Abstract
A 54-year-old man presented with two episodes of dysarthria and left facial droop. Both episodes resolved by the time of examination. MRI of the brain revealed a right frontotemporal, heterogeneously enhancing mass with surrounding vasogenic oedema, suggestive of a high-grade primary brain neoplasm. The patient was administered preoperative 5-aminolevulinic acid hydrochloride (Gliolan), and fluorescence-guided resection of the lesion was undertaken. Cryptococcus gattii infection was diagnosed from the specimen and the patient was given appropriate antifungal treatment. This is the first reported case of Gliolan-mediated fluorescence in a fungal abscess and highlights one of the potential pitfalls in fluorescence-guided surgery.
Keywords: Neurosurgery, Infectious diseases, Drug therapy related to surgery
Background
Exogenous 5-aminolevulinic acid (5-ALA) has been used in fluorescence-guided neurosurgery over the past 15 years in order to improve rates of gross total resection in gliomas.1 Preoperative administration of Gliolan at appropriate dosage causes accumulation of fluorescent protoporphyrin IX (PpIX) in glioma cells without affecting the normal brain tissue.2 In the presence of visible violet, the surgeon can differentiate pink tumour tissue from blue brain tissue. The current Therapeutic Goods Administration in Australia approves Gliolan for use in the resection of glioblastoma multiforme.3 5-ALA is a precursor to PpIX in the porphyrin production pathway, necessary for the production of haem, an important cofactor for growth in all eukaryote cells. Haem biosynthesis in fungi occurs via the same initial pathway as in mammals.4 It is known that exogenous administration of 5-ALA in fungi leads to PpIX-mediated fluorescence.5 Despite this, there have been no previously reported cases of intraoperative fluorescence of fungal abscesses.
Cryptococcus gattii is a rare Australian pathogen responsible for intracerebral infection, which causes significant morbidity and mortality.6 Its presentation can be clinically and radiologically similar to brain neoplasms. In this report, we discuss Gliolan-mediated fluorescence in a fungal abscess and the necessary consideration of this differential in fluorescence-guided neurosurgery.
Case presentation
A 54-year-old man presented with two episodes of dysarthria and left facial droop.
He has no significant comorbidities and does not take any regular medications. He is an ex-smoker with a 20-pack year history and drinks minimal alcohol. He has no recreational drug use. He lives in rural New South Wales, Australia, and often works with timber. He has no known drug allergies.
He presented to a peripheral hospital with episodes of dysarthria and left facial droop. The initial episode lasted 15 min while the second occurred hours later and lasted 30 min. Both episodes were self-limited and prompted presentation to the local hospital. He reported no recent history of headaches, nausea, weight loss or fevers. A similar milder episode had occurred a fortnight prior, but he denied any other neurological symptoms. There were no recent infectious contacts, overseas travel or change in medications.
On initial examination he was afebrile and had no evidence of meningeal irritation. He was oriented to time and place. He had no evidence of speech deficit on examination by the medical team and a speech pathologist. There was a subtle facial droop but no other neurological weakness.
Investigations
His initial CT of the brain revealed right frontotemporal cytotoxic oedema with mild mass effect and an ill-defined area of underlying contrast enhancement. His initial inflammatory markers, biochemistry and peripheral cell count were unremarkable. He was given high-dose corticosteroids and transferred to a tertiary centre for further investigation.
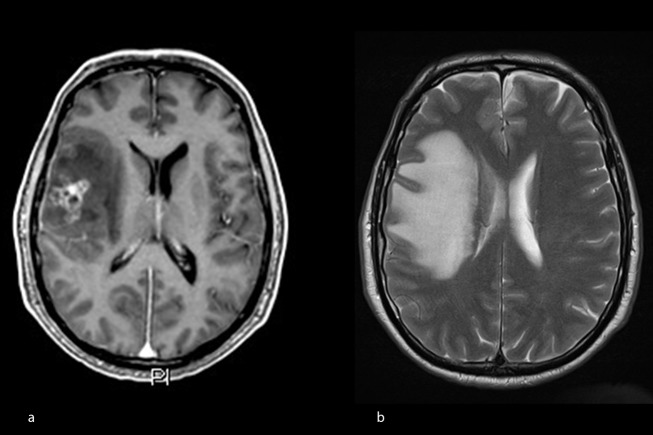
MRI of the brain defined a 19×30×25 mm heterogeneously enhancing mass within the right frontal lobe inferiorly, abutting the operculum. The lesion demonstrated diffusion restriction along its margin, suggesting high cellularity. There were scattered micro haemorrhages within the lesion. It had associated vasogenic oedema (figure 1).
Figure 1.
(A) T1 MRI with gadolinium enhancement shows a heterogeneously enhancing lesion. (B) T2-weighted image demonstrates perilesional vasogenic oedema.
A chest X-ray was performed for preanaesthetic assessment and no significant abnormalities were initially noted. On retrospect, a small right pulmonary opacity was visible.
Differential diagnosis
The working diagnosis was a high-grade primary neoplasm of the brain. A differential diagnosis of metastatic disease was also considered. Fungal abscess was considered much less likely.
Treatment
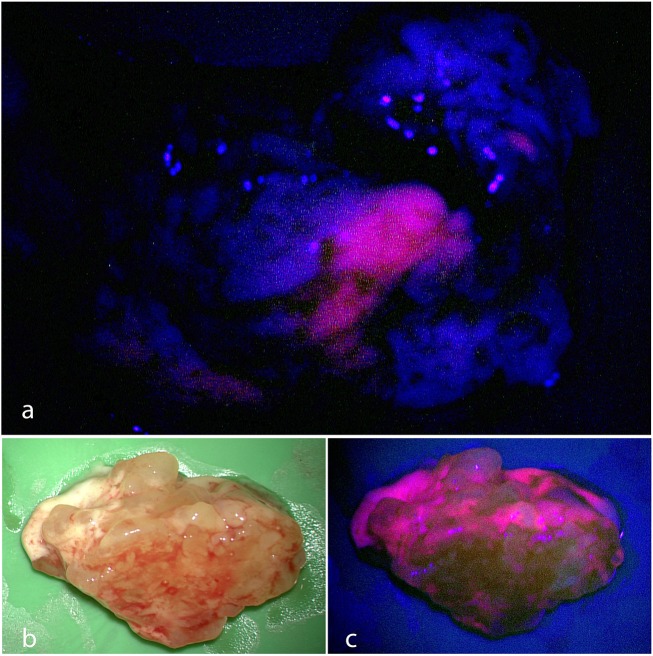
One and a half grams of Gliolan was administered 6 hours prior to a stereotactic right frontotemporal craniotomy. The lesion was resected en bloc with neuronavigation and intraoperative fluorescence (figure 2). Frozen section was consistent with Cryptococcus infection and the patient was given liposomal amphotericin B at 3 mg/kg daily and flucytosine at 2 mg eight-hourly.
Figure 2.
(A) Intraoperative view of cryptococcoma after administration of 5-ALA. Under the presence of blue light, Cryptococcus gattii fluoresces pink, while the normal brain tissue remains blue. Similar to glioblastomas. (B) Excised cryptococcoma under white light. (C) Excised cryptococcoma under blue light. 5-ALA, 5-aminolevulinic acid.
Further microbiological analysis was consistent with C. gattii. A lumbar puncture was carried out 2 days postoperatively. Cerebrospinal fluid white cells were 2×106 per litre, and red cells were 146×106 per litre. Protein was 0.64 g/L. Cryptococcus antigen was negative. A subsequent CT of the chest defined a right pulmonary nodule of 2 cm in diameter consistent with Cryptococcus infection. Formal ophthalmological assessment excluded ocular disease.
The patient received 4 weeks of intravenous liposomal amphotericin B with concurrent 16 days of flucytosine. He has then remained on itraconazole with an expected treatment course of 12 months.
Outcome and follow-up
The patient experienced an episode of acute kidney injury secondary to his antifungal therapy post initial treatment. This improved with intravenous fluid administration and temporary dose adjustment of his antifungal therapy. An MRI of the brain and a chest X-ray were performed 4 months postoperatively. There was no evidence of intracerebral abscesses and the pulmonary nodule was no longer visible. At 9 months since presentation, the patient remains clinically well, with no significant neurological deficit.
Discussion
5-ALA is an amino acid precursor in the synthesis of porphyrin groups, specifically the fluorescent molecule PpIX in eukaryotic cells.1 4 These porphyrin groups are commonly known to form haem groups, which are critical molecules for growth in any mammalian cell. Exogenous 5-ALA has the potential of causing accumulation of PpIX in any rapidly diving cells, including neoplasms and infection.5 Glioblastoma cells tend to show fluorescence 20–50 times more when compared with normal brain cells, allowing for intraoperative identification of tumour margins.1
Fluorescence-guided tumour resection in neurosurgery was first described in the 1940s.7 The use of Gliolan in the resection of gliomas has been present for the last 15 years and has shown increasing rates of gross total resections.1 Although there are varying results with regard to overall survival benefit, the current recommendation is for maximum safe resection.8 A variety of mechanisms are attributed to the higher 5-ALA uptake into cerebral neoplasms. This includes blood–brain barrier disruption, overexpression of membrane transporters, altered metabolism of haem in tumour tissue and increased cell density.1 3
One pitfall of Gliolan is that its fluorescence can be confounded with other unrelated pathologies, including other neoplasms such as metastasis, abscesses and even inflammatory diseases such as multiple sclerosis.2 9 Fluorescence of a cerebral abscess after administration of Gliolan has been described in an infection with Listeria monocytogenes; however, there have been no previously reported cases of fluorescence in C. gattii cerebral infections.10
Similar to mammals, the production of PpIX in fungi is via the same initial haem pathway using 5-ALA and tends to accumulate in the cell membranes of fungi.11 Unlike many other microbial pathogens such as bacteria and viruses, fungi are eukaryotic organisms. The importance of the haem biosynthesis pathway in fungi and its role in virulence is well established.4 12 The use of 5-ALA in photodynamic therapy in fungi is also well studied as a treatment modality.4 13 Despite PpIX fluorescence description in in vitro experiments of C. neoformans,5 this is the first description of a clinical case in which the fluorescence was seen in vivo in a fungal cerebral abscess. The highly elevated metabolic rate of fungi in comparison with normal brain tissue, disruption of the blood–brain barrier and preoperative administration of corticosteroids may be the mechanisms for the relative fluorescence of the fungal abscess in our case.
C. gattii is an intracellular pathogen endemic to Australia, affecting immunosuppressed and immunocompetent hosts.6 14 It enters the body as an inhaled spore and disseminates via the bloodstream, often into the central nervous system causing meningoencephalitis and abscesses. C. gattii infections have a significant morbidity and mortality requiring prompt treatment with antifungals and surgery to manage raised intracranial pressure.6 Imaging findings of fungal cerebral abscesses are often similar to those of neoplasms, including postcontrast peripheral enhancement. Characteristically, fungal abscesses are multiple in number, located within the basal ganglia and may show a ‘dual-rim sign’ on diffusion-weighted imaging.15 None of these characteristic features were present in our patient, stressing how it ought to remain an important differential diagnosis even in light of atypical imaging patterns.
Given the common pathway of synthesis of PpIX in fungi with mammalian cells, it becomes clear that preoperative administration of Gliolan could lead to inadvertent resection of infected brain tissue, which could respond to antimicrobial treatment.
Learning points.
Our case demonstrates fluorescence of Cryptococcus gattii following administration of Gliolan.
The aim of surgical intervention in cerebral abscess is to drain purulent material, decreasing intracranial pressure, while limiting resection of viable brain tissue.
Given the common pathway of synthesis of protoporphyrin IX in fungi with mammalian cells, it becomes clear that preoperative administration of Gliolan could lead to inadvertent resection of infected brain tissue, which could respond to antimicrobial treatment.
Awareness of such an important differential diagnosis for patients with intracerebral lesions and the use of intraoperative frozen section can limit potential iatrogenic neurological deficit.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: WGS wrote and analysed the study and prepared the literature search. MH analysed, edited and finalised the study.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Guyotat J, Pallud J, Armoiry X, et al. 5-Aminolevulinic acid-protoporphyrin IX fluorescence-guided surgery of high-grade gliomas: a systematic review. Adv Tech Stand Neurosurg 2016;43:61–90. 10.1007/978-3-319-21359-0_3 [DOI] [PubMed] [Google Scholar]
- 2. Tonn JC, Stummer W. Fluorescence-guided resection of malignant gliomas using 5-aminolevulinic acid: practical use, risks, and pitfalls. Clin Neurosurg 2008;55:20–6. [PubMed] [Google Scholar]
- 3. Therapeutic Goods Australia. Australian public assessment report for aminolevulinic acid HCl. Woden (AU): Australian Government, Department of Health, 2014:62 https://www.tga.gov.au/sites/default/files/auspar-aminolevulinic-acid-140303.pdf (accessed Apr 2017). [Google Scholar]
- 4. Franken AC, Lokman BC, Ram AF, et al. Heme biosynthesis and its regulation: towards understanding and improvement of heme biosynthesis in filamentous fungi. Appl Microbiol Biotechnol 2011;91:447–60. 10.1007/s00253-011-3391-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kennedy JC, Pottier RH, Reid RL, et al. Photochemotherapeutic method using 5-aminolevulinic acid and other precursors of endogenous porphyrins. US patent 20010021370. 13 Sep 2001.
- 6. Chen SC, Meyer W, Sorrell TC. Cryptococcus gattii infections. Clin Microbiol Rev 2014;27:980–1024. 10.1128/CMR.00126-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Moore GE, Peyton WT, Hubbard TB. The clinical use of sodium fluorescein and radioactive diiodofluorescein in the localization of tumors of the central nervous system. Minn Med 1948;31:1073–6. [PubMed] [Google Scholar]
- 8. Orringer D, Lau D, Khatri S, et al. Extent of resection in patients with glioblastoma: limiting factors, perception of resectability, and effect on survival. J Neurosurg 2012;117:851–9. 10.3171/2012.8.JNS12234 [DOI] [PubMed] [Google Scholar]
- 9. Nestler U, Warter A, Cabre P, et al. A case of late-onset multiple sclerosis mimicking glioblastoma and displaying intraoperative 5-aminolevulinic acid fluorescence. Acta Neurochir 2012;154:899–901. 10.1007/s00701-012-1319-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Voellger B, Klein J, Mawrin C, et al. 5-aminolevulinic acid (5-ALA) fluorescence in infectious disease of the brain. Acta Neurochir 2014;156:1977–8. 10.1007/s00701-014-2169-7 [DOI] [PubMed] [Google Scholar]
- 11. Kosman DJ. Transition metal ion uptake in yeasts and filamentous fungi : Winkelmann G, Winge DR, Metal ions in fungi. New York: Mercel Dekker, 1994:1–38. [Google Scholar]
- 12. Kronstad JW, Hu G, Jung WH. An encapsulation of iron homeostasis and virulence in Cryptococcus neoformans . Trends Microbiol 2013;21:457–65. 10.1016/j.tim.2013.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Calzavara-Pinton P, Rossi MT, Sala R, et al. Photodynamic antifungal chemotherapy. Photochem Photobiol 2012;88:512–22. 10.1111/j.1751-1097.2012.01107.x [DOI] [PubMed] [Google Scholar]
- 14. Ellis DH, Pfeiffer TJ. Natural habitat of Cryptococcus neoformans var. gattii. J Clin Microbiol 1990;28:1642–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gavito-Higuera J, Mullins CB, Ramos-Duran L, et al. Fungal infections of the central nervous system: a pictorial review. J Clin Imaging Sci 2016;6:24 10.4103/2156-7514.184244 [DOI] [PMC free article] [PubMed] [Google Scholar]