Abstract
A previously healthy 48-year-old man presented with a 1-week history of migrating polyarthropathy preceded by a viral illness, dysuria and bilateral red eyes. Ocular examination revealed anterior and interstitial stromal keratitis. He was systemically well but had raised erythrocyte sedimentation rate and C reactive protein and was positive for human leucocyte antigen B27 on extensive infective, rheumatological and autoimmune investigations. Although the exact triggering pathogen was not identified, clinical findings were consistent with reactive arthritis. Bilateral interstitial keratitis is a rare manifestation of reactive arthritis which, along with the anterior stromal keratitis, responded well to topical prednisolone sodium phosphate 0.5%. Systemic joint symptoms improved on oral sulfasalazine, non-steroid anti-inflammatory agent and low-dose prednisolone.
Keywords: ophthalmology, rheumatology
Background
Bilateral ocular inflammation of any form in the context of multiple-joint inflammation and additional systemic involvement warrants multidisciplinary assessment and thorough investigations to exclude an underlying infective, rheumatological or autoimmune condition.
This case highlights a rare ocular association with reactive arthritis. Bilateral interstitial and anterior stromal keratitis in a patient with reactive arthritis was successfully treated with topical steroid therapy, after exclusion of other associated systemic conditions which may cause this keratitis subtype.
Case presentation
A previously healthy 48-year-old Caucasian man who has been working in Indonesia presented with a 1-week history of migrating polyarthropathy and bilateral painful red eyes, worse on the right. He experienced dysuria 6 weeks prior to presentation which spontaneously resolved after a few days, followed by flu-like symptoms 1 month ago with dry cough and oral ulcers, which also self-resolved. He had previously experienced a sore red right eye initially 2 months ago which was diagnosed as conjunctivitis. Similar symptoms recurred 1 month ago. On both the occasions, the symptoms resolved with topical antibiotic and steroid.
On general examination, he appeared systemically well but had swollen and tender ankles, wrists and fingers (figure 1). Ophthalmic examination showed reduced visual acuity in the right eye (6/18) compared with the left eye (6/6). Corneal sensation was reduced bilaterally. Slit-lamp examination initially showed multiple dendriform epithelial lesions and mild conjunctivitis, worse on the right. Dilated fundus examination was unremarkable. The patient was treated with oral valaciclovir for presumed herpetic keratitis, given a history of facial (lips) and genital herpes simplex infection.
Figure 1.

Patient with swollen joints in fingers and hand (left greater than right).
However, on review 3 days later, visual acuity had reduced to R 6/24 and L 6/60. Slit-lamp examination now showed bilateral focal anterior stromal infiltrates (figure 2) and diffuse interstitial (intrastromal) keratitis (figure 3), in addition to epithelial oedema on the left. The anterior chambers remained quiet.
Figure 2.
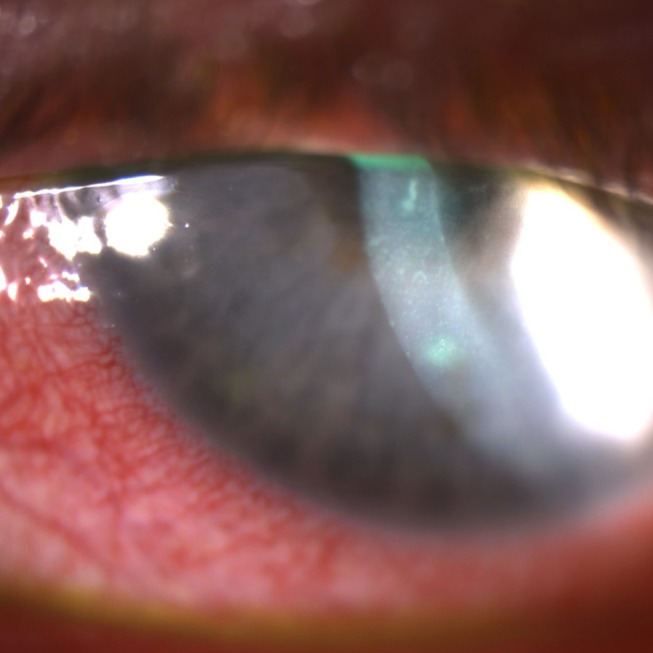
Focal anterior corneal stromal infiltrates (right eye). Similar appearance was seen in the left eye.
Figure 3.

Diffuse interstitial corneal stromal infiltrates (right eye). Similar appearance was seen in the left eye.
Investigations
An extensive autoimmune and infective screen including urine microscopy and cultures/PCR for sexually transmitted infections and HIV, hepatitis B/C, syphilis, cytomegaloviral and Epstein-Barr viral serology, ACE and rheumatoid factor was unremarkable except for raised erythrocyte sedimentation rate (ESR) 95, C reactive protein (CRP) 131 and positive human leucocyte antigen (HLA)-B27. Testing was negative for HLA-B51.
Viral PCR eye swabs were negative for herpes simplex virus (HSV) and chlamydia.
Chest X-ray showed changes suggestive of lower respiratory tract infection, which resolved on repeat imaging without treatment, as the patient was asymptomatic.
Differential diagnosis
Differential diagnoses included:
reactive arthritis
seronegative rheumatoid arthritis
Behçet’s disease
syphilis
herpetic keratoconjunctivitis
sarcoidosis
The bilaterality of the presentation, negative HSV PCR swabs and appearance of the anterior and interstitial keratitis were not typical of herpetic keratitis, corresponding to the lack of clinical response despite systemic antiviral treatment. After assessment by infectious diseases and rheumatology physicians, the patient was diagnosed with reactive arthritis, although no specific pathogen triggering the condition could be detected in this case. Sarcoidosis and Behçet’s disease were also excluded after thorough clinical assessment and systemic investigations.
Treatment
The stromal keratitis was treated with topical prednisolone sodium phosphate 0.5% four times per day in both the eyes with the aim to prevent corneal neovascularisation and scarring. Systemically, valaciclovir was ceased, and the patient was started on naproxen 500 mg two times per day and enteric-coated sulfasalazine 500 mg daily, which was increased to 500 mg two times per day after 1 week. He was also started on low-dose oral prednisolone for ongoing joint pain and swelling, while awaiting sulfasalazine to take effect.
Outcome and follow-up
After 2 weeks of topical steroid therapy, the stromal keratitis was noted to be nearly resolved in the right but mild corneal haze remained in the left eye.
Due to a mild increase in the intraocular pressure from baseline, likely secondary to topical steroids, he was advised to wean off prednisolone sodium phosphate 0.5% over the next 6 weeks with addition of topical diclofenac 0.1% three times per day.
Joint pain and swelling in the wrists improved 1 week after additionally taking oral prednisolone (10 mg) daily, which was to be weaned over 2 months. He was advised to seek ongoing ophthalmology and rheumatology follow-up on return home to the UK.
Discussion
Reactive arthritis, formerly Reiter’s syndrome, is a rare autoimmune seronegative spondyloarthropathy which typically develops following an infection of the gastrointestinal or genitourinary system a few weeks prior.1 However, it may be triggered by other pathogens associated with respiratory tract and other infections.1 Reactive arthritis is more common in young adult males.1
While the classic triad of urethritis, conjunctivitis and arthritis is found in a third of patients,1 other findings may manifest in the eye, genitourinary system and elsewhere, including the kidney and heart.1 Interestingly, mucocutaneous lesions are present in up to 50% of the patients.1 This was experienced by our patient in the form of oral ulceration. Similar to a previous case of reactive arthritis associated with concurrent keratitis,2 ESR and CRP in this case were elevated. A retrospective study previously found 85% of patients with reactive arthritis to be HLA-B27-positive,3 as was the case here. This supports the multifactorial aetiology of the condition where a host—pathogen interaction occurs, leading to an immune response at the affected sites.1
While conjunctivitis, uveitis and scleritis are more common ocular occurrences during first episode of reactive arthritis, keratitis affecting various layers of the cornea is rare3 and more commonly occurs in patients with chronic Reiter’s syndrome.3
Collins et al4 treated a patient with an established history of reactive arthritis and bilateral anterior stromal keratitis involving the epithelial and subepithelial layers with topical prednisolone acetate, which resolved after 3 weeks. Similarly, Rowson and Dart5 described a case of bilateral anterior stromal keratitis with epithelial defect which improved within 1 month on topical prednisolone, without any residual scarring. Self-limiting conjunctivitis reportedly preceded the keratitis.5
Disciform keratitis associated with reactive arthritis has additionally been observed during the first presentation of reactive arthritis,2 where the endothelium and deep stroma were affected. In that case, diminished corneal sensation was also elicited which initially suggested a viral disciform keratitis.2 However, the condition did not improve on topical and systemic antiviral therapy. The patient was subsequently prescribed topical and oral prednisolone and sulfasalazine, which completely treated the keratitis except for a small non-visually significant scar in one eye.
Unilateral interstitial (mid-stromal) keratitis, followed by deep stromal keratitis and anterior uveitis, was reported by Cass6 in a patient recently diagnosed with reactive arthritis. Other causes of interstitial keratitis which need to be excluded include syphilis (common prior to availability of treatment), herpetic and other viral infections, tuberculosis, sarcoidosis and Cogan syndrome.7
A bilateral case of conjunctivitis epithelial and subepithelial opacities, followed by foci of central punctate stromal keratitis, has previously been reported in a reactive arthritis patient.8 Mark and McCulley9 have also cited prodromal conjunctivitis, subepithelial and anterior stromal infiltrates in two patients with Reiter’s syndrome. However, to our knowledge, this is the first documented case of bilateral diffuse interstitial keratitis presenting in combination with anterior stromal infiltrates, preceded by consecutive conjunctivitis and epithelial involvement, during an initial episode of reactive arthritis. There was a rapid response to topical steroid therapy with gradual dose reduction to prevent corneal stromal neovascularisation and scarring. Systemic joint symptoms also improved on oral anti-inflammatories, sulfasalazine and low-dose prednisolone.
Learning points.
Bilateral ocular inflammation in the setting of multiple-joint inflammation and/or other system involvement warrants multidisciplinary assessment and thorough investigations to exclude underlying systemic infective, rheumatological or autoimmune condition.
Reactive arthritis is an autoimmune condition triggered by a preceding infection, classically presenting with a triad of seronegative spondyloarthropathy, urethritis and conjunctivitis.
Other systemic and ocular manifestations such as uveitis and scleritis may occur, but keratitis is rare during an initial episode of reactive arthritis.
Topical steroids help prevent vision-threatening stromal neovascularisation and scarring in interstitial keratitis.
Footnotes
Contributors: JW and YEH were involved in the management of and capturing photographs of the patient. YEH prepared the manuscript. JW supervised the writing and editing of the report.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Stavropoulos PG, Soura E, Kanelleas A, et al. Reactive arthritis. J Eur Acad Dermatol Venereol 2015;29:415–24. 10.1111/jdv.12741 [DOI] [PubMed] [Google Scholar]
- 2.Khandgave T, Kulkarni V, Puthran N. Bilateral disciform keratitis: a rare feature of Reiter′s syndrome. Journal of Clinical Ophthalmology and Research 2015;3:102–4. 10.4103/2320-3897.156605 [DOI] [Google Scholar]
- 3.Kiss S, Letko E, Qamruddin S, et al. Long-term progression, prognosis, and treatment of patients with recurrent ocular manifestations of Reiter's syndrome. Ophthalmology 2003;110:1764–9. 10.1016/S0161-6420(03)00620-1 [DOI] [PubMed] [Google Scholar]
- 4.Collins NE, Fitzgerald O, Murphy CC. Clinical image: keratitis in reactive arthritis. Arthritis Rheum 2011;63:2522 10.1002/art.30397 [DOI] [PubMed] [Google Scholar]
- 5.Rowson NJ, Dart JK. Keratitis in Reiter's syndrome. Br J Ophthalmol 1992;76:126 10.1136/bjo.76.2.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cass EE. Interstitial keratitis occurring in a case of Reiter's disease. Br J Ophthalmol 1949;33:454–5. 10.1136/bjo.33.7.454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kanski KJ, Bowling B. Clinical ophthalmology: a systematic approach. 7th edn Edinburgh: Elsevier, 2011. [Google Scholar]
- 8.Mills RP, Kalina RE. Reiter's keratitis. Arch Ophthalmol 1972;87:447–9. 10.1001/archopht.1972.01000020449017 [DOI] [PubMed] [Google Scholar]
- 9.Mark DB, McCulley JB. Reiter's keratitis. Arch Ophthalmol 1982;100:781–4. 10.1001/archopht.1982.01030030785011 [DOI] [PubMed] [Google Scholar]


