Description
An 85-year-old man presented with orthopnoea and dyspnoea, symptoms of which were suspicious for heart failure. He was in respiratory distress and oxygen saturation was 85% on 4 L oxygen. On initial assessment, lungs were clear and heart sounds were normal. What was immediately evident was a distended abdomen. Digital rectal examination revealed hard faeces in rectum. He had a history of chronic constipation and last bowel movement was over 5 days ago.
Chest X-ray (figure 1) showed raised diaphragms with loops of large bowel interposed between the right hemidiaphragm and liver. An abdominal X-ray (figure 2) confirmed faecal impaction. Brain natriuretic peptide, d-dimer and echocardiogram were normal. He eventually underwent manual evacuation following failure of oral laxatives and enemas (figure 3 for follow-up chest X-ray).
Figure 1.
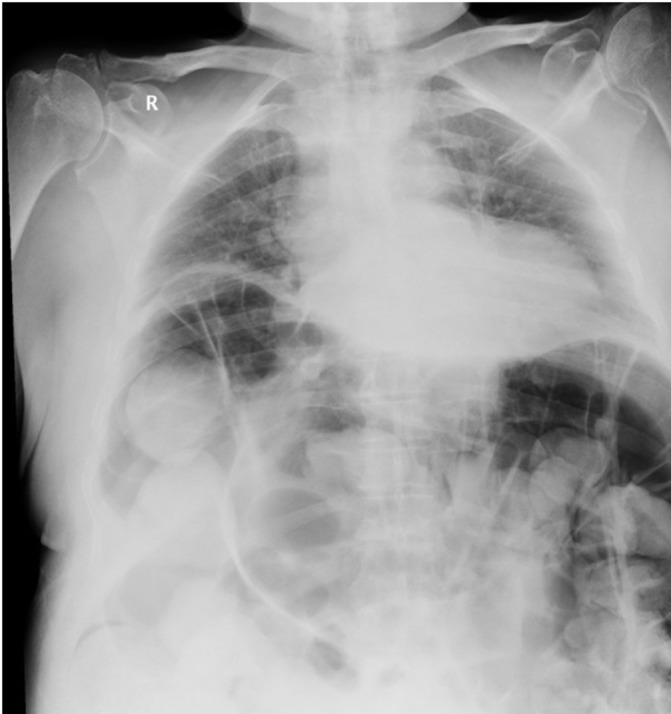
Chest X-ray on presentation showing Chilaiditi sign and lungs compressed.
Figure 2.

Abdominal X-ray on presentation showing faecal impaction.
Figure 3.

Chest X-ray showing improvement after manual evacuation.
This chest X-ray shows Chilaiditi sign (CS), a rare anomaly where bowel lies between the liver and right diaphragm. CS may be congenital or acquired. Chronic constipation is a recognised cause of acquired CS. Other acquired causes are cirrhosis, raised intra-abdominal pressure and diaphragmatic paralysis.1 CS is asymptomatic but when causing symptoms, the term Chilaiditi syndrome is used.1–3 Chilaiditi syndrome is a great mimicker since patients may present with signs and symptoms that imitate various medical and surgical emergencies. Initial chest X-ray showed our patient’s lungs critically compressed by the distended loops of bowel underneath his diaphragms and this was conceivably the cause of his respiratory distress, similar to dyspnoea associated with ascites.
Initial management includes laxatives but surgical intervention may be indicated if bowel obstruction or perforation ensues.1 2
Learning points.
In patients with respiratory distress and incidental Chilaiditi sign, it is important to consider Chilaiditi syndrome as a cause for sudden deterioration as prompt bowel decompression would be paramount.
Though rare, Chilaiditi syndrome may be associated with severe complications if diagnosis is overlooked.
Acknowledgments
The author would like to thank Dr. Paula Hickey (Consultant Geriatrician, Sligo University Hospital, Sligo, Ireland), who oversaw the care of the patient from admission till discharged.
Footnotes
Contributors: JOO: admitting doctor, conception, acquisition of data, write-up of the case, referencing.
Competing interests: None declared.
Patient consent: Obtained from next of kin.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Kang D, Pan AS, Lopez MA, et al. . Acute abdominal pain secondary to chilaiditi syndrome. Case Rep Surg 2013;2013:1–3.doi:10.1155/2013/756590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Moaven O, Hodin RA. Chilaiditi syndrome. Gastroenterol Hepatol 2012;8:276–8. [PMC free article] [PubMed] [Google Scholar]
- 3. Nair N, Takieddine Z, Tariq H. Colonic Interposition between the Liver and Diaphragm: "The Chilaiditi Sign". Can J Gastroenterol Hepatol 2016;2016:1–2.doi:10.1155/2016/2174704 [DOI] [PMC free article] [PubMed] [Google Scholar]


