Abstract
Macular hole-associated retinal detachment in high myopia is described as a final stage in progression of myopic traction maculopathy (MTM).1–3 Shimada et al4 described the progressive stages of MTM from macular retinoschisis to serous retinal detachment in high myopia. Stage 4 MTM is characterised as disappearance of retinoschisis with progression to retinal detachment due to macular hole formation. It is hypothesised that vitreoschisis and abnormal vitreo-retinal interface create the premacular tangential traction.5 6 Intraoperative triamcinolone acetonide is used to visualise the residual posterior vitreous cortex (PVC). We hereby describe the utility of microscope-integrated optical coherence tomography (MIOCT) in assisting complete removal of PVC and internal limiting membrane (ILM) peeling with multilayered inverted ILM flap in the treatment of myopic macular hole retinal detachment. MIOCT helped identify vitreoschisis and confirm the position of ILM flaps over the macular hole intraoperatively.
Keywords: ophthalmology, macula, retina
Background
Our case highlights the decisive role that real-time intraoperative optical coherence tomography (OCT) imaging plays in retinal surgery. To our knowledge, this is the first report of intraoperative use of microscope-integrated OCT (MIOCT) in myopic macular hole retinal detachment (MMHRD), illustrating its importance in ensuring complete vitreous removal and confirming the closure of macular hole (MH) in real time with multilayered inverted internal limiting membrane (ILM) flaps.
Case presentation
Presence of rhegmatogenous retinal detachment associated with MH in high myopia is well known.1–6 Panozzo and Mercanti first used the term ‘myopic traction maculopathy’ (MTM) for a spectrum of diseases varying from macular retinoschisis to MH retinal detachments in high myopes.7 Residual posterior vitreous cortex remaining after anomalous posterior vitreous detachment, posterior staphyloma and chorioretinal degeneration have been attributed to the development of MH. In such eyes, anomalous posterior vitreous detachment causes anteroposterior and tangential traction, subsequently leading to retinal detachment.8 Complete removal of this posterior vitreous cortex is of utmost importance in treating MTM, especially when not combined with macular buckling. Recurrence of MTM due to fibrocellular proliferation over the residual vitreous cortex post vitrectomy has been reported.9
First demonstrated by Tao et al at Duke University in 2010,10 intraoperative MIOCT has been shown to be useful for intraoperative retinal imaging.11–13 We describe a case with MMHRD where MIOCT was used to guide and confirm removal of posterior vitreous cortex and placement of inverted ILM flap intraoperatively.
Case history
A 51-year-old man presented to us with complaints of slowly progressive painless decrease in vision in his right eye for the past 4 years with a significant fall over the last 6 months. He had history of low vision in his right eye since childhood, suggesting severe anisometropic amblyopia as described thereafter. No other significant ocular or systemic history was found. Ocular examination revealed a best corrected visual acuity of counting fingers at 1 metre OD and 20/20 OS. Slit lamp biomicroscopy of the anterior segment was within normal limits except for OD showing nuclear sclerosis (NS) grade 2 with cortical spokes while OS was NS 1. Further 90D biomicroscopy showed myopic fundus with tilted disc, peripapillary atrophy and posterior staphyloma in OD. An MH of one-third disc diameter was found, with posterior pole retinal detachment that extended inferotemporally beyond the major arcade vessels in OD. OS showed a non-myopic fundus. Peripheral paving stone and pigmentary degenerations were present oculus uterque (OU). Patient was diagnosed as a case of OD unilateral high myopia with cataract with MMHRD and OS early cataract.
Investigations
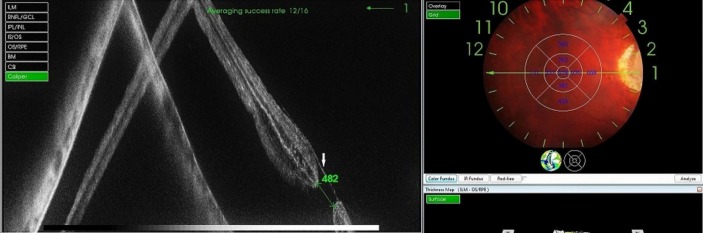
His old records revealed a unilateral myopia of −7.5 DS in OD. Immersion axial length measurement was 28.73 mm OD and 23.89 mm OS. A swept-source OCT (DRI OCT Triton, Topcon, the Netherlands) showed a full-thickness MH with a horizontal minimum diameter of 432 µ (figure 1) with posterior detachment. A layer of hyaloid was also seen over the inner retinal surface, bridging over the hole with adherence to its edges.
Figure 1.
Preoperative swept-source optical coherence tomography of the right eye showing a full-thickness macular hole of 432 µ horizontal diameter with macular detachment. A fine layer of vitreous cortex referring to the posterior hyaloid is also visualised bridging over the macular hole (white arrow).
Treatment
Surgical technique
Right eye phacoemulsification with posterior chamber implantation of a single-piece acrylic foldable intraocular lens in capsular bag (+5D), followed by a 23-gauge standard pars plana vitrectomy, was performed. After core vitrectomy, preservative-free triamcinolone acetonide (TA) was injected into the vitreous cavity, and posterior vitreous detachment (PVD) was induced. After successful induction of PVD, peripheral vitrectomy was done without indentation. MIOCT (Zeiss RESCAN 700, Carl Zeiss Meditec, Germany) was used to evaluate the intraoperative configuration of MH before membrane peeling. Despite induction of PVD, a minimal traction, probably related to incomplete removal of the posterior hyaloid, as typically observed in high myopic eyes with vitreoschisis, was noted on the edges of the MH (figure 2). After reinjection of TA, few crystals were noted to be adherent in a fine sheet around and over the hole. This layer of residual posterior vitreous cortex was mechanically peeled off using intravitreal forceps with direct visualisation aided by MIOCT (figure 3). After its removal, 0.025% Brilliant Blue G (ILM Blue, D.O.R.C. International, the Netherlands) was injected to stain the ILM. Some amount of dye was noted to pass subretinal. Perfluorocarbon liquid (PFCL) (Aurooctane, Aurolab, Aravind Eye Care System, Madurai, India) was injected a little beyond the posterior staphyloma, and flattening of retina was noted by MIOCT. PFCL injection displaced the subretinal dye peripherally, which was removed subsequently during subretinal fluid drainage at a later step. MIOCT-guided ILM peeling was done by pinch and grasp technique. Multiple ILM flaps were raised, and multilayered inverted ILM flaps were tucked into the MH with Tano’s diamond dusted membrane scraper. MIOCT confirmed the presence of ILM flaps within the MH (figure 4). Residual peripheral subretinal fluid was then drained through a peripheral superotemporal retinotomy followed by fluid/air exchange. Peripheral interface vitrectomy was done to complete shaving of the vitreous base. Endolaser was done at the retinotomy site and the peripheral degenerations followed by injection of perfluoropropane (14% C3F8) gas. Sclerotomies were then sutured, and the patient was asked to maintain a prone positioning for 2 weeks. A longer positioning was advised in view of associated retinal detachment, although MH closure is reported usually within 1 week.
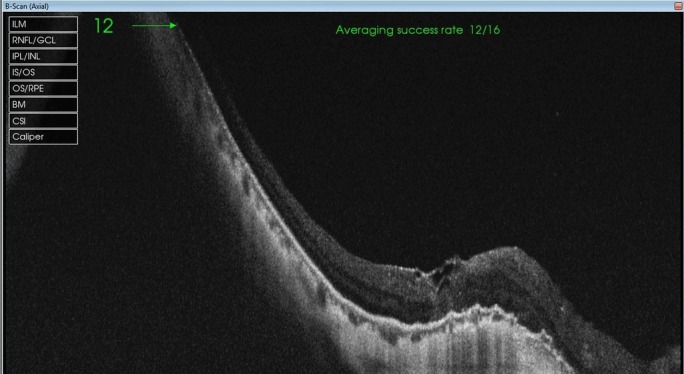
Figure 2.
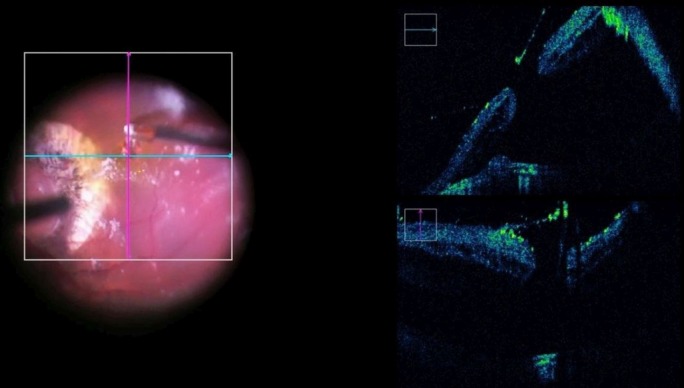
Intraoperative microscope-integrated optical coherence tomography image after posterior vitreous detachment induction, showing vitreoretinal traction at the edge of the macular hole, suggestive of an intact layer of posterior vitreous cortex, which is well identified by triamcinolone acetonide crystals.
Figure 3.
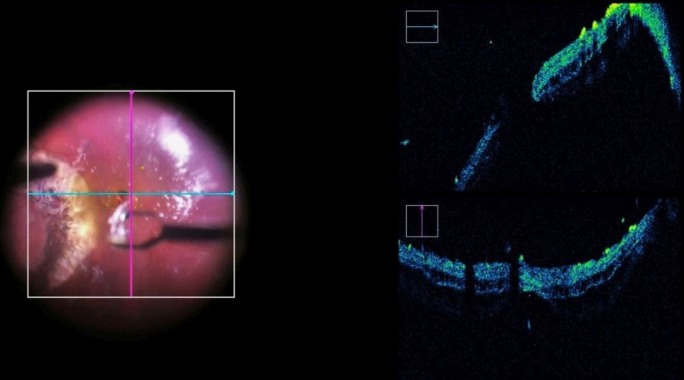
Intraoperative microscope-integrated optical coherence tomography grab showing sudden release of traction at the macular hole edges after the posterior hyaloid is peeled off from the macula.
Figure 4.
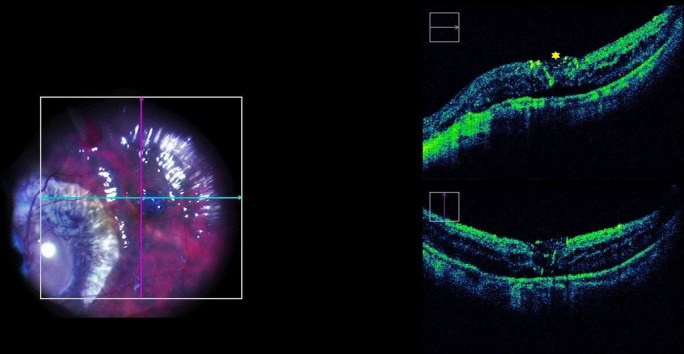
Intraoperative image of microscope-integrated intraoperative optical coherence tomography (MIOCT) grab after inverted internal limiting membrane (ILM) flap technique, facilitating macular hole closure with ILM flaps visible into the macular hole (yellow asterisk). The position of flaps is confirmed in real time via MIOCT.
Outcome and follow-up
On postoperative day 1, the retina was attached, and the MH appeared closed with the ILM flap. A swept-source OCT confirmed the position of ILM flaps over the hole with retinal attachment (figure 5). On follow-up after 4 weeks, the MH was found to have a type 1 closure with the retina well attached.
Figure 5.
Postoperative swept-source optical coherence tomography of the right eye showing closure of macular hole with reattachment of neurosensory retina.
Discussion
MH leading to retinal detachment is well known in severely myopic eyes.14 Tangential vitreous traction over the retina is only one of multiple factors responsible for myopic retinoschisis,4 15 myopic MH and MMHRD.4 8 16 Other factors which contribute significantly to such pathologies include posterior staphyloma causing anteroposterior traction, chorioretinal atrophy leading to weak adhesion between neurosensory retina and retinal pigment epithelium, the ILM and the inelasticity of stretched retinal vessels.8 16
Many surgical options have been advocated for treatment of MH-related retinal detachments. Proposed techniques include vitrectomy with posterior hyaloid removal,17 with or without ILM peeling,4 18–20 using gas21 or silicon oil tamponade.22 Macular buckling,23 vitrectomy with scleral imbrication24 and gas injection25 are other treatment options described to increase rate of success. Recently, the use of inverted ILM flap technique into MH for retinal reattachment has also been described.26
Presence of PVD in high myopia is approximately 50% in eyes undergoing vitrectomy, with less than 15% PVD in eyes having myopic foveoschisis.27 This emphasises the need for complete PVD induction in eyes with MMHRD. Triamcinolone acetonide crystal-assisted removal of posterior hyaloid has been considered as the gold standard to achieve this aim.
In our case, MIOCT (Zeiss RESCAN, Carl Zeiss Meditec, Germany) was especially helpful to identify intraoperatively the presence of a fine layer of posterior vitreous cortex. MIOCT guided us in real time in confirming the complete removal of traction over the edge of the MH. This allowed the surgeon to avoid MH closure failure or recurrence due to reproliferation of any epiretinal tissue as reported by Sepúlveda et al9 with subsequent macular redetachment.
MHs are often missed in pathological myopes due to chorioretinal scarring and thin retinal tissue. Intraoperatively, it is always a challenge to identify the hole edge and ILM once the subretinal fluid is displaced peripherally by heavier PFCL. In our case, MIOCT facilitated the visualisation of MH edges and guided the peeling of ILM with real-time feedback on the heads-up display within the eyepiece. This allowed to confirm the presence of ILM flaps in multiple layers into the MH.
MIOCT has been reported to affect the surgical decision making intraoperatively in more than 40% cases by Pfau et al.28 MIOCT influenced surgical decision making by helping in identification of ILM/epiretinal membrane (ERM) cleavage sites. In our case as well, intraoperative OCT played a significant role in decision making. To the best of our knowledge, the use of MIOCT has not been previously reported in cases with MMHRD.
In conclusion, we advise pars plana vitrectomy with removal of complete posterior vitreous cortex with inverted multilayered ILM flap placement over the MH for MMHRD patients. MIOCT is an invaluable tool for the treatment of such cases, providing real-time feedback to the surgeon helping to better visualise both the MH and ILM/ERM visualisation intraoperatively.
Learning points.
Complete removal of posterior vitreous cortex and internal limiting membrane (ILM) peeling are the ‘cornerstone’ of surgery for myopic traction maculopathy.
Microscope-integrated optical coherence tomography (MIOCT) is a critically important tool in modern-day microincision vitreous surgery and impacts surgical decision making.
An inverted ILM flap technique is a useful method for closure of macular holes in such retinal detachments.
MIOCT helps the surgeon in confirming the position of ILM flaps intraoperatively in real-time surgery. A displaced or lost flaps can be recognised and corrected during the surgery.
Footnotes
Contributors: AK was involved in planning, reporting and forming the concept and design of our report. He was also the surgeon and the one who operated the MIOCT. AK also contributed to the preparation of manuscript and proofreading. PK contributed in reporting, data acquisition, analysis, manuscript preparation and proofreading. RR contributed in planning, manuscript preparation, analysis and proofreading. AM helped in data acquisition and analysis for the report.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Hirakata A, Hida T. Vitrectomy for myopic posterior retinoschisis or foveal detachment. Jpn J Ophthalmol 2006;50:53–61. 10.1007/s10384-005-0270-4 [DOI] [PubMed] [Google Scholar]
- 2.Panozzo G, Mercanti A. Vitrectomy for myopic traction maculopathy. Arch Ophthalmol 2007;125:767–72. 10.1001/archopht.125.6.767 [DOI] [PubMed] [Google Scholar]
- 3.Smiddy WE, Kim SS, Lujan BJ, et al. Myopic traction maculopathy: spectral domain optical coherence tomographic imaging and a hypothesized mechanism. Ophthalmic Surg Lasers Imaging 2009;40:169–73. 10.3928/15428877-20090301-21 [DOI] [PubMed] [Google Scholar]
- 4.Shimada N, Ohno-Matsui K, Yoshida T, et al. Progression from macular retinoschisis to retinal detachment in highly myopic eyes is associated with outer lamellar hole formation. Br J Ophthalmol 2008;92:762–4. 10.1136/bjo.2007.131359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Panozzo G, Mercanti A. Vitrectomy for myopic traction maculopathy. Arch Ophthalmol 2007;125:767–72. 10.1001/archopht.125.6.767 [DOI] [PubMed] [Google Scholar]
- 6.Ishida S, Yamazaki K, Shinoda K, et al. Macular hole retinal detachment in highly myopic eyes: ultrastructure of surgically removed epiretinal membrane and clinicopathologic correlation. Retina 2000;20:176–83. 10.1097/00006982-200002000-00011 [DOI] [PubMed] [Google Scholar]
- 7.Ouyang PB, Duan XC, Zhu XH. Diagnosis and treatment of myopic traction maculopathy. Int J Ophthalmol 2012;5:754–8. 10.3980/j.issn.2222-3959.2012.06.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu HY, Zou HD, Liu K, et al. Posterior vitreous cortex contributes to macular hole in highly myopic eyes with retinal detachment. Chin Med J 2011;124:2474–9. [PubMed] [Google Scholar]
- 9.Sepúlveda G, Chang S, Freund KB, et al. Late recurrence of myopic foveoschisis after successful repair with primary vitrectomy and incomplete membrane peeling. Retina 2014;34:1841–7. 10.1097/IAE.0000000000000156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tao YK, Ehlers JP, Toth CA, et al. Intraoperative spectral domain optical coherence tomography for vitreoretinal surgery. Opt Lett 2010;35:3315–7. 10.1364/OL.35.003315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ehlers JP, Kaiser PK, Srivastava SK. Intraoperative optical coherence tomography using the RESCAN 700: preliminary results from the DISCOVER study. Br J Ophthalmol 2014;98:1329–32. 10.1136/bjophthalmol-2014-305294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hahn P, Carrasco-Zevallos O, Cunefare D, et al. Intrasurgical human retinal Imaging with Manual Instrument Tracking using a Microscope-Integrated Spectral-Domain Optical Coherence Tomography Device. Transl Vis Sci Technol 2015;4:1–9. 10.1167/tvst.4.4.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Falkner-Radler CI, Glittenberg C, Gabriel M, et al. Intrasurgical microscope-integrated spectral domain optical coherence tomography-assisted membrane peeling. Retina 2015;35:2100–6. 10.1097/IAE.0000000000000596 [DOI] [PubMed] [Google Scholar]
- 14.Akiba J, Konno S, Yoshida A. Retinal detachment associated with a macular hole in severely myopic eyes. Am J Ophthalmol 1999;128:654–5. 10.1016/S0002-9394(99)00240-8 [DOI] [PubMed] [Google Scholar]
- 15.Gaucher D, Haouchine B, Tadayoni R, et al. Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol 2007;143:455–62. 10.1016/j.ajo.2006.10.053 [DOI] [PubMed] [Google Scholar]
- 16.Morita H, Ideta H, Ito K, et al. Causative factors of retinal detachment in macular holes. Retina 1991;11:281–4. 10.1097/00006982-199111030-00002 [DOI] [PubMed] [Google Scholar]
- 17.Ichibe M, Yoshizawa T, Murakami K, et al. Surgical management of retinal detachment associated with myopic macular hole: anatomic and functional status of the macula. Am J Ophthalmol 2003;136:277–84. 10.1016/S0002-9394(03)00186-7 [DOI] [PubMed] [Google Scholar]
- 18.Uemoto R, Yamamoto S, Tsukahara I, et al. Efficacy of internal limiting membrane removal for retinal detachments resulting from a myopic macular hole. Retina 2004;24:560–6. 10.1097/00006982-200408000-00009 [DOI] [PubMed] [Google Scholar]
- 19.Kwok AK, Lai TY. Internal limiting membrane removal in macular hole surgery for severely myopic eyes: a case-control study. Br J Ophthalmol 2003;87:885–9. 10.1136/bjo.87.7.885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Qi Y, Duan AL, Meng X, et al. Vitrectomy without inner limiting membrane peeling for macular retinoschisis in highly myopic eyes. Retina 2016;36:953–6. 10.1097/IAE.0000000000000826 [DOI] [PubMed] [Google Scholar]
- 21.Lam RF, Lai WW, Cheung BT, et al. Pars plana vitrectomy and perfluoropropane (C3F8) tamponade for retinal detachment due to myopic macular hole: a prognostic factor analysis. Am J Ophthalmol 2006;142:938–44. 10.1016/j.ajo.2006.07.056 [DOI] [PubMed] [Google Scholar]
- 22.Scholda C, Egger SF. Silicone oil tamponade in eyes with posterior staphyloma and retinal detachment caused by macular hole. Acta Ophthalmol Scand 1998;76:704–6. 10.1034/j.1600-0420.1998.760615.x [DOI] [PubMed] [Google Scholar]
- 23.Ando F, Ohba N, Touura K, et al. Anatomical and visual outcomes after episcleral macular buckling compared with those after pars plana vitrectomy for retinal detachment caused by macular hole in highly myopic eyes. Retina 2007;27:37–44. 10.1097/01.iae.0000256660.48993.9e [DOI] [PubMed] [Google Scholar]
- 24.Fujikawa M, Kawamura H, Kakinoki M, et al. Scleral imbrication combined with vitrectomy and gas tamponade for refractory macular hole retinal detachment associated with high myopia. Retina 2014;34:2451–7. 10.1097/IAE.0000000000000246 [DOI] [PubMed] [Google Scholar]
- 25.Chen FT, Yeh PT, Lin CP, et al. Intravitreal gas injection for macular hole with localized retinal detachment in highly myopic patients. Acta Ophthalmol 2011;89:172–8. 10.1111/j.1755-3768.2009.01649.x [DOI] [PubMed] [Google Scholar]
- 26.Chen SN, Yang CM. Inverted internal limiting membrane insertion for macular Hole-Associated retinal detachment in high Myopia. Am J Ophthalmol 2016;162:99–106. 10.1016/j.ajo.2015.11.013 [DOI] [PubMed] [Google Scholar]
- 27.Philippakis E, Couturier A, Gaucher D, et al. Posterior vitreous detachment in highly myopic eyes undergoing vitrectomy. Retina 2016;36:1070–5. 10.1097/IAE.0000000000000857 [DOI] [PubMed] [Google Scholar]
- 28.Pfau M, Michels S, Binder S, et al. Clinical experience with the First commercially available intraoperative Optical Coherence Tomography System. Ophthalmic Surg Lasers Imaging Retina 2015;46:1001–8. 10.3928/23258160-20151027-03 [DOI] [PubMed] [Google Scholar]