Abstract
Hydroxychloroquine is an oral antimalarial medication commonly used off-label for a variety of rheumatological conditions, including systemic lupus erythematosus, rheumatoid arthritis, Sjögren’s syndrome and dermatomyositis. We present a case of a 64-year-old woman who presented with acute onset headache, bilateral tinnitus, and left-sided facial numbness and tingling in the setting of accidentally overdosing on hydroxychloroquine. By the next morning, the patient began to experience worsening in the tingling sensation and it eventually spread to her left arm, thigh and distal extremities. The patient also complained of new onset blurring of her peripheral vision and feeling ‘off balance.’ Despite a complete neurological and ophthalmological work-up with unremarkable imaging and blood work, the patient has had no improvement in her tinnitus, left-sided paresthesias, visual disturbance or ataxia. This is a unique case of hydroxychloroquine overdose resulting in permanent neurotoxic vestibulopathy.
Keywords: Emergency medicine, Sjogren's syndrome, Neurological injury, Rheumatology
Background
Hydroxychloroquine is an antimalarial and anti-inflammatory medication that was originally derived from the β hydroxylation of chloroquine in 1946 with the aim of producing a less-toxic sister compound.1 2 Increasingly prescribed for the management of a variety of autoimmune and rheumatological disorders, such as systemic lupus erythematosus, rheumatoid arthritis, Sjögren’s syndrome and dermatomyositis, hydroxychloroquine is often considered first-line treatment by rheumatologists and dermatologists. Currently, when dosed appropriately using actual body weight, the main significant long-term risk is retinopathy. Updated 2016 guidelines from the American Academy of Ophthalmology on screening for hydroxychloroquine retinopathy recommend a baseline fundoscopic examination followed by annual screening after 5 years with visual fields and optical coherence tomography in patients without elevated risk factors.3 Despite a good safety profile and minimal side effects, hydroxychloroquine can be toxic and even fatal when taken in excess.
Although the incidence of hydroxychloroquine overdose is relatively rare, several case reports have demonstrated the potential for this medication to be acutely life threatening.1 4 Most of our current understanding of toxicity and management of hydroxychloroquine overdose stems from comprehensive experience with poisoning from the parent compound, chloroquine.5 Due to infrequent reporting and lack of data, there is no established lethal or toxic dose of hydroxychloroquine in humans.6 A review of the literature demonstrates a wide range of outcomes with varying doses of hydroxychloroquine overdose, documenting the death of a patient after the ingestion of as little as 5 g and the survival of a patient after the intake of over 20 g.1 The consumption of more than 4 g of hydroxychloroquine is generally accepted as a severe intoxication based on the onset of hypotension or fatal ventricular arrhythmias in 10 of 11 cases.4 6–8 Mortality from hydroxychloroquine overdose is primarily due to its cardiotoxic effects, resulting in a triad of intractable hypotension, life-threatening arrhythmias and hypokalaemia-induced conduction abnormalities.5 The lethal impact on the cardiovascular system has been heavily emphasised with minimal evidence for central nervous system abnormalities.1
Chloroquine poisoning, on the other hand, is well understood due to its widespread use in parts of Asia, Africa and Europe for inducing abortion and attempting suicide.6 9 Animal studies have shown the toxicity profile of chloroquine to be approximately two to three times that of hydroxychloroquine.7 Moreover, fatality rates for chloroquine overdose are significantly higher, ranging from 10% to 30% but reported as high as 90%.6 In the paediatric population, the mortality rate is 80% and many suffer from neurological sequelae.10 While cardiotoxicity is still the main cause of death, chloroquine is associated with the development of seizures, visual disturbance, dizziness and other neurological abnormalities.6 There is no documentation in the literature of such findings in hydroxychloroquine overdose.
Given that much of our understanding of hydroxychloroquine toxicity is quite limited and arises from experience with its molecular predecessor, chloroquine, the full range of side effects from hydroxychloroquine poisoning is still poorly understood. Here, we present a case of a 64-year-old woman who inadvertently overdosed on hydroxychloroquine and developed a neurotoxic vestibulopathy presenting as chronic ataxia, tinnitus, paresthesias and visual disturbance.
Case presentation
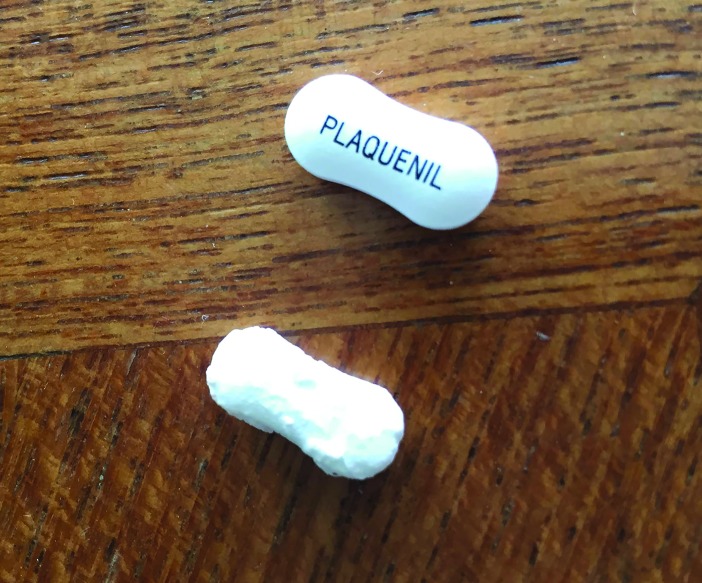
A 64-year-old woman with a history of Sjögren’s syndrome, gastro-oesophageal reflux, hypertension, hyperlipidaemia and nail psoriasis presents with a month of persistent neurological complaints in the setting of accidentally overdosing on her hydroxychloroquine medication. The patient keeps her daily medications (aspirin, Crestor, Plaquenil and Lisinopril) in a four-compartment pill box. Each individual section contains 18–20 pills and she refilled her Plaquenil compartment in the morning of the overdose with 200 mg tablets (figure 1). The patient was sipping an open-top beverage from a straw while driving and accidentally knocked her pill box into her drink when rummaging in her purse. Two compartments, those containing the Plaquenil and Crestor, were fully submerged and soaked for 1 hour before she finished the drink (figure 2). The water soaked through the outer coating of the Plaquenil pills and most dissolved, leaving only 10 half-size fragments behind (figure 3). Many of the Crestor pills remained intact. The estimated ingested dose of hydroxychloroquine was 3 g, since 10 pills completely dissolved and 10 pills were half-dissolved. She stopped all of her medications after the ingestion.
Figure 1.
Image of filled pill box compartments prior to submersion in water.
Figure 2.
Image of pill box compartments after falling into water and soaking for an hour.
Figure 3.
Image of normal Plaquenil pill on top compared with partially dissolved pill on the bottom.
Later that same day, the patient began to experience ringing in her ears, a bad headache, and facial numbness and ‘tingling’ below her left eye. She went to bed and woke up the following morning with a diminished headache but continued tinnitus and spread of the numbness and ‘tingling’ sensation to her left tongue, arm, thigh, foot and toes. She also described a newfound sense of feeling ‘off balance’ and paroxysmal ‘fluttering’ in her peripheral vision, but visual acuity was intact. Complete ophthalmological evaluation, including assessment of visual fields, visual acuity and optic nerve function, was normal. The patient also received a full work-up from her primary care doctor and neurologist with an unremarkable physical examination, blood work and imaging notable for negative Lyme serology, normal MRI of the brain with and without contrast, and magnetic resonance angiography of the head and neck unchanged from baseline.
The patient presented to clinic 2 months after her initial overdose with persistent ringing in her ears, left-sided facial and lower extremity paresthesias, abnormalities in her peripheral vision and sense of postural disequilibrium. Her family history is notable for death of her uncle due to complications of systemic lupus erythematosus and a mother and sister with thyroid disease. Currently, the patient is retired, drinks socially and reports no prior history of tobacco use.
Investigations
None.
Differential diagnosis
A woman in her 60s with a history of Sjögren’s syndrome, hypertension, and hyperlipidaemia and a family history of autoimmune disease who presents with acute onset headache, tinnitus, unilateral facial and distal extremity paresthesias, ataxia and visual disturbance in the setting of medication overdose may have a stroke, Lyme infection, demyelinating disease, migraine, underlying vasculitis or neurotoxicity from the medication. Negative Lyme serology, unremarkable neurological examination, and normal brain MRI and MRA of the head and neck exclude ischaemia, demyelination, infection and vascular inflammation.
Treatment
None.
Outcome and follow-up
The patient is now 12 weeks out from the original overdose episode and has had only mild improvement in her neurological symptoms. Stress and fatigue exacerbate her symptoms.
Discussion
Given the patient’s persistent constellation of neurological symptoms and negative diagnostic work-up in the setting of a hydroxychloroquine overdose, she has experienced hydroxychloroquine-induced neurotoxic vestibulopathy. This phenomenon is well documented in the literature with another antimalarial drug mefloquine, known by the trade name Lariam. Mefloquine, also a member of the drug class quinolines, is a synthetic antimalarial originally developed in the 1970s to treat Plasmodium falciparum malaria resistant to chloroquine in Southeast Asia.11 Mefloquine was first discovered to exhibit neurotoxic properties in 2006 and is known to cause or exacerbate neuropsychiatric conditions.12 In 2013–2014, mefloquine was postulated to induce a chronic toxicity syndrome in the central nervous system due to injury of the neuronal cells of the vestibular system and brainstem.13 14 The symptoms include tinnitus, hearing loss, vertigo, dizziness, headache, paresthesias, neuropathy and disrupted balance and are usually irreversible due to the poor regenerative potential of the nervous system.11 This collection of symptoms best characterises a neurotoxic vestibulopathy, which results from the neurotoxic potential of quinoline antimalarial drugs to accumulate in the neuronal cells of the vestibular nuclei, brain and brainstem.12 14 15 Although the majority of literature on antimalarial toxicity focuses on the slowly evolving retinal damage from hydroxychloroquine and chloroquine, animal studies also demonstrate the potential for intoxication to cause broad neuronal damage which could involve vestibular cells and other neurons.16 Unfortunately, due to the microscopic nature of cellular injury, the diagnosis can only be confirmed by pathological examination on autopsy.
This is the first documented case in the literature of hydroxychloroquine overdose resulting in a neurotoxic vestibulopathy. Due to the life-threatening nature of hydroxychloroquine overdose, it is important to review the appropriate steps in management. First, a patient should immediately report to the nearest emergency department for a full evaluation. The cornerstone of treatment for hydroxychloroquine overdose includes close cardiac monitoring for stabilisation and evaluation of arrhythmias, haemodynamic support for potential hypotension and myocardial depression, electrolyte balance in the setting of hypokalaemia, and gastric decontamination with activated charcoal and lavage if presenting within the first hour of overdose.17 Furthermore, recent literature also supports the life-saving benefit of intravenous lipid emulsion to block cardiotoxicity in hydroxychloroquine poisoning.18
Learning points.
Hydroxychloroquine, a quinoline antimalarial drug, has the potential to produce permanent symptoms of neurotoxic vestibulopathy including tinnitus, headache, dizziness, vertigo, disequilibrium, paresthesias, ocular disturbance and neuropathy.
The mechanism of hydroxychloroquine-induced neurotoxicity is thought to be similar to that of mefloquine, involving the toxic accumulation in the neuronal cells of the vestibular nuclei and brainstem.
First-line treatment for hydroxychloroquine overdose involves an immediate visit to the nearest emergency department followed by early gastric decontamination, haemodynamic support, cardiac monitoring, arrhythmia evaluation, electrolyte repletion and potentially intravenous lipid emulsion to avoid fatal cardiovascular complications.
Footnotes
Contributors: PBC was responsible for conduct and drafting the article. VW was responsible for critical revision and final approval of the version to be submitted for publication. Both authors were involved in the original conception and planning of the case report
Funding: This study was supported in part by NIH R21 AR066286, and Pfizer Corporation. We are indebted to the Department of Veterans Affairs Veterans Health Administration, Office of Research and Development, Biomedical Laboratory Research and Development. Funding/Sponsor was not involved. This study’s contents are solely the responsibility of the authors and do not necessarily represent the official view of NIH.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Yanturali S, Aksay E, Demir OF, et al. Massive hydroxychloroquine overdose. Acta Anaesthesiol Scand 2004;48:379–81. 10.1111/j.0001-5172.2004.0302.x [DOI] [PubMed] [Google Scholar]
- 2. Ling Ngan Wong A, Tsz Fung Cheung I, Graham CA. Hydroxychloroquine overdose: case report and recommendations for management. Eur J Emerg Med 2008;15:16–18. 10.1097/MEJ.0b013e3280adcb56 [DOI] [PubMed] [Google Scholar]
- 3. Marmor MF, Kellner U, Lai TY, et al. Recommendations on screening for chloroquine and hydroxychloroquine retinopathy (2016 revision). Ophthalmology 2016;123:1386–94. 10.1016/j.ophtha.2016.01.058 [DOI] [PubMed] [Google Scholar]
- 4. Isbister GK, Dawson A, Whyte IM. Hydroxychloroquine overdose: a prospective case series. Am J Emerg Med 2002;20:377–8. 10.1053/ajem.2002.33775 [DOI] [PubMed] [Google Scholar]
- 5. Gunja N, Roberts D, McCoubrie D, et al. Survival after massive hydroxychloroquine overdose. Anaesth Intensive Care 2009;37:130–3. [DOI] [PubMed] [Google Scholar]
- 6. Marquardt K, Albertson TE. Treatment of hydroxychloroquine overdose. Am J Emerg Med 2001;19:420–4. 10.1053/ajem.2001.25774 [DOI] [PubMed] [Google Scholar]
- 7. Jordan P, Brookes JG, Nikolic G, et al. Hydroxychloroquine overdose: toxicokinetics and management. J Toxicol Clin Toxicol 1999;37:861–4. 10.1081/CLT-100102466 [DOI] [PubMed] [Google Scholar]
- 8. de Jong-Straková Z, Blaauw AA, van der Linden SJ, et al. A patient with acute hydroxychloroquine poisoning; recommendation for treatment. Ned Tijdschr Geneeskd 1990;134:2445–6. [PubMed] [Google Scholar]
- 9. Ball DE, Tagwireyi D, Nhachi CF. Chloroquine poisoning in Zimbabwe: a toxicoepidemiological study. J Appl Toxicol 2002;22:311–5. 10.1002/jat.864 [DOI] [PubMed] [Google Scholar]
- 10. McCarthy VP, Swabe GL. Chloroquine poisoning in a child. Pediatr Emerg Care 1996;12:207–9. 10.1097/00006565-199606000-00015 [DOI] [PubMed] [Google Scholar]
- 11. McCarthy S. Malaria prevention, mefloquine neurotoxicity, neuropsychiatric illness, and risk-benefit analysis in the Australian defence force. J Parasitol Res 2015;2015:1–23. 10.1155/2015/287651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dow G, Bauman R, Caridha D, et al. Mefloquine induces dose-related neurological effects in a rat model. Antimicrob Agents Chemother 2006;50:1045–53. 10.1128/AAC.50.3.1045-1053.2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ritchie EC, Block J, Nevin RL. Psychiatric side effects of mefloquine: applications to forensic psychiatry. J Am Acad Psychiatry Law 2013;41:224–35. [PubMed] [Google Scholar]
- 14. Nevin RL. Idiosyncratic quinoline central nervous system toxicity: historical insights into the chronic neurological sequelae of mefloquine. Int J Parasitol Drugs Drug Resist 2014;4:118–25. 10.1016/j.ijpddr.2014.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Nevin RL. Limbic encephalopathy and central vestibulopathy caused by mefloquine: a case report. Travel Med Infect Dis 2012;10:144–51. 10.1016/j.tmaid.2012.03.006 [DOI] [PubMed] [Google Scholar]
- 16. Rosenthal AR, Kolb H, Bergsma D, et al. Chloroquine retinopathy in the rhesus monkey. Invest Ophthalmol Vis Sci 1978;17:1158–75. [PubMed] [Google Scholar]
- 17. McBeth PB, Missirlis PI, Brar H, et al. Novel therapies for myocardial irritability following extreme hydroxychloroquine toxicity. Case Rep Emerg Med 2015;2015:1–4. 10.1155/2015/692948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ten Broeke R, Mestrom E, Woo L, et al. Early treatment with intravenous lipid emulsion in a potentially lethal hydroxychloroquine intoxication. Neth J Med 2016;74:210–4. [PubMed] [Google Scholar]