Abstract
Background
Influenza vaccinations are commonly administered and effectively prevent influenza. Most vaccine reactions are mild and self-limiting with few reported cases of vasculitis. We present a case of vasculitis post-vaccination unique for its dramatic visual presentation and rapid response to treatment with the aim to emphasise possible causation and timely treatment.
Case presentation
This is a case of a 60-year-old man with chronic idiopathic pulmonary fibrosis, with fever, arthralgias and rash characterised by extensive erythematous plaques on his limbs and trunk 5 days after influenza vaccination. Skin biopsy revealed leucocytoclastic vasculitis. Rash and symptoms resolved 10 days after initiating treatment with oral prednisone.
Conclusions
Influenza vaccines can potentially precipitate cutaneous vasculitis, and timely treatment reduces morbidity in the elderly.
Keywords: Immunological Products And Vaccines, Vasculitis
Background
Annual influenza vaccinations are the most important way to prevent seasonal influenza and are commonly administered to the North American population with increasing uptake.1–7 Influenza can cause serious mortality and morbidity in the elderly (persons aged 65 years and older) and those with complex medical illness.1 Most reactions to the vaccination are mild and self-limiting. Several cases of vasculitis post-influenza vaccination have been reported since 1974. There have been seven reported cases of specifically leucocytoclastic vasculitis, a rare small vessel vasculitis, in the English language literature since 1980, summarised in table 1.3–6 The skin was affected in all cases, and in six of these cases, there was also renal involvement. The novelty of our particular case is the visually dramatic widespread dermal reaction, as well as the rapid response to timely treatment. By reporting this case, we to aim further increase the medical community’s awareness of possibly strong reactions to influenza vaccinations especially in the elderly or those with chronic disease and the importance of timely diagnosis and treatment.
Table 1.
Cases of leucocytoclastic vasculitis following influenza vaccination
| Author | Patient age, sex | Previous vaccine | Organs | Treatment | Recovery time |
| Yanai-Berar et al3 | 63, male | Unknown | Skin, kidneys | Prednisone | 6 weeks |
| Tavadia et al4 | 74, female | Yes | Skin, kidneys | Prednisolone | 10 months |
| 71, female | Yes | Skin, kidneys | Prednisolone | 10 months | |
| 76, female | No | Skin, kidneys | Clobetasol propionate ointment | 2 weeks | |
| 79, female | Yes | Skin, kidneys | Clobetasol propionate ointment | 3 months | |
| Walker et al5 | 64, female | Unknown | Skin | Prednisolone | 3 months |
| Famularo et al6 | 71, male | Unknown | Skin, kidneys | Prednisone | 2 weeks |
Case presentation
A 60-year-old man presented to the emergency room with an extensive rash and fever. Five days prior, he had received his annual influenza vaccine. He had received it previously with no reactions. He developed chills and diffuse joint pain that same evening and a rash with a fever of 39°C next day. During this time, he also reported developing diffuse arthralgias involving his hips, knees and ankles. His medical history included only a 3-year history of idiopathic pulmonary fibrosis (IPF), diagnosed through CT thorax. He had been home oxygen-dependent for 10 months, and his only medication was N-acetylcysteine that he had been taking for 1 year.
On examination, the patient had a temperature of 37.6°C. There were extensive erythematous plaques with petechiae involving the face, trunk, bilateral hands, arms, thighs and feet, along with striking palmar erythaema (figure 1). There were also periungual haemorrhages on the fingers and toes.
Figure 1.
Extensive erythematous urticarial macular rash over the trunk.
Investigations
Blood work showed leucocytosis of 15.8×109/L (4.0–10.0), an elevated C reactive protein of 200 mg/L (normal ≤5.0) and elevated liver enzymes. Work-up was negative for rheumatoid factor, anti-neutrophil cytoplasmic antibodies (ANCA), cryoglobulin and antinuclear antibodies. Serology was negative for acute infection with hepatitis A, B, C, Epstein-Barr virus, cytomegalovirusor parvovirus B19. Further investigations were performed to exclude systemic manifestations. A punch biopsy of the skin of his chest was obtained. Histological examination revealed patchy spongiosis and scattered lymphocytes and neutrophils in the epidermis. In the superficial dermis, there was perivascular mixed inflammatory infiltrate with numerous neutrophils and nuclear debris, features consistent with leucocytoclastic vasculitis (figure 2). The laboratory and histological findings were consistent with a diagnosis of leucocytoclastic vasculitis.
Figure 2.
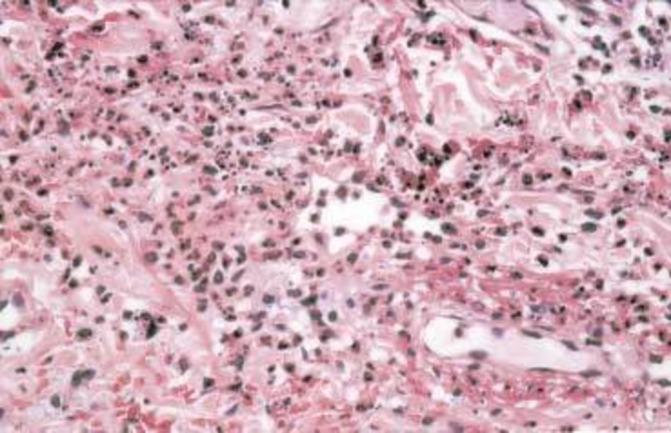
Histological leucocytoclastic vasculitis. Perivascular neutrophilic infiltration of small vessels with inflammatory infiltrate, nuclear dust and extravasation of red cells. Adapted from Tavadia et al.4
Differential diagnosis
Henoch-Schonlein purpura was excluded due to the lack of renal involvement and abdominal pain. His otherwise negative work-up excluded the rest of the differential diagnosis, including ANCA-associated small vessel vasculitides and cryoglobulinaemia, leaving only the possibility of a viral exanthema.
Treatment
The patient was treated with oral prednisone and showed a rapid response. After 2 days in hospital, his rash dramatically improved.
Outcome and follow-up
He was discharged from hospital on prednisone 40 mg daily for 4 days. On follow-up 10 days later, his leucocytosis had resolved, and his skin was dry and beginning to slough.
Discussion
Leucocytoclastic vasculitis is a small vessel vasculitis with an incidence rate of 30 cases per million people per year.1 Histologically, vascular damage is caused by nuclear debris from infiltrating neutrophils. Clinically, the hallmark lesions are erythematous non-blanchable papules known as palpable purpura. Macules, urticaria, ulcers and necrosis may also occur.1 It may be associated with autoimmune diseases or be precipitated by underlying infections, medications, collagen vascular disorders or malignancy.2
This case emphasises the possible temporal association between influenza vaccination and vasculitis in patients with chronic disease. While causation is difficult to ascribe, the association between autoimmune conditions and vaccines has been described, with latency periods ranging from days to years. A possible mechanism for the link is an innate immunity-mediated response to viral antigens or vaccine excipients via molecular mimicry.8 Cutaneous involvement was present in all seven reported cases of leucocytoclastic vasculitis postvaccination, and in six of these cases, there was also renal involvement (table 1).
All cases resolved with a course of corticosteroids, with the fastest recovery time being 2 weeks in two cases and longest being 10 months in two cases.3–6 Our patient possessed a unique case of post-vaccination vasculitis with visually dramatic and widespread dermal reaction. Compared with other reported cases, he responded more rapidly to corticosteroids.
There has only been one described case of acute exacerbation of IPF following H1N1 vaccination of worsening respiratory symptoms, which our patient did not have.9 There have been no described association in the English language literature between IPF and vasculitis in relation to vaccination.
Currently, acute illness is screened for prior to vaccination.7 However, while the influenza vaccine is highly safe and effective, we demonstrate with this case that influenza vaccines can potentially precipitate cutaneous vasculitis and treatment in a timely manner reduces morbidity, particularly in the elderly.
Learning points.
Recognise that while adverse reactions to vaccinations are uncommon, they have potential to precipitate cutaneous vasculitides.
Consider a broad differential diagnosis and provide a definitive diagnosis using biopsies of affected areas.
Provide investigations and treatment in a timely manner to reduce patient morbidity and mortality.
Footnotes
Contributors: All authors contributed to and agreed upon the content in this manuscript. Individual author contributions: SC acquired patient data and case information; also completed literature review, compiled and summarised other relevant case reports and drafted Table 1; drafted the article or revised it critically for important intellectual content; gave final approval of the version to be published after several drafts; and agreed to act as guarantor of the work (ensuring that questions related to any part of the work are appropriately investigated and resolved). DS provided patient data and case information as well as interpretation of findings, revised the article critically for important intellectual content, gave final approval of the version to be published after several drafts and agreed to act as guarantor of the work (ensuring that questions related to any part of the work are appropriately investigated and resolved).
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Zafrir Y, Agmon-Levin N, Shoenfeld Y. Post-influenza vaccination vasculitides: a possible new entity. J Clin Rheumatol 2009;15:269–70. 10.1097/RHU.0b013e3181b56177 [DOI] [PubMed] [Google Scholar]
- 2.Fitzpatrick TB, Wolff K. Fitzpatrick's dermatology in general medicine. 7th ed New York: McGraw-Hill Medical, 2008. [Google Scholar]
- 3.Yanai-Berar N, Ben-Itzhak O, Gree J, et al. Influenza vaccination induced leukocytoclastic vasculitis and pauci-immune crescentic glomerulonephritis. Clin Nephrol 2002;58:220–3. 10.5414/CNP58220 [DOI] [PubMed] [Google Scholar]
- 4.Tavadia S, Drummond A, Evans CD, et al. Leucocytoclastic vasculitis and influenza vaccination. Clin Exp Dermatol 2003;28:154–6. 10.1046/j.1365-2230.2003.01188.x [DOI] [PubMed] [Google Scholar]
- 5.Walker SL, Swindells KJ, Chalmers RJ. Leucocytoclastic vasculitis and influenza immunization. Clin Exp Dermatol 2004;29:95–6. 10.1111/j.1365-2230.2004.01430.x [DOI] [PubMed] [Google Scholar]
- 6.Famularo G, Nicotra GC, Minisola G, et al. Leukocytoclastic vasculitis after influenza vaccination. J Clin Rheumatol 2006;12:48–50. 10.1097/01.rhu.0000200341.38947.43 [DOI] [PubMed] [Google Scholar]
- 7.Grohskopf LA, Sokolow LZ, Olsen SJ, et al. Prevention and control of influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices, United States, 2015-16 Influenza Season. MMWR Morb Mortal Wkly Rep 2015;64:818–25. 10.15585/mmwr.mm6430a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Agmon-Levin N, Paz Z, Israeli E, et al. Vaccines and autoimmunity. Nat Rev Rheumatol 2009;5:648–52. 10.1038/nrrheum.2009.196 [DOI] [PubMed] [Google Scholar]
- 9.Umeda Y, Morikawa M, Anzai M, et al. Acute exacerbation of idiopathic pulmonary fibrosis after pandemic influenza A (H1N1) vaccination. Intern Med 2010;49:2333–6. 10.2169/internalmedicine.49.3890 [DOI] [PubMed] [Google Scholar]



