Abstract
Objective
To determine whether preferred language for care and insurance type are associated with cost among hospitalized children.
Methods
We conducted a retrospective cohort study of inpatients at a freestanding children’s hospital from 1/2011 to 12/2012. Patient clinical and demographic information and hospital costs were obtained from administrative data. Cost differences by language and insurance were calculated based on multivariate generalized linear model estimates, which allowed for language-insurance interaction effects. Models were also stratified by medical complexity and length of stay (LOS) ≥3 days.
Results
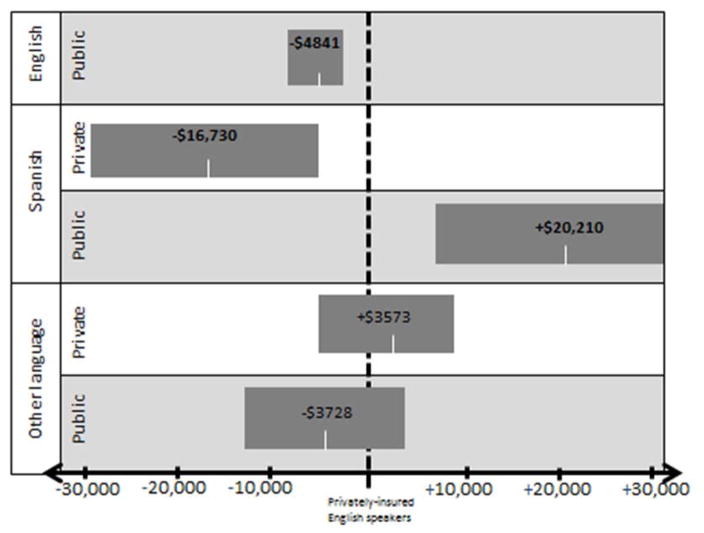
Of 19,249 inpatient admissions, 8% preferred Spanish, 6% preferred another language, and 47% had public insurance. Models controlled for LOS, medical complexity, distance from home to hospital, age, asthma diagnosis, and race/ethnicity. Compared to privately-insured English speakers, total hospital costs were significantly higher for publicly-insured Spanish speakers (+$20,211 [95% CI +$7781, +$32,641]), and lower for privately-insured Spanish speakers (−$16,730 [−$28,265, −$5195]) and publicly-insured English speakers (−$4841 [−$6781, −$2902]). A similar pattern was found for pharmacy costs. Differences were most pronounced among children with medical complexity and with LOS ≥3 days.
Conclusions
Hospital costs varied significantly by preferred language and insurance type, even after adjusting for LOS and medical complexity. These differences in the amount of billable inpatient care provided to medically similar patients may represent either under- or over-provision of care on the basis of sociodemographic factors and communication, suggesting problems with care efficiency and equity. Further investigation into the causes may inform development of effective interventions.
Background
In 2011, 15% of US children lived with at least one parent who had limited English proficiency (LEP), defined as speaking English less than “very well.”1 Language barriers in health care have been associated with decreased adherence, comprehension, and satisfaction with care,2,3 along with increased resource utilization in some settings4–7, worse condition-specific outcomes,8–11 and increased risk for serious adverse events.12–15 Language barriers often co-occur with other potential barriers to high quality care, including poverty, low health literacy, and public insurance.10 However, the degree to which these factors interact with LEP to influence utilization and outcomes are poorly understood. Understanding these interactions may help target interventions to the patient population most likely to benefit.
Health care costs may be used to identify disparities in the provision of health care, by revealing differences in care patterns at the clinic, hospital, or population level. Cost serves as a proxy for the amount of billable care provided to a given patient, which should be similar for medically similar patients. Examining differences in costs on the basis of demographic factors can facilitate identification of disparities in care, which in turn facilitates investigation and intervention.
This study’s primary objective was to examine the association between costs of hospitalization and the interaction between patient language and insurance type at a freestanding children’s hospital. We used insurance type (private versus public) as a proxy for income level, as it is highly correlated with family income and was available for all patients.16 Secondary objectives included determining if cost variation was consistent across subpopulations defined by level of medical complexity and length of stay (LOS).
Patients and Methods
Study population and setting
Patients ≤ 21 years of age discharged from a freestanding children’s hospital’s inpatient medical or surgical units from 01/01/2011 to 12/31/2012 were eligible. Patients admitted to observation status, bone marrow transplant, rehabilitation or inpatient psychiatry were excluded, as these admission types have unique patterns of resource utilization. Both medical and surgical inpatient (but not observation) admissions were included, as we expected family language, culture, and social or financial constraints to be interfacing with care delivery in similar ways for both groups. We included all eligible admissions for a given patient, clustering by individual in the analysis. We also restricted to first hospitalization in the study period in a sensitivity analysis.
The study hospital has comprehensive professional interpreter services (in-person, telephone, and video), although this study was unable to track type and amount of interpretation provided.
Predictors and Covariates
Primary Independent Variables
Caregiver-reported preferred language for medical communication was recorded in the electronic medical record at hospital registration. Patient caregivers were classified as preferring English (hereafter “English speakers”), Spanish (hereafter “Spanish speakers”, or another language.
Insurance type was obtained from hospital administrative data and categorized as private or public (i.e., Medicaid). As <1% of children hospitalized at our institution are uninsured, they were included with the publicly-insured patients.
Covariates
Patient race and ethnicity were collected at registration by caregiver-report. We used the following mutually exclusive categories for analysis: non-Hispanic white (“white”), non-Hispanic black (“black”), Hispanic of any race (“Hispanic”), Asian or Pacific Islander, other or mixed, and refused or unknown.
Patient medical complexity was categorized using the Pediatric Medical Complexity Algorithm (PMCA), which classifies children as having no chronic illness, non-complex chronic illness, or complex chronic illness using retrospective International Classification of Disease 9th Revision Clinical Modification (ICD-9) codes.17 PMCA accounts for both diagnoses and intensity of utilization, and does not require a minimum amount of retrospective data; however, it uses only data from the previous 3 years, beginning with the date of admission.
Patient LOS was obtained from hospital administrative data. Given its skewed distribution, the variable was winsorized at the 99th percentile. Accordingly, 192 admissions with LOS > 60.7 days were assigned a LOS of 60.7 days.
We used patient address and geographic information systems software to determine distance between home address and the hospital.18 Distances from the hospital were classified as <30 miles, 30–60 miles, 61–120 miles, >120 miles, or missing. Distance provided information both about potential barriers to discharge and severity of illness, as children who reside long distances from this hospital are typically those who require tertiary- and quaternary-level care.
We controlled for having an ICD-9-coded asthma diagnosis for several reasons. First, asthma is a common reason for admission that disproportionately affects lower income and minority children.19–22 Second, asthma admissions have shorter LOS and lower costs compared to other admissions, which might confound our analysis. We also used hospital administrative data to identify the primary treating service (e.g., hematology-oncology) for each admission.
Outcomes
Hospital charges were obtained from administrative data, including total charges and those designated as laboratory, pharmacy, and radiology. Charges for interpretation were not included, as these are not billed to families. Charges were converted to costs using the hospital-specific cost-to-charge-ratio, then inflation adjusted to 2012 US dollars using the medical care component of the Consumer Price Index.23,24 As cost data has a skewed distribution, costs within each category were winsorized at the 99th percentile, impacting 193 encounters with total cost values from $362,661 to $3,455,981.
Primary Analysis
Descriptive statistics were generated for all predictors and outcomes. Multivariate analyses utilized generalized linear models with a log link and gamma family.25
A separate multivariate model was constructed for each cost outcome: total, pharmacy, laboratory, and radiology. The relationships between the predictors of interest (language and insurance type) and each outcome were assessed, adjusting for race/ethnicity, LOS, age, medical complexity, distance from the hospital, and asthma diagnosis, and clustered on individual. Given the potential for collinearity between language, race/ethnicity, and insurance status, multicollinearity diagnostics were performed. All variance inflation factors were < 5, indicating no problematic multicollinearity within the data set.26
Interaction terms between language, insurance type, and race/ethnicity were introduced into the multivariate models. Interactions associated with the outcomes at P<.05 were retained.
Marginal differences in costs, by language and insurance type, were then predicted from the generalized linear models.
Secondary Analysis
To investigate whether observed variation in costs differed by patient medical complexity, we repeated the primary analysis of total costs after stratifying by medical complexity level: non-chronic, non-complex chronic, and complex chronic. We also repeated the primary analysis after stratifying by LOS ≥3 days. In both cases, we controlled for all covariates listed in the main analysis, excluding the stratification variable.
Sensitivity analyses
To assess whether cost patterns by demographic characteristics were due to different types of illnesses requiring hospitalization, each of 26 admitting services was assessed for association with language, insurance type, and language-insurance combinations. The 12 services that were significantly associated with any of the predictors were included as additional covariates in a sensitivity analysis, which otherwise included the variables described previously. We also re-ran the models looking at total costs without controlling for LOS, and after restricting inclusion to each patient’s first hospitalization during the study period. Finally, we re-ran the analyses after winsorizing total costs and LOS at the 95th percentile, rather than the 99th percentile, to assess the influence of the most extreme values on our outcomes.
RESULTS
There were 19,249 hospital admissions that met study inclusion criteria, of which 47% were covered by public insurance and 14% involved caregivers preferring a non-English language for medical care (Table 1). Among admissions from Spanish-speaking families, 96% had public insurance. Overall median LOS was 2.6 days (interquartile range (IQR), 1.2 – 5.1 days, 95th percentile 19.5 days; mean 5.8 days, standard deviation (SD) 13.5 days), and overall median hospital costs were $12,842 (IQR $6550 – $27,011, 95th percentile $106,195; mean $32,542, SD $89,830).
Table 1.
Characteristics of patients discharged from the study hospital between 1/1/2011 and 12/30/2012 (N=19,249)
| Characteristic | Percent (n) |
|---|---|
| Age group, in years | |
| <2 | 33.4 (6436) |
| 2–4 | 16.7 (3220) |
| 5–12 | 27.0 (5189) |
| 13–18 | 20.2 (3894) |
| 19–21 | 2.7 (510) |
|
| |
| Race/Ethnicity | |
| Non-Hispanic white | 52.6 (10,121) |
| Hispanic | 16.4 (3165) |
| Black/African American | 7.0 (1355) |
| Other, multiracial, and unknown1 | 23.9 (4608) |
|
| |
| Language preferred for care | |
| English | 86.0 (16,559) |
| Spanish | 8.4 (1623) |
| Other2 | 5.5 (1067) |
|
| |
| Public Insurance (yes)3 | 47.0 (9041) |
|
| |
| Public Insurance, by preferred language4 | |
| English (n=16,559) | 40.6 (6727) |
| Spanish (n=1623) | 95.7 (1553) |
| Other (n=1067) | 71.3 (761) |
|
| |
| Asthma diagnosis | 10.1 (1946) |
|
| |
| Home distance from hospital | |
| <30 miles | 47.0 (9039) |
| 30–60 miles | 13.7 (2643) |
| 61–120 miles | 8.4 (1625) |
| >120 miles | 13.5 (2589) |
| Missing5 | 17.4 (3353) |
|
| |
| Medical Complexity (using PMCA) | |
| Non-chronic | 25.1 (4826) |
| Non-complex Chronic | 24.7 (4754) |
| Complex Chronic | 50.2 (9669) |
|
| |
| Length of stay in days (median, IQR) | 2.6 (1.2, 5.1) |
| By language | |
| English | 2.6 (1.2, 5.0) |
| Spanish | 2.6 (1.4, 5.8) |
| Other | 2.6 (1.3, 5.1) |
| By insurance type | |
| Public insurance | 2.7 (1.3, 5.8) |
| Private insurance | 2.5 (1.1, 4.8) |
|
| |
| Costs, US dollars (median, IQR) | |
| Total (n=19,255) | 12,842 (6550, 27,011) |
| Pharmacy (n=18,973) | 1029 (397, 3102) |
| Lab (n=16,240) | 733 (294, 1962) |
| Radiology (n=11,911) | 779 (301, 2113) |
This category includes 6.7% (of total) Asian/Pacific Islander, 4.3% multiracial, 1.7% American Indian or Alaska Native, 1.2% Native Hawaiian or other Pacific Islander, 4.8% other, and 5.2% refused/unknown.
This category includes 1.0% (of total) Somali, 0.8% Vietnamese, 0.7% Russian, 0.5% Chinese, 0.2% Amharic, and 0.2% sign language; the remaining 42 languages account for less than 0.15% each.
This category includes 0.4% of total receiving charity care and 0.1% self-pay; the remainder have some type of insurance coverage.
Values listed after each language reflect the number and percent of families with public insurance within each language-preference group
Missing distances were mostly due to home addresses listed as a post office box or private mailbox.
Total Costs
In multivariate analysis, the interaction term between language and insurance type was statistically significant and so was retained in the model. Because of the interaction term, the reference group for all language and insurance combinations was privately-insured English speakers. In adjusted analyses, publicly-insured English speakers had hospital stays that were $4841 less expensive (95% CI −$6781, −$2902, P<.001; Figure 1) than the referent. Similarly, privately-insured Spanish speakers had hospital stays that were $16,730 less expensive (95% CI −$28,265, −$5195, P=.004). Publicly-insured Spanish speakers, in contrast, had hospital stays that were $20,211 more expensive (95% CI $7781, $32,641, P=.001) than the referent. There were no significant differences in total cost among either privately- or publicly-insured children from families preferring other languages compared to the referent.
Figure 1.
Adjusted relative differences in total costs in 2012 US dollars for language and insurance categories.
The reference category denoted by the dotted line is privately insured English speakers. Results are adjusted for length of stay, race/ethnicity, distance from hospital, medical complexity, asthma diagnosis, age category, insurance type, preferred language, and the interaction between insurance and language. Bars represent 95% confidence intervals.
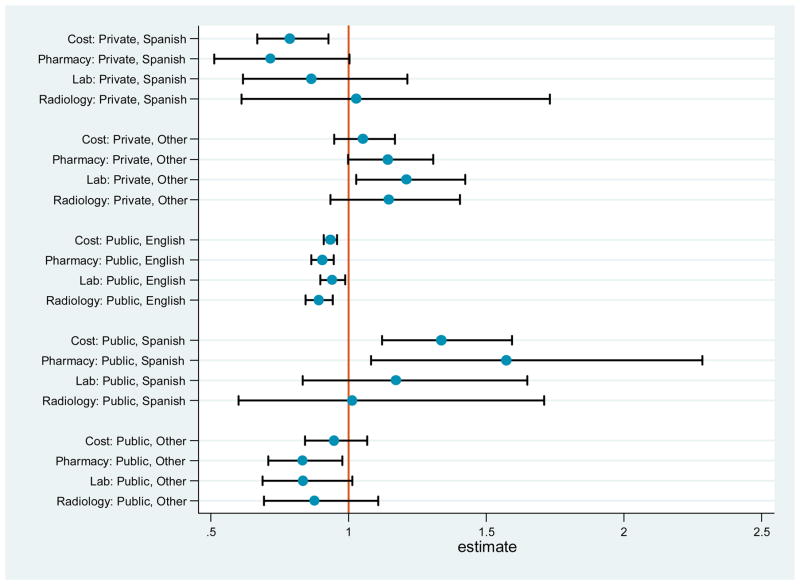
Pharmacy, Laboratory, and Radiology Costs
In the multivariate analysis of pharmacy costs (n= 18,973), we found a similar pattern to overall costs (Figure 2). Compared to privately-insured English speakers, pharmacy costs were lower for publicly-insured English speakers (−$3463 [95% CI −$5228, −$1697], P<.001) and privately-insured Spanish speakers (−$11,485 [95% CI −$23,285, $314], P=0.056), and higher for publicly-insured Spanish speakers ($15,560 [95% CI $2529, $28,592], P=.01). Among families preferring other languages for care, pharmacy costs were lower for those with public insurance (−$6317 [95% CI −$12093, −$541], P=.03).
Figure 2.
Adjusted relative ratios for total, pharmacy, laboratory, and radiology costs, by language and insurance groups. See Appendix for relative ratio values with 95% confidence intervals and P-values.
Relative ratios are compared to privately-insured English speakers, denoted by the center line. Results are adjusted for length of stay, race/ethnicity, distance from hospital, medical complexity, asthma diagnosis, age category, insurance type, preferred language, and the interaction between insurance and language. Bars represent 95% confidence intervals.
Adjusted analysis of laboratory costs (n=16,240) revealed lower average costs for publicly-insured English speakers (−$429 [95% CI −$778, −$79], P=.02) and higher costs for publicly-insured children preferring other languages ($1351 [95% CI $174, $2528], P=.02).
Analysis of radiology costs (n=11,911) revealed lower costs for publicly-insured English speakers only (−$269 [95% CI −$399, −$139]).
Secondary Analyses
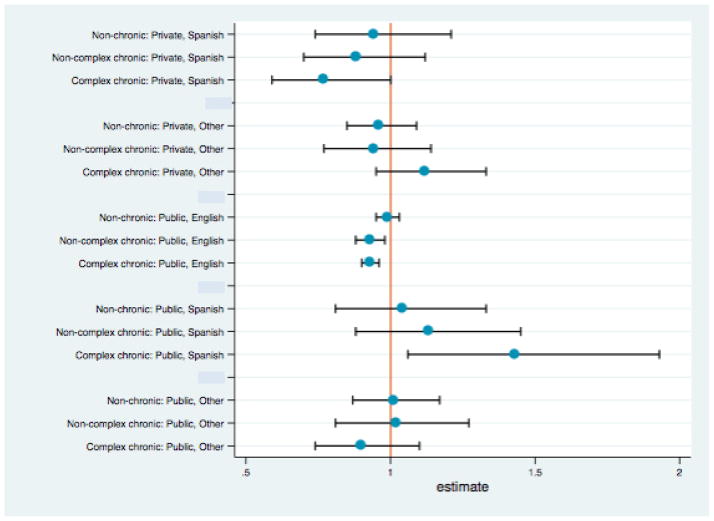
Stratification by medical complexity revealed no variation in cost by insurance or language among children with no chronic illness (n=4826). Among children with non-complex chronic illness (n=4754), publicly-insured English speakers had significantly less expensive hospital stays (−$6240, 95% CI −$12,275, −$205, P=.01), but there were no differences detected among non-English speakers. Among children with complex chronic illness (n=9669), results mirrored those of our primary analysis, with less expensive hospitalizations for publicly-insured English speakers and privately-insured Spanish speakers, and more expensive hospital stays for publicly-insured Spanish speakers (Figure 3). Stratification of the main analysis by LOS ≥ 3 days revealed no differences by group among those with a short stay (Table 2). Among those with LOS ≥3 days, there were no differences for publicly-insured English speakers, while patterns for Spanish speakers were similar to the primary analysis.
Figure 3.
Adjusted relative ratios for total costs, stratified by complex chronic illness, by language and insurance groups. See Appendix for relative ratio values with 95% confidence intervals and P-values.
Relative ratios are compared to privately-insured English speakers, denoted by the center line. Results are adjusted for length of stay, race/ethnicity, distance from hospital, asthma diagnosis, age category, insurance type, preferred language, and the interaction between insurance and language. Bars represent 95% confidence intervals.
Table 2.
Adjusted relative differences in total costs with 95% confidence intervals, compared to hospital costs for privately-insured English speakers.
| Preferred language | Insurance type | Main analysisa (n=19,249) | Stratified analysisb | Sensitivity analysisc (n=19,249) | |
|---|---|---|---|---|---|
|
| |||||
| LOS <3 days (n=11,122) | LOS ≥3 days (n= 8127) | ||||
| English | Public | 0.93 (0.91, 0.96)* | 0.97 (0.94, 1.01) | 0.98 (0.93, 1.04) | 0.99 (0.94, 1.04) |
|
| |||||
| Spanish | Private | 0.79 (0.67, 0.93)* | 0.94 (0.80, 1.12) | 0.59 (0.34, 1.00)** | 0.59 (0.44, 0.79)* |
| Public | 1.34 (1.12, 1.59)* | 1.08 (0.91, 1.30) | 1.75 (1.01, 3.02)* | 1.75 (1.30, 2.35)* | |
|
| |||||
| Other languages | Private | 1.05 (0.95, 1.17) | 1.01 (0.87, 1.18) | 1.11 (0.91, 1.37) | 1.14 (0.94, 1.37) |
| Public | 0.95 (0.84, 1.07) | 0.94 (0.80, 1.11) | 1.01 (0.80, 1.28) | 0.99 (0.80, 1.23) | |
Based on a generalized linear model with log link, gamma family, and clustered on individual, controlling for length of stay (LOS), race/ethnicity, distance from hospital, medical complexity, asthma diagnosis, age category, insurance type, preferred language, and the interaction between insurance and language
Adjusting for same potential covariates as main analysis, and stratified by LOS ≥3 days
Identical to main analysis, but not controlling for LOS
P < .05
P < .055
Sensitivity Analyses
Results for the total cost model were unchanged after controlling for 12 clinical service lines or restricting to the first admission per patient during the study time period (data not shown). Results were similar, with similar to slightly attenuated effect sizes, when costs and LOS were winsorized at the 95th rather than 99th percentile (see Appendix). When not controlling for LOS, the total cost findings for both publicly- and privately-insured Spanish speakers were more pronounced, while the findings for publicly-insured English-speakers became non-significant (Table 2).
Discussion
In this study of 19,249 hospital admissions, we found that patterns of hospital costs varied significantly by insurance type and preferred language for medical communication, even after controlling for potential confounders including medical complexity, LOS, hospital service, and distance between the child’s home and hospital. Compared to privately-insured English speakers, publicly-insured English speakers and privately-insured Spanish speakers had less costly hospital stays, while publicly-insured Spanish speakers had more expensive stays. These patterns were most pronounced among children with hospital stays ≥ 3 days in length and those with complex, chronic illness. Pharmacy and laboratory costs generally mirrored total cost patterns, with less variation in radiology costs. These results suggest there were differences in the amount of billable care provided to hospitalized children on the basis of demographic, rather than clinical, characteristics.
For publicly-insured English speakers, we found lower hospital costs compared to their privately-insured counterparts in all cost categories. However, the cost differences were not significant when we stratified by LOS or did not adjust for LOS. Since LOS is the largest contributor to hospital costs, this suggests that publicly-insured English speakers may have been staying longer but using fewer resources per day. This lower intensity of resource utilization may be due to several factors. For example, perceived barriers to discharge, e.g. lack of transportation and/or access to follow-up care for publicly-insured patients may lead to keeping a child in the hospital longer than might be strictly medically necessary. Previous studies have found longer LOS among children with Medicaid, in populations hospitalized for spinal fusion,27 infections,7 and asthma.28 For example, Glick reports longer LOS and similar costs (adjusted for LOS) among Medicaid-insured children with asthma, but found low-income patients to have longer LOS but lower LOS-adjusted costs, similar to our findings.28 Another mediating factor may be lower parent engagement among publicly-insured families, leading to less parental advocacy for additional clinical diagnostics and intervention. Previous studies have found that minority and/or low income children were less likely to receive potentially inappropriate antibiotic prescriptions, suggesting less parent demand for unnecessary treatment.29,30 However, the current analysis cannot determine whether there was under-utilization for publicly-insured patients, over-utilization for privately-insured patients, or some combination of both.
Hospital stays among privately-insured Spanish speakers were less expensive. While registered as preferring Spanish for medical communication, the fact that these children had private insurance suggests that at least one parent may have been English-proficient, as the majority of private insurance at the time was employer-based,31 and most jobs offering insurance likely required some English proficiency. The language barrier for these families may have been lower than for publicly-insured Spanish-speakers, but their hospital costs still significantly differed from their privately-insured English-speaking counterparts. This highlights a central difficulty in identifying LEP families in pediatrics. Whose English proficiency matters? Even if we know that caregivers’ English proficiencies differ, how can we know which caregiver was at the bedside, and when? Controlling for LOS attenuated but did not adjust away the difference, suggesting a shorter stay contributed to but did not entirely explain the cost findings. These results could be accounted for by less parental advocacy, perhaps informed by the cultural value among Latinos of respect for authority figures,32 but without the delays to discharge that are associated with public insurance. These lower cost findings were primarily driven by children with medical complexity and longer LOS. Since many of the children without medical complexity at our institution receive medical care that is standardized by diagnosis,33 there may have been fewer opportunities to provide unequal care based on family characteristics or provider biases for those children.
Publicly-insured Spanish speakers had more expensive hospital stays, likely reflecting the impact of language barriers. As seen in previous studies, parental LEP may result in providers performing more tests, trying more treatments, or observing patients for longer periods to compensate for incomplete information and poor communication.4,5,7,34 These more expensive stays may also reflect poorer access to outpatient care or delayed presentation,10 although controlling for distance from home to hospital likely attenuated those associations. As we found among privately-insured Spanish-speakers, these cost differences were driven by children with medical complexity and prolonged LOS, suggesting that language barriers, cultural factors, and provider biases are most likely to impact care in visible ways when that care is more complicated or less evidence-based and standardized.
We found no associations between total cost, insurance type, and preferring a non-English, non-Spanish language, likely because the “other” group is a mix of many smaller languages and cultures, each too small to evaluate individually. Consolidation of these groups for analysis, while presently unavoidable, may be obscuring associations. Evaluation with larger samples is needed.
Prior studies examining language and hospital utilization have demonstrated mixed results, with some finding increased LOS5,7 or resource utilization6,35, generally within more narrowly defined diagnosis groups, and some finding none.36 Public insurance and/or other markers for socioeconomic status have also been linked to increased LOS and, in some cases, increased resource utilization (including costs).37–39. In our study, because we included children with many conditions, we chose cost as our outcome, rather than utilization of specific resources, as it provides a measure of all billable medical care that was provided during a hospitalization. We are unaware of other studies successfully able to examine the joint impact of language and insurance type on cost or utilization. Levas and colleagues, in their study of children hospitalized with infections, found increased LOS associated with both parental LEP and public insurance, but failed to find statistical interaction between the two; however, they were likely under-powered for such an analysis, with only 39 LEP families, of whom only 3 were privately insured.7 Failure to consider interactions between the multiple barriers to full engagement with the healthcare system that a family faces may mask the effects of factors that are exerting simultaneous, opposing pressures. For example, because the privately- and publicly-insured Spanish speakers had different cost patterns, assessment of cost by language alone might miss important differences that deserve evaluation. Aside from language and insurance, other factors may create barriers to receiving equitable care, such as low health literacy, limited self-efficacy, and lack of trust in the system; these should also be considered when targeting interventions to improve equity.
This study has several limitations. It was conducted at a single institution, so results may not be generalizable. However, preferred language is generally not available in multi-institution datasets, as few institutions routinely collect or report it. We were unable to account for the amount and type of professional interpretation provided in our analysis; costs may have differed by the degree to which the language barrier was effectively bridged. Another limitation was our use of insurance type as a proxy for family income. We used insurance, rather than census tract income data, because we had it for all participants, but were missing home address data for nearly 20% of subjects (mostly PO Box addresses). While insurance type provides some idea of family income for many families, it may misclassify children with public insurance due to medical complexity, and it fails to account for additional elements of socioeconomic status like parent education. It is also possible that the identified cost differences were driven by medical needs, or the continuation of expensive home medications, rather than demographic characteristics; however, our findings were robust to adjustment for a variety of markers of complexity and illness type. It should also be noted that LOS is central to overall costs, pharmacy costs (as most medications are given daily), and, to a lesser extent, laboratory costs; while all of our analyses controlled for LOS, differences in LOS likely remain an important driver of those outcomes. Finally, it is unclear whether the observed cost differences in this study reflect over- or under-utilization.
Conclusions
We found that costs of pediatric hospitalizations varied significantly based on the child’s insurance type and the family’s preferred language for care, even after controlling for LOS and medical complexity. This suggests disparities may exist in the provision of medical care on the basis of demographic characteristics. Poor access to outpatient care may lead to requiring more services when inpatient; however, we found lower LOS-adjusted costs for publicly-insured English speakers and privately-insured Spanish speakers, and only publicly-insured Spanish speakers had more expensive stays. These differences in the amount of billable care being provided between language and insurance groups require additional investigation to determine whether they reflect over-utilization, under-utilization, or both. Additionally, the relative contributions of language barriers, health literacy, parental activation and advocacy, and provider bias should be explored. Identifying patterns of disparate care and their causes is essential for development of interventions to improve the equity and efficiency of inpatient pediatric care.
Supplementary Material
Acknowledgments
Funding source: No external funding was obtained for this work. Dr. Lion’s time was supported by National Institute of Child Health and Human Development grant K23 HD078507 (PI Lion). Dr. Wright’s time was supported by The University of Washington Institute for Translational Health Sciences (UL1 TR000423). Dr. Desai’s time was supported by Agency for Healthcare Research and Quality grant 1 K08 HS024299-01 (PI Desai).
Footnotes
Financial disclosures: The authors have no financial relationships relevant to this article to disclose.
Conflict of Interest: The authors have no conflicts of interest to disclose.
Contributor’s Statements: K. Casey Lion: Dr. Lion participated in study conceptualization and design, performed the data analysis, drafted the initial manuscript, revised it critically, and approved the final manuscript as submitted.
Davene R. Wright: Dr. Wright participated in study conceptualization and design, assisted with data analysis, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
Arti D. Desai: Dr. Desai participated in study conceptualization, assisted with data analysis, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
Rita Mangione-Smith: Dr. Mangione-Smith oversaw all aspects of the study, participated in study conceptualization and design, critically reviewed and revised the manuscript, and approved the final manuscript as submitted.
References
- 1.Migration Policy Institute. [Accessed July 26, 2015];The Limited English Proficient Population in the United States. 2015 http://www.migrationpolicy.org/article/limited-english-proficient-population-united-states.
- 2.Morales LS, Cunningham WE, Brown JA, Liu H, Hays RD. Are Latinos less satisfied with communication by health care providers? J Gen Intern Med. 1999;14(7):409–417. doi: 10.1046/j.1525-1497.1999.06198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wilson E, Chen AH, Grumbach K, Wang F, Fernandez A. Effects of limited English proficiency and physician language on health care comprehension. J Gen Intern Med. 2005;20(9):800–806. doi: 10.1111/j.1525-1497.2005.0174.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hampers LC, McNulty JE. Professional interpreters and bilingual physicians in a pediatric emergency department: effect on resource utilization. Arch Pediatr Adolesc Med. 2002;156(11):1108–1113. doi: 10.1001/archpedi.156.11.1108. [DOI] [PubMed] [Google Scholar]
- 5.John-Baptiste A, Naglie G, Tomlinson G, et al. The effect of English language proficiency on length of stay and in-hospital mortality. J Gen Intern Med. 2004;19(3):221–228. doi: 10.1111/j.1525-1497.2004.21205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kravitz RL, Helms LJ, Azari R, Antonius D, Melnikow J. Comparing the use of physician time and health care resources among patients speaking English, Spanish, and Russian. Med Care. 2000;38(7):728–738. doi: 10.1097/00005650-200007000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Levas MN, Cowden JD, Dowd MD. Effects of the limited English proficiency of parents on hospital length of stay and home health care referral for their home health care-eligible children with infections. Arch Pediatr Adolesc Med. 2011;165(9):831–836. doi: 10.1001/archpediatrics.2011.61. [DOI] [PubMed] [Google Scholar]
- 8.Fernandez A, Schillinger D, Warton EM, et al. Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE) J Gen Intern Med. 2011;26(2):170–176. doi: 10.1007/s11606-010-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flores G. Language barriers to health care in the United States. N Engl J Med. 2006;355(3):229–231. doi: 10.1056/NEJMp058316. [DOI] [PubMed] [Google Scholar]
- 10.Flores G, Abreu M, Tomany-Korman SC. Limited english proficiency, primary language at home, and disparities in children’s health care: how language barriers are measured matters. Public Health Rep. 2005;120(4):418–430. doi: 10.1177/003335490512000409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Flores G, Tomany-Korman SC. The language spoken at home and disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121(6):e1703–1714. doi: 10.1542/peds.2007-2906. [DOI] [PubMed] [Google Scholar]
- 12.Bartlett G, Blais R, Tamblyn R, Clermont R, MacGibbon B. Impact of patient communication problems on the risk of preventable adverse events in acute care settings. CMAJ. 2008;178(12):1555–1562. doi: 10.1503/cmaj.070690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cohen AL, Rivara F, Marcuse EK, McPhillips H, Davis R. Are language barriers associated with serious medical events in hospitalized pediatric patients? Pediatrics. 2005;116(3):575–579. doi: 10.1542/peds.2005-0521. [DOI] [PubMed] [Google Scholar]
- 14.Divi C, Koss RG, Schmaltz SP, Loeb JM. Language proficiency and adverse events in US hospitals: a pilot study. Int J Qual Health Care. 2007;19(2):60–67. doi: 10.1093/intqhc/mzl069. [DOI] [PubMed] [Google Scholar]
- 15.Lion KC, Rafton SA, Shafii J, et al. Association between Language, Serious Adverse Events and Length of Stay among Hospitalized Children. Hospital Pediatrics. 2013;(3):219–225. doi: 10.1542/hpeds.2012-0091. [DOI] [PubMed] [Google Scholar]
- 16.Crimmel B. Health Insurance Coverage and Income Levels for the U.S. Noninstitutionalized Population under Age 65, 2001. Rockland, MD: Agency for Healthcare Research and Quality; 2004. [Google Scholar]
- 17.Simon TD, Cawthon L, Stanford S, Popalisky J, Mangione-Smith R. Development of a methodology to stratify children by level of medical complexity using hospital discharge and Medicaid claims data. Pediatric Academic Societies Annual Meeting; 2013; Washington, D.C. [Google Scholar]
- 18.Environmental Systems Research Institute. ArcGIS Desktop: Release 10. 2013 www.arcgis.com.
- 19.Claudio L, Stingone JA, Godbold J. Prevalence of childhood asthma in urban communities: the impact of ethnicity and income. Annals of epidemiology. 2006;16(5):332–340. doi: 10.1016/j.annepidem.2005.06.046. [DOI] [PubMed] [Google Scholar]
- 20.Halfon N, Newacheck PW. Childhood asthma and poverty: differential impacts and utilization of health services. Pediatrics. 1993;91(1):56–61. [PubMed] [Google Scholar]
- 21.Moorman JE, Rudd RA, Johnson CA, et al. National surveillance for asthma--United States, 1980–2004. Morbidity and mortality weekly report. Surveillance summaries (Washington, D.C.: 2002) 2007;56(8):1–54. [PubMed] [Google Scholar]
- 22.Stingone JA, Claudio L. Disparities in the use of urgent health care services among asthmatic children. Ann Allergy Asthma Immunol. 2006;97(2):244–250. doi: 10.1016/S1081-1206(10)60021-X. [DOI] [PubMed] [Google Scholar]
- 23.Bureau of Labor Statistics. Consumer Price Index. United States Department of Labor; 2013. http://data.bls.gov/timeseries/CUUR0000SAM. [Google Scholar]
- 24.Luce B, Manning W, Siegel J, Lipscomb J. Chapter 6: Estimating Costs in Cost-Effectiveness Analysis. In: Gold M, Siegel J, Russell L, Weinstein M, editors. Cost-Effectiveness in Health and Medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 25.Buntin MB, Zaslavsky AM. Too much ado about two-part models and transformation? Comparing methods of modeling Medicare expenditures. J Health Econ. 2004;23(3):525–542. doi: 10.1016/j.jhealeco.2003.10.005. [DOI] [PubMed] [Google Scholar]
- 26.Dormann CF, Elith J, Bacher S, et al. Collinearity: a review of methods to deal with it and a simulation study evaluating their performance. Ecography. 2013;36(1):27–46. [Google Scholar]
- 27.Cho SK, Egorova NN. The association between insurance status and complications, length of stay, and costs for pediatric idiopathic scoliosis. Spine. 2015;40(4):247–256. doi: 10.1097/BRS.0000000000000729. [DOI] [PubMed] [Google Scholar]
- 28.Glick AF, Tomopoulos S, Fierman AH, Trasande L. Disparities in Mortality and Morbidity in Pediatric Asthma Hospitalizations, 2007 to 2011. Acad Pediatr. 2016;16(5):430–437. doi: 10.1016/j.acap.2015.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Fleming-Dutra KE, Shapiro DJ, Hicks LA, Gerber JS, Hersh AL. Race, otitis media, and antibiotic selection. Pediatrics. 2014;134(6):1059–1066. doi: 10.1542/peds.2014-1781. [DOI] [PubMed] [Google Scholar]
- 30.Sarpong EM, Miller GE. Narrow- and Broad-Spectrum Antibiotic Use among U.S. Children. Health Serv Res. 2015;50(3):830–846. doi: 10.1111/1475-6773.12260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fronstin P. Sources of health insurance and characteristics of the uninsured: analysis of the March 2012 Current Population Survey. EBRI issue brief / Employee Benefit Research Institute. 2012;(376):1–34. [PubMed] [Google Scholar]
- 32.Flores G, Abreu M, Schwartz I, Hill M. The importance of language and culture in pediatric care: case studies from the Latino community. J Pediatr. 2000;137(6):842–848. doi: 10.1067/mpd.2000.109150. [DOI] [PubMed] [Google Scholar]
- 33.Lion KC, Wright DR, Spencer S, Zhou C, Del Beccaro M, Mangione-Smith R. Standardized Clinical Pathways for Hospitalized Children and Outcomes. Pediatrics. 2016;137(4) doi: 10.1542/peds.2015-1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lindholm M, Hargraves JL, Ferguson WJ, Reed G. Professional Language Interpretation and Inpatient Length of Stay and Readmission Rates. J Gen Intern Med. 2012 doi: 10.1007/s11606-012-2041-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hampers LC, Cha S, Gutglass DJ, Binns HJ, Krug SE. Language Barriers and Resource Utilization in a Pediatric Emergency Department. Pediatrics. 1999;103:1253–1256. doi: 10.1542/peds.103.6.1253. [DOI] [PubMed] [Google Scholar]
- 36.Karliner LS, Kim SE, Meltzer DO, Auerbach AD. Influence of language barriers on outcomes of hospital care for general medicine inpatients. J Hosp Med. 2010;5(5):276–282. doi: 10.1002/jhm.658. [DOI] [PubMed] [Google Scholar]
- 37.Porter M, Diaz VA, Gavin JK, et al. Cost and Utilization: Hospitalized Patients on a Family Medicine Service. Southern medical journal. 2015;108(6):364–369. doi: 10.14423/SMJ.0000000000000293. [DOI] [PubMed] [Google Scholar]
- 38.Duquette S, Soleimani T, Hartman B, Tahiri Y, Sood R, Tholpady S. Does Payer Type Influence Pediatric Burn Outcomes? A National Study Using the Healthcare Cost and Utilization Project Kids’ Inpatient Database. Journal of burn care & research : official publication of the American Burn Association. 2015 doi: 10.1097/BCR.0000000000000290. [DOI] [PubMed] [Google Scholar]
- 39.Stone ML, LaPar DJ, Mulloy DP, et al. Primary payer status is significantly associated with postoperative mortality, morbidity, and hospital resource utilization in pediatric surgical patients within the United States. Journal of pediatric surgery. 2013;48(1):81–87. doi: 10.1016/j.jpedsurg.2012.10.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.