Abstract
Capillary haemangiomas are relatively common tumours, typically occurring in the subcutaneous tissue during childhood. However, visceral occurrence is very rare. These tumours make up a subset of vascular lesions that have previously, although rarely, been described in case reports in association with the kidney. Here we review the literature and describe a capillary haemangioma occurring in the renal hilum found to be coexistent with end-stage renal disease, renal cell carcinoma and polycythaemia. To our knowledge, this is the first case report to describe the occurrence of this tumour in the renal hilum in association with this constitution of renal pathologies.
Keywords: urological cancer, urological surgery, chronic renal failure, renal intervention
Background
Benign vascular tumours, particularly haemangiomas, are very common occurrences but are very rarely encountered in the kidney. Attesting to their rarity, a case series conducted at Loyola University Medical Center reported only 15 cases between 1999 and 2011 including arteriovenous malformations, capillary haemangiomas, anastomosing haemangiomas, lymphangiomas and a single case of solid intravascular papillary endothelial hyperplasia.1 To date, case reports and small case series have reported approximately 200 renal haemangiomas in total.2 Various subtypes exist including capillary, cavernous and anastomosing.
Capillary haemangiomas are more frequent in childhood and commonly occur in the skin, subcutaneous tissues and mucous membranes. However, occurrences in visceral organs such as the liver, spleen and kidney have also been reported. They are benign lesions and are usually found incidentally on cross-sectional imaging. While patients are generally asymptomatic, symptoms of haematuria, renal colic and hypertension have been reported.3 Tumours can be distinguished histologically based on morphology, identifying an unencapsulated, lobulated collection of thin-walled capillaries, with flat epithelium and minimal connective tissue stroma. Differentiating this benign tumour from a malignancy on radiographic imaging is near impossible.2 3 However, delayed enhancement on contrast CT with an area of lower central attenuation has been shown to correlate with this tumour type.
Case presentation
A 22-year-old man with end-stage renal disease (ESRD) secondary to IgA nephropathy who had been on dialysis since 2012 was found to have polycythaemia with a haematocrit of 59% and elevated erythropoietin level of 22 mIU/mL (normal range 2.6–18.5 mIU/mL). He denied haematuria or flank pain. A contrast enhanced CT scan of the abdomen showed acquired cystic disease of the kidneys. Additionally, it showed a 2.7×1.7 cm peripherally enhancing mass with a central area of hypointensity located within the right renal hilum, which was concerning for possible malignancy (figure 1). The patient underwent an uncomplicated bilateral laparoscopic radical nephrectomy.
Figure 1.
Presurgical CT imaging of capillary haemangioma. (A) Non-contrast axial view of capillary haemangioma (arrow). (B) Axial view with IV contrast in the venous phase showing enhancement of capillary haemangioma suggestive of a vascular mass (arrow). (C) IV contrast venous phase coronal view showing the tumour’s relationship to the renal hilum (arrow). IV, intravenous.
The pathology was significant for diffuse glomerulosclerosis, tubular atrophy, marked hypertensive vasculopathy and chronic interstitial inflammation consistent with known ESRD. Additionally, a 1.4 cm multiloculated cystic renal cell carcinoma (RCC) limited to the renal parenchyma was found in the right kidney. Finally, a 1.5×1×0.8 cm well-circumscribed, dark red homogeneous soft nodule was found in the hilum, 2.5 cm from the vascular margin and 0.5 cm from the renal pelvis which corresponded with the concerning mass on preoperative imaging study. This hilar mass was identified as a capillary haemangioma based on the typical morphological features consisting of a lobulated aggregation of thin-walled capillaries and scant connective tissue (figure 2).
Figure 2.
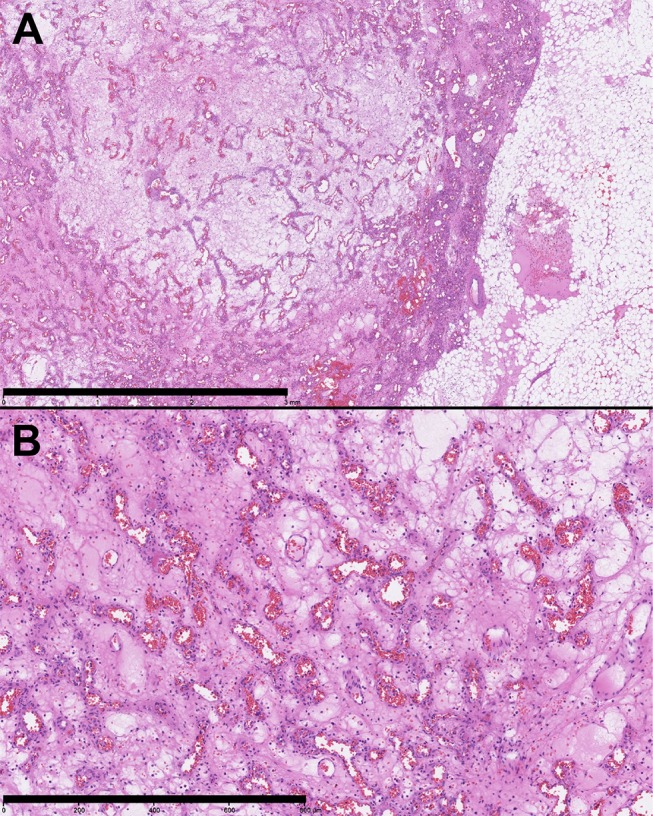
Capillary haemangioma histological images. H&E preparations of capillary haemangioma slices (A) showing the association with the renal hilar fat (scale bar: 3 mm). (B) The morphology of the tumour including lobulated nature and collection of complex vascular spaces surrounded by delicate stoma is consistent with a capillary haemangioma (scale bar: 800 µm).
Discussion
While multiple case reports and case series detail capillary haemangiomas in the kidney, the majority are found in the renal pelvis (48.7%), renal pyramids (42.1%) or the renal cortex (9.2%).1 To our knowledge, only two cases have been reported in the renal hilum. One case from Loyola University noted a 3 cm mass abutting a renal artery and was originally confused for a pseudoaneurysm.3 Another case reported in Hirosaki, Japan, described a hilar 6.4 cm capillary haemangioma with adhesions to the renal vein.4
Similar to our patient, the association of ESRD and renal haemangiomas has been reported. A retrospective study across five institutions reported 23 cases of renal haemangioma. Of these, 16 patients were also diagnosed with ESRD.5 However, the majority of haemangiomas were of a newly described subtype, anastomosing haemangiomas. A capillary haemangioma was found in only one patient. Additionally, the majority of tumours were located in the renal medulla and renal sinus, with none found in the renal hilum.
While haemangiomas are often identified incidentally on imaging or in conjunction with an additional diagnosis, few cases have been reported of the tumour’s association with RCC. In 2012, Mehta et al reported the first case of a capillary haemangioma associated with RCC as part of a benign vascular tumour case series.1 In 2014, three additional cases reporting the association of ESRD, RCC and renal haemangiomas were described in a case series. However, all were of the anastomosing rather than capillary subtype.5
The association between polycythaemia in patients with both renal cysts and RCC has been well recognised. However, only one known case of polycythaemia and renal haemangioma has been described in the literature.2 In this case, a 6–7 cm capillary haemangioma was identified and removed as the cause of the patient’s polycythaemia. Given that our patient was found to have RCC, renal cysts and capillary haemangioma the definitive aetiology of his polycythaemia cannot be determined and was likely multifactorial.
Learning points.
Benign vascular lesions present a clinical challenge, as a presurgical diagnosis is difficult or near impossible to obtain. Additionally, the rarity of these tumours makes it difficult to study presenting features.
The association of capillary haemangioma with end-stage renal disease (ESRD), renal cell carcinoma (RCC) and polycythaemia has previously been described. However, this case represents the first, to our knowledge, of a capillary haemangioma presenting with ESRD, RCC and polycythaemia located in the renal hilum.
As imaging and diagnostic modalities continue to improve, it is important to keep capillary haemangioma in the differential when patients present with similar features.
Footnotes
Contributors: MB contributed to the design, acquisition and contextual analysis of the case. He also participated in the drafting and revision of the manuscript. ML contributed to the design, acquisition and analysis of information. He also participated in the critical revision of the work. SG contributed to the design, acquisition and interpretation of information. He also participated in the critical revision of content. All authors reviewed the final version of the manuscript for accuracy and integrity prior to submission, agreeing to be accountable for the work.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Mehta V, Ananthanarayanan V, Antic T, et al. . Primary benign vascular tumors and tumorlike lesions of the kidney: a clinicopathologic analysis of 15 cases. Virchows Arch 2012;461:669–76. 10.1007/s00428-012-1333-9 [DOI] [PubMed] [Google Scholar]
- 2.Leak BJ, Javidan J, Dagher R. A rare case of renal hemangioma presenting as polycythemia. Urology 2001;57:975 10.1016/S0090-4295(01)00910-4 [DOI] [PubMed] [Google Scholar]
- 3.Vasquez E, Aulivola B, Picken M, et al. . Capillary hemangioma masquerading as a renal artery pseudoaneurysm. Urology 2012;79:987–9. 10.1016/j.urology.2011.12.020 [DOI] [PubMed] [Google Scholar]
- 4.Oikawa M, Hatakeyama S, Hamano I, et al. . Capillary hemangioma in renal hilum; a case report. Hinyokika Kiyo 2014;60:33–7. [PubMed] [Google Scholar]
- 5.Kryvenko ON, Haley SL, Smith SC, et al. . Haemangiomas in kidneys with end-stage renal disease: a novel clinicopathological association. Histopathology 2014;65:309–18. 10.1111/his.12394 [DOI] [PubMed] [Google Scholar]



