Abstract
Rationale
Effective translation of genomics research into practice depends on public acceptance of genomics-related health information.
Objective
To explore how smokers come to accept or reject information about the relationship between genetics and nicotine addiction.
Methods
Thirteen focus groups (N=84) were stratified by education (seven <Bachelor’s degree, six ≥Bachelor’s degree) and race (eight black, five white). Participants viewed a one-minute video describing the discovery of a genetic variant associated with increased risk of nicotine addiction and lung cancer. Next, they provided their opinions about the information. Two coders analyzed the data using grounded theory.
Results
Pre-video knowledge about why people smoke cigarettes and what genetic risk means informed beliefs about the relationship between genes and addiction. These beliefs were not always consistent with biomedical explanations, but formed the context through which participants processed the video’s information. This, in turn, led to information acceptance or skepticism. Participants explained their reactions in terms of the scientific merits of the research and used their existing knowledge and beliefs to explain their acceptance of or skepticism about the information.
Conclusion
Laypeople hold complex understandings of genetics and addiction. However, when lay and biomedical explanations diverge, genetics-related health information may be rejected.
Keywords: Gene-Environment Interaction, Health Communication, Information Processing, Message Rejection, Tobacco Use
Advances in genomics research hold promise for improving clinical outcomes and population health (Green, Dotson, Bowen, Kolor, & Khoury, 2015), although this promise depends on the translation of results into clinical and public health practice. This translation effort requires helping the public understand that health problems tend to be multifactorial—that is, they are caused by a combination of genetic, environmental, and behavioral risk factors (McBride, Birmingham, & Kinney, 2015). For example, certain genetic variants on the nicotinic cholinergic receptor are associated with an increased risk of severe nicotine dependence and an increased risk of lung cancer independent from the risk conferred from severe nicotine dependence (Bierut, 2010). Yet, the high-risk allele cannot be expressed unless the person with the variant uses tobacco.
Two possible strategies for promoting public health by providing information about the multifactorial nature of nicotine addiction and lung cancer are attempting to motivate smokers to quit by informing them that they have a high-risk genotype (Hartz et al., 2015; Smerecnik, Grispen, & Quaak, 2012) and tailoring smoking cessation therapies to genotypes (Marteau et al., 2012). Informing individuals that they have a high-risk variant can increase their lung cancer risk perceptions (Lipkus, Schwartz-Bloom, Kelley, & Pan, 2015; Sanderson et al., 2014; Shepperd et al., 2013), worry (Shepperd et al., 2013), and 30-day cessation (Lipkus et al., 2015). However, systematic reviews, a meta-analysis, and a randomized controlled trial have each questioned the efficacy of using personalized genetic testing to motivate smoking cessation and other health behavior changes (Godino et al., 2016; Hollands et al., 2016; Marteau et al., 2010).
Another consideration is that individuals with limited access to healthcare may lack affordable or convenient access to genomic technologies, thus limiting their exposure to genomic information to mass media news reports and social networks. Because medically underserved populations have lower cessation rates (US Department of Health and Human Services, 2014), translating genomics research findings without considering healthcare access could inadvertently exacerbate health disparities. Relatedly, most genomics research is conducted with samples that are primarily white, highly educated, and motivated to engage in healthy behaviors (McBride et al., 2015). The reach of genomics-related health advances and their consequent health benefits will be limited if we fail to consider the perspectives of socio-demographically diverse groups.
To understand how people understand and act on information about the combined effect of genetic and behavioral risk factors while being cognizant of the likely inaccessibility of genomic testing for medically underserved populations, the present study initially sought to identify gaps in the understanding of genomics research conveyed via the mass media among socio-demographically diverse smokers. One area of concern was that the news media might inadvertently discourage engaging in healthy behaviors because it does not always communicate genetics research findings effectively (Condit, 2007; Donelle, Hoffman-Goetz, & Clarke, 2004; Petersen, 2001). Our conceptual framework asserted that information about the genetic basis of nicotine addiction and lung cancer might produce unfavorable changes in health beliefs and attitudes that can lead to smoking cessation, such as lower perceived harm from smoking and lower quitting self-efficacy (Jeong, 2007; Sanderson et al., 2009; Smerecnik, Mesters, de Vries, & de Vries, 2009). However, it also allowed for the possibility that participants’ interpretations of the information might be influenced by their current beliefs about genes and genetics, by the extent to which they held multifactorial causal beliefs about nicotine addiction and lung cancer, by the extent to which they understood the mechanisms that linked genes to addiction, and by the extent to which genes do or do not determine one’s fate (Bates, Templeton, Achter, Harris, & Condit, 2003; Cameron, Marteau, Brown, Klein, & Sherman, 2012; Condit, 2010, 2011; Condit & Shen, 2011; Wang & Coups, 2010). The results were intended to be used to develop health communications that conveyed these complex concepts in a way that was accurate, clear, meaningful, and useful.
The study methodology was based on the constructivist paradigm, which asserts that a person or group’s reality is based on specific social and individual experiences (Guba & Lincoln, 1994). Critically, these realities are not static and can be refined. This paradigm is consistent with the study’s focus on explicating how individuals understand the relationship between genes and nicotine addiction (Charmaz, 2006), with the study’s goal of improving genetic communication (i.e., “refining realities”), and with the overarching conceptual framework that was used to guide the focus groups.
Halfway through data collection, it became apparent that participants were very skeptical about the validity of the genetics research findings being presented to them. This skepticism was unexpected, and by the end of data collection (using the same interview guide throughout), the research team noted that such widespread skepticism seemed to reduce participants’ receptivity to genetics-related health information. Recognizing that such skepticism might reduce the effectiveness of communication in actual public health and clinical settings, our planned analyses shifted course from identifying better communication strategies to exploring the process by which smokers come to accept or reject information about a genetic basis for nicotine addiction.
Method
Study Overview
Thirteen focus groups (N=84) were conducted in the St. Louis metropolitan area from April to August 2012. Participants stratified by race (African American, White) and educational attainment (<Bachelor’s degree, ≥Bachelor’s degree). Four groups fell within the higher education/African American and lower education/African American strata, two groups within the higher education/White stratum, and three groups in the lower education/White stratum. Assuming six to eight participants per group, we estimated reaching thematic saturation after two to three groups per stratum. We allowed for the possibility that additional groups might be needed. Mean attendance was six participants per group (range three to ten).
Participants
All study materials and procedures were approved by the Washington University in St. Louis Human Research Protection Office. Recruitment occurred in the local community using several methods, including distributing and posting flyers, word of mouth, and a volunteer research participant registry. Individuals were eligible for participation if they were 18 years or older, had smoked at least 100 cigarettes during their lifetimes, currently smoked every or some days of the week, self-identified as African American or White, and attended to the news at least once in the previous week. Participants could not consider themselves a genetics expert but needed to have basic knowledge of the terms “gene” or “genetic” (e.g., “passed down”, “where you get your traits from”). This requirement was because the initial study goal of examining how smokers conceptualize the idea that there is a genetic basis for nicotine addiction was predicated on participants having at least some idea of what the word “gene” meant. We were also concerned that including individuals with no knowledge of genetics would marginalize them relative to other participants and would limit the extent to which they could participate meaningfully in a discussion about genetics.
Procedure
Participants provided written informed consent and verified their demographic and tobacco history information. After introductions, the facilitators asked participants why they thought people smoke and what they thought the terms genes and genetics meant. Then, the terms genes and genetics were briefly explained in lay terms to so the conversation could proceed with all participants having a minimum level of common understanding. Participants were asked to convey their beliefs about the role of genetics in the etiology of chronic health conditions and in cigarette smoking. Next, they viewed a one-minute Associated Press video clip that described the discovery of a genetic variant associated with severe nicotine addiction and an increased risk of lung cancer (http://youtu.be/sO3×8xBr8YQ). The video cited a geneticist who described the variant as a “double-whammy gene” because it has dual negative effects (i.e., a “whammy”): one effect maintains addiction and one effect increases lung cancer risk. Last, participants were asked to provide their thoughts about the believability and potential utility of the information presented in the video. Groups lasted 60–90 minutes and were audio-recorded. Each participant received a $40 gift card.
Each focus group was led by a facilitator who conducted the group according to an interview guide composed of open ended questions (Appendix 1) and a note-taker, both of whom were race-matched to the group. The questions were crafted to be flexible enough to elicit beliefs related to the concepts identified in prior research that examined genetics beliefs (e.g., Condit, 2010), while allowing the group to convey novel ideas (Charmaz, 2006). If group members did not spontaneously mention a construct of interest, moderators probed for it. To reduce the risk of bias, the questions and probes targeted the concepts indirectly. For example, to elicit concerns about discrimination, participants were asked whether there were any disadvantages to learning about a genetic link to nicotine addiction. Questions and probes were phrased using informal, non-academic language. The facilitator and note-taker debriefed with one another after each session to summarize main points, relate how the comments from the group related to previous groups, identify unusual events and how they may have affected conversation, and evaluate whether thematic saturation was reached.
Data Analysis
Audio recordings were transcribed, and the accuracy of the transcriptions was verified by the second author. Data were analyzed using a grounded theory approach (Charmaz, 2006) by the first and second authors, with insight from the third author for particularly challenging issues. Codes were identified inductively to identify concepts that emerged spontaneously from participants and deductively for a priori concepts of interest. Data coding and interpretation were iterative. The coders coded the transcripts independently but conferred regularly to identify and resolve discrepancies, prevent drift in the definition of codes, identify themes that arose from groups of codes, and examine areas of potential saturation. Inter-coder agreement was achieved by consensus.
Next, a model was developed to describe the factors contributing to information acceptance or skepticism. Throughout this stage, codes and themes were compared to one another, to the demographic characteristics of the groups, and between pre- and post-video. The first author developed preliminary models describing the findings and refined them based on intensive examination and re-examination of the codes, themes, and their interrelationships. She searched for contradictory examples and presented the preliminary models to the co-authors and a transdisciplinary group of qualitative and quantitative researchers who attended a working group meeting but were unaffiliated with the study. The codes, themes, and interrelationships were re-analyzed based on this feedback, the model was finalized, and the results were again presented to the study co-authors and external experts for review.
To evaluate whether the themes varied by race or educational stratum, the proportion of groups in each stratum in which a given theme emerged was noted and compared to its companion stratum (e.g., a theme that emerged in six of eight African American groups vs. four of six White groups). Because the total number of groups for each stratum was unequal, evaluations of comparability are approximate. NVivo was used to facilitate data analysis.
Information processing occurs extremely quickly and often outside conscious awareness (Chen & Chaiken, 1999; Zajonc, 1980), and people generally cannot provide accurate descriptions of their information processing experiences (Wilson & Schooler, 1991). Thus, we cannot claim to describe the information processing process itself. We can, however, discuss its consequences and illustrate how participants explained their reasons for accepting or rejecting the information. This general process, which did not seem to vary considerably by racial or educational background, is described below.
Results
Preliminary Analyses
Of 84 participants, 44 (52.4%) were men, 52 (61.9%) were African American, and 57 (67.9%) reported having less than a Bachelor’s degree. Their mean age was 42.8 years (SD=12.9 years). Participants were established smokers; 78 (95.9%) smoked daily and 25 (29.8%) smoked at least a pack of cigarettes daily.
Model Summary
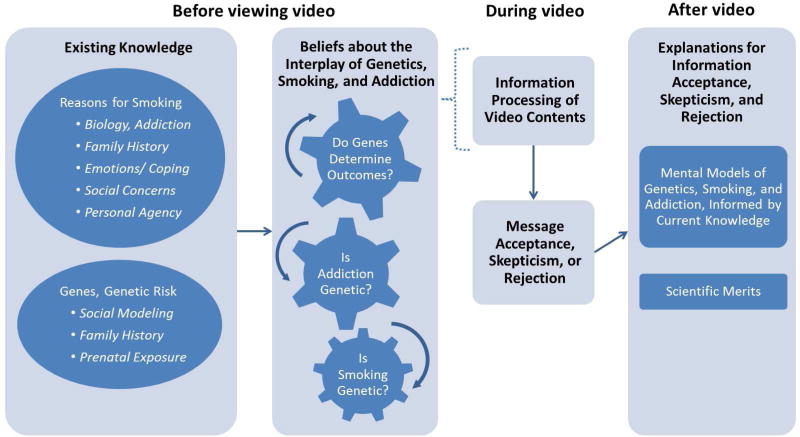
As described in detail below, participants’ explanations for accepting, rejecting, or being skeptical of the news that nicotine addiction has a genetic component were based primarily on their own unique understandings of the mechanisms by which such a relationship might or might not occur (i.e., mental models). Often, these complex understandings were framed as family histories or personal experiences. This strategy seemed to bring meaning to unfamiliar, complex, and abstract ideas. In brief (see Figure 1), it appeared that the knowledge that participants brought with them into the focus groups about (1a) why people smoke cigarettes and (1b) the meaning of the terms genes and genetic risk informed an interacting set of beliefs about (2a) the extent to which genetics determined ones fate, (2b) whether addiction was genetic, and (2c) whether smoking was genetic. The complex interplay among these beliefs formed the context (or mental model) through which participants processed the information in the video. When participants’ mental models diverged from expert mental models, there was the potential for skepticism.
Figure 1. Factors that inform the acceptance or skepticism of genetic health information.
Note. The dashed bracket illustrates that existing knowledge provides a basis for beliefs about genes and addiction, which forms the context through which participants process the information in the video.
“It sound[s] like some BS”: Acceptance and skepticism of genetic health information
Model Details
Pre-video: Existing knowledge
Before viewing the video, participants generally distinguished between reasons for initiating smoking cigarettes and reasons for continuing to smoke. Factors contributing to initiation centered mostly on social influences from peers, family, and society. One white woman with higher education indicated she started smoking “because it was cool at first.” A small number of participants indicated that they initiated smoking because they were “curious.” Continuing to smoke, on the other hand, was influenced by a wider array of factors that included emotional reasons such as being “mad” or “stressed,” biological reasons such as having a “chemical imbalance” or “being addicted to the nicotine,” and social concerns. One African American woman with lower education noted that “everybody is smoking a cigarette, and you’re going to have one too” at parties. Participants in all 13 groups mentioned the importance of personal agency in their continued smoking behavior: “I would say smoking is about choice…you make some good choices and some bad choices” [African American woman with higher education].
Participants demonstrated their existing knowledge about genes using lay terminology such as “passed down” from generation to generation and “you get it from your parents,” as well as formal biomedical terms such as “DNA,” “traits,” “heredity,” and “chromosomes” (not shown in Figure 1). The concept of genetic risk seemed to be multifaceted. In many groups, genetic risk was discussed as family history. One African American woman with lower education explained, “genetic risk would be your grandma, your mom have a situation with [diagnosis of] cancer…because their DNA grows through you and it’s a risk that you might be getting.” People in several groups indicated that that a trait could “skip generations” and affect every 2nd generation, rather than every generation. In one rare interpretation that was mentioned in two groups, social modeling was considered a genetic process because the trait was “passed down.” In the words of one African American man with lower education, “…you grow up and you see your mother and your father smoking, most likely you might end up picking up a cigarette.” Moderator: “Because of genetic risk?” Man: “Yeah.”
In a small number of groups, the idea was mentioned that prenatal exposure to toxins could either alter a fetus’ genes or could give it “a taste” for the substance that could express itself in adolescence or adulthood:
“My mom smoked like two packs a day when she was pregnant with me…both my mom and dad smoked for, I don’t know, maybe about 20 years….And my- my oldest brother who she smoked with when she was pregnant with him he smoked…. So I don’t know. I mean I think that, you know, it does-- I think it’s already in your system. And that, you know, you had it in the womb and you pick it up again and you’re like oh, wow, I remember that.” [White man with lower education].
Pre-video: Beliefs about genes, smoking, and addiction
Beliefs about the extent to which people’s fates are bound by their genes (i.e., genetic determinism) formed the basis for a discussion of the role of genes in health, addiction, and smoking. At least one participant in all groups recognized that having a gene for a chronic health condition did not always mean that the gene would lead to illness. Instead, most indicated that a gene led to an increased “chance,” “likelihood,” or “predisposition” to illness. Furthermore, members of most groups indicated that people who had a gene that placed them at risk of a disease could reduce their risk by engaging in health protective behaviors such as “exercise,” “[eating a healthy] diet,” and “not smoking.” However, the members of several groups discussed genetic risk in terms that described the multifactorial etiology of cancer that combined behavioral control and determinism: “[If] you’ve got the gene [and] you eat the wrong kind of steak one time…that could be what sets the gene in motion to give you cancer” [white man with lower education].
Participants generally agreed that substance addiction has a genetic component. Some participants spontaneously identified specific behaviors that they thought might be genetic (e.g., use of tobacco, alcohol, and illicit drugs, gambling), whereas others believed that genes could predispose someone to have an “addictive personality” that produced addiction to whatever substance they may be exposed. Other participants indicated that addiction to nicotine was simply one way a generalized “addiction gene” could be expressed, but doubted that there was a specific “smoking gene.” In a few cases, having an “addiction gene” or an “addictive personality” was discussed in a deterministic manner. One African American woman with lower education noted, “…I think it is predetermined…if it’s in your genes, it’s in your genes. It doesn’t have to necessarily be that you channel it in to being an alcoholic or you channel it into being a smoker, but I think that if it’s a personality trait that your parent passed down to you—it will be channeled in a different way.” However, in every group, most participants who endorsed the idea of a genetic link to addiction rejected genetic determinism by emphasizing that an individual’s efforts to assert their personal agency can overcome the effects of genetics. This was demonstrated by assertions about smoking being a “choice” and quitting being a matter of “willpower” [the mental and emotional fortitude to persevere at a task]. The belief that addiction could be overcome by personal agency was illustrated by a white man with lower education who noted, “You can have all the genetics of the alcoholic, smoker, weed [marijuana]…whatever…[but] it’s your choice whether you want to continue [using] or not…[genetics] doesn't tell you what to do.”
Post-video: Information acceptance
Immediate responses to the video varied widely. In almost every group, at least one participant indicated believing that the information presented in the video was true: “I think I got the double-whammy [gene]” [white man with lower education]. However, skepticism was widespread. At least one person in each group made statements indicating disbelief (e.g., “It just sound like some B.S. [“bullshit”; scornful tone]” [African American man with lower education]). Other expressions of skepticism were subtle (e.g., “Well, it seems as though they were saying it’s genetic” [African American woman with higher education]).
Post-video: Explanations for information acceptance or skepticism
As shown below, explanations for accepting, rejecting, or being skeptical of the information presented were based on participants’ own unique understandings of the way genetics might or might not be related to nicotine addiction. These understandings were informed by two broad lines of thought: (1) the extent to which the information presented in the study was consistent with their pre-video knowledge and beliefs about smoking, genetics, addiction, and their interaction, and (2) the extent to which participants believed the study had a high degree of scientific merit. Often (but not always), these complex understandings were framed in terms of family histories or personal experiences. This strategy seemed to help bring meaning to unfamiliar, complex, and abstract ideas. Some of the statements participants made to support their assertions echoed those group members mentioned before they viewed the video. Other statements were not explicit echoes, but the way in which they were stated indicated participants’ reliance on beliefs that they brought with them into the focus groups.
Consistency with mental models of genetics, smoking, and addiction
Several participants made statements indicating the extent to which the information was consistent with their mental models of genetics, smoking, and addiction. According to one white woman with lower education, “I believe that it’s genetic to some degree, especially…like if you smoked when you were pregnant…why couldn’t you pass on that gene? You can pass on other things.” This quote demonstrates that participants integrate several concepts, some of which may vary in technical accuracy, to come to a conclusion about the validity of the study. In this case, the participant accurately identified the inheritance of genetic variants through generations, although her belief about the exact mechanism by which this occurs was not entirely correct.
Other participants, however, used discrepancies between their understanding of the relationship between genetics and addiction and the contents of the video to explain their skepticism. For example, a small number of participants rejected the information based on the premise that a “behavior” – particularly a “learned” behavior like smoking – cannot be genetic. More often, skepticism arose because participants’ understandings were based on an incomplete understanding of addiction. For instance, many participants were surprised by the video’s statement that the effects of the genetic variant were unrelated to “the pleasure centers” in the brain. As illustrated by one white man with lower education, “most people say they enjoy smoking and they do it for pleasure. And if you’re addicted to smoking and you’re not doing it for pleasure, why are you doing it?” From this point of view, any explanation for smoking is flawed if it does not account for the pleasurable sensations smoking causes. Yet, this explanation does consider the stimulative nature of nicotine, and that many nicotine withdrawal symptoms are associated with stimulant withdrawal (e.g., decreased attention, increased anxiety). Other participants indicated that the idea of a gene associated with nicotine addiction was “too specific,” but an “addiction gene” that predisposed people to addiction to a variety of addictive substances was possible.
Sometimes the pre-video knowledge that participants used to evaluate the contents of the video was discussed in scientific terms rather than personal experiences. Occasionally, their discussions were inconsistent with current scientific evidence. This discrepancy was often associated with skepticism. One African American man with higher education wondered, “in the history of mankind, we haven’t been smoking cigarettes or tobacco for hundreds of generations. Where did this genetic problem come from?” The statement is consistent with understanding that genes are inherited through a family lineage and being aware of evolutionary concepts. However, it does not account for current scientific thought about how the specific receptors associated with nicotine addiction are used for multiple purposes necessary for human survival, and that nicotine just happens to fit in the same receptor.
Nearly all participants rejected genetic determinism in the context of nicotine addiction. This occurred regardless of whether participants believed the information, and the statements used to reject determinism were consistent with many statements made before they saw the video. Sometimes it was framed in terms of a reaction against a perceived trend in society of rejecting the role of personal agency and responsibility for behaviors. According to one white man with higher education,
“For me…if I could just be very blatant, [this] scream[s] a left-wing liberal agenda…Pretty soon, we’re not responsible for anything. There’s a reason…No, is it not James Holmes’ fault that he shot those people. No, he’s, you know, genetically disposed and you know, maybe cuz…[he] had schizophrenia or you know [had a] family problem with it. There’s personal responsibility. There’s not always a genetic reason for why people do things you know even though there may be a disposition towards it.” [frustrated tone of voice].
In a similar vein, participants in several groups said that some smokers might use information about a genetic link to nicotine addiction as an “excuse” or justification to not quit smoking.
Evaluating the scientific merits of the study
Another distinction between people who did and did not accept the information occurred in relation to their beliefs about the scientific merits of the study presented in the video. People who accepted the information tended not to question the quality of the scientific research. One African American man with higher education began his explanation by saying, “…every day with the advancements in science, people are finding different gene variants…I’m not 100% sure, but I’ll believe it.” In contrast, many people who expressed skepticism indicated that they would need additional information about the study design before deciding whether to accept or reject it: “…you need to know how many people did they test…how long did they follow these people…the age of ‘em…I just think it’s not enough information” [African American woman with higher education]. Still other participants rejected the information outright, expressing a strong mistrust of scientists and pharmaceutical companies: “I’m in a class…dealing with…mathematical terms, and scales, and graphs…my professor [says] they show you what they want you to see…I’m not gonna believe what their study is saying” [African American man with higher education].
Skeptical participants also expressed concerns about the relevance of the study to real-world populations and settings. One white woman with higher education wondered how many people would be affected by the gene by inquiring about the absolute likelihood of inheriting the genetic variant given its prevalence in the population: “What’s the probability of someone ending up with this assortment of genes even in the first place?” In contrast, an African American man with lower education indicated that genetics researchers overlooked obvious information about the true causes of smoking; this oversight decreased the extent to which he believed the research was relevant to him and his neighbors. For this man, smoking resulted from stress, and stress resulted from financial difficulties:
“I think you get me money—I'll quit smokin’…I think that…these big, brainiac researchers and stuff, they—they getting too far into the—I mean look, talking about molecular genes and genetics, and they need to just basically study what's right in front of you, is these people, people are stressed. People you know, smoke because of stress. A lot of people smoke. Now, you may get hooked because of the stuff, like I say the stuff in the cigarettes, but a lot of people get hooked because of stress…If you wanna do a study, do the money study [i.e., offer financial incentives to quit]. That's not gonna hurt nobody, you know? Giving somebody some money ain't gonna hurt 'em… I wish they would do a study like that, come to the—come to the hood.”
This statement, which uses a fairly pejorative term for an intelligent person – brainiac – illustrates that this man believed that seemingly intelligent tobacco researchers are overlooking an obvious cause of tobacco use and, further, that this type of genetic research is not relevant for individuals who reside in neighborhoods whose residents are primarily African American and often have low incomes.
Discussion
Ineffective communication is a critical barrier to the successful translation of genomics research into public health and clinical practice. Overcoming this barrier would facilitate translation and might help prevent the exacerbation of health disparities due to unequal access to genomics technologies. The present research makes four key contributions. First, it fills a gap in scientific understanding of the way in which the general public—particularly those who may be medically underserved, such as racial minorities and people with less formal education— understand and draw meaning from mass media news reports describing genomics research discoveries. Specifically, the extent to which an individual accepts mass media-based genomic information as true versus greets the information with skepticism or outright rejection is based on the knowledge and beliefs that they held prior to being exposed to the new information.
These findings are consistent with predictions from theories of persuasion and information processing (Chen & Chaiken, 1999; Petty & Cacioppo, 1996), with the mental models approach to risk communication (Fischhoff, 1999; Morgan, Fischhoff, Bostrom, & Atman, 2002), and with research illustrating that the public critically evaluates, rather than passively receives, media portrayals of genes and genetics (Bates, 2005; Condit et al., 2001). The results are also consistent with emerging research emphasizing the importance of having a coherent understanding of the biological mechanisms that link a specific behavior to a specific health outcome (Cameron et al., 2012; Marteau & Weinman, 2006). However, our study is the first to illustrate how these distinct but overlapping processes interact to result in participants’ (non)willingness to entertain the mere possibility of a link between genetics and a common behavioral risk factor for cancer and other chronic diseases.
Although this study was conducted in the context of nicotine addiction, the general findings are likely applicable to other health conditions with a multifactorial etiology. The basic components of the information processing model (i.e., pre-video knowledge informing beliefs are used as a filter through which to evaluate information) are likely to apply more broadly than to nicotine addiction alone. For example, based on statements calling a genetic basic for nicotine addiction “too specific,” genetic variants associated with a different highly-specific behavior (e.g., running marathons) might be perceived as less credible than a variant associated with a more general behavior or constellation of behaviors (e.g., exercising). Future research should explore the conditions under which a genetic link to a behavior is likely to be believed. Communication strategies that provide a coherent explanation for genetic links to behavior in a way that incorporates laypeople’s strong beliefs about the importance of personal agency and willpower for behavior change may be particularly powerful (Marteau & Weinman, 2006).
The study’s second contribution is its emphasis on the potentially detrimental consequences of conflicting expert and lay understandings of disease etiology. Consistent with prior research (Davison, Frankel, & Smith, 1992; Gurmankin Levy, Weinstein, Kidney, Scheld, & Guarnaccia, 2008; Slovic, 2000), participants responded with mistrust and skepticism when their ideas about how genetics “worked” conflicted with current scientific evidence. However, the lay models could not be considered irrational; they were informed by personal experiences and prior knowledge, particularly family history. These experiences and knowledge pervaded every aspect of the information acceptance or rejection process. Some discrepancies resulted in particularly strong responses. Participants who strongly believed that smoking was either learned or due entirely to “choice” and who also endorsed a relatively deterministic view of the role of genetics in specific diseases were particularly likely to reject the information. Consequently, rather than taking a paternalistic approach to educating the public about genomics, a more effective strategy might be to work with members of the public to achieve a common understanding of genetics and genomics based on the prior knowledge and experiences of both groups, not only experts (Morgan et al., 2002). This common understanding would likely expand discussion from focusing only on biology and individual choice to include the role of factors outside of the participant’s control, such as social and environmental factors and the element of randomness that is inherent in any distribution of disease (Davison et al., 1992). Future intervention efforts could be based on this shared understanding of a richer and more complete picture of the etiology of tobacco use.
Our third contribution is adding nuance to reports that many Americans endorse a multifactorial etiological model for common diseases (Hay et al., 2011; Sanderson et al., 2013; Waters, Muff, & Hamilton, 2014). It could be that type of health problem is an important boundary condition that determines the extent to which the public accepts or rejects information describing a genetic link to some health outcome. For example, people might more readily accept the idea of a genetic link to conditions that are obviously physical, such as cancer or heart disease, compared to conditions that are more commonly associated with mental health (e.g., addiction) or behavior (e.g., smoking). Future research should investigate this possibility.
Much research has used the Common Sense Model (Leventhal, Brissette, & Leventhal, 2003) to examine how beliefs about the factors that cause a disease (i.e., its causal beliefs) affect subsequent behavior. In general, people who attribute a disease to primarily genetic factors tend to favor biomedical approaches to prevention and treatment (Phelan, Yang, & Cruz-Rojas, 2006), whereas people who hold behavioral attributions tend to endorse lifestyle and behavioral prevention strategies (Petrie, Myrtveit, Partridge, Stephens, & Stanton, 2015). Informing people of a genetic basis for disease resulted in unfavorable changes to health beliefs and cognitions in some studies (Smerecnik et al., 2009), but favorable or null effects in others (Sanderson, Persky, & Michie, 2010; Waters, Kincaid, et al., 2014). The present study expands such work by describing how both genetic and behavioral causal beliefs combine with mental models about how genes “work” to affect information acceptance. In this way, it enriches research that focuses only on health cognitions, which are downstream consequences of information acceptance. Understanding factors that could lead to information acceptance or rejection will facilitate the development of more effective genomic health communications.
From a more speculative and hypothesis-generating perspective, this research might provide preliminary indications of the defensive processing of genomics research findings. Statements that evaluated the scientific merits of the study could be construed as counter– arguing (van ‘t Riet & Ruiter, 2013), which is a form of defensive processing people use when they receive information that threatens their sense of self (Ditto & Lopez, 1992). In this case, smokers who believe that they have control over their smoking and also hold somewhat deterministic beliefs about genetics may feel that their sense of self as agentic beings is threatened when they learn about a genetic link to nicotine addiction. Denigrating the quality or source of the information reduces that threat. This hypothesis is consistent with a recent study that reported college smokers who reported they would want to have a genetic test repeated, but only if they were told that they had a genetic marker for increased lung cancer risk (Shepperd et al., 2014).
The defensive processing hypothesis might also explain the tendency for people to simultaneously hold both deterministic beliefs and more agentic beliefs about genetics (Condit, 2011; Condit et al., 2009). Condit and colleagues assert that whether an individual “deploys” the deterministic or agentic attitude towards genetics depends on which strategy would best protect their self-interests, such as maintaining a favorable view about themselves. Nevertheless, because this study was not designed specifically to test the role of defensive processing in acceptance of genetic information, nor in the use of deterministic beliefs, these hypotheses should be verified in future research.
Limitations and Strengths
Strong representation in the sample from traditionally underrepresented groups increases confidence that our findings are relevant to two of the many groups that experience disproportionately high difficulty quitting and morbidity and mortality from smoking-related illnesses. However, because most participants were established smokers, the results may not be applicable to light or intermittent smokers.
Conducting focus groups instead of interviews or surveys enabled the research team to capitalize on the ability of group dynamics to enrich the discussions. This effect was most apparent in two areas. First, despite stratifying groups by education, there was considerable within-group variation in knowledge about genes and genetic risk. This variation was so great that we were unable to detect differences in knowledge based on education (i.e., within-group differences were greater than between-group differences). Nevertheless, within-group transfer of knowledge from participants with relatively more knowledge to participants with relatively less knowledge enabled participants with less knowledge to contribute to the conversation.
The second area of influence was less desirable. In some groups a participant either monopolized portions of the conversation or held such strong opinions that other voices were silenced. The facilitator addressed this by asking for others’ opinions and by emphasizing that all voices were important. Such events were added to field notes and used as context to interpret the data. In a small number of cases participants changed their minds about the validity of the video contents after hearing others’ opinions. However, there was insufficient data to explore predictors of this.
Conclusions
Smokers used their existing knowledge and beliefs as context through which to interpret a novel mass media report about the discovery of a genetic variant associated with increased severity of nicotine addiction. Many smokers responded with skepticism and mistrust, due in part to discrepancies between their understandings of the smoking-genetics relationship and expert understandings. Resolving these discrepancies in a way that respects smokers’ experiential knowledge and also helps them to update their knowledge with scientific evidence to develop coherent understandings of the gene-behavior-health link will facilitate the translation of basic genomics research into public health and clinical practice. Leaving the discrepancies unresolved may result in laypeople rejecting the value of genomics research and genomic-based medicine just when the clinical utility of such information is increasing.
Supplementary Material
Highlights.
Lay conceptualizations of genetic risk include a complex constellation of beliefs.
Lay skepticism of genetic information can result from divergent lay/expert beliefs.
Genetic communications that incorporate lay beliefs may be more effective.
Acknowledgments
This research was supported by a grant from the American Cancer Society (ACS) to Erika Waters (MRSG-11-214-01-CPPB) and by the Washington University Institute of Clinical and Translational Sciences grant UL1TR000448 from the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH or ACS.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of interest: Erika Waters, Linda Ball, and Sarah Gehlert each declare that they have no financial or personal conflicts of interest. The study sponsors had no role in study design; collection, analysis and interpretation of data; writing of the report and in the decision to submit the report for publication.
References
- Bates BR. Public culture and public understanding of genetics: A focus group study. Public Understanding of Science. 2005;14:47–65. doi: 10.1177/0963662505048409. [DOI] [PubMed] [Google Scholar]
- Bates BR, Templeton A, Achter PJ, Harris TM, Condit CM. What does "A gene for heart disease" mean? A focus group study of public understandings of genetic risk factors. American Journal of Medical Genetics. 2003;119A:156–161. doi: 10.1002/ajmg.a.20113. [DOI] [PubMed] [Google Scholar]
- Bierut LJ. Convergence of genetic findings for nicotine dependence and smoking related diseases with chromosome 15q24-25. Trends in Pharmacological Science. 2010;31(1):46–51. doi: 10.1016/j.tips.2009.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron LD, Marteau TM, Brown PM, Klein WM, Sherman KA. Communication strategies for enhancing understanding of the behavioral implications of genetic and biomarker tests for disease risk: The role of coherence. Journal of Behavioral Medicine. 2012;35(3):286–298. doi: 10.1007/s10865-011-9361-5. [DOI] [PubMed] [Google Scholar]
- Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. Thousand Oaks, CA: Sage; 2006. [Google Scholar]
- Chen S, Chaiken S. The heuristic-systematic model in its broader context. In: Chaiken S, Trope Y, editors. Dual-Process Theories in Social Psychology. New York, NY: The Guilford Press; 1999. pp. 73–96. [Google Scholar]
- Condit CM. How geneticists can help reporters to get their story right. Nature Reviews Genetics. 2007;8(10):815–820. doi: 10.1038/nrg2201. [DOI] [PubMed] [Google Scholar]
- Condit CM. Public understandings of genetics and health. Clinical Genetics. 2010;77(1):1–9. doi: 10.1111/j.1399-0004.2009.01316.x. [DOI] [PubMed] [Google Scholar]
- Condit CM. When do people deploy genetic determinism? A review pointing to the need for multifactorial theories of public utilization of scientific discources. Sociology Compass. 2011;5(7):618–635. [Google Scholar]
- Condit CM, Ferfuson A, Kassel RCT, Gooding C, Parrott R. An exploratory study of the impact of news headlines on genetic determinism. Science Communication. 2001;22:379–395. [Google Scholar]
- Condit CM, Gronnvoll M, Landau J, Shen L, Wright L, Harris TM. Believing in both genetic determinism and behavioral action: a materialist framework and implications. Public Understanding of Science. 2009;18(6):730–746. [Google Scholar]
- Condit CM, Shen L. Public understanding of risks from gene-environment interaction in common diseases: implications for public communications. Public Health Genomics. 2011;14(2):115–124. doi: 10.1159/000314915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davison C, Frankel S, Smith GD. The limits of lifestyle: re-assessing 'fatalism' in the popular culture of illness prevention. Social Science and Medicine. 1992;34(6):675–685. doi: 10.1016/0277-9536(92)90195-v. [DOI] [PubMed] [Google Scholar]
- Ditto PH, Lopez DF. Motivated skepticism: use of differential decision criteria for preferred and nonpreferred conclusions. Journal of Personality and Social Psychology. 1992;63(4):568–584. [Google Scholar]
- Donelle L, Hoffman-Goetz L, Clarke JN. Portrayal of genetic risk for breast cancer in ethnic and non-ethnic newspapers. Women's Health. 2004;40(4):93–111. doi: 10.1300/j013v40n04_06. [DOI] [PubMed] [Google Scholar]
- Fischhoff B. Why (cancer) communication can be hard. Journal of the National Cancer Institute Monographs. 1999;25:7–13. doi: 10.1093/oxfordjournals.jncimonographs.a024213. [DOI] [PubMed] [Google Scholar]
- Godino JG, van Sluijs EM, Marteau TM, Sutton S, Sharp SJ, Griffin SJ. Lifestyle Advice Combined with Personalized Estimates of Genetic or Phenotypic Risk of Type 2 Diabetes, and Objectively Measured Physical Activity: A Randomized Controlled Trial. PLoS Medicine. 2016;13(11):e1002185. doi: 10.1371/journal.pmed.1002185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green RF, Dotson WD, Bowen S, Kolor K, Khoury MJ. Genomics in Public Health: Perspective from the Office of Public Health Genomics at the Centers for Disease Control and Prevention (CDC) Healthcare (Basel) 2015;3(3):830–837. doi: 10.3390/healthcare3030830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guba EG, Lincoln YS. Competing paradigms in qualitative research. In: Denzin NK, Lincoln YS, editors. Handbook of Qualitative Research. 3rd. Thousand Oaks, CA: Sage; 1994. pp. 105–117. [Google Scholar]
- Gurmankin Levy A, Weinstein N, Kidney E, Scheld S, Guarnaccia P. Lay and expert interpretations of cancer cluster evidence. Risk Analysis. 2008;28(6):1531–1538. doi: 10.1111/j.1539-6924.2008.01110.x. [DOI] [PubMed] [Google Scholar]
- Hartz SM, Olfson E, Culverhouse R, Cavazos-Rehg P, Chen LS, DuBois J, Bierut LJ. Return of individual genetic results in a high-risk sample: enthusiasm and positive behavioral change. Genetics in Medicine. 2015;17(5):374–379. doi: 10.1038/gim.2014.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hay J, DiBonaventura M, Baser R, Press N, Shoveller J, Bowen D. Personal attributions for melanoma risk in melanoma-affected patients and family members. Journal of Behavioral Medicine. 2011;34(1):53–63. doi: 10.1007/s10865-010-9286-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollands GJ, French DP, Griffin SJ, Prevost AT, Sutton S, King S, Marteau TM. The impact of communicating genetic risks of disease on risk-reducing health behaviour: systematic review with meta-analysis. BMJ. 2016;352:1102. doi: 10.1136/bmj.i1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeong S-H. Effects of news about genetics and obesity on controllability attribution and helping behavior. Health Communication. 2007;22(3):221–228. doi: 10.1080/10410230701626877. [DOI] [PubMed] [Google Scholar]
- Leventhal H, Brissette I, Leventhal EA. The common-sense model of self-regulation of health and illness. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behaviour. New York, NY: Routledge; 2003. pp. 42–65. [Google Scholar]
- Lipkus IM, Schwartz-Bloom R, Kelley MJ, Pan W. A preliminary exploration of college smokers' reactions to nicotine dependence genetic susceptibility feedback. Nicotine and Tobacco Research. 2015;17(3):337–343. doi: 10.1093/ntr/ntu155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marteau TM, Aveyard P, Munafo MR, Prevost AT, Hollands GJ, Armstrong D, Kinmonth AL. Effect on adherence to nicotine replacement therapy of informing smokers their dose is determined by their genotype: a randomised controlled trial. PloS One. 2012;7(4):e35249. doi: 10.1371/journal.pone.0035249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marteau TM, French DP, Griffin SJ, Prevost AT, Sutton S, Watkinson C, Hollands GJ. Effects of communicating DNA-based disease risk estimates on risk-reducing behaviours. Cochrane Database Systematic Review. 2010;(10):CD007275. doi: 10.1002/14651858.CD007275.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marteau TM, Weinman J. Self-regulation and the behavioural response to DNA risk information: A theoretical analysis and framework for future research. Social Science and Medicine. 2006;62:1360–1368. doi: 10.1016/j.socscimed.2005.08.005. [DOI] [PubMed] [Google Scholar]
- McBride CM, Birmingham WC, Kinney AY. Health psychology and translational genomic research: Bringing innovation to cancer-related behavioral interventions. American Psychologist. 2015;70(2):91–104. doi: 10.1037/a0036568. [DOI] [PubMed] [Google Scholar]
- Morgan MG, Fischhoff B, Bostrom A, Atman CJ. Risk Communication: A Mental Models Approach. Cambridge, UK: Cambridge University Press; 2002. [Google Scholar]
- Petersen A. Biofantasies: Genetics and medicine in the print news media. Social Science in Medicine. 2001;52(8):1255–1268. doi: 10.1016/s0277-9536(00)00229-x. [DOI] [PubMed] [Google Scholar]
- Petrie KJ, Myrtveit SM, Partridge AH, Stephens M, Stanton AL. The relationship between the belief in a genetic cause for breast cancer and bilateral mastectomy. Health Psychology. 2015;34(5):473–476. doi: 10.1037/hea0000118. [DOI] [PubMed] [Google Scholar]
- Petty RE, Cacioppo JT. The elaboration likelihood model of persuasion. In: Berkowitz L, editor. Advances in Experimental Social Psychology. Vol. 19. New York, NY: Academic Press; 1996. pp. 123–205. [Google Scholar]
- Phelan JC, Yang LH, Cruz-Rojas R. Effects of attributing serious mental illnesses to genetic causes on orientations to treatment. Psychiatric Services. 2006;57:382–387. doi: 10.1176/appi.ps.57.3.382. [DOI] [PubMed] [Google Scholar]
- Sanderson SC, Diefenbach MA, Streicher SA, Jabs EW, Smirnoff M, Horowitz CR, Richardson LD. Genetic and lifestyle causal beliefs about obesity and associated diseases among ethnically diverse patients: a structured interview study. Public Health Genomics. 2013;16(3):83–93. doi: 10.1159/000343793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanderson SC, McBride CM, O'Neill SC, Docherty S, Shepperd J, Lipkus IM. Young smokers' interpretations of the estimated lung cancer risk associated with a common genetic variant of low penetrance. Public Health Genomics. 2014;17(2):68–75. doi: 10.1159/000356708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanderson SC, O'Neill SC, White DB, Bepler G, Bastian L, Lipkus IM, McBride CM. Responses to online GSTM1 genetic test results among smokers related to patients with lung cancer: a pilot study. Cancer Epidemiology, Biomarkers, and Prevention. 2009;18(7):1953–1961. doi: 10.1158/1055-9965.EPI-08-0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanderson SC, Persky S, Michie S. Psychological and behavioral responses to genetic test results indicating increased risk of obesity: does the causal pathway from gene to obesity matter? Public Health Genomics. 2010;13(1):34–47. doi: 10.1159/000217794. [DOI] [PubMed] [Google Scholar]
- Shepperd JA, Lipkus IM, Sanderson SC, McBride CM, O'Neill SC, Docherty S. Testing different communication formats on responses to imagined risk of having versus missing the GSTM1 gene. Journal of Health Communication. 2013;18(1):124–137. doi: 10.1080/10810730.2012.688245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepperd JA, Novell CA, O'Neill SC, Docherty SL, Sanderson SC, McBride CM, Lipkus IM. Contemplating genetic feedback regarding lung cancer susceptibility. Annals of Behavioral Medicine. 2014;47(3):395–403. doi: 10.1007/s12160-013-9561-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slovic P. Trust, emotion, sex, politics, and science: Surveying the risk-assessment battlefield. In: Slovic P, editor. The Perception of Risk. London: Earthscan Publications, Ltd; 2000. pp. 390–412. [DOI] [PubMed] [Google Scholar]
- Smerecnik CMR, Grispen JE, Quaak M. Effectiveness of testing for genetic susceptibility to smoking-related diseases on smoking cessation outcomes: a systematic review and meta-analysis. Tobacco Control. 2012;21(3):347–354. doi: 10.1136/tc.2011.042739. [DOI] [PubMed] [Google Scholar]
- Smerecnik CMR, Mesters I, de Vries NK, de Vries H. Alerting the general population to genetic risks: The value of health messages communicating the existence of genetic risk factors for public health promotion. Health Psychology. 2009;28(6):734–745. doi: 10.1037/a0016386. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. The Health Consequences of Smoking— 50 Years of Progress. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- van ‘t Riet J, Ruiter RA. Defensive reactions to health-promoting information: An overview and implications for future research. Health Psychology Review. 2013;7(sup1):S104–S136. [Google Scholar]
- Wang C, Coups EJ. Causal beliefs about obesity and associated health behaviors: results from a population-based survey. International Journal of Behavioral Nutrition and Physical Activity. 2010;7:19. doi: 10.1186/1479-5868-7-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters EA, Kincaid C, Kaufman AR, Stock ML, Peterson LM, Muscanell NL, Guadagno RE. Concerns about unintended negative consequences of informing the public about multifactorial risks may be premature for young adult smokers. British Journal of Health Psychology. 2014;19(4):720–736. doi: 10.1111/bjhp.12069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waters EA, Muff J, Hamilton JG. Multifactorial beliefs about the role of genetics and behavior in common health conditions: prevalence and associations with participant characteristics and engagement in health behaviors. Genetics in Medicine. 2014;16(12):913–921. doi: 10.1038/gim.2014.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson TD, Schooler JW. Thinking too much: Introspection can reduce the quality of preferences and decisions. Journal of Personality and Social Psychology. 1991;60(2):181–192. doi: 10.1037//0022-3514.60.2.181. [DOI] [PubMed] [Google Scholar]
- Zajonc RB. Feeling and thinking: Preferences need no inferences. American Psychologist. 1980;35(2):151–175. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.