Abstract
The best-defined primary esophageal motor disorder is achalasia. However, symptoms such as dysphagia, regurgitation and chest pain can be caused by other esophageal motility disorders. The Chicago classification introduced new manometric parameters and better defined esophageal motility disorders. Motility disorders beyond achalasia with the current classification are: esophagogastric junction outflow obstruction, major disorders of peristalsis (distal esophageal spasm, hypercontractile esophagus, absent contractility) and minor disorders of peristalsis (ineffective esophageal motility, fragmented peristalsis). The aim of this study was to review the current diagnosis and management of esophageal motility disorders other than achalasia.
Keywords: esophageal motility disorders, high-resolution manometry, Chicago classification
1. Introduction
The best-defined primary esophageal motor disorder is achalasia. However, symptoms such as dysphagia, regurgitation and chest pain can be caused by other esophageal motility disorders. Unfortunately, while there is a reasonable consensus on the pathophysiology, diagnosis and treatment of achalasia, this has not occurred for other motility disorders [1].
Esophageal manometry, the best method to evaluate esophageal motility, evolved from intraluminal balloons to water perfused catheters, and then to solid state probes; from unidirectional measurements to circumferential data gathering; and from simple pressure curves to intuitive colorful temporal-pressure plots. This technological evolution led to the development of high-resolution manometry (HRM) [2].
The more comprehensive HRM plots provoked esophageal physiologists to develop new manometric parameters and reclassify esophageal motility disorders. This led to a compilation of significant clinical findings under the Chicago classification [3]. This classification was recently revised (version 3.0) to exclude some previous parameters without clear clinical application, characterize new parameters, and redefine motility disorders [4]. Motility disorders beyond achalasia now include: esophagogastric junction outflow obstruction, major disorders of peristalsis (distal esophageal spasm, hypercontractile esophagus, absent contractility) and minor disorders of peristalsis (ineffective esophageal motility, fragmented peristalsis).
The aim of this study was to review the current diagnosis and management of esophageal motility disorders beyond achalasia.
2. HRM Parameters
2.1. Contractile Vigor—Distal Contractile Integral
HRM allows the evaluation of contractility through a combination of amplitude, time and length of the peristaltic wave. This parameter is the distal contractile integral (DCI). DCI value is calculated as the product of the mean amplitude of contraction in the distal esophagus (mmHg), the duration of contraction (seconds), and the length of the distal esophageal segment (cm) exceeding 20 mmHg for the region spanning from the transition zone to the proximal aspect of the lower esophageal sphincter (LES). DCI classifies waves as failed (DCI < 100 mmHg/s/cm), weak (DCI 100–450 mmHg/s/cm), ineffective (failed or weak), normal (DCI 450–8000 mmHg/s/cm) or hypercontractile (DCI > 8000 mmHg/s/cm).
2.2. Peristalsis—Distal Latency
HRM evaluates peristalsis by the distal latency (DL) which measures objectively the timeframe of the wave from the beginning of the swallow (upper esophageal sphincter relaxation) to an inflection of the peristaltic axis known as the contractile deceleration point. Premature contractions are defined with a DL < 4.5 s.
Fragmented contractions are considered segmental defects (break in the 20-mmHg isobaric contour > 5 cm) with normal contraction vigor.
2.3. Lower Esophageal Sphincter Pressure
The Chicago Classification did not define parameters for lower esophageal sphincter (LES) length or basal pressure, but simply recommended assessment of pressure as an average of inspiratory and expiratory values for three normal respiratory cycles. Relaxation, however, is measured not by the nadir pressure, as previously done with conventional manometry, but with the integrated relaxation pressure (IRP), which corresponds to the mean pressure of 4 s of greatest post deglutive relaxation in a 10 s gap, triggered at the beginning of a swallow.
3. Esophageal Motility Disorders beyond Achalasia
Esophagogastric Junction Outflow Obstruction
Esophagogastric junction (EGJ) outflow obstruction is characterized by an impaired LES relaxation (IRP > 15 mmHg) with normal or weak peristalsis.
4. Major Disorders of Peristalsis
4.1. Distal Esophageal Spasm
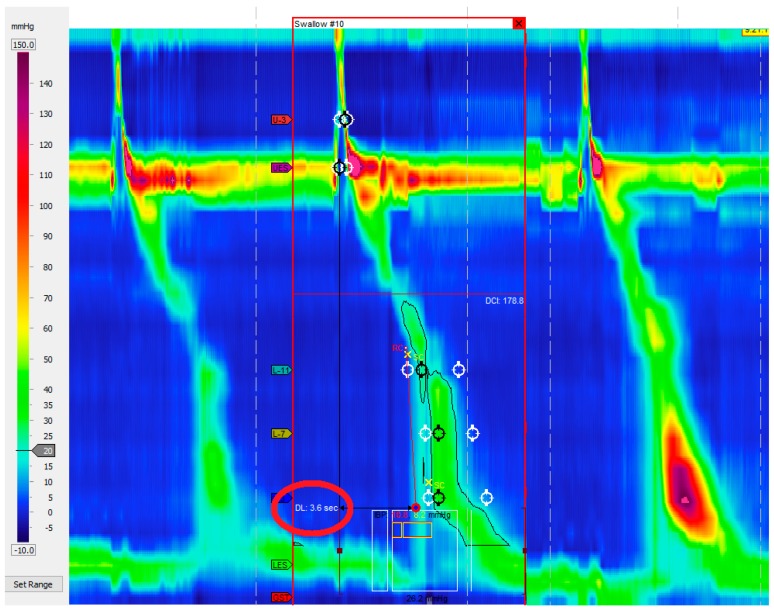
Distal esophageal spasm (DES) is defined by premature contractions (DL < 4.5 s) in at least 20% of swallows with a normal IRP (Figure 1).
Figure 1.
Distal esophageal spasm. Premature contractions (DL < 4.5 s) in at least 20% of swallows.
4.2. Hypercontractile Esophagus
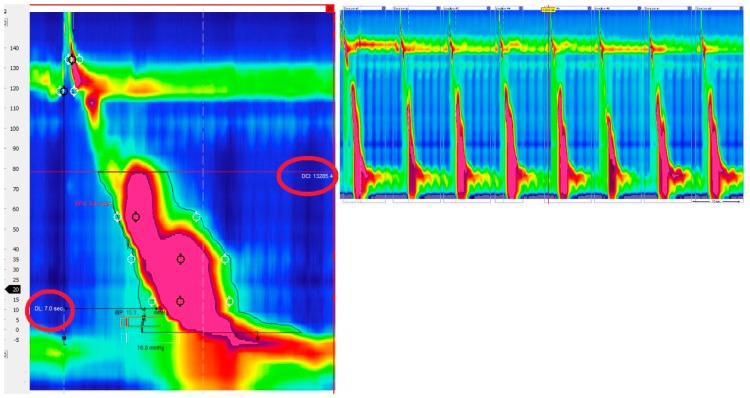
Hypercontractile esophagus (jackhammer esophagus) is characterized by DCI > 8000 mmHg/s/cm in at least 20% of swallows and normal DL (Figure 2).
Figure 2.
Hypercontractile esophagus (jackhammer esophagus). DCI > 8000 mmHg/s/cm in at least 20% of swallows and normal DL.
4.3. Absent Contractility
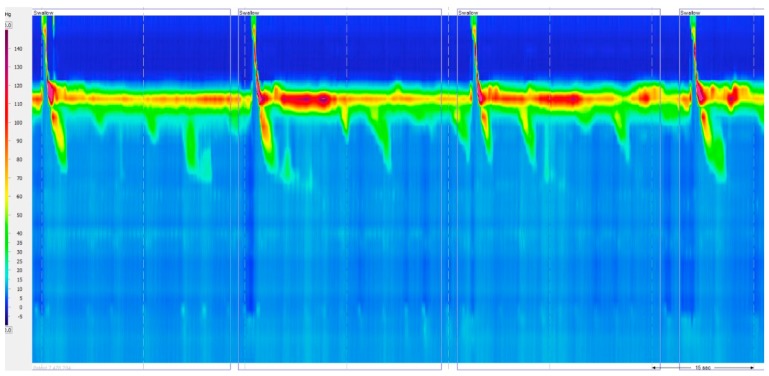
Absent contractility is characterized by aperistalsis in the setting of normal LES relaxation (IRP < 10 mmHg) (Figure 3).
Figure 3.
Absent contractility. Aperistalsis in the setting of normal LES relaxation (IRP < 10 mmHg).
5. Minor Disorders of Peristalsis
5.1. Ineffective Esophageal Motility
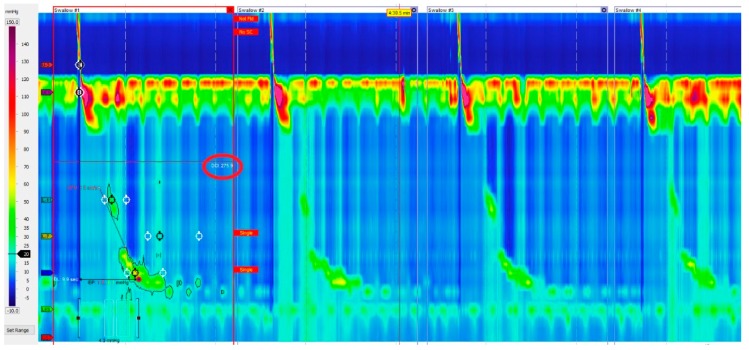
Ineffective esophageal motility is defined by ≥ 50% ineffective swallows (failed or weak—DCI < 450 mmHg/s/cm) (Figure 4).
Figure 4.
Ineffective esophageal motility. Failed or weak peristalsis in at least 30% of swallows.
5.2. Fragmented Peristalsis
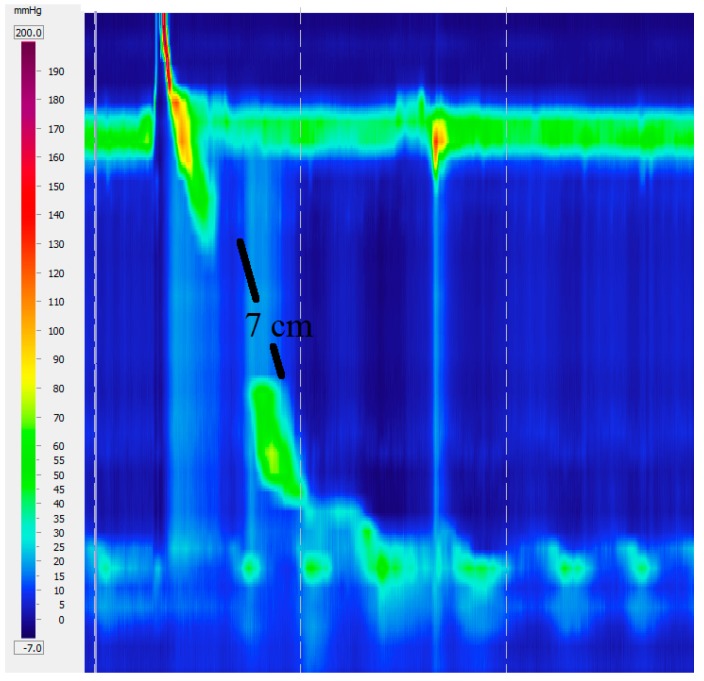
Fragmented peristalsis is defined by ≥50% fragmented contractions with normal contraction vigor (Figure 5).
Figure 5.
Fragmented peristalsis with a 7 cm gap.
6. Management of Motility Disorders beyond Achalasia
Esophagogastric Junction Outflow Obstruction
The definition of EGJ outflow obstruction based solely on the IRP with the exclusion of achalasia allows this diagnosis to be superimposed to other diagnosis dependent on the esophageal body motility. It may be caused by an anatomical abnormality at the cardia (hiatal hernia, diseases of the esophageal wall, etc.) or be idiopathic with normal anatomy.
Similar to achalasia, treatment is directed towards relief of the obstruction and can be accomplished by botulinum toxin injection, pneumatic dilatation (PD), laparoscopic Heller myotomy (LHM) or peroral endoscopic myotomy (POEM). Both botulinum injection and PD showed good relief of dysphagia but with ephemeral duration [5]. Scherer and colleagues [6], diagnosed 16 patients (1.6%) with EGJ outflow obstruction in doing 1000 HRM and treated them with botulinum toxin injection, PD or LHM. Only the three patients treated with LHM responded well. Interestingly, Pérez-Fernández et al. [7] reported that over one-third of the patients with EGJ outflow obstruction presented a spontaneous resolution of the symptoms, concluding that surgical treatment should be considered with special caution in these patients. In the setting of an anatomic abnormality such as a hiatal hernia, surgical correction is associated with long-lasting and excellent results [8].
EGJ outflow obstruction is now recognized as a distinct entity in the Chicago Classification. However, the real clinical significance of this diagnosis is still uncertain. In fact, it could be an early or incomplete expression of a variant of achalasia. Thus, the exact significance and clinical management of these patients remains unclear.
7. Major Disorders of Peristalsis
As the symptoms and the manometric picture of esophageal motility disorders can be due to gastroesophageal reflux disease (GERD), it is of paramount importance to rule out abnormal reflux by pH monitoring. If GERD is present, either medical or surgical treatment should be directed towards the control of the reflux [9].
The management of DES remains elusive. The Chicago Classification defines this disorder with a new parameter: the distal latency (DL). Previous reports showed good results in patients with “diffuse esophageal spasm” (Richter classification) [10] who underwent LHM with an extended myotomy [11,12]. However, scarce data are available after the new classification defined DES. A review of the publications after this definition became publicized showed that botulinum toxin injection in the esophageal body was superior to placebo to relieve dysphagia in patients with DES, and that POEM is a promising treatment for these patients [13].
The definition of hypercontractile esophagus (jackhammer) was updated in the last version of the Chicago Classification to include only cases with ≥20% of swallows with a DCI > 8000 mmHg/s/cm, excluding a single altered swallow from the definition. Pharmacological relaxation of the smooth muscle with phosphodiesterase-5 inhibitors or anticholinergic agents has shown symptomatic improvement [14]. Studies focusing on surgical therapy for hypercontractile esophagus based on the new classification are not available. Previous reports not using HRM or the Chicago Classification; however, showed acceptable outcomes after surgical myotomy [15,16].
Absent contractility is mostly diagnosed in patients with connective tissue diseases. There is no specific treatment to restore or improve peristalsis in these patients. Associated GERD is usually the target of therapy [17].
8. Minor Disorders of Peristalsis
Therapeutic options for ineffective esophageal motility are still limited, as no effective treatment is available to restore impaired esophageal smooth muscle contractility [18]. Treatment directed towards gastroesophageal reflux disease is helpful when dysmotility is secondary to this disease.
The concept of fragmented peristalsis changed radically from previous versions to the version 3.0. Only large breaks (>5 cm) with normal peristalsis are included. This is more clinically relevant, since incomplete bolus transit is observed in 100% of the cases of large breaks but only in 16% of small breaks [19]. It is unclear how to treat this finding since there are no studies focusing on the treatment for this disease under these criteria. There are no studies evaluating changes in the motility pattern after therapy for gastroesophageal reflux disease as well, since both conditions are frequently associated.
9. Conclusions
HRM and the Chicago classification certainly contributed to a better definition of esophageal motility disorders beyond achalasia. Although they have a much lower prevalence than achalasia, they need to be considered in the differential diagnosis of a patient presenting with achalasia symptoms. Unfortunately, the real clinical significance and correct management of these motility disorders are still under investigation.
Author Contributions
Francisco Schlottmann and Marco G. Patti, conceived the study and helped with literature search and writing of the manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Schlottmann F., Shaheen N.J., Madanick R.D., Patti M.G. The role of Heller myotomy and POEM for nonachalasia motility disorders. Dis. Esophagus. 2017;30:1–5. doi: 10.1093/dote/dox003. [DOI] [PubMed] [Google Scholar]
- 2.Herbella F.A.M., del Grande J.C. New ambulatory techniques for assessment of esophageal motility and their applicability on achalasia study. Rev. CBC. 2008;35:199–202. [Google Scholar]
- 3.Kahrilas P.J., Ghosh S.K., Pandolfino J.E. Esophageal motility disorders in terms of pressure topography: The Chicago Classification. J. Clin. Gastroenterol. 2008;42:627–635. doi: 10.1097/MCG.0b013e31815ea291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kahrilas P.J., Bredenoord A.J., Fox M., Gyawali C.P., Roman S., Smout A.J., Pandolfino J.E. International high resolution manometry working group. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol. Motil. 2015;27:160–174. doi: 10.1111/nmo.12477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Hoeij F.B., Smout A.J., Bredenoord A.J. Characterization of idiopathic esophagogastric junction outflow obstruction. Neurogastroenterol. Motil. 2015;27:1310–1316. doi: 10.1111/nmo.12625. [DOI] [PubMed] [Google Scholar]
- 6.Scherer J.R., Kwiatek M.A., Soper N.J., Pandolfino J.E., Kahrilas P.J. Functional esophagogastric junction obstruction with intact peristalsis: A heterogeneous syndrome sometimes akin to achalasia. J. Gastrointest. Surg. 2009;13:2219–2225. doi: 10.1007/s11605-009-0975-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pérez-Fernández M.T., Santander C., Marinero A., Burgos-Santamaría D., Chavarría-Herbozo C. Characterization and follow-up of esophagogastric junction outflow obstruction detected by high resolution manometry. Neurogastroenterol. Motil. 2016;28:116–126. doi: 10.1111/nmo.12708. [DOI] [PubMed] [Google Scholar]
- 8.DeLay K., Austin G.L., Menard-Katcher P. Anatomic abnormalities are common potential explanations of manometric esophagogastric junction outflow obstruction. Neurogastroenterol. Motil. 2016;28:1166–1171. doi: 10.1111/nmo.12814. [DOI] [PubMed] [Google Scholar]
- 9.Herbella F.A., Raz D.J., Nipomnick I., Patti M.G. Primary versus secondary esophageal motility disorders: Diagnosis and implications for treatment. J. Laparaoendosc. Adv. Surg. Tech. A. 2009;19:195–198. doi: 10.1089/lap.2008.0317. [DOI] [PubMed] [Google Scholar]
- 10.Richter J.E. Oesophageal motility disorders. Lancet. 2001;358:823–828. doi: 10.1016/S0140-6736(01)05973-6. [DOI] [PubMed] [Google Scholar]
- 11.Patti M.G., Gorodner M.V., Galvani C., Tedesco P., Fisichella P.M., Ostroff J.W., Bagatelos K.C., Way L.W. Spectrum of esophageal motility disorders: Implications for diagnosis and treatment. Arch. Surg. 2005;140:442. doi: 10.1001/archsurg.140.5.442. [DOI] [PubMed] [Google Scholar]
- 12.Leconte M., Douard R., Gaudric M., Dumontier I., Chaussade S., Dousset B. Functional results after extended myotomy for diffuse oesophageal spasm. Br. J. Surg. 2007;94:113–118. doi: 10.1002/bjs.5761. [DOI] [PubMed] [Google Scholar]
- 13.Roman S., Kahrilas P.J. Distal esophageal spasm. Curr. Opin. Gastroenterol. 2015;31:328–333. doi: 10.1097/MOG.0000000000000187. [DOI] [PubMed] [Google Scholar]
- 14.Hong Y.S., Min Y.W., Rhee P.L. Two distinct types of hypercontractile esophagus: Classic and spastic jackhammer. Gut Liver. 2016;10:859–863. doi: 10.5009/gnl15388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patti M.G., Pellegrini C.A., Arcerito M., Tong J., Mulvihill S.J., Way L.W. Comparison of medical and minimally invasive surgical therapy for primary esophageal motility disorders. Arch. Surg. 1995;130:609–615. doi: 10.1001/archsurg.1995.01430060047009. [DOI] [PubMed] [Google Scholar]
- 16.Herbella F.A., Tineli A.C., Wilson J.L., Jr., del Grande J.C. Surgical treatment of primary esophageal motility disorders. J. Gastrointest. Surg. 2008;12:604–608. doi: 10.1007/s11605-007-0379-5. [DOI] [PubMed] [Google Scholar]
- 17.Menezes M.A., Herbella F.A., Patti M.G. Laparoscopic antireflux surgery in patients with connective tissue diseases. J. Laparoendosc. Adv. Surg. Tech. A. 2016;26:296–298. doi: 10.1089/lap.2016.0097. [DOI] [PubMed] [Google Scholar]
- 18.Scheerens C., Tack J., Rommel N. Buspirone, a new drug for the management of patients with ineffective esophageal motility? United Eur. Gastroenterol. J. 2015;3:261–265. doi: 10.1177/2050640615585688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Herbella F.A., Tedesco P., Nipomnick I., Fisichella P.M., Patti M.G. Effect of partial and total laparoscopic fundoplication on esophageal body motility. Surg. Endosc. 2007;21:285–288. doi: 10.1007/s00464-006-0108-2. [DOI] [PubMed] [Google Scholar]