Abstract
Emerging evidence suggests that the enzymes in the biosynthetic pathway for the synthesis of heparan sulfate moieties of heparan sulfate proteoglycans (HSPGs) are epigenetically regulated at many levels. As the exact composition of the heparan sulfate portion of the resulting HSPG molecules is critical to the broad spectrum of biological processes involved in oncogenesis, the epigenetic regulation of heparan sulfate biosynthesis has far-reaching effects on many cellular activities related to cancer progression. Given the current focus on developing new anti-cancer therapeutics focused on epigenetic targets, it is important to understand the effects that these emerging therapeutics may have on the synthesis of HSPGs as alterations in HSPG composition may have profound and unanticipated effects. As an introduction, this review will briefly summarize the variety of important roles which HSPGs play in a wide-spectrum of cancer-related cellular and physiological functions and then describe the biosynthesis of the heparan sulfate chains of HSPGs, including how alterations observed in cancer cells serve as potential biomarkers. This review will then focus on detailing the multiple levels of epigenetic regulation of the enzymes in the heparan sulfate synthesis pathway with a particular focus on regulation by miRNA and effects of epigenetic therapies on HSPGs. We will also explore the use of lectins to detect differences in heparan sulfate composition and preview their potential diagnostic and prognostic use in the clinic.
Keywords: biomarkers, biosynthetic pathways, enzymatic modification, epigenetic regulation, glycosylation, heparan sulfate proteoglycans, lectin arrays, sulfation
1. Introduction
1.1. Structure and Types of Heparan Sulfate Proteoglycans (HSPGs)
Heparan sulfate proteoglycans (HSPGs) are a diverse group of glycoproteins composed of one or more chains of heparan sulfate (HS) covalently bound to a core protein through a tetrasaccharide bridge. HSPGs vary considerably in molecular mass, from ~10 to over 400 kDa (as reviewed in [1]) depending on the nature of the core protein as well as the number and length of HS chains. There is limited diversity in the protein core structure [2], with most variability observed within the HS chains. More than 25 enzymes have been identified that are involved in HS synthesis and modification [3]. Due to their sulfation, the HS chains are negatively charged and can bind to many different ligands at the cell surface, within the extracellular matrix, and within the plasma [4]. HSPGs can be broadly classified into three main categories depending on their cellular/tissue location: (1) plasma membrane-associated; (2) secreted into the extracellular matrix; and (3) within secretory vesicles (as reviewed in [1]).
The major plasma membrane-associated HSPGs are the syndecans and the glypicans [1,4,5]. Structurally, the syndecans (syndecan-1, -2, -3, and -4) are transmembrane proteins composed of an N-terminal signal sequence, an ectodomain, a hydrophobic transmembrane domain, and a short C-terminal cytosolic tail. The addition of the HS chain occurs post-translationally on a serine residue. In contrast to syndecans, glypicans are not transmembrane glycoproteins but are extracellularly attached to the membrane via a glycosylphosphatidylinositol (GPI) anchor. There are six glypican family members (GPC1–6) that can be further classified into two subfamilies: GPC1/2/4/6 and GPC3/5 based on sequence similarity. Structurally, glypicans contain a hydrophobic domain at the C-terminus, allowing for the attachment of the protein to the GPI anchor. Unlike the syndecans, the HS chains on glypicans are covalently bound near the C-terminus, resulting in chains which are very close to the cell surface and can be liberated from the cell by lipase activity [6,7]. Most of the GPI-anchored glypicans are found within lipid rafts on the apical side of the cell [8,9,10], but this is not exclusive. Minor membrane-associated HSPGs, also known as “part-time HSPGs”, include betaglycan, neuropilin-1, and CD44v3 and are single-pass transmembrane receptors. Betaglycan, also known as transforming growth factor β receptor III (TGFβR3), contains either heparan sulfate (HS) or chondroitin sulfate (CS) chains and functions as a co-receptor for the TGFβ superfamily [11,12]. Neuropilin-1 also contains either HS or CS chains and functions as a mediator of angiogenesis and axonal guidance by regulating cellular responses to vascular endothelial growth factor (VEGF) [13,14,15] and semaphorins [16]. CD44v3, a splice variant of CD44, is an HS-containing transmembrane receptor for hyaluronan and has been shown to promote tumor growth and metastasis in breast cancer [17] and head and neck squamous cell carcinoma [18,19].
The second category of HSPGs are those secreted into the extracellular matrix (ECM). These include perlecan, agrin, and collagen XVIII, which are all large, multidomain proteins (reviewed in [1,20,21]). Perlecan, synthesized and secreted by endothelial and vascular smooth muscle cells, binds and cross-links various ECM and cell-membrane components. The HS chains are bound to perlecan at the N-terminal domain. Binding of HS chains to perlecan is not required for proper protein folding or secretion, but decreases in number and/or sulfation has been shown to reduce perlecan function. Agrin is secreted by neuronal cells into the ECM and is important in the formation of the neuromuscular junction during embryogenesis. Agrin contains up to three heparan sulfate attachment sites, although most studies have shown that only two HS chains are typically found on the secreted form. Collagen XVIII, a ubiquitously expressed component of basement membranes, has a C-terminal domain known as endostatin that functions to inhibit angiogenesis and tumor growth when cleaved.
The last category of HSPGs are those found within secretory vesicles. At this time, the only characterized proteoglycan within this category is serglycin. Serglycin is primarily expressed in hematopoietic and endothelial cells and serves an important role in formation and retention of inflammatory mediators inside storage granules and secretory vesicles [1,22].
1.2. General Functions of HSPGs
A major determinant of HSPG function is the pattern of glycosylation and sulfation of the HS chains, which is highly controlled by the cells/tissues expressing the HSPG [3]. The ligands that HSPGs bind are also quite varied and include, but are not limited to, cell surface receptors, extracellular matrix proteins, growth factors, cytokines and morphogens (reviewed in [21]).
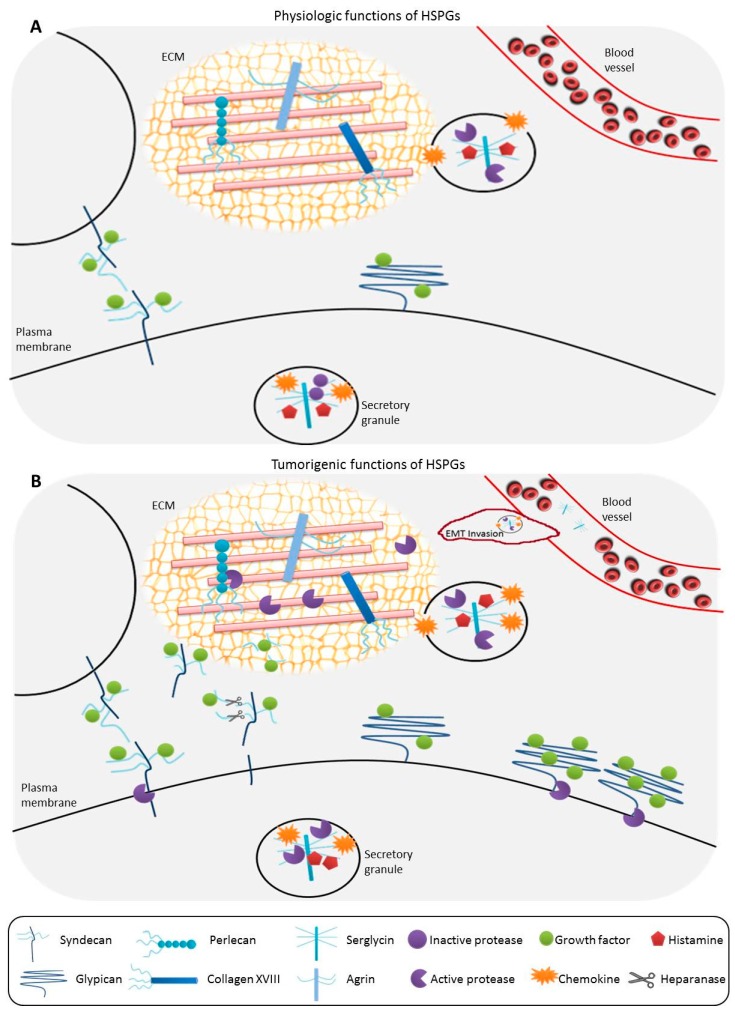
Due to the large diversity in HSPGs and their ligands, it is naturally unsurprising that the collective functions ascribed to HSPGs are just as numerous (as reviewed in [1,23,24]). HSPGs are involved in the development of the basement membrane barrier, providing a framework for epithelial support, regulating transport of solutes, and promoting the extravasation of cells during inflammatory responses [23,25,26,27]. HSPGs that are located at the cell surface are also involved in the establishment of morphogen and chemokine gradients important in WBC extravasation, but are also vital during development [28,29,30]. HSPGs located within secretory vesicles are involved in the packaging of vesicular contents, maintenance of protease activity, and regulating various activities upon secretion, such as host defense mechanisms and wound repair (e.g., [22,31,32,33]). Membrane-associated HSPGs are also involved as receptors or coreceptors on the cell surface promoting a variety of activities: (1) they can function as coreceptors for growth factor receptors, mediating signal transduction pathways (e.g., [34,35,36]); (2) they can function as endocytic receptors, facilitating the transcytosis and/or clearance of lipoproteins [37,38] and promoting exosome uptake [39,40]; (3) they can cooperate with cell adhesion molecules, such as integrins, to affect cellular migration (e.g., [27,41,42]); (4) they can bind to and regulate the activity of matrix metalloproteases within the ECM (e.g., [43]); and (5) they can act to mediate cytokine-induced signal transduction pathways (e.g., [44,45]) (Figure 1A). Given how many essential cellular and developmental processes involve the activity of HSPGs, it is not surprising that modifications or alterations in HSPG structure could impart a dysregulation in function and potentially lead to the development of cancer (Figure 1B).
Figure 1.
(A) Under physiologic conditions, syndecans are located at the cell surface, functioning as growth factor receptors and are important for cell-to-cell communication. Glypicans are also located at the cell surface, attached to the membrane through a glycosylphosphatidylinositol (GPI) anchor, and function as growth factor receptors. Perlecan, agrin, and serglycin are found within the extracellular matrix (ECM) and aid in the formation and structural integrity of the ECM barrier. Serglycins are the only intracellular heparan sulfate proteoglycans (HSPGs), found in secretory granules with chemokines and histamine, and function in maintaining proteases in their inactive form. Upon secretion, serglycins activate ECM proteases and are important in regulation of host defenses and wound repair; (B) In tumorigenesis, syndecans can be proteolytically cleaved, and these soluble syndecans can sequester growth factors in the ECM. Heparanases can cleave HS chains, which can also bind and complex with growth factors in the ECM. Glypican expression at the cell surface is often upregulated, resulting in increased growth factor binding and uptake which mediates tumor cell growth. Tumor cells have increased serglycin secretion, causing enhanced protease activity, facilitating ECM breakdown that promotes tumor invasiveness and metastasis.
1.3. Alterations of HSPGs Serving as Biomarkers in Cancer
Several HSPGs have been shown to be upregulated in many cancers and can serve as biomarkers for cancer diagnosis and/or prognosis. As one example, neuropilin-1 has been shown to be a prognostic indicator for tumor metastasis in oral squamous cell carcinoma [46], prostate cancer [47], and malignant melanoma [48]. However, the remodeling of HSPGs through enzymatic modification of HS chains is associated with malignant transformation of cells, and can potentially serve as molecular biomarkers to aid in the diagnosis and prognosis of cancer. Alterations in glycosylation of HSPGs can facilitate the metastasis of cancer cells by affecting cellular adhesion. As one example, Ferguson and Datta reported that activity of heparan sulfate 2-O-sulfotransferase (2OST) was critical in invasion of LNCaP-C4-2B prostate cancer cells [49]. In their study, they documented increases in E-cadherin and actin expression at the cell surface upon 2OST knockdown, indicating stable adherens junction formation. Additionally, activity of 2OST was increased in response to stress-inducible transcription factors, which these authors hypothesize would be elevated in cancer progression.
One of the first reports indicating that structural alterations in glycosylation can result in tumorigenesis is in hereditary multiple exostosis and chondrosarcoma [50]. Most of these cases arise due to mutations in the exostosin (EXT) genes EXT1 and EXT2, encoding enzymes involved in biosynthesis of heparan sulfate [51], and further work demonstrated that these mutations interfere with proper glycosylation and function of HSPGs [52]. Since these early reports, numerous studies have been published that provide evidence of structural alterations of HSPGs and development of cancer. In a recent study by Jao et al. [53] using a mouse knockout model, they showed that loss of N-deacetylase and N-sulfotransferase 4 (NDST4), an enzyme involved in HS sulfation, may result in tumorigenesis and progression of colorectal cancer. As reviewed in [54], a loss of syndecan-1 is associated with a decrease in E-cadherin expression, which can alter the adhesion and migration properties in some tumors; this loss of syndecan-1 is associated with accelerated tumor progression and poor prognosis in head and neck, lung, and colorectal cancer. Glypican-3 (GPC3) is well characterized as a negative regulator of cell growth and functions as a tumor suppressor protein. Several studies have shown that aberrant expression of GPC3 in hepatocellular carcinoma [55,56] and urothelial cancer [57] can serve as a biomarker for diagnosis and prognosis. Wade et al. [58] reported that alterations in activity of the sulfatase enzymes SULF1 and SULF2 promote receptor tyrosine kinase signaling and progression in glioblastoma, and suggest that these alterations “are promising biomarkers for disease and therapeutic targets.” Not only can alterations occur between cancerous and non-cancerous cells, Fernandez-Vega et al. [59] reported that HS modifications may also be different in right-sided colorectal cancer (CRC), depending on the stage of the tumor. They reported increased expression of five genes encoding HSPG-modifying enzymes (See Table 1) between normal and non-metastatic CRC tissue, but when comparing normal tissues with metastatic CRC tissue, these same five genes were not differentially expressed. In total, less than 20% of the genes involved in HSPG biosynthesis were differentially expressed in metastatic tumors versus nearly 40% in non-metastatic tumors [59], allowing for the potential of these genes to serve as biomarkers for staging of colorectal cancer.
Table 1.
Heparan sulfate proteoglycan (HSPG) enzymes involved in tumor progression.
| Enzyme | Major Function | Expression Change | Possible Therapeutic Targeting | Type(s) of Cancer | References |
|---|---|---|---|---|---|
| XYLT1/2 | Addition of xylose to a serine on a core HSPG to initiate HS chain synthesis | Up | shRNA targeting of XYLT1; DNA methylating agents | Breast cancer/bone metastasis; breast cancer associate fibroblasts; multidrug resistance | [66,179,180] |
| B4GALT1 | Formation of the β 4 xyl-gal linkage | Varied | 5-Aza-dC treatment; estrogen receptor blockers | Colon cancer; breast cancer | [68,69,70,181,182,183] |
| B3GALT6 | Formation of the β 3 gal-gal linkage | Up | Liver X receptor agonists | Colon cancer | [184] |
| B3GAT3 | Catalyzes the β 3 glc-gal linkage | Up | DNA methylating agent | Multidrug resistance | [66] |
| EXT1/2 | Catalyzes the addition of both α-d-glucoronate (GlcA) and GlcNAc during HS chain elongation | Varied | 5-Aza-dc treatment | Osteochondromas, cholangiocarcinoma, leukemia | [89,90] |
| EXTL1/2/3 | Adds the required N-acetyl-d-Glucosamine (GlcNAc) for elongation of the HS chain | Down | 5-Aza-dc treatment; siRNA | Colon cancer | [185] |
| NDST1-4 | Replaces the N-acetyl groups (GlcNAc) with N-sulfate groups (GlcNS) on a glucosamine residue | Varied | 5-Aza-dc treatment; miRNA interference | Colon cancer (NDST4); breast cancer | [101,112,113,177] |
| GLCE | Converts glucuronic acid (GlcA) to its epimer iduronic acid | Varied | Cancer-type dependent; ectopic overexpression improves breast and lung cancer prognosis, while overexpression is associated with increased aggressiveness in prostate cancer | Breast cancer; lung cancer; prostate cancer | [93,116,117,118,119,120] |
| HS2ST1 | Mediates 2-O-sulfation of both l-iduronyl and d-glucuronyl residues within the maturing HS | Up | Heparin treatment; histone methyltransferase inhibitor | Breast cancer; multiple myeloma | [186,187,188] |
| HS6ST1-3 | Catalyzes the transfer of sulfate from 3-Phosphoadenosine 5-Phosphosulfate (PAPS) to position 6 of the N-sulfoglucosamine residue (GlcNS) of heparan sulfate | Up | HS6ST inhibitors and HS mimetics | Ovarian cancer; breast cancer; pancreatic cancer | [59,189,190,191] |
| HS3ST1-6 | Utilizes 3-phospho-5-adenylyl sulfate (PAPS) to catalyze the transfer of a sulfo group to position 3 of glucosamine residues in heparan | Down | 5-Aza-dc treatment | Breast cancer; invasive ductal carcinomas; chondrosarcoma | [59,110,134,135,136,177,192] |
| SULF1 | Selectively removes 6-O-sulfate groups from HS chains | Varied | HS mimetic (PI-88); 5-Aza-dc treatment; miRNA interference | Multiple cancers | [193,194,195] |
| SULF2 | Selectively remove 6-O-sulfate groups from heparan sulfate | Up | Sulf inhibitors (OKN-007); proteasome inhibitors (bortezomib); HS mimetic (PI-88) | Multiple cancers | [154,193,194] |
| HPSE | Cleaves heparan sulfate proteoglycans to permit cell movement through remodeling of the extracellular matrix | Up | Roneparstat; miRNA interference; estrogen receptor antagonists | Multiple myeloma; brain cancer; breast cancer; colon cancer | [173,174,175,176,196,197] |
| HPSE2 | Binds heparin and heparan sulfate with high affinity, but lacks heparanase activity | Down | Prognostic biomarker as elevated HPSE2 is correlated to improved outcomes | Breast cancers; head and neck cancers | [177,198] |
Based on the compilation of reports documenting HSPGs and their influence in tumorigenesis, it is now accepted that structural alterations in the HS chains, typically assessed using antibody-based techniques, can serve as biomarkers for various cancers. Normal HS biosynthesis is variable and highly regulated within tissues, allowing for coordinated cellular responses to ligand binding; these processes can be commandeered by cancer cells, resulting in changes to the structure, degree of expression, and/or function of HSPGs within cancer cells [4]. As Kreuger and Kjeller [60] point out: “The key to understanding the function of HSPGs [and their utility as biomarkers] is to clarify how HS biosynthesis is regulated in different biological contexts.” The following sections will address the regulation of HS biosynthesis in the context of cancer.
2. Heparan Sulfate Biosynthetic Pathway
2.1. Synthesis of the Serine-Linked Tetrasaccharide Linker
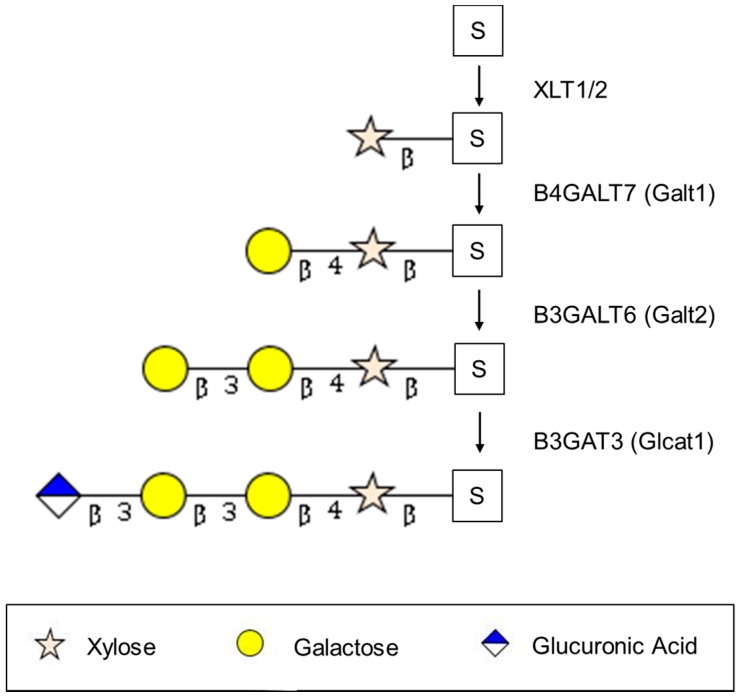
All HS moieties are linked to a serine residue on the core protein by a tetrasaccharide (Xyl-Gal-Gal-GlcA). The initial and apparently rate limiting step in HS chain synthesis is the addition of xylose (catalyzed by Xylt1/2 or XYLT1/2) to a serine on the core protein [61,62]. Little is known about the subsequent three enzymes in the synthesis of this tetrasaccharide linkage. Most recent reviews present these enzymes as Galt1/2 and Glcat1 but these names are non-standard. The formation of the β-4 xyl-gal linkage (described as Galt1) can be catalyzed by a family of seven β-4 galactosyl transferases (B4GALT) which transfer galactose to a variety of sugars including xylose but B4GALT7 appears to predominate [63]. The formation of the β-3 gal-gal linkage (described as Galt2) is more appropriately known as B3GALT6 while the enzyme catalyzing the β-3 glc-gal linkage is catalyzed by B3GAT3 [64,65].
Although likely related to other glycosylation pathways, enzymes catalyzing identical linkages have recently been linked to cancer, and are of therapeutic interest because they have been demonstrated to be epigenetically regulated. For example, XYLT1, B3GALT6, and B3GAT3 were all found to be hypomethylated in multi-drug resistant A549 lung cancer cells compared to progenitor A549 cells [66]. Similarly, B3GALT4, closely associated with ganglioside biosynthesis, has been linked to neuroblastoma tumors in a genome-wide methylation screen [67]. B4GALT1 has been found to be hypermethylated in invasive colorectal cancers, and was shown to be re-expressed upon treatment with the DNA methyltransferase inhibitor 5-Aza-dc [68,69]. Conversely, in breast cancer, estrogen-induced expression of B4GALT1 is associated with enhanced breast cancer cell proliferation, and thus estrogen receptor agonists have been suggested as a potential therapeutic approach [70]. These seemingly opposing roles of B4GALT1 highlight the context-dependence of HSPG regulation and function.
2.2. Elongation of the Tetrasaccharide Linker to Form the HS Chain: Exostosin Family
The 5-member exostosin family of genes, which consists of exostosin (EXT) and exostosin-like (EXTL) genes, is required for elongation of the tetrasaccharide core. Although there is some confusion about the possible redundancy and overlapping function of these enzymes in cell lines [71,72,73], the importance of the family is illustrated by the disparate genetic disorders which are associated with mutations in exostosin gene family members [74,75]. Evidence from in vitro experiments suggests that EXTL2 is the key enzyme for the initiation of elongation of the linker tetrasaccharide, adding the required N-acetyl-d-glucosamine (GlcNAc) [76] and may control HSPG biosynthesis [77,78]. EXTL3 (uniprot entry O43909) appears to have identical enzymatic activity by similarity with EXTL2 [79]. As with the EXTL2/3, EXTL1 also only adds GlcNAc residues to the growing chain. Unlike the exostosin-like (EXTL) family members, EXT1/2 catalyze the addition of both α-d-glucoronate (GlcA) and GlcNAc [80] and are therefore required for the addition of at least every other monosaccharide in the growing chain. As EXT2 does not harbor significant glycosyltransferase activity in the absence of EXT1, the EXT1/2 heterooligomeric complex localized in the Golgi is essential for the polymerization of HS [81], although recent data suggest that EXT1 deficient cells may produce shorter HS chains [82]. In vivo, mutations in EXT1, -2 or -3 lead to Multiple Hereditary Exostoses, a disease that starts with benign outgrowths termed exostoses or osteochondromas, which may develop into chondrosarcomas [75,83,84]. Interestingly, the condition may be modeled in mice and potentially treated with bone morphogenic protein [85]. However, EXT2 is also associated with seizures-scoliosis-macrocephaly syndrome without exostoses [86] while mutations in EXTL3 are linked to skeletal abnormalities and neurodevelopmental defects with severe combined immunodeficiency in some cases [74,87,88].
EXT1 is the first of several enzymes in the HS biosynthetic pathway for which strong evidence for epigenetic regulation exists. As EXT1 plays a fundamental role in the elongation of HS chains, the epigenetic regulation of this enzyme has the capacity to affect many downstream HS functions, and impact carcinogenesis. EXT1 is hypermethylated in leukemia (especially acute promyelotic leukemia and acute lymphoblastic leukemia) and nonmelanoma skin cancer in a screen of 454 primary tumors of different types and 79 human cancer cell lines, implying that epigenetic regulation of EXT1 is linked to oncogenesis [89]. Epigenetic silencing of EXT1 by hypermethylation in the promoter region results in loss of HS synthesis and promotes tumor progression in cancer cells, which can be reversed by a DNA demethylating agent [89]. Recently, however, EXT1 was found to be elevated in the liver and plasma of an animal model of cholangiocarcinoma (CCA) [90]. The fact that EXT1 levels rose as early as 1 month before tumor development, and that it was also found to be elevated in the plasma of human patients with CCA, indicate that it might be useful as an early diagnostic biomarker of the disease.
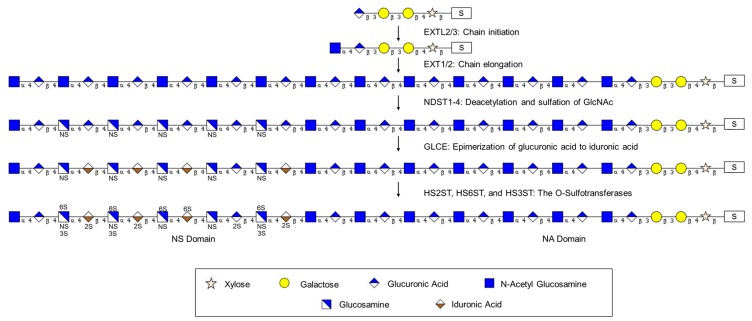
2.3. Modification of the HS Chain: Formation of Domains
The HS chain that results from the activity of the combined exostosin protein activities is a repeating dimer of glucoronic acid and N-acetylglucosamine residues. This chain is then modified in a series of sequential steps and involves four separate sulfation reactions and conversion of d-glucuronic acid residues to l-iduronic acid. The combined activities of these enzymes result in a clustering of modifications into N-sulfated regions (NS domains) and non-sulfated regions rich in GlcNAc (NA- or N-acetylated domains). NS domains consist of sulfated regions containing GlcNAc, GlcA, and IdoA in contrast to the NA domains, which are non-sulfated regions composed of GlcNAc and IdoA. The activity of these enzymes is thought to be determined by cell type so that a core protein may be modified differently in a tissue-specific fashion [91,92,93]. As several of these modification enzymes are subject to epigenetic regulation, the modification of HS chains may be modulated therapeutically [92,93].
2.3.1. Modification of the HS Chain: Glucosaminyl N-Deacetylase/N-Sulfotransferases (NDSTs)
This family of four enzymes with two subtypes NDST1/2 and NDST3/4 with overlapping but distinct specificities and functions is necessary for the modification of the HS chain [94,95,96]. The enzymes are bifunctional and remove an N-acetyl group from glucosamine (GlucNAc), replacing it with a sulfo group to form N-sulfated heparosan, the substrate for subsequent modifications in the HSPG biosynthetic pathway [96]. Specifically, cells not expressing NDST1 or -2 may be 6-O-sulfated but not modified by 2-O- or 3-O-sulfotransferases. Overexpression or deletion of members of this family alters the composition of the HS on HSPG [97,98] and it has been suggested that some initiate HS modification/sulfation reactions, whereas others later on fill in or extend already modified HS sequences [94]. NDST2 knockout mice have defects in mast cell proteases [99,100] which can mold the tumor microenvironment. Recently, NDST4 was identified as a tumor suppressor linked to colorectal cancer [101]. Consistent with its role in colon cancer [101], mice deficient in NDST4 show altered development and homeostasis of the colonic epithelium [53] and this locus is linked to circulating resistin levels [102]. Interestingly, NDST4 has also been associated with reading disability and language impairment [103], mirroring the autosomal recessive intellectual disability linked to NDST1 [104,105] and schizophrenia and bipolar disorder linked to NDST3 [106,107]. Additional links between genes of this family and cancer may be delineated in the future as NDSTs may determine length of the HS chain [108] and are considered to be key in forming domains within the HSPG that are fundamental to determining protein interactions [95,104,105,109].
The potential tumor suppressive qualities of NDSTs [101] underscore the growing interest in modifying their expression via manipulation of their epigenetic regulation. Treatment of H-HEMC-SS chondrosarcoma cells with 5-Aza-dc decreased NDST1 promoter methylation, increasing NDST1 mRNA expression, and reducing their proliferative and invasive properties [110]. However, methylation-dependent regulation of NDST1 is cell type dependent. In prostate cancer cells, NDST1 expression was increased following 5-Aza-dc treatment in androgen-dependent non-metastatic LNCaP cells, but was unaffected in the androgen-independent metastatic PC3 cell line [93].
NDST1 expression can also be epigenetically regulated via direct microRNA (miRNA) targeting, but the influence of miRNA-dependent regulation of NDST1 expression on cancer prognosis and progression seems to be context dependent (e.g., affected by experimental conditions, cancer and cell type). For example, in the gastric carcinoma cell line MGC803, miR-191 targeting of NDST1 suppresses apoptosis and promotes cancer cell growth [111]. However, in HUVEC cells, the downregulation of NDST1 by miR-24 reduced HS chain formation and the chemotactic response to growth factor treatment [112]. Similarly, the de-repression of NDST1 following the downregulation of its targeting miRNA, miR-149 was associated with chemoresistance and an unfavorable diagnosis in Her2-positive and basal breast cancers [113]. Interestingly, in this study, control of miR-149 expression was shown to be methylation dependent adding yet another layer to NDST1 epigenetic control.
2.3.2. Modification of the HS Chain: d-Glucuronyl C5-Epimerase (GLCE)
By changing the stereochemistry of the C5 chiral center, this step converts d-glucuronic acid residues adjacent to N-sulfate sugar residues in heparosan-N-sulfate to l-iduronic acid residues in the maturing HS chain [114]. This is important for further modifications that determine the specificity of interactions between these glycosaminoglycans and proteins as this step is required for the formation of NS-domains (N-sulfated disaccharide units) which are distinct from NA domains (N-acetylated disaccharide units) and are key for associations of proteins. There is some interplay between GLCE, exostosin, and HS2ST activity as overexpression of GLCE increased HS chain length but this effect was abolished by simultaneous overexpression of HS2ST and this was not seen with expression of mutant GLCE [115].
The dysregulation of GLCE expression has been observed in many cancer types, but its exact role in cancer progression is not clear. In breast and lung cancers, GLCE has a demonstrated anti-proliferative effect, but its overexpression in prostate cancer cells is associated with a much more aggressive phenotype [116,117,118]. In breast cancer cells, epigenetic regulation of GLCE is thought to be dependent on chromatin structure and not DNA methylation as GLCE expression was significantly increased following histone deacetylase (HDAC) inhibitor treatment, but was unaffected by 5-Aza-dc treatment [119]. Conversely, in prostate cancer cells, GLCE dysregulation appears to be largely mediated via aberrant GLCE promoter methylation, which varies dramatically between prostate cancer cell types and has been proposed to be a potential contributor to intratumor heterogeneity [120].
2.3.3. Modification of the HS Chain: The O-Sulfotransferases HS2ST, HS6ST, and HS3ST
Heparan sulfate chains are sequentially modified by sulfation on C2, C6, and C3 by three different families of sulfotransferase enzymes (HS2ST, HS6ST, and HS3ST, respectively). As there are multiple isoforms of the HS6ST and HS3ST enzymes, a total of eleven sulfation enzymes exist which leads to variability in sulfation during HS biosynthesis. HS2ST catalyzes the sulfation on the C2 of both l-iduronyl (IdoA) and d-glucuronyl (GlcA) acid residues with a strong preference for IdoA [121]. HS2ST is required for Erk/Mapk signaling and knockout mice are perinatal lethal, potentially due to increased sulfation on other carbons, maintaining the level of HS sulfation and charge [122,123,124]. As HS3ST requires that the HS chain be previously modified by HS2ST, any compensatory sulfation must be catalyzed by HS6ST which does not require prior 2-O-sulfation. Thus, although 2-O-sulfation appears to be largely restricted to NS-domains while 6-O-sulfation is seen in domains with and without N-sulfation [125]. HS6ST may partially substitute for a lack of HS2ST activity, an activity that is key to maintaining growth factor binding sites [122,123]. In addition, as the 6-O-sulfations of heavily sulfated NS-domains [126,127] are targets of both SULF1 and SULF2 (see below), the binding domains for growth factors and other proteins may be edited after synthesis is complete. The family of seven HS3ST isoenzymes are thought to catalyze the rate limiting step in sulfation, producing either antithrombin III or herpes simplex binding envelope protein binding sites [128,129]. However, this site classification is undoubtedly simplistic. 3-O-sulfatation was recently shown to enhance Wnt binding [130] and other binding sites are likely to follow.
Although sulfation is thought to be extremely important in determining the binding of associated proteins, much remains to be determined about the importance of variations in sulfation patterns in cancer. In prostate cancer, stress-induced transcription factors increase transcription of HS2ST to increase metastatic potential [49] and the 2-O-sulfate modification is linked to angiogenesis [131]. Expression of the HS3ST3B1 isoform of the 3-O-sulfotransferase has been shown to regulate breast cancer invasiveness [132]. Interestingly, the anticoagulant heparin is much less sulfated, at 0.8 sulfates per disaccharide rather than the typical HS chain at 2.3 per disaccharide [1] but despite this, there is a large degree of overlapping specificity in protein binding between heparan and heparin [133]. Thus, much more work is needed in order to understand how this large family of sulfation enzymes functions to regulate HS structure and function.
There is currently a paucity of data regarding the epigenetic regulation of O-sulfotransferases, though evidence is starting to suggest its relative importance in cancer. In addition to genes involved in initiation of HS chain formation, several O-sulfotransferases (HS3ST1, HS3ST2, HS3STSA1, HS3ST3B1) were also found to be hypomethylated in multidrug resistant A549 lung cancer cells compared to the A549 progenitor cells [66], though the downstream effects of this hypomethylation remain uninvestigated. In H-EMC-SS chondrosarcoma cells hypermethylation, and thus decreased expression of the 3-O-sulfotransferases HS3ST1, HS3ST2, HS3ST3A1 was associated with a more invasive phenotype [134]. Importantly, treatment with 5-Aza-dc restored both 3-O-sulfotransferase gene expression and HS sulfation patterns, and reduced the proliferative and invasive capacity of the chondrosarcoma cells [110]. Similar patterns of hypermethylation of HS3ST2 and increased tumor invasiveness have also been observed in lung and bladder cancers indicating substantial tumor suppressive properties associated with proper HS3ST2 function and HS chain sulfation [135,136].
2.4. Summary of Modification of the HS Chain: Complexity, Redundancy, and Protein Interactions
Several authors have proposed complex regulatory interactions between proteins involved in HS biogenesis [71,115,137,138,139]. Esko and Selleck first suggested that a macromolecular GAGosome enzyme complex [140] may function to integrate the complex regulation of the enzymes in the HS biosynthetic pathway. This proposed complex may include the family of exostosin enzymes as the length of the HS chain may be regulated by NDST, a proposed member of the GAGosome [108], and there is increasing experimental evidence to support such a complex [115,141,142]. Recently, Zhang et al. have proposed that the enzymes involved in the modification of HS chains are tightly regulated to read and write a code involved to synthesize the appropriate HS [143]. Although this is an evolving story, the regulation of HS modification enzymes is likely to be key to the overall function of HSPG.
As the exact modification of the heparan sulfate moiety is key to its function, the binding of proteins to HSPG will also be greatly affected by the exact HS structure. For example, fibroblast growth factor (FGF) 1 and 2 binding to HS chains of differing composition varies with significant implications for signaling through FGF receptor [144] and this differential growth factor signaling has been proposed to have implications for cancer [145]. Differential binding of growth factors to HS chains may affect morphogenesis [29,146,147]. In addition, HS composition affects the activity of the complement cascade which affect inflammation [148] and unsubstituted glucosamine residues inhibit heparanase activity [149] which has been implicated in metastasis. Thus, given the potent pleotropic effects of HS composition on downstream events, it is not surprising that recent work has focused modulating the activity of HS modification enzymes and on screening for HS binding affinity [150].
3. Heparan Sulfate Modification and Degradation Enzymes
Once synthesized, the HS chain of an HSPG may be modified or degraded by extracellular enzymes. Modification involves removal of the sulfo group at the C6 position in regions of the HS chain by SULF1/2 to reduce signaling by heparin-dependent growth factors and tumor growth [151]. In addition, the HS chain may be shortened or degraded by heparanase (HPSE1/2) to functionally remove growth factor binding sites and affect cancer progression [152].
3.1. SULF1 and SULF2
These extracellular enzymes remove sulfo groups from the C6 position, reducing the overall sulfation (and negative charges) of HSPGs. As SULF1/2 modify the sulfate-rich NS domains more than the glucuronic acid-rich NA domains, the domains closely associated with growth factor binding are predominately altered [137,153]. Despite functional similarities between SULF1 and SULF2, the roles of these two enzymes in the pathogenesis of cancer seem to diverge. SULF1 has been shown to exhibit tumor suppressive properties in hepatocellular carcinomas (HCC), as well as breast and ovarian cancers [154,155], potentially acting by reducing growth factor binding and signaling in expressing cells [156,157]. In contrast, SULF2 has been shown to promote growth and metastasis of solid tumors [158]. However, upregulation of both SULF1 and SULF2 has been shown to be a poor prognostic indicator for gastric cancer patients [159]. In addition, expression of SULF1 or -2 has been shown to affect response to multiple cancer chemotherapeutics. In HCC, SULF1 induction has been shown to increase histone acetylation, and can potentiate the apoptotic effects of HDAC inhibitors [160] while SULF2 methylation is negatively associated with cisplatin sensitivity [161]. Conversely, in lung cancer, SULF2 methylation increases sensitivity to topoisomerase-I inhibitors by inducing IGS15 expression, subsequently enhancing the apoptotic response [158].
The expression of both SULF1 and SULF2 can be regulated by the degree of promoter methylation. Hypermethylation of SULF2 is associated with increased chemosensitivity and better survival of lung adenocarcinoma patients [158]. Contrarily, hypomethylation of SULF1 is commonly observed in HCC, but its expression can be restored with 5-Aza-dc treatment [155]. Interestingly, while SULF1 expression is unaffected by HDAC inhibition, restoration of SULF1 expression by 5-Aza-dc potentiated the response of HCC to HDAC inhibitor treatment compounding the growth suppressive apoptotic affects [160]. Thus, HCC may represent a cancer type in which combinatorial epigenetic therapies could be particularly effective.
SULF1 expression has also been demonstrated to be controlled by miRNA regulation as well. In gastric cancer patients, overexpression of miR-516-3p is associated with decreased SULF1 expression and increased survival [162]. However, in HCC, miR-21-mediated inhibition of SULF1 and PTEN promoted growth factor signaling and tumor progression [163]. Thus, as with the majority of modes of epigenetic regulation, the effects of miRNA-dependent control of SULF1 appear to be context and cell type dependent.
3.2. Heparanase
Heparanase (HSPE) is an endoglycosidase that participates in the degradation and remodeling of the HS portion of HSPGs and is overexpressed in many cancer types. HSPE is associated with increased cancer metastasis, chemoresistance, and reduced patient survival. The enzyme is selective for the glycosidic bond between a glucuronic acid and an N-sulfo glucosamine but not a 2-O-sulfated iduronic acid. This action particularly affects the NS domains rich in sulfated residues and alters the binding of growth factors and other proteins [164,165]. HSPE is essentially inactive at neutral pH [166] but is activated under acidic conditions, such as tumor invasion, hypoxia, and inflammatory processes, and it activates a variety of signaling pathways [167,168,169,170,171]. As such, small molecule inhibitors of heparanase, such as Roneparstat are under intense investigation. Promising work has recently demonstrated that Roneparstat treatment during or after chemotherapy can diminish tumor regrowth in multiple myeloma patients (ClinicalTrials.gov Identifier: NCT01764880) [172,173].
Significant evidence for HPSE epigenetic regulation exists as well. HPSE overexpression was shown to result from promoter hypomethylation in prostate cancer [174]. In neuroblastoma cells, HPSE overexpression is induced by the expression of miR-558, which increased cell growth and invasive capacity [175]. However, in breast cancer cells, miR-1258 targeting of HPSE reduced its expression and blocked in vitro cell invasion and metastasis [176].
Though the HPSE homolog HPSE2 also binds heparan with high affinity, it lacks heparanase activity and can thus competitively inhibit HPSE function. As such, HPSE2 has been suggested to have anti-metastatic features, and its strong downregulation in infiltrating ductal adenocarcinomas has led to its proposal as a diagnostic indicator [177]. Currently, no direct evidence of HPSE2 epigenetic regulation is available, but its expression was shown to be induced in vascular endothelial cells by homocysteine metabolites, which suggests a potential correlation between HPSE2 regulation and methyl-donor availability [178].
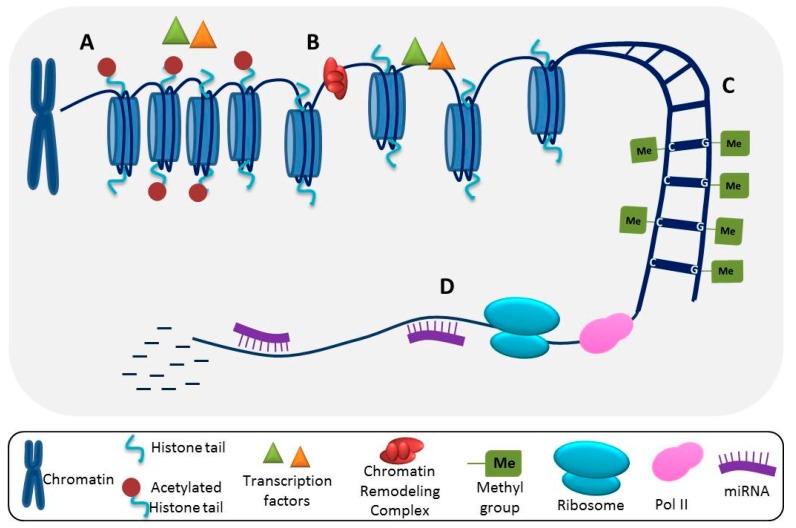
Figure 2 summarizes the synthesis of the tetrasaccharide linker, while Figure 3 summarizes the elongation and modification of the HS chain. Figure 4 illustrates how gene expression may be regulated by different epigenetic mechanisms. The epigenetic regulation of these enzymes in cancer is delineated in Table 1.
Figure 2.
The initial step in the synthesis of the heparan sulfate proteoglycan (HSPG) linker is the linkage of xylose to a serine residue in the core protein. Subsequent linkages are catalyzed by the family sugar transferases as indicated in the text.
Figure 3.
Initially, the EXT (exostosin) family of enzymes are responsible for heparan sulfate (HS) chain initiation and elongation from the serine residue (S) on a core protein. Deacetylation and sulfation of HS is performed by the NDST (N-deacetylase/N-sulfotransferase) family of enzymes. Enzymatic activity of GLCE (d-glucuronyl C5-epimerase) results in epimerization of glucuronic acid to iduronic acid on the HS chain. Finally, the HSxST family of enzymes (heparan sulfate O-sulfotransferases; x = 2, 3, or 6) catalyzes additional sulfation of the HS chain on C2, C3, and C6, respectively, within the NS domains.
Figure 4.
Several epigenetic mechanisms can lead to altered gene expression in tumor cells. (A) Histone acetylation results in tightly wound chromatin and inaccessibility of transcription factors to DNA; (B) Histone deacetylation and chromatin remodeling complexes promote the unwinding of chromatin complexes, allowing for transcriptional upregulation; (C) DNA can be methylated on C and G residues, which can lead to transcriptional repression; (D) Following transcription initiation by RNA polymerase II (Pol II), miRNAs can prevent protein translation by either blocking translocation of ribosomes down the mRNA transcript or by directing mRNA degradation.
4. Conclusions and Future Directions
Given the roles of HS signaling in oncogenesis, and interactions with the tumor microenvironment, one can begin to appreciate how components of this pathway may provide a novel set of targets for cancer diagnostics and therapeutics. The fact that many of the genes involved in HS biosynthesis are epigenetically regulated makes them particularly attractive targets, but as illustrated above, conventional epigenetic therapies, such as DNA demethylase and histone deacetylase inhibitors, may not prove particularly successful as their effects are both cancer and cell type specific. Furthermore, these types of broad-spectrum inhibitors impact far more than a given gene of interest, which can both lead to severe side effects and result in worsening outcomes [199,200].
Targeting a precise gene of interest then could improve specificity and therapeutic efficacy. However, HS biosynthesis and cancer progression are multi-faceted processes in which a number of genes can be dysregulated, often at the same time, thus a single gene candidate may not be able to be pinpointed. For example, multiple genes involved in HS biosynthesis have been shown to be differentially expressed between normal and malignant human plasma cells [186,201]. Adding to this complexity, differential transcription patterns of HS biosynthetic enzymes have been identified between cancer cells from the same type of cancer [93]. Furthermore, even targeted upregulation of a given HS biosynthetic enzyme has been demonstrated to differentially affect the expression of other HS metabolic enzymes in distinct cell types derived from the same cancer [42,64,65,93]. Another approach then might be to take advantage of the fact that these changes in transcription patterns can lead to specific glycosignatures that can then be recognized and targeted.
Ultimately, the end products of these enzymatic processes are what are impacting the cellular events that eventually lead to malignancy. For example, changes in HS chain sulfation have been linked to both the progression of cancer and cancer invasiveness [202]. Furthermore, protein glycosylation has been demonstrated to play a role in every recognized cancer hallmark, so our ability to interpret the glycocode will be crucial to the development of improved cancer therapies [203]. Indeed, some of the most common clinically used biomarkers for cancer diagnosis and monitoring are glycoproteins, and are known to be aberrantly glycosylated in cancer (e.g., PSA for prostate cancer; MUC16 for ovarian cancer; and SLea for pancreatic cancer) [204]. However, current assays assessing these proteins lack the necessary specificity and sensitivity for early cancer detection, thus the identification of specific glycoforms of a certain protein could improve diagnostic potential and, theoretically, improve patient prognosis.
One approach to begin deciphering the cancer glycome is using high-throughput glycan and lectin arrays for the identification of glycan substrate specificities and changes in glycan moieties. As lectins can distinguish between linkages and nuances of glycan moieties, they can serve as very sensitive and precise detectors of changes in glycoprotein structures. Recently, glycan array analysis and lectin profiling identified a novel lectin overexpressed in pancreatic cancer and was able to detect pancreatic cancer with higher sensitivity than the current best biomarker, SLea [205]. Further, in a subset of breast cancer patients, lectin-binding profiles were able to distinguish glycan binding differences within the serum from metastatic and non-metastatic patients [206]. Lectin arrays have also been used to identify key changes in glycosylation patters for the monitoring of cancer cell metastasis and response to treatment [207,208]. These findings illustrate the utility of lectin-based arrays for both clinical and research applications in cancer.
Lectin arrays can also been used to isolate and characterize the glycosignatures of extracellular vesicles [209,210]. Extracellular vesicles play a key role in intercellular communication by transporting biomolecules from cell to cell, and are released by virtually all cell types, yet seem to play a particularly vital role in the transmission of pathogenic signaling disease processes such as cancer. Intriguingly, extracellular vesicles are rich in glycoconjugates, and cancer cell-derived extracellular vesicles exhibit unique glycan profiles which depend on cell surface HSPGs for their internalization and functional activity [39,211]. Thus it is exciting to think of the potential to utilize glycan- and lectin-based arrays to identify cancer these cancer-specific glycosignatures to manipulate extracellular vesicle uptake and delivery based on the unique HSPG network of a given cancer cell type.
In this review, we have detailed an argument that epigenetic based therapies focused on the HSPG biosynthetic pathway have tremendous potential for the treatment of multiple types of cancers. The importance of HSPGs in oncogenesis is demonstrated by the fact that potential biomarkers exist for the progression of many disparate cancers. Epigenetic therapies are likely to act on multiple levels as HS structure affects growth factor signaling and sensitivity to chemotherapeutics. The importance of changes in HS composition supports utilization of lectin-based arrays to guide the development of these therapies.
Acknowledgments
This work was supported by a research incentive grant to Elizabeth E. Hull and intramural funding to Kathryn J. Leyva. We thank the creators of the GlycanBuilder software for making their tool freely available [212].
Abbreviations
| BxGALT | β 1-x galactosyltransferase |
| BxGAT | β 1-x glucuronyltransferase |
| EXT | Exostosin |
| EXTL | Exostosin-like |
| GLCE | d-glucuronyl C5-epimerase |
| GPC | Glypican |
| HS | Heparan sulfate |
| HSPE | Heparanase |
| HSPG | Heparan sulfate proteoglycan |
| HSxST | Heparan sulfate x-O-sulfotransferase |
| NA domain | N-acetylated disaccharide units |
| NS domain | N-sulfated disaccharide units |
| NDST | N-deacetylase/N-sulfotransferases |
| SULF | Sulfatase |
| XYLT | Xylosyltransferase |
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Sarrazin S., Lamanna W.C., Esko J.D. Heparan sulfate proteoglycans. Cold Spring Harb. Perspect. Biol. 2011;3:a004952. doi: 10.1101/cshperspect.a004952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Iozzo R.V. Heparan sulfate proteoglycans: Intricate molecules with intriguing functions. J. Clin. Investig. 2001;108:165–167. doi: 10.1172/JCI200113560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Couchman J.R., Pataki C.A. An introduction to proteoglycans and their localization. J. Histochem. Cytochem. 2012;60:885–897. doi: 10.1369/0022155412464638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blackhall F.H., Merry C.L., Davies E.J., Jayson G.C. Heparan sulfate proteoglycans and cancer. Br. J. Cancer. 2001;85:1094–1098. doi: 10.1054/bjoc.2001.2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bernfield M., Gotte M., Park P.W., Reizes O., Fitzgerald M.L., Lincecum J., Zako M. Functions of cell surface heparan sulfate proteoglycans. Annu. Rev. Biochem. 1999;68:729–777. doi: 10.1146/annurev.biochem.68.1.729. [DOI] [PubMed] [Google Scholar]
- 6.Filmus J., Selleck S.B. Glypicans: Proteoglycans with a surprise. J. Clin. Investig. 2001;108:497–501. doi: 10.1172/JCI200113712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Filmus J., Capurro M., Rast J. Glypicans. Genome Biol. 2008;9:224. doi: 10.1186/gb-2008-9-5-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taylor D.R., Whitehouse I.J., Hooper N.M. Glypican-1 mediates both prion protein lipid raft association and disease isoform formation. PLoS Pathog. 2009;5:e1000666. doi: 10.1371/journal.ppat.1000666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zeng Y., Waters M., Andrews A., Honarmandi P., Ebong E.E., Rizzo V., Tarbell J.M. Fluid shear stress induces the clustering of heparan sulfate via mobility of glypican-1 in lipid rafts. Am. J. Physiol. Heart Circ. Physiol. 2013;305:811–820. doi: 10.1152/ajpheart.00764.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zeng Y., Tarbell J.M. The adaptive remodeling of endothelial glycocalyx in response to fluid shear stress. PLoS ONE. 2014;9:e86249. doi: 10.1371/journal.pone.0086249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lopez-Casillas F., Payne H.M., Andres J.L., Massague J. Betaglycan can act as a dual modulator of TGF-β access to signaling receptors: Mapping of ligand binding and gag attachment sites. J. Cell Biol. 1994;124:557–568. doi: 10.1083/jcb.124.4.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bilandzic M., Stenvers K.L. Betaglycan: A multifunctional accessory. Mol. Cell Endocrinol. 2011;339:180–189. doi: 10.1016/j.mce.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 13.Shintani Y., Takashima S., Asano Y., Kato H., Liao Y., Yamazaki S., Tsukamoto O., Seguchi O., Yamamoto H., Fukushima T., et al. Glycosaminoglycan modification of neuropilin-1 modulates VEGFR2 signaling. EMBO J. 2006;25:3045–3055. doi: 10.1038/sj.emboj.7601188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miao H.Q., Klagsbrun M. Neuropilin is a mediator of angiogenesis. Cancer Met. Rev. 2000;19:29–37. doi: 10.1023/A:1026579711033. [DOI] [PubMed] [Google Scholar]
- 15.Soker S., Takashima S., Miao H.Q., Neufeld G., Klagsbrun M. Neuropilin-1 is expressed by endothelial and tumor cells as an isoform-specific receptor for vascular endothelial growth factor. Cell. 1998;92:735–745. doi: 10.1016/S0092-8674(00)81402-6. [DOI] [PubMed] [Google Scholar]
- 16.Kolodkin A.L., Levengood D.V., Rowe E.G., Tai Y.T., Giger R.J., Ginty D.D. Neuropilin is a semaphorin III receptor. Cell. 1997;90:753–762. doi: 10.1016/S0092-8674(00)80535-8. [DOI] [PubMed] [Google Scholar]
- 17.Kalish E.D., Iida N., Moffat F.L., Bourguignon L.Y. A new CD44v3-containing isoform is involved in tumor cell growth and migration during human breast carcinoma progression. Front. Biosci. 1999;4:1–8. doi: 10.2741/Kalish. [DOI] [PubMed] [Google Scholar]
- 18.Wang S.J., Bourguignon L.Y. Role of hyaluronan-mediated CD44 signaling in head and neck squamous cell carcinoma progression and chemoresistance. Am. J. Pathol. 2011;178:956–963. doi: 10.1016/j.ajpath.2010.11.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang S.J., Wong G., de Heer A.M., Xia W., Bourguignon L.Y. CD44 variant isoforms in head and neck squamous cell carcinoma progression. Laryngoscope. 2009;119:1518–1530. doi: 10.1002/lary.20506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jayadev R., Sherwood D.R. Basement membranes. Curr. Biol. 2017;27:R207–R211. doi: 10.1016/j.cub.2017.02.006. [DOI] [PubMed] [Google Scholar]
- 21.Dreyfuss J.L., Regatieri C.V., Jarrouge T.R., Cavalheiro R.P., Sampaio L.O., Nader H.B. Heparan sulfate proteoglycans: Structure, protein interactions and cell signaling. An. Acad. Bras. Cienc. 2009;81:409–429. doi: 10.1590/S0001-37652009000300007. [DOI] [PubMed] [Google Scholar]
- 22.Korpetinou A., Skandalis S.S., Labropoulou V.T., Smirlaki G., Noulas A., Karamanos N.K., Theocharis A.D. Serglycin: At the crossroad of inflammation and malignancy. Front. Oncol. 2014;3:327. doi: 10.3389/fonc.2013.00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bishop J.R., Schuksz M., Esko J.D. Heparan sulphate proteoglycans fine-tune mammalian physiology. Nature. 2007;446:1030–1037. doi: 10.1038/nature05817. [DOI] [PubMed] [Google Scholar]
- 24.Olczyk P., Mencner L., Komosinska-Vassev K. Diverse roles of heparan sulfate and heparin in wound repair. BioMed. Res. Int. 2015;2015:549417. doi: 10.1155/2015/549417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Celie J.W., Beelen R.H., van den Born J. Heparan sulfate proteoglycans in extravasation: Assisting leukocyte guidance. Front. Biosci. 2009;14:4932–4949. doi: 10.2741/3578. [DOI] [PubMed] [Google Scholar]
- 26.Kumar A.V., Katakam S.K., Urbanowitz A.K., Gotte M. Heparan sulphate as a regulator of leukocyte recruitment in inflammation. Curr. Protein Pept. Sci. 2015;16:77–86. doi: 10.2174/1573402111666150213165054. [DOI] [PubMed] [Google Scholar]
- 27.Soares M.A., Teixeira F.C., Fontes M., Areas A.L., Leal M.G., Pavao M.S., Stelling M.P. Heparan sulfate proteoglycans may promote or inhibit cancer progression by interacting with integrins and affecting cell migration. BioMed. Res. Int. 2015;2015:453801. doi: 10.1155/2015/453801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown D.S., Eames B.F. Emerging tools to study proteoglycan function during skeletal development. Methods Cell Biol. 2016;134:485–530. doi: 10.1016/bs.mcb.2016.03.001. [DOI] [PubMed] [Google Scholar]
- 29.Patel V.N., Pineda D.L., Hoffman M.P. The function of heparan sulfate during branching morphogenesis. Matrix Biol. J. Int. Soc. Matrix Biol. 2017;57–58:311–323. doi: 10.1016/j.matbio.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Coulson-Thomas V.J. The role of heparan sulphate in development: The ectodermal story. Int. J. Exp. Pathol. 2016;97:213–229. doi: 10.1111/iep.12180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reine T.M., Vuong T.T., Rutkovskiy A., Meen A.J., Vaage J., Jenssen T.G., Kolset S.O. Serglycin in quiescent and proliferating primary endothelial cells. PLoS ONE. 2015;10:e0145584. doi: 10.1371/journal.pone.0145584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sutton V.R., Brennan A.J., Ellis S., Danne J., Thia K., Jenkins M.R., Voskoboinik I., Pejler G., Johnstone R.W., Andrews D.M., et al. Serglycin determines secretory granule repertoire and regulates natural killer cell and cytotoxic T lymphocyte cytotoxicity. FEBS J. 2016;283:947–961. doi: 10.1111/febs.13649. [DOI] [PubMed] [Google Scholar]
- 33.Melo F.R., Vita F., Berent-Maoz B., Levi-Schaffer F., Zabucchi G., Pejler G. Proteolytic histone modification by mast cell tryptase, a serglycin proteoglycan-dependent secretory granule protease. J. Biol. Chem. 2014;289:7682–7690. doi: 10.1074/jbc.M113.546895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elfenbein A., Lanahan A., Zhou T.X., Yamasaki A., Tkachenko E., Matsuda M., Simons M. Syndecan 4 regulates FGFR1 signaling in endothelial cells by directing macropinocytosis. Sci. Signal. 2012;5:ra36. doi: 10.1126/scisignal.2002495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hara T., Yoshida E., Shinkai Y., Yamamoto C., Fujiwara Y., Kumagai Y., Kaji T. Biglycan intensifies alk5-smad2/3 signaling by TGF-β1 and downregulates syndecan-4 in cultured vascular endothelial cells. J. Cell Biochem. 2017;118:1087–1096. doi: 10.1002/jcb.25721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hara T., Yoshida E., Fujiwara Y., Yamamoto C., Kaji T. Transforming growth factor-β1 modulates the expression of syndecan-4 in cultured vascular endothelial cells in a biphasic manner. J. Cell Biochem. 2016;118:2009–2017. doi: 10.1002/jcb.25861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Obunike J.C., Lutz E.P., Li Z., Paka L., Katopodis T., Strickland D.K., Kozarsky K.F., Pillarisetti S., Goldberg I.J. Transcytosis of lipoprotein lipase across cultured endothelial cells requires both heparan sulfate proteoglycans and the very low density lipoprotein receptor. J. Biol. Chem. 2001;276:8934–8941. doi: 10.1074/jbc.M008813200. [DOI] [PubMed] [Google Scholar]
- 38.Leonova E.I., Galzitskaya O.V. Role of syndecans in lipid metabolism and human diseases. Adv. Exp. Med. Biol. 2015;855:241–258. doi: 10.1007/978-3-319-17344-3_10. [DOI] [PubMed] [Google Scholar]
- 39.Christianson H.C., Svensson K.J., van Kuppevelt T.H., Li J.P., Belting M. Cancer cell exosomes depend on cell-surface heparan sulfate proteoglycans for their internalization and functional activity. Proc. Natl. Acad. Sci. USA. 2013;110:17380–17385. doi: 10.1073/pnas.1304266110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Christianson H.C., Belting M. Heparan sulfate proteoglycan as a cell-surface endocytosis receptor. Matrix Biol. J. Int. Soc. Matrix Biol. 2014;35:51–55. doi: 10.1016/j.matbio.2013.10.004. [DOI] [PubMed] [Google Scholar]
- 41.Wang H., Jin H., Beauvais D.M., Rapraeger A.C. Cytoplasmic domain interactions of syndecan-1 and syndecan-4 with α6β4 integrin mediate human epidermal growth factor receptor (HER1 and HER2)-dependent motility and survival. J. Biol. Chem. 2014;289:30318–30332. doi: 10.1074/jbc.M114.586438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Beauvais D.M., Burbach B.J., Rapraeger A.C. The syndecan-1 ectodomain regulates αvβ3 integrin activity in human mammary carcinoma cells. J. Cell Biol. 2004;167:171–181. doi: 10.1083/jcb.200404171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gomes A.M., Bhat R., Correia A.L., Mott J.D., Ilan N., Vlodavsky I., Pavao M.S., Bissell M. Mammary branching morphogenesis requires reciprocal signaling by heparanase and mmp-14. J. Cell Biochem. 2015;116:1668–1679. doi: 10.1002/jcb.25127. [DOI] [PubMed] [Google Scholar]
- 44.Wang D., Sai J., Richmond A. Cell surface heparan sulfate participates in cxcl1-induced signaling. Biochemistry. 2003;42:1071–1077. doi: 10.1021/bi026425a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li J.P., Spillmann D. Heparan sulfate proteoglycans as multifunctional cell regulators: Cell surface receptors. Methods Mol. Biol. 2012;836:239–255. doi: 10.1007/978-1-61779-498-8_16. [DOI] [PubMed] [Google Scholar]
- 46.Chu W., Song X., Yang X., Ma L., Zhu J., He M., Wang Z., Wu Y. Neuropilin-1 promotes epithelial-to-mesenchymal transition by stimulating nuclear factor-κb and is associated with poor prognosis in human oral squamous cell carcinoma. PLoS ONE. 2014;9:e101931. doi: 10.1371/journal.pone.0101931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Tse B.W., Volpert M., Ratther E., Stylianou N., Nouri M., McGowan K., Lehman M.L., McPherson S.J., Roshan-Moniri M., Butler M.S., et al. Neuropilin-1 is upregulated in the adaptive response of prostate tumors to androgen-targeted therapies and is prognostic of metastatic progression and patient mortality. Oncogene. 2017;36:3417–3427. doi: 10.1038/onc.2016.482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Graziani G., Lacal P.M. Neuropilin-1 as therapeutic target for malignant melanoma. Front. Oncol. 2015;5:125. doi: 10.3389/fonc.2015.00125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ferguson B.W., Datta S. Role of heparan sulfate 2-O-sulfotransferase in prostate cancer cell proliferation, invasion, and growth factor signaling. Prostate Cancer. 2011;2011:893208. doi: 10.1155/2011/893208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hecht J.T., Hogue D., Strong L.C., Hansen M.F., Blanton S.H., Wagner M. Hereditary multiple exostosis and chondrosarcoma: Linkage to chromosome II and loss of heterozygosity for EXT-linked markers on chromosomes II and 8. Am. J. Hum. Gen. 1995;56:1125–1131. [PMC free article] [PubMed] [Google Scholar]
- 51.Lind T., Tufaro F., McCormick C., Lindahl U., Lidholt K. The putative tumor suppressors EXT1 and EXT2 are glycosyltransferases required for the biosynthesis of heparan sulfate. J. Biol. Chem. 1998;273:26265–26268. doi: 10.1074/jbc.273.41.26265. [DOI] [PubMed] [Google Scholar]
- 52.Kobayashi S., Morimoto K., Shimizu T., Takahashi M., Kurosawa H., Shirasawa T. Association of EXT1 and EXT2, hereditary multiple exostoses gene products, in golgi apparatus. Biochem. Biophys. Res. Commun. 2000;268:860–867. doi: 10.1006/bbrc.2000.2219. [DOI] [PubMed] [Google Scholar]
- 53.Jao T.M., Li Y.L., Lin S.W., Tzeng S.T., Yu I.S., Yen S.J., Tsai M.H., Yang Y.C. Alteration of colonic epithelial cell differentiation in mice deficient for glucosaminyl N-deacetylase/N-sulfotransferase 4. Oncotarget. 2016;7:84938–84950. doi: 10.18632/oncotarget.12915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Couchman J.R., Gopal S., Lim H.C., Norgaard S., Multhaupt H.A. Syndecans: From peripheral coreceptors to mainstream regulators of cell behaviour. Int. J. Exp. Pathol. 2015;96:1–10. doi: 10.1111/iep.12112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wu Y., Liu H., Ding H. Gpc-3 in hepatocellular carcinoma: Current perspectives. J. Hepatocell. Carcinoma. 2016;3:63–67. doi: 10.2147/JHC.S116513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Montalbano M., Georgiadis J., Masterson A.L., McGuire J.T., Prajapati J., Shirafkan A., Rastellini C., Cicalese L. Biology and function of glypican-3 as a candidate for early cancerous transformation of hepatocytes in hepatocellular carcinoma (review) Oncol. Rep. 2017;37:1291–1300. doi: 10.3892/or.2017.5387. [DOI] [PubMed] [Google Scholar]
- 57.Aydin O., Yildiz L., Baris S., Dundar C., Karagoz F. Expression of glypican 3 in low and high grade urothelial carcinomas. Diagn. Pathol. 2015;10:34. doi: 10.1186/s13000-015-0266-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wade A., Robinson A.E., Engler J.R., Petritsch C., James C.D., Phillips J.J. Proteoglycans and their roles in brain cancer. FEBS J. 2013;280:2399–2417. doi: 10.1111/febs.12109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Fernandez-Vega I., Garcia-Suarez O., Garcia B., Crespo A., Astudillo A., Quiros L.M. Heparan sulfate proteoglycans undergo differential expression alterations in right sided colorectal cancer, depending on their metastatic character. BMC Cancer. 2015;15:742. doi: 10.1186/s12885-015-1724-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kreuger J., Kjellen L. Heparan sulfate biosynthesis: Regulation and variability. J. Histochem. Cytochem. 2012;60:898–907. doi: 10.1369/0022155412464972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kuhn J., Gotting C., Schnolzer M., Kempf T., Brinkmann T., Kleesiek K. First isolation of human UDP-d-Xylose: Proteoglycan core protein β-d-xylosyltransferase secreted from cultured jar choriocarcinoma cells. J. Biol. Chem. 2001;276:4940–4947. doi: 10.1074/jbc.M005111200. [DOI] [PubMed] [Google Scholar]
- 62.Gotting C., Kuhn J., Zahn R., Brinkmann T., Kleesiek K. Molecular cloning and expression of human UDP-d-Xylose:Proteoglycan core protein β-d-xylosyltransferase and its first isoform XT-II. J. Mol. Biol. 2000;304:517–528. doi: 10.1006/jmbi.2000.4261. [DOI] [PubMed] [Google Scholar]
- 63.Tsutsui Y., Ramakrishnan B., Qasba P.K. Crystal structures of β-1,4-galactosyltransferase 7 enzyme reveal conformational changes and substrate binding. J. Biol. Chem. 2013;288:31963–31970. doi: 10.1074/jbc.M113.509984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hiyama A., Gogate S.S., Gajghate S., Mochida J., Shapiro I.M., Risbud M.V. Bmp-2 and TGF-β stimulate expression of β1,3-glucuronosyl transferase 1 (Glcat-1) in nucleus pulposus cells through AP1, tonebp, and Sp1: Role of mapks. J. Bone Miner. Res. 2010;25:1179–1190. doi: 10.1359/jbmr.091202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Koike T., Izumikawa T., Sato B., Kitagawa H. Identification of phosphatase that dephosphorylates xylose in the glycosaminoglycan-protein linkage region of proteoglycans. J. Biol. Chem. 2014;289:6695–6708. doi: 10.1074/jbc.M113.520536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Guo R., Wu G., Li H., Qian P., Han J., Pan F., Li W., Li J., Ji F. Promoter methylation profiles between human lung adenocarcinoma multidrug resistant a549/cisplatin (a549/ddp) cells and its progenitor a549 cells. Biol. Pharm. Bull. 2013;36:1310–1316. doi: 10.1248/bpb.b13-00153. [DOI] [PubMed] [Google Scholar]
- 67.Olsson M., Beck S., Kogner P., Martinsson T., Caren H. Genome-wide methylation profiling identifies novel methylated genes in neuroblastoma tumors. Epigenetics. 2016;11:74–84. doi: 10.1080/15592294.2016.1138195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Poeta M.L., Massi E., Parrella P., Pellegrini P., de Robertis M., Copetti M., Rabitti C., Perrone G., Muda A.O., Molinari F., et al. Aberrant promoter methylation of β-1,4 galactosyltransferase 1 as potential cancer-specific biomarker of colorectal tumors. Genes Chromosomes Cancer. 2012;51:1133–1143. doi: 10.1002/gcc.21998. [DOI] [PubMed] [Google Scholar]
- 69.Kim M.S., Louwagie J., Carvalho B., Terhaar Sive Droste J.S., Park H.L., Chae Y.K., Yamashita K., Liu J., Ostrow K.L., Ling S., et al. Promoter DNA methylation of oncostatin M receptor-β as a novel diagnostic and therapeutic marker in colon cancer. PLoS ONE. 2009;4:e6555. doi: 10.1371/journal.pone.0006555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Choi H.J., Chung T.W., Kim C.H., Jeong H.S., Joo M., Youn B., Ha K.T. Estrogen induced β-1,4-galactosyltransferase 1 expression regulates proliferation of human breast cancer MCF-7 cells. Biochem. Biophys. Res. Commun. 2012;426:620–625. doi: 10.1016/j.bbrc.2012.08.140. [DOI] [PubMed] [Google Scholar]
- 71.Busse M., Feta A., Presto J., Wilen M., Gronning M., Kjellen L., Kusche-Gullberg M. Contribution of EXT1, EXT2, and EXTL3 to heparan sulfate chain elongation. J. Biol. Chem. 2007;282:32802–32810. doi: 10.1074/jbc.M703560200. [DOI] [PubMed] [Google Scholar]
- 72.Busse-Wicher M., Wicher K.B., Kusche-Gullberg M. The extostosin family: Proteins with many functions. Matrix Biol. 2014;35:25–33. doi: 10.1016/j.matbio.2013.10.001. [DOI] [PubMed] [Google Scholar]
- 73.Katta K., Imran T., Busse-Wicher M., Gronning M., Czajkowski S., Kusche-Gullberg M. Reduced expression of EXTL2, a member of the exostosin (EXT) family of glycosyltransferases, in human embryonic kidney 293 cells results in longer heparan sulfate chains. J. Biol. Chem. 2015;290:13168–13177. doi: 10.1074/jbc.M114.631754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Oud M.M., Tuijnenburg P., Hempel M., van Vlies N., Ren Z., Ferdinandusse S., Jansen M.H., Santer R., Johannsen J., Bacchelli C., et al. Mutations in EXTL3 cause neuro-immuno-skeletal dysplasia syndrome. Am. J. Hum. Gen. 2017;100:281–296. doi: 10.1016/j.ajhg.2017.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Jones K.B., Pacifici M., Hilton M.J. Multiple hereditary exostoses (MHE): Elucidating the pathogenesis of a rare skeletal disorder through interdisciplinary research. Connect. Tissue Res. 2014;55:80–88. doi: 10.3109/03008207.2013.867957. [DOI] [PubMed] [Google Scholar]
- 76.Kitagawa H., Shimakawa H., Sugahara K. The tumor suppressor EXT-like gene EXTL2 encodes an α1, 4-N-acetylhexosaminyltransferase that transfersn-acetylgalactosamine and N-acetylglucosamine to the common glycosaminoglycan-protein linkage region: The key enzyme for the chain initiation of heparan sulfate. J. Biol. Chem. 1999;274:13933–13937. doi: 10.1074/jbc.274.20.13933. [DOI] [PubMed] [Google Scholar]
- 77.Nadanaka S., Zhou S., Kagiyama S., Shoji N., Sugahara K., Sugihara K., Asano M., Kitagawa H. EXTL2, a member of the EXT family of tumor suppressors, controls glycosaminoglycan biosynthesis in a xylose kinase-dependent manner. J. Biol. Chem. 2013;288:9321–9333. doi: 10.1074/jbc.M112.416909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nadanaka S., Kitagawa H. EXTL2 controls liver regeneration and aortic calcification through xylose kinase-dependent regulation of glycosaminoglycan biosynthesis. Matrix Biol. J. Int. Soc. Matrix Biol. 2014;35:18–24. doi: 10.1016/j.matbio.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 79.Boutet E., Lieberherr D., Tognolli M., Schneider M., Bansal P., Bridge A.J., Poux S., Bougueleret L., Xenarios I. Uniprotkb/swiss-prot, the manually annotated section of the uniprot knowledgebase: How to use the entry view. Methods Mol. Biol. 2016;1374:23–54. doi: 10.1007/978-1-4939-3167-5_2. [DOI] [PubMed] [Google Scholar]
- 80.Duncan G., McCormick C., Tufaro F. The link between heparan sulfate and hereditary bone disease: Finding a function for the ext family of putative tumor suppressor proteins. J. Clin. Investig. 2001;108:511–516. doi: 10.1172/JCI13737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.McCormick C., Duncan G., Goutsos K.T., Tufaro F. The putative tumor suppressors EXT1 and EXT2 form a stable complex that accumulates in the golgi apparatus and catalyzes the synthesis of heparan sulfate. Proc. Natl. Acad. Sci. USA. 2000;97:668–673. doi: 10.1073/pnas.97.2.668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Okada M., Nadanaka S., Shoji N., Tamura J., Kitagawa H. Biosynthesis of heparan sulfate in EXT1-deficient cells. Biochem. J. 2010;428:463–471. doi: 10.1042/BJ20100101. [DOI] [PubMed] [Google Scholar]
- 83.Ahn J., Ludecke H.J., Lindow S., Horton W.A., Lee B., Wagner M.J., Horsthemke B., Wells D.E. Cloning of the putative tumour suppressor gene for hereditary multiple exostoses (EXT1) Nat. Genet. 1995;11:137–143. doi: 10.1038/ng1095-137. [DOI] [PubMed] [Google Scholar]
- 84.Francannet C., Cohen-Tanugi A., Le Merrer M., Munnich A., Bonaventure J., Legeai-Mallet L. Genotype-phenotype correlation in hereditary multiple exostoses. J. Med. Gen. 2001;38:430–434. doi: 10.1136/jmg.38.7.430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Sinha S., Mundy C., Bechtold T., Sgariglia F., Ibrahim M.M., Billings P.C., Carroll K., Koyama E., Jones K.B., Pacifici M. Unsuspected osteochondroma-like outgrowths in the cranial base of hereditary multiple exostoses patients and modeling and treatment with a bmp antagonist in mice. PLoS Genet. 2017;13:e1006742. doi: 10.1371/journal.pgen.1006742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Farhan S.M., Wang J., Robinson J.F., Prasad A.N., Rupar C.A., Siu V.M., Hegele R.A. Old gene, new phenotype: Mutations in heparan sulfate synthesis enzyme, ext2 leads to seizure and developmental disorder, no exostoses. J. Med. Gen. 2015;52:666–675. doi: 10.1136/jmedgenet-2015-103279. [DOI] [PubMed] [Google Scholar]
- 87.Volpi S., Yamazaki Y., Brauer P.M., van Rooijen E., Hayashida A., Slavotinek A., Sun Kuehn H., Di Rocco M., Rivolta C., Bortolomai I., et al. EXTL3 mutations cause skeletal dysplasia, immune deficiency, and developmental delay. J. Exp. Med. 2017;214:623–637. doi: 10.1084/jem.20161525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Guo L., Elcioglu N.H., Mizumoto S., Wang Z., Noyan B., Albayrak H.M., Yamada S., Matsumoto N., Miyake N., Nishimura G., et al. Identification of biallelic EXTL3 mutations in a novel type of spondylo-epi-metaphyseal dysplasia. J. Hum. Genet. 2017 doi: 10.1038/jhg.2017.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Ropero S., Setien F., Espada J., Fraga M.F., Herranz M., Asp J., Benassi M.S., Franchi A., Patino A., Ward L.S., et al. Epigenetic loss of the familial tumor-suppressor gene exostosin-1 (EXT1) disrupts heparan sulfate synthesis in cancer cells. Hum. Mol. Genet. 2004;13:2753–2765. doi: 10.1093/hmg/ddh298. [DOI] [PubMed] [Google Scholar]
- 90.Khoontawad J., Hongsrichan N., Chamgramol Y., Pinlaor P., Wongkham C., Yongvanit P., Pairojkul C., Khuntikeo N., Roytrakul S., Boonmars T., et al. Increase of exostosin 1 in plasma as a potential biomarker for opisthorchiasis-associated cholangiocarcinoma. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2014;35:1029–1039. doi: 10.1007/s13277-013-1137-9. [DOI] [PubMed] [Google Scholar]
- 91.Kato M., Wang H., Bernfield M., Gallagher J.T., Turnbull J.E. Cell surface syndecan-1 on distinct cell types differs in fine structure and ligand binding of its heparan sulfate chains. J. Biol. Chem. 1994;269:18881–18890. [PubMed] [Google Scholar]
- 92.Suhovskih A.V., Domanitskaya N.V., Tsidulko A.Y., Prudnikova T.Y., Kashuba V.I., Grigorieva E.V. Tissue-specificity of heparan sulfate biosynthetic machinery in cancer. Cell Adh. Migr. 2015;9:452–459. doi: 10.1080/19336918.2015.1049801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Suhovskih A.V., Tsidulko A.Y., Kutsenko O.S., Kovner A.V., Aidagulova S.V., Ernberg I., Grigorieva E.V. Transcriptional activity of heparan sulfate biosynthetic machinery is specifically impaired in benign prostate hyperplasia and prostate cancer. Front. Oncol. 2014;4:79. doi: 10.3389/fonc.2014.00079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Van den Born J., Pikas D.S., Pisa B.J., Eriksson I., Kjellen L., Berden J.H. Antibody-based assay for N-deacetylase activity of heparan sulfate/heparin N-deacetylase/N-sulfotransferase (NDST): Novel characteristics of NDST-1 and -2. Glycobiology. 2003;13:1–10. doi: 10.1093/glycob/cwg011. [DOI] [PubMed] [Google Scholar]
- 95.Dou W., Xu Y., Pagadala V., Pedersen L.C., Liu J. Role of deacetylase activity of N-deacetylase/N-sulfotransferase 1 in forming N-sulfated domain in heparan sulfate. J. Biol. Chem. 2015;290:20427–20437. doi: 10.1074/jbc.M115.664409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Aikawa J., Grobe K., Tsujimoto M., Esko J.D. Multiple isozymes of heparan sulfate/heparin glcnac N-deacetylase/glcn N-sulfotransferase. Structure and activity of the fourth member, NDST4. J. Biol. Chem. 2001;276:5876–5882. doi: 10.1074/jbc.M009606200. [DOI] [PubMed] [Google Scholar]
- 97.Pikas D.S., Eriksson I., Kjellen L. Overexpression of different isoforms of glucosaminyl N-deacetylase/N-sulfotransferase results in distinct heparan sulfate N-sulfation patterns. Biochemistry. 2000;39:4552–4558. doi: 10.1021/bi992524l. [DOI] [PubMed] [Google Scholar]
- 98.Holmborn K., Ledin J., Smeds E., Eriksson I., Kusche-Gullberg M., Kjellen L. Heparan sulfate synthesized by mouse embryonic stem cells deficient in NDST1 and NDST2 is 6-O-sulfated but contains no N-sulfate groups. J. Biol. Chem. 2004;279:42355–42358. doi: 10.1074/jbc.C400373200. [DOI] [PubMed] [Google Scholar]
- 99.Humphries D.E., Wong G.W., Friend D.S., Gurish M.F., Qiu W.T., Huang C., Sharpe A.H., Stevens R.L. Heparin is essential for the storage of specific granule proteases in mast cells. Nature. 1999;400:769–772. doi: 10.1038/23481. [DOI] [PubMed] [Google Scholar]
- 100.Forsberg E., Pejler G., Ringvall M., Lunderius C., Tomasini-Johansson B., Kusche-Gullberg M., Eriksson I., Ledin J., Hellman L., Kjellen L. Abnormal mast cells in mice deficient in a heparin-synthesizing enzyme. Nature. 1999;400:773–776. doi: 10.1038/23488. [DOI] [PubMed] [Google Scholar]
- 101.Tzeng S.T., Tsai M.H., Chen C.L., Lee J.X., Jao T.M., Yu S.L., Yen S.J., Yang Y.C. NDST4 is a novel candidate tumor suppressor gene at chromosome 4q26 and its genetic loss predicts adverse prognosis in colorectal cancer. PLoS ONE. 2013;8:e67040. doi: 10.1371/journal.pone.0067040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Qi Q., Menzaghi C., Smith S., Liang L., de Rekeneire N., Garcia M.E., Lohman K.K., Miljkovic I., Strotmeyer E.S., Cummings S.R., et al. Genome-wide association analysis identifies TYW3/CRYZ and NDST4 loci associated with circulating resistin levels. Hum. Mol. Genet. 2012;21:4774–4780. doi: 10.1093/hmg/dds300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Eicher J.D., Powers N.R., Miller L.L., Akshoomoff N., Amaral D.G., Bloss C.S., Libiger O., Schork N.J., Darst B.F., Casey B.J., et al. Genome-wide association study of shared components of reading disability and language impairment. Genes Brain Behav. 2013;12:792–801. doi: 10.1111/gbb.12085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Reuter M.S., Musante L., Hu H., Diederich S., Sticht H., Ekici A.B., Uebe S., Wienker T.F., Bartsch O., Zechner U., et al. NDST1 missense mutations in autosomal recessive intellectual disability. Am. J. Med. Genet. Part A. 2014;164A:2753–2763. doi: 10.1002/ajmg.a.36723. [DOI] [PubMed] [Google Scholar]
- 105.Najmabadi H., Hu H., Garshasbi M., Zemojtel T., Abedini S.S., Chen W., Hosseini M., Behjati F., Haas S., Jamali P., et al. Deep sequencing reveals 50 novel genes for recessive cognitive disorders. Nature. 2011;478:57–63. doi: 10.1038/nature10423. [DOI] [PubMed] [Google Scholar]
- 106.Lencz T., Guha S., Liu C., Rosenfeld J., Mukherjee S., DeRosse P., John M., Cheng L., Zhang C., Badner J.A., et al. Genome-wide association study implicates NDST3 in schizophrenia and bipolar disorder. Nat. Commun. 2013;4:2739. doi: 10.1038/ncomms3739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Zhang C., Lu W., Wang Z., Ni J., Zhang J., Tang W., Fang Y. A comprehensive analysis of NDST3 for schizophrenia and bipolar disorder in han chinese. Trans. Psychiatry. 2016;6:e701. doi: 10.1038/tp.2015.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Deligny A., Dierker T., Dagalv A., Lundequist A., Eriksson I., Nairn A.V., Moremen K.W., Merry C.L., Kjellen L. NDST2 (N-deacetylase/N-sulfotransferase-2) enzyme regulates heparan sulfate chain length. J. Biol. Chem. 2016;291:18600–18607. doi: 10.1074/jbc.M116.744433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Sheng J., Liu R., Xu Y., Liu J. The dominating role of N-deacetylase/N-sulfotransferase 1 in forming domain structures in heparan sulfate. J. Biol. Chem. 2011;286:19768–19776. doi: 10.1074/jbc.M111.224311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Bui C., Ouzzine M., Talhaoui I., Sharp S., Prydz K., Coughtrie M.W., Fournel-Gigleux S. Epigenetics: Methylation-associated repression of heparan sulfate 3-O-sulfotransferase gene expression contributes to the invasive phenotype of h-emc-ss chondrosarcoma cells. FASEB J. 2010;24:436–450. doi: 10.1096/fj.09-136291. [DOI] [PubMed] [Google Scholar]
- 111.Shi X., Su S., Long J., Mei B., Chen Y. Microrna-191 targets N-deacetylase/N-sulfotransferase 1 and promotes cell growth in human gastric carcinoma cell line MGC803. Acta Biochim. Biophys. Sin. 2011;43:849–856. doi: 10.1093/abbs/gmr084. [DOI] [PubMed] [Google Scholar]
- 112.Kasza Z., Fredlund Fuchs P., Tamm C., Eriksson A.S., O’Callaghan P., Heindryckx F., Spillmann D., Larsson E., Le Jan S., Eriksson I., et al. Microrna-24 suppression of N-deacetylase/N-sulfotransferase-1 (NDST1) reduces endothelial cell responsiveness to vascular endothelial growth factor a (VEGFA) J. Biol. Chem. 2013;288:25956–25963. doi: 10.1074/jbc.M113.484360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.He D.X., Gu X.T., Li Y.R., Jiang L., Jin J., Ma X. Methylation-regulated mir-149 modulates chemoresistance by targeting glcnac N-deacetylase/N-sulfotransferase-1 in human breast cancer. FEBS J. 2014;281:4718–4730. doi: 10.1111/febs.13012. [DOI] [PubMed] [Google Scholar]
- 114.Sheng J., Xu Y., Dulaney S.B., Huang X., Liu J. Uncovering biphasic catalytic mode of c5-epimerase in heparan sulfate biosynthesis. J. Biol. Chem. 2012;287:20996–21002. doi: 10.1074/jbc.M112.359885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fang J., Song T., Lindahl U., Li J.P. Enzyme overexpression—An exercise toward understanding regulation of heparan sulfate biosynthesis. Sci. Rep. 2016;6:31242. doi: 10.1038/srep31242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Grigorieva E.V., Prudnikova T.Y., Domanitskaya N.V., Mostovich L.A., Pavlova T.V., Kashuba V.I., Zabarovsky E.R. d-Glucuronyl c5-epimerase suppresses small-cell lung cancer cell proliferation in vitro and tumour growth in vivo. Br. J. Cancer. 2011;105:74–82. doi: 10.1038/bjc.2011.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Prudnikova T.Y., Mostovich L.A., Domanitskaya N.V., Pavlova T.V., Kashuba V.I., Zabarovsky E.R., Grigorieva E.V. Antiproliferative effect of d-glucuronyl c5-epimerase in human breast cancer cells. Cancer Cell Int. 2010;10:27. doi: 10.1186/1475-2867-10-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Rosenberg E.E., Prudnikova T.Y., Zabarovsky E.R., Kashuba V.I., Grigorieva E.V. d-Glucuronyl c5-epimerase cell type specifically affects angiogenesis pathway in different prostate cancer cells. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2014;35:3237–3245. doi: 10.1007/s13277-013-1423-6. [DOI] [PubMed] [Google Scholar]
- 119.Mostovich L.A., Prudnikova T.Y., Kondratov A.G., Gubanova N.V., Kharchenko O.A., Kutsenko O.S., Vavilov P.V., Haraldson K., Kashuba V.I., Ernberg I., et al. The TCF4/β-catenin pathway and chromatin structure cooperate to regulate d-glucuronyl c5-epimerase expression in breast cancer. Epigenetics. 2012;7:930–939. doi: 10.4161/epi.21199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Prudnikova T.Y., Soulitzis N., Kutsenko O.S., Mostovich L.A., Haraldson K., Ernberg I., Kashuba V.I., Spandidos D.A., Zabarovsky E.R., Grigorieva E.V. Heterogeneity of d-glucuronyl c5-epimerase expression and epigenetic regulation in prostate cancer. Cancer Med. 2013;2:654–661. doi: 10.1002/cam4.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Smeds E., Feta A., Kusche-Gullberg M. Target selection of heparan sulfate hexuronic acid 2-O-sulfotransferase. Glycobiology. 2010;20:1274–1282. doi: 10.1093/glycob/cwq089. [DOI] [PubMed] [Google Scholar]
- 122.Clegg J.M., Conway C.D., Howe K.M., Price D.J., Mason J.O., Turnbull J.E., Basson M.A., Pratt T. Heparan sulfotransferases HS6ST1 and HS2ST keep erk in check for mouse corpus callosum development. J. Neurosci. 2014;34:2389–2401. doi: 10.1523/JNEUROSCI.3157-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Conway C.D., Howe K.M., Nettleton N.K., Price D.J., Mason J.O., Pratt T. Heparan sulfate sugar modifications mediate the functions of slits and other factors needed for mouse forebrain commissure development. J. Neurosci. 2011;31:1955–1970. doi: 10.1523/JNEUROSCI.2579-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Merry C.L., Bullock S.L., Swan D.C., Backen A.C., Lyon M., Beddington R.S., Wilson V.A., Gallagher J.T. The molecular phenotype of heparan sulfate in the Hs2st−/− mutant mouse. J. Biol. Chem. 2001;276:35429–35434. doi: 10.1074/jbc.M100379200. [DOI] [PubMed] [Google Scholar]
- 125.Maccarana M., Sakura Y., Tawada A., Yoshida K., Lindahl U. Domain structure of heparan sulfates from bovine organs. J. Biol. Chem. 1996;271:17804–17810. doi: 10.1074/jbc.271.30.17804. [DOI] [PubMed] [Google Scholar]
- 126.Ai X., Do A.T., Kusche-Gullberg M., Lindahl U., Lu K., Emerson C.P., Jr. Substrate specificity and domain functions of extracellular heparan sulfate 6-O-endosulfatases, QSULF1 and QSULF2. J. Biol. Chem. 2006;281:4969–4976. doi: 10.1074/jbc.M511902200. [DOI] [PubMed] [Google Scholar]
- 127.Uchimura K., Morimoto-Tomita M., Rosen S.D. Measuring the activities of the sulfs: Two novel heparin/heparan sulfate endosulfatases. Methods Enzymol. 2006;416:243–253. doi: 10.1016/S0076-6879(06)16015-2. [DOI] [PubMed] [Google Scholar]
- 128.Shworak N.W., HajMohammadi S., de Agostini A.I., Rosenberg R.D. Mice deficient in heparan sulfate 3-O-sulfotransferase-1: Normal hemostasis with unexpected perinatal phenotypes. Glycoconj. J. 2002;19:355–361. doi: 10.1023/A:1025377206600. [DOI] [PubMed] [Google Scholar]
- 129.Yabe T., Shukla D., Spear P.G., Rosenberg R.D., Seeberger P.H., Shworak N.W. Portable sulphotransferase domain determines sequence specificity of heparan sulphate 3-O-sulphotransferases. Biochem. J. 2001;359:235–241. doi: 10.1042/bj3590235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gao W., Xu Y., Liu J., Ho M. Epitope mapping by a wnt-blocking antibody: Evidence of the wnt binding domain in heparan sulfate. Sci. Rep. 2016;6:26245. doi: 10.1038/srep26245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Cole C.L., Hansen S.U., Barath M., Rushton G., Gardiner J.M., Avizienyte E., Jayson G.C. Synthetic heparan sulfate oligosaccharides inhibit endothelial cell functions essential for angiogenesis. PLoS ONE. 2010;5:e11644. doi: 10.1371/journal.pone.0011644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Vijaya Kumar A., Salem Gassar E., Spillmann D., Stock C., Sen Y.P., Zhang T., Van Kuppevelt T.H., Hulsewig C., Koszlowski E.O., Pavao M.S., et al. HS3ST2 modulates breast cancer cell invasiveness via map kinase- and Tcf4 (Tcf7l2)-dependent regulation of protease and cadherin expression. Int. J. Cancer. 2014;135:2579–2592. doi: 10.1002/ijc.28921. [DOI] [PubMed] [Google Scholar]
- 133.Meneghetti M.C.Z., Hughes A.J., Rudd T.R., Nader H.B., Powell A.K., Yates E.A., Lima M.A. Heparan sulfate and heparin interactions with proteins. J. Royal Soc. Interface. 2015;12:0589. doi: 10.1098/rsif.2015.0589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Mao X., Gauche C., Coughtrie M.W., Bui C., Gulberti S., Merhi-Soussi F., Ramalanjaona N., Bertin-Jung I., Diot A., Dumas D., et al. The heparan sulfate sulfotransferase 3-OST3A (HS3ST3A) is a novel tumor regulator and a prognostic marker in breast cancer. Oncogene. 2016;35:5043–5055. doi: 10.1038/onc.2016.44. [DOI] [PubMed] [Google Scholar]
- 135.Hwang J.A., Kim Y., Hong S.H., Lee J., Cho Y.G., Han J.Y., Kim Y.H., Han J., Shim Y.M., Lee Y.S., et al. Epigenetic inactivation of heparan sulfate (glucosamine) 3-O-sulfotransferase 2 in lung cancer and its role in tumorigenesis. PLoS ONE. 2013;8:e79634. doi: 10.1371/journal.pone.0079634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Roperch J.P., Grandchamp B., Desgrandchamps F., Mongiat-Artus P., Ravery V., Ouzaid I., Roupret M., Phe V., Ciofu C., Tubach F., et al. Promoter hypermethylation of HS3ST2, SEPTIN9 and SLIT2 combined with FGFR3 mutations as a sensitive/specific urinary assay for diagnosis and surveillance in patients with low or high-risk non-muscle-invasive bladder cancer. BMC Cancer. 2016;16:704. doi: 10.1186/s12885-016-2748-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Lamanna W.C., Frese M.A., Balleininger M., Dierks T. Sulf loss influences N-, 2-O-, and 6-O-sulfation of multiple heparan sulfate proteoglycans and modulates fibroblast growth factor signaling. J. Biol. Chem. 2008;283:27724–27735. doi: 10.1074/jbc.M802130200. [DOI] [PubMed] [Google Scholar]
- 138.Li K., Bethea H.N., Liu J. Using engineered 2-O-sulfotransferase to determine the activity of heparan sulfate c5-epimerase and its mutants. J. Biol. Chem. 2010;285:11106–11113. doi: 10.1074/jbc.M109.081059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Presto J., Thuveson M., Carlsson P., Busse M., Wilen M., Eriksson I., Kusche-Gullberg M., Kjellen L. Heparan sulfate biosynthesis enzymes EXT1 and EXT2 affect NDST1 expression and heparan sulfate sulfation. Proc. Natl Acad Sci. USA. 2008;105:4751–4756. doi: 10.1073/pnas.0705807105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Esko J.D., Selleck S.B. Order out of chaos: Assembly of ligand binding sites in heparan sulfate. Annu Rev. Biochem. 2002;71:435–471. doi: 10.1146/annurev.biochem.71.110601.135458. [DOI] [PubMed] [Google Scholar]
- 141.Hassinen A., Kellokumpu S. Organizational interplay of golgi N-glycosyltransferases involves organelle microenvironment-dependent transitions between enzyme homo- and heteromers. J. Biol. Chem. 2014;289:26937–26948. doi: 10.1074/jbc.M114.595058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Hassinen A., Pujol F.M., Kokkonen N., Pieters C., Kihlstrom M., Korhonen K., Kellokumpu S. Functional organization of golgi N- and O-glycosylation pathways involves pH-dependent complex formation that is impaired in cancer cells. J. Biol. Chem. 2011;286:38329–38340. doi: 10.1074/jbc.M111.277681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Zhang X., Wang F., Sheng J. “Coding” and “decoding”: Hypothesis for the regulatory mechanism involved in heparan sulfate biosynthesis. Carbohydr. Res. 2016;428:1–7. doi: 10.1016/j.carres.2016.04.002. [DOI] [PubMed] [Google Scholar]
- 144.Schultz V., Suflita M., Liu X., Zhang X., Yu Y., Li L., Green D.E., Xu Y., Zhang F., DeAngelis P.L., et al. Heparan sulfate domains required for fibroblast growth factor 1 and 2 signaling through fibroblast growth factor receptor 1c. J. Biol. Chem. 2017;292:2495–2509. doi: 10.1074/jbc.M116.761585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Nagarajan U., Pakkiriswami S., Pillai A.B. Sugar tags and tumorigenesis. Front. Cell Dev. Biol. 2015;3:69. doi: 10.3389/fcell.2015.00069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Nigam S.K., Bush K.T. Growth factor-heparan sulfate “switches” regulating stages of branching morphogenesis. Pediatr. Nephrol. 2014;29:727–735. doi: 10.1007/s00467-013-2725-z. [DOI] [PubMed] [Google Scholar]
- 147.Poulain F.E., Yost H.J. Heparan sulfate proteoglycans: A sugar code for vertebrate development? Development. 2015;142:3456–3467. doi: 10.1242/dev.098178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Borza D.-B. Glomerular basement membrane heparan sulfate in health and disease: A regulator of local complement activation. Matrix Biol. 2017;57–58:299–310. doi: 10.1016/j.matbio.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Nadanaka S., Purunomo E., Takeda N., Tamura J., Kitagawa H. Heparan sulfate containing unsubstituted glucosamine residues: Biosynthesis and heparanase-inhibitory activity. J. Biol. Chem. 2014;289:15231–15243. doi: 10.1074/jbc.M113.545343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Sankaranarayanan N.V., Sarkar A., Desai U.R., Mosier P.D. Designing “high-affinity, high-specificity” glycosaminoglycan sequences through computerized modeling. Methods Mol. Biol. 2015;1229:289–314. doi: 10.1007/978-1-4939-1714-3_24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Dai Y., Yang Y., MacLeod V., Yue X., Rapraeger A.C., Shriver Z., Venkataraman G., Sasisekharan R., Sanderson R.D. Hsulf-1 and hsulf-2 are potent inhibitors of myeloma tumor growth in vivo. J. Biol. Chem. 2005;280:40066–40073. doi: 10.1074/jbc.M508136200. [DOI] [PubMed] [Google Scholar]
- 152.Kundu S., Xiong A., Spyrou A., Wicher G., Marinescu V.D., Edqvist P.D., Zhang L., Essand M., Dimberg A., Smits A., et al. Heparanase promotes glioma progression and is inversely correlated with patient survival. Mol. Cancer Res. 2016;14:1243–1253. doi: 10.1158/1541-7786.MCR-16-0223. [DOI] [PubMed] [Google Scholar]
- 153.Higginson J.R., Thompson S.M., Santos-Silva A., Guimond S.E., Turnbull J.E., Barnett S.C. Differential sulfation remodelling of heparan sulfate by extracellular 6-O-sulfatases regulates fibroblast growth factor-induced boundary formation by glial cells: Implications for glial cell transplantation. J. Neurosci. 2012;32:15902–15912. doi: 10.1523/JNEUROSCI.6340-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Khurana A., Beleford D., He X., Chien J., Shridhar V. Role of heparan sulfatases in ovarian and breast cancer. Am. J. Cancer Res. 2013;3:34–45. [PMC free article] [PubMed] [Google Scholar]
- 155.Shire A., Lomberk G., Lai J.P., Zou H., Tsuchiya N., Aderca I., Moser C.D., Gulaid K.H., Oseini A., Hu C., et al. Restoration of epigenetically silenced sulf1 expression by 5-aza-2-deoxycytidine sensitizes hepatocellular carcinoma cells to chemotherapy-induced apoptosis. Med. Epigenet. 2015;3:1–18. doi: 10.1159/000375461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Zhang H., Newman D.R., Sannes P.L. Hsulf-1 inhibits erk and akt signaling and decreases cell viability in vitro in human lung epithelial cells. Respirat. Res. 2012;13:69. doi: 10.1186/1465-9921-13-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Xu G., Ji W., Su Y., Xu Y., Yan Y., Shen S., Li X., Sun B., Qian H., Chen L., et al. Sulfatase 1 (HSULF-1) reverses basic fibroblast growth factor-stimulated signaling and inhibits growth of hepatocellular carcinoma in animal model. Oncotarget. 2014;5:5029–5039. doi: 10.18632/oncotarget.2078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Tessema M., Yingling C.M., Thomas C.L., Klinge D.M., Bernauer A.M., Liu Y., Dacic S., Siegfried J.M., Dahlberg S.E., Schiller J.H., et al. Sulf2 methylation is prognostic for lung cancer survival and increases sensitivity to topoisomerase-i inhibitors via induction of ISG15. Oncogene. 2012;31:4107–4116. doi: 10.1038/onc.2011.577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Hur K., Han T.S., Jung E.J., Yu J., Lee H.J., Kim W.H., Goel A., Yang H.K. Up-regulated expression of sulfatases (SULF1 and SULF2) as prognostic and metastasis predictive markers in human gastric cancer. J. Pathol. 2012;228:88–98. doi: 10.1002/path.4055. [DOI] [PubMed] [Google Scholar]
- 160.Lai J.P., Yu C., Moser C.D., Aderca I., Han T., Garvey T.D., Murphy L.M., Garrity-Park M.M., Shridhar V., Adjei A.A., et al. Sulf1 inhibits tumor growth and potentiates the effects of histone deacetylase inhibitors in hepatocellular carcinoma. Gastroenterology. 2006;130:2130–2144. doi: 10.1053/j.gastro.2006.02.056. [DOI] [PubMed] [Google Scholar]
- 161.Shen J., Wei J., Wang H., Yang Y., Yue G., Wang L., Yu L., Xie L., Sun X., Bian X., et al. Sulf2 methylation is associated with in vitro cisplatin sensitivity and clinical efficacy for gastric cancer patients treated with a modified folfox regimen. PLoS ONE. 2013;8:e75564. doi: 10.1371/journal.pone.0075564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Takei Y., Takigahira M., Mihara K., Tarumi Y., Yanagihara K. The metastasis-associated microrna mir-516a-3p is a novel therapeutic target for inhibiting peritoneal dissemination of human scirrhous gastric cancer. Cancer Res. 2011;71:1442–1453. doi: 10.1158/0008-5472.CAN-10-2530. [DOI] [PubMed] [Google Scholar]
- 163.Bao L., Yan Y., Xu C., Ji W., Shen S., Xu G., Zeng Y., Sun B., Qian H., Chen L., et al. microRNA-21 suppresses PTEN and HSULF-1 expression and promotes hepatocellular carcinoma progression through AKT/ERK pathways. Cancer Lett. 2013;337:226–236. doi: 10.1016/j.canlet.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 164.Okada Y., Yamada S., Toyoshima M., Dong J., Nakajima M., Sugahara K. Structural recognition by recombinant human heparanase that plays critical roles in tumor metastasis. Hierarchical sulfate groups with different effects and the essential target disulfated trisaccharide sequence. J. Biol. Chem. 2002;277:42488–42495. doi: 10.1074/jbc.M206510200. [DOI] [PubMed] [Google Scholar]
- 165.Peterson S.B., Liu J. Unraveling the specificity of heparanase utilizing synthetic substrates. J. Biol. Chem. 2010;285:14504–14513. doi: 10.1074/jbc.M110.104166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Cohen E., Atzmon R., Vlodavsky I., Ilan N. Heparanase processing by lysosomal/endosomal protein preparation. FEBS Lett. 2005;579:2334–2338. doi: 10.1016/j.febslet.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 167.Gingis-Velitski S., Zetser A., Flugelman M.Y., Vlodavsky I., Ilan N. Heparanase induces endothelial cell migration via protein kinase b/AKT activation. J. Biol. Chem. 2004;279:23536–23541. doi: 10.1074/jbc.M400554200. [DOI] [PubMed] [Google Scholar]
- 168.Zetser A., Bashenko Y., Edovitsky E., Levy-Adam F., Vlodavsky I., Ilan N. Heparanase induces vascular endothelial growth factor expression: Correlation with p38 phosphorylation levels and src activation. Cancer Res. 2006;66:1455–1463. doi: 10.1158/0008-5472.CAN-05-1811. [DOI] [PubMed] [Google Scholar]
- 169.Cohen-Kaplan V., Naroditsky I., Zetser A., Ilan N., Vlodavsky I., Doweck I. Heparanase induces VEGF c and facilitates tumor lymphangiogenesis. Int. J. Cancer. 2008;123:2566–2573. doi: 10.1002/ijc.23898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Ramani V.C., Yang Y., Ren Y., Nan L., Sanderson R.D. Heparanase plays a dual role in driving hepatocyte growth factor (HGF) signaling by enhancing hgf expression and activity. J. Biol. Chem. 2011;286:6490–6499. doi: 10.1074/jbc.M110.183277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.He X., Brenchley P.E., Jayson G.C., Hampson L., Davies J., Hampson I.N. Hypoxia increases heparanase-dependent tumor cell invasion, which can be inhibited by antiheparanase antibodies. Cancer Res. 2004;64:3928–3933. doi: 10.1158/0008-5472.CAN-03-2718. [DOI] [PubMed] [Google Scholar]
- 172.Cassinelli G., Favini E., Dal Bo L., Tortoreto M., De Maglie M., Dagrada G., Pilotti S., Zunino F., Zaffaroni N., Lanzi C. Antitumor efficacy of the heparan sulfate mimic roneparstat (SST0001) against sarcoma models involves multi-target inhibition of receptor tyrosine kinases. Oncotarget. 2016;7:47848–47863. doi: 10.18632/oncotarget.10292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Ramani V.C., Zhan F., He J., Barbieri P., Noseda A., Tricot G., Sanderson R.D. Targeting heparanase overcomes chemoresistance and diminishes relapse in myeloma. Oncotarget. 2016;7:1598–1607. doi: 10.18632/oncotarget.6408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Ogishima T., Shiina H., Breault J.E., Tabatabai L., Bassett W.W., Enokida H., Li L.C., Kawakami T., Urakami S., Ribeiro-Filho L.A., et al. Increased heparanase expression is caused by promoter hypomethylation and up-regulation of transcriptional factor early growth response-1 in human prostate cancer. Clin. Cancer Res. 2005;11:1028–1036. [PubMed] [Google Scholar]
- 175.Qu H., Zheng L., Pu J., Mei H., Xiang X., Zhao X., Li D., Li S., Mao L., Huang K., et al. miRNA-558 promotes tumorigenesis and aggressiveness of neuroblastoma cells through activating the transcription of heparanase. Hum. Mol. Genet. 2015;24:2539–2551. doi: 10.1093/hmg/ddv018. [DOI] [PubMed] [Google Scholar]
- 176.Zhang L., Sullivan P.S., Goodman J.C., Gunaratne P.H., Marchetti D. microRNA-1258 suppresses breast cancer brain metastasis by targeting heparanase. Cancer Res. 2011;71:645–654. doi: 10.1158/0008-5472.CAN-10-1910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Fernandez-Vega I., Garcia O., Crespo A., Castanon S., Menendez P., Astudillo A., Quiros L.M. Specific genes involved in synthesis and editing of heparan sulfate proteoglycans show altered expression patterns in breast cancer. BMC Cancer. 2013;13:24. doi: 10.1186/1471-2407-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Gurda D., Handschuh L., Kotkowiak W., Jakubowski H. Homocysteine thiolactone and N-homocysteinylated protein induce pro-atherogenic changes in gene expression in human vascular endothelial cells. Amino Acids. 2015;47:1319–1339. doi: 10.1007/s00726-015-1956-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Okuda H., Kobayashi A., Xia B., Watabe M., Pai S.K., Hirota S., Xing F., Liu W., Pandey P.R., Fukuda K., et al. Hyaluronan synthase has 2 promotes tumor progression in bone by stimulating the interaction of breast cancer stem-like cells with macrophages and stromal cells. Cancer Res. 2012;72:537–547. doi: 10.1158/0008-5472.CAN-11-1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Mercier I., Casimiro M.C., Wang C., Rosenberg A.L., Quong J., Minkeu A., Allen K.G., Danilo C., Sotgia F., Bonuccelli G., et al. Human breast cancer-associated fibroblasts (CAFS) show caveolin-1 downregulation and RB tumor suppressor functional inactivation: Implications for the response to hormonal therapy. Cancer Biol. Ther. 2008;7:1212–1225. doi: 10.4161/cbt.7.8.6220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Zhou H., Zhang Z., Liu C., Jin C., Zhang J., Miao X., Jia L. B4galt1 gene knockdown inhibits the Hedgehog pathway and reverses multidrug resistance in the human leukemia k562/adriamycin-resistant cell line. IUBMB Life. 2012;64:889–900. doi: 10.1002/iub.1080. [DOI] [PubMed] [Google Scholar]
- 182.Xie H., Zhu Y., An H., Wang H., Zhu Y., Fu H., Wang Z., Fu Q., Xu J., Ye D. Increased b4galt1 expression associates with adverse outcome in patients with non-metastatic clear cell renal cell carcinoma. Oncotarget. 2016;7:32723–32730. doi: 10.18632/oncotarget.8737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Zhang H., Liu Y., Xie H., Fu Q., Liu Z., Zhu Y., Xu L., Zhang W., Yang Y., Xu J. β-1,4-galactosyltransferase II predicts poor prognosis of patients with non-metastatic clear-cell renal cell carcinoma. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2017;39:1010428317691417. doi: 10.1177/1010428317691417. [DOI] [PubMed] [Google Scholar]
- 184.Lo Sasso G., Bovenga F., Murzilli S., Salvatore L., di Tullio G., Martelli N., D’Orazio A., Rainaldi S., Vacca M., Mangia A., et al. Liver x receptors inhibit proliferation of human colorectal cancer cells and growth of intestinal tumors in mice. Gastroenterology. 2013;144:1497–1507. doi: 10.1053/j.gastro.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 185.Karibe T., Fukui H., Sekikawa A., Shiratori K., Fujimori T. EXTL3 promoter methylation down-regulates EXTL3 and heparan sulphate expression in mucinous colorectal cancers. J. Pathol. 2008;216:32–42. doi: 10.1002/path.2377. [DOI] [PubMed] [Google Scholar]
- 186.Bret C., Hose D., Reme T., Sprynski A.C., Mahtouk K., Schved J.F., Quittet P., Rossi J.F., Goldschmidt H., Klein B. Expression of genes encoding for proteins involved in heparan sulphate and chondroitin sulphate chain synthesis and modification in normal and malignant plasma cells. Br. J. Haematol. 2009;145:350–368. doi: 10.1111/j.1365-2141.2009.07633.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Okolicsanyi R.K., van Wijnen A.J., Cool S.M., Stein G.S., Griffiths L.R., Haupt L.M. Heparan sulfate proteoglycans and human breast cancer epithelial cell tumorigenicity. J. Cell Biochem. 2014;115:967–976. doi: 10.1002/jcb.24746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Paschall A.V., Liu K. Epigenetic regulation of apoptosis and cell cycle regulatory genes in human colon carcinoma cells. Genom. Data. 2015;5:189–191. doi: 10.1016/j.gdata.2015.05.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Song K., Li Q., Peng Y.B., Li J., Ding K., Chen L.J., Shao C.H., Zhang L.J., Li P. Silencing of HHS6ST2 inhibits progression of pancreatic cancer through inhibition of notch signalling. Biochem. J. 2011;436:271–282. doi: 10.1042/BJ20110297. [DOI] [PubMed] [Google Scholar]
- 190.Iravani O., Bay B.H., Yip G.W. Silencing HS6ST3 inhibits growth and progression of breast cancer cells through suppressing IGF1R and inducing XAF1. Exp. Cell Res. 2017;350:380–389. doi: 10.1016/j.yexcr.2016.12.019. [DOI] [PubMed] [Google Scholar]
- 191.Cole C.L., Rushton G., Jayson G.C., Avizienyte E. Ovarian cancer cell heparan sulfate 6-O-sulfotransferases regulate an angiogenic program induced by heparin-binding epidermal growth factor (EGF)-like growth factor/egf receptor signaling. J. Biol. Chem. 2014;289:10488–10501. doi: 10.1074/jbc.M113.534263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 192.Martinez P., Vergoten G., Colomb F., Bobowski M., Steenackers A., Carpentier M., Allain F., Delannoy P., Julien S. Over-sulfated glycosaminoglycans are alternative selectin ligands: Insights into molecular interactions and possible role in breast cancer metastasis. Clin. Exp. Met. 2013;30:919–931. doi: 10.1007/s10585-013-9592-7. [DOI] [PubMed] [Google Scholar]
- 193.Zheng X., Gai X., Han S., Moser C.D., Hu C., Shire A.M., Floyd R.A., Roberts L.R. The human sulfatase 2 inhibitor 2,4-disulfonylphenyl-TERT-butylnitrone (OKN-007) has an antitumor effect in hepatocellular carcinoma mediated via suppression of TGFB1/SMAD2 and Hedgehog/GLI1 signaling. Genes. Chromosomes Cancer. 2013;52:225–236. doi: 10.1002/gcc.22022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Hossain M.M., Hosono-Fukao T., Tang R., Sugaya N., van Kuppevelt T.H., Jenniskens G.J., Kimata K., Rosen S.D., Uchimura K. Direct detection of HSULF-1 and HSULF-2 activities on extracellular heparan sulfate and their inhibition by PI-88. Glycobiology. 2010;20:175–186. doi: 10.1093/glycob/cwp159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Lai J.P., Sandhu D.S., Yu C., Moser C.D., Hu C., Shire A.M., Aderca I., Murphy L.M., Adjei A.A., Sanderson S., et al. Sulfatase 2 protects hepatocellular carcinoma cells against apoptosis induced by the pi3k inhibitor ly294002 and erk and jnk kinase inhibitors. Liver Int. 2010;30:1522–1528. doi: 10.1111/j.1478-3231.2010.02336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Elkin M., Cohen I., Zcharia E., Orgel A., Guatta-Rangini Z., Peretz T., Vlodavsky I., Kleinman H.K. Regulation of heparanase gene expression by estrogen in breast cancer. Cancer Res. 2003;63:8821–8826. [PubMed] [Google Scholar]
- 197.Jiang G., Zheng L., Pu J., Mei H., Zhao J., Huang K., Zeng F., Tong Q. Small RNAs targeting transcription start site induce heparanase silencing through interference with transcription initiation in human cancer cells. PLoS ONE. 2012;7:e31379. doi: 10.1371/journal.pone.0031379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Levy-Adam F., Feld S., Cohen-Kaplan V., Shteingauz A., Gross M., Arvatz G., Naroditsky I., Ilan N., Doweck I., Vlodavsky I. Heparanase 2 interacts with heparan sulfate with high affinity and inhibits heparanase activity. J. Biol. Chem. 2010;285:28010–28019. doi: 10.1074/jbc.M110.116384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Debeb B.G., Lacerda L., Xu W., Larson R., Solley T., Atkinson R., Sulman E.P., Ueno N.T., Krishnamurthy S., Reuben J.M., et al. Histone deacetylase inhibitors stimulate dedifferentiation of human breast cancer cells through WNT/β-catenin signaling. Stem. Cells. 2012;30:2366–2377. doi: 10.1002/stem.1219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Slingerland M., Guchelaar H.J., Gelderblom H. Histone deacetylase inhibitors: An overview of the clinical studies in solid tumors. Anti-Cancer Drugs. 2014;25:140–149. doi: 10.1097/CAD.0000000000000040. [DOI] [PubMed] [Google Scholar]
- 201.Hameetman L., David G., Yavas A., White S.J., Taminiau A.H., Cleton-Jansen A.M., Hogendoorn P.C., Bovee J.V. Decreased ext expression and intracellular accumulation of heparan sulphate proteoglycan in osteochondromas and peripheral chondrosarcomas. J. Pathol. 2007;211:399–409. doi: 10.1002/path.2127. [DOI] [PubMed] [Google Scholar]
- 202.Jayson G.C., Lyon M., Paraskeva C., Turnbull J.E., Deakin J.A., Gallagher J.T. Heparan sulfate undergoes specific structural changes during the progression from human colon adenoma to carcinoma in vitro. J. Biol. Chem. 1998;273:51–57. doi: 10.1074/jbc.273.1.51. [DOI] [PubMed] [Google Scholar]
- 203.Munkley J., Elliott D.J. Hallmarks of glycosylation in cancer. Oncotarget. 2016;7:35478–35489. doi: 10.18632/oncotarget.8155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Pinho S.S., Reis C.A. Glycosylation in cancer: Mechanisms and clinical implications. Nat. Rev. Cancer. 2015;15:540–555. doi: 10.1038/nrc3982. [DOI] [PubMed] [Google Scholar]
- 205.Singh S., Pal K., Yadav J., Tang H., Partyka K., Kletter D., Hsueh P., Ensink E., Kc B., Hostetter G., et al. Upregulation of glycans containing 3’ fucose in a subset of pancreatic cancers uncovered using fusion-tagged lectins. J. Proteome Res. 2015;14:2594–2605. doi: 10.1021/acs.jproteome.5b00142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Fry S.A., Afrough B., Lomax-Browne H.J., Timms J.F., Velentzis L.S., Leathem A.J. Lectin microarray profiling of metastatic breast cancers. Glycobiology. 2011;21:1060–1070. doi: 10.1093/glycob/cwr045. [DOI] [PubMed] [Google Scholar]
- 207.Tan Z., Lu W., Li X., Yang G., Guo J., Yu H., Li Z., Guan F. Altered N-glycan expression profile in epithelial-to-mesenchymal transition of nmumg cells revealed by an integrated strategy using mass spectrometry and glycogene and lectin microarray analysis. J. Proteom. Res. 2014;13:2783–2795. doi: 10.1021/pr401185z. [DOI] [PubMed] [Google Scholar]
- 208.Patsos G., Hebbe-Viton V., Robbe-Masselot C., Masselot D., San Martin R., Greenwood R., Paraskeva C., Klein A., Graessmann M., Michalski J.C., et al. O-glycan inhibitors generate aryl-glycans, induce apoptosis and lead to growth inhibition in colorectal cancer cell lines. Glycobiology. 2009;19:382–398. doi: 10.1093/glycob/cwn149. [DOI] [PubMed] [Google Scholar]
- 209.Costa J. Glycoconjugates from extracellular vesicles: Structures, functions and emerging potential as cancer biomarkers. Biochim. Biophys. Acta. 2017;1868:157–166. doi: 10.1016/j.bbcan.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 210.Echevarria J., Royo F., Pazos R., Salazar L., Falcon-Perez J.M., Reichardt N.C. Microarray-based identification of lectins for the purification of human urinary extracellular vesicles directly from urine samples. Chembiochem. 2014;15:1621–1626. doi: 10.1002/cbic.201402058. [DOI] [PubMed] [Google Scholar]
- 211.Gomes J., Gomes-Alves P., Carvalho S.B., Peixoto C., Alves P.M., Altevogt P., Costa J. Extracellular vesicles from ovarian carcinoma cells display specific glycosignatures. Biomolecules. 2015;5:1741–1761. doi: 10.3390/biom5031741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Ceroni A., Dell A., Haslam S.M. The glycanbuilder: A fast, intuitive and flexible software tool for building and displaying glycan structures. Source Code Biol. Med. 2007;2:3. doi: 10.1186/1751-0473-2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]