Health Soc Behav. 2009;50:31–48. doi: 10.1177/002214650905000103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Southern Africa Labour and Development Research Unit. NIDS Wave 2: Overview 2012. Cape Town: Southern Africa Labour and Development Research Unit; 2013. [Google Scholar]
- 25.Radloff LS. The CES-D Scale. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 26.Andersen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: Evaluation of a short form of the CES-D. Am J Prev Med. 1994;10:77–84. [PubMed] [Google Scholar]
- 27.Björgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20:429–36. doi: 10.1177/1073191113481998. [DOI] [PubMed] [Google Scholar]
- 28.Cole JC, Rabin AS, Smith TL, Kaufman AS. Development and validation of a Rasch-derived CES-D short form. Psychol Assess. 2004;16:360–372. doi: 10.1037/1040-3590.16.4.360. [DOI] [PubMed] [Google Scholar]
- 29.KwaZulu-Natal Department of Health. [Accessed October 2016];List of clinics. 2013 from: http://www.kznhealth.gov.za/Provincial_Clinic_10.2013.xlsx.
- 30.QGIS Development Team. QGIS Geographic Information System. Open Source Geospatial foundation; 2015. [Google Scholar]
- 31.Picard R. Statistical Software Components. 2012. GEODIST: Stata module to compute geodetic distances. [Google Scholar]
- 32.Vincenty T. Direct and inverse solutions of geodesics on the ellipsoid with application of nested equations. Survey Review. 1975;22:88–93. [Google Scholar]
- 33.McLaren ZM, Ardington C, Leibbrandt M. Distance decay and persistent health care disparities in South Africa. BMC Health Serv Res. 2014;14:1. doi: 10.1186/s12913-014-0541-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wittenberg M. Weights: Report on NIDS Wave 1. Cape Town: Southern Africa Labour and Development Research Unit; 2009. [Google Scholar]
- 35.Brown M, Daniels RC, de Villiers L, Leibbrandt M, Woolard I. National Income Dynamics Study Wave 2 user manual. Cape Town: Southern Africa Labour and Development Research Unit; 2013. [Google Scholar]
- 36.Simon GE, Fleck M, Lucas R, Bushnell DM. Prevalence and predictors of depression treatment in an international primary care study. Am J Psychiatry. 2004;161:1626–34. doi: 10.1176/appi.ajp.161.9.1626. [DOI] [PubMed] [Google Scholar]
- 37.Fortney J, Rost K, Zhang M, Warren J. The impact of geographic accessibility on the intensity and quality of depression treatment. Med Care. 1999;37:884–93. doi: 10.1097/00005650-199909000-00005. [DOI] [PubMed] [Google Scholar]
- 38.Pfeiffer PN, Glass J, Austin K, Valenstein M, McCarthy JF, Zivin K. Impact of distance and facility of initial diagnosis on depression treatment. Health Serv Res. 2011;46:768–86. doi: 10.1111/j.1475-6773.2010.01228.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marcus SC, Fortney JC, Olfson M, Ryan ND. Travel distance to outpatient treatment for depression. Psychiatr Serv. 1997;48:1005. doi: 10.1176/ps.48.8.1005. [DOI] [PubMed] [Google Scholar]
- 40.Schmitt SK, Phibbs CS, Piette JD. The influence of distance on utilization of outpatient mental health aftercare following inpatient substance abuse treatment. Addict Behav. 2003;28:1183–92. doi: 10.1016/s0306-4603(02)00218-6. [DOI] [PubMed] [Google Scholar]
- 41.Dohrenwend BP, Dohrenwend BS. Psychiatric disorders in urban settings. In: Arieti S, Caplan S, editors. American Handbook of Psychiatry. Basic Books; New York: 1974. pp. 424–447. [Google Scholar]
- 42.Mueller DP. The current status of urban-rural differences in psychiatric disorder. An emerging trend for depression. J Nerv Ment Dis. 1981;169:18–27. doi: 10.1097/00005053-198101000-00003. [DOI] [PubMed] [Google Scholar]
- 43.Marsella AJ. Urbanization, mental health, and social deviancy: A review of issues and research. Am Psychol. 1998;53:624. doi: 10.1037//0003-066x.53.6.624. [DOI] [PubMed] [Google Scholar]
- 44.Neff JA. Urbanicity and depression reconsidered: The evidence regarding depressive symptomatology. J Nerv Ment Dis. 1983;171:546–552. doi: 10.1097/00005053-198309000-00004. [DOI] [PubMed] [Google Scholar]
- 45.Verheij RA. Explaining urban-rural variations in health: a review of interactions between individual and environment. Soc Sci Med. 1996;42:923–935. doi: 10.1016/0277-9536(95)00190-5. [DOI] [PubMed] [Google Scholar]
- 46.Webb SD. Rural-urban differences in mental health. In: Freeman H, editor. Mental health and the environment. Churchill Livingston; London: 1984. pp. 226–249. [Google Scholar]
- 47.Peen J, Schoevers RA, Beekman AT, Dekker J. The current status of urban-rural differences in psychiatric disorders. Acta Psychiatrica Scandinavica. 2010;121:84–93. doi: 10.1111/j.1600-0447.2009.01438.x. [DOI] [PubMed] [Google Scholar]
- 48.Gibbs A, Govender K, Jewkes R. An exploratory analysis of factors associated with depression in a vulnerable group of young people living in informal settlements in South Africa. Glob Public Health. 2016:1–16. doi: 10.1080/17441692.2016.1214281. dx.doi.org/10.1080/17441692.2016.1214281. [DOI] [PubMed]
- 49.Coovadia H, Jewkes R, Barron P, Sanders D, McIntyre D. The health and health system of South Africa: historical roots of current public health challenges. Lancet. 2009;374:817–834. doi: 10.1016/S0140-6736(09)60951-X. [DOI] [PubMed] [Google Scholar]
- 50.Harington JS, McGlashan ND, Chelkowska EZ. A century of migrant labour in the gold mines of South Africa. Journal of the South African Institute of Mining and Metallurgy. 2004;104:65–72. [Google Scholar]
- 51.Smit R. The impact of labor migration on African families in South Africa: Yesterday and today. J Comp Fam Stud. 2001;32:533–548. [Google Scholar]
- 52.Moeno SN. Family life in Soweto, Gauteng, South Africa. In: Oheneba-Sakyi Y, Takyi BK, editors. African families at the turn of the 21st century. Praeger, Westport: 2006. p. 249. [Google Scholar]
- 53.Lurie MN, Williams BG. Migration and health in Southern Africa: 100 years and still circulating. Health Psychol Behav Med. 2014;2:34–40. doi: 10.1080/21642850.2013.866898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Thase ME, Greenhouse JB, Frank E, Reynolds CF, Pilkonis PA, Hurley K, Grochocinski V, Kupfer DJ. Treatment of major depression with psychotherapy or psychotherapy-pharmacotherapy combinations. Arch Gen Psychiatry. 1997;54:1009–15. doi: 10.1001/archpsyc.1997.01830230043006. [DOI] [PubMed] [Google Scholar]
- 55.Schneider M, Baron E, Breuer E, Docrat S, Honikman S, Kagee A, Onah M, Skeen S, Sorsdahl K, Tomlinson M, Van der Westhuizen C, Lund C. Integrating mental health into South Africa’s health system: current status and way forward. South African Health Review. 2016:153–63. [Google Scholar]
- 56.Tsai AC, Tomlinson M, Dewing S, Le Roux IM, Harwood JM, Chopra M, Rotheram-Borus MJ. Antenatal depression case finding by community health workers in South Africa: feasibility of a mobile phone application. Arch Womens Ment Health. 2014;17:423–31. doi: 10.1007/s00737-014-0426-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tomita A, Kandolo KM, Susser E, Burns JK. Use of short messaging services to assess depressive symptoms among refugees in South Africa: Implications for social services providing mental health care in resource-poor settings. J Telemed Telecare. 2016;22:369–77. doi: 10.1177/1357633X15605406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Petersen I, Ssebunnya J, Bhana A, Baillie K. Lessons from case studies of integrating mental health into primary health care in South Africa and Uganda. Int J Ment Health Syst. 2011;5:1. doi: 10.1186/1752-4458-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tanser F, Hosegood V, Benzler J, Solarsh G. New approaches to spatially analyse primary health care usage patterns in rural South Africa. Trop Med Int Health. 2001;6:826–38. doi: 10.1046/j.1365-3156.2001.00794.x. [DOI] [PubMed] [Google Scholar]
- 60.Tanser F. Methodology for optimising location of new primary health care facilities in rural communities: a case study in KwaZulu-Natal, South Africa. J Epidemiol Community Health. 2006;60:846–50. doi: 10.1136/jech.2005.043265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tanser F, Gijsbertsen B, Herbst K. Modelling and understanding primary health care accessibility and utilization in rural South Africa: an exploration using a geographical information system. Soc Sci Med. 2006;63:691–705. doi: 10.1016/j.socscimed.2006.01.015. [DOI] [PubMed] [Google Scholar]
- 62.Statistics South Africa. Concept and defenitions. Pretoria: Statistics South Africa; 2004. [Google Scholar]
- 63.Brown K. Coloured and black relations in South Africa: The burden of racialized hierarchy. Macalester International. 2000;9:198–203. [Google Scholar]