Abstract
CONTEXT
Although institutional coverage of childbirth is increasing in the developing world, a substantial minority of births in rural Mozambique still occur outside of health facilities. Identifying the remaining barriers to safe professional delivery services can aid in achieving universal coverage.
METHODS
Survey data collected in 2009 from 1,373 women in Gaza, Mozambique, were used in combination with spatial, meteorological and health facility data to examine patterns in place of delivery. Geographic information system–based visualization and mapping and exploratory spatial data analysis were used to outline the spatial distribution of home deliveries. Multilevel logistic regression models were constructed to identify associations between individual, spatial and other characteristics and whether women’s most recent delivery took place at home.
RESULTS
Spatial analysis revealed high- and low-prevalence clusters of home births. In multivariate analyses, women with a higher number of clinics within 10 kilometers of their home had a reduced likelihood of home delivery, but those living closer to urban centers had an increased likelihood. Giving birth during the rainy, high agricultural season was positively associated with home delivery, while household wealth was negatively associated with home birth. No associations were evident for measures of exposure to and experience with health institutions.
CONCLUSIONS
The results suggest the need for a comprehensive approach to expansion of professional delivery services. Such an approach should complement measures facilitating physical access to health institutions for residents of harder-to-reach areas with community-based interventions aimed at improving rural women’s living conditions and opportunities, while also taking into account seasonal and other variables.
Universal access to institutional deliveries is a critical goal of rural maternal and child health care systems in resource-limited settings. Even in countries where maternal and child health care is heavily subsidized or free and where the proportion of institutional deliveries has markedly increased in recent times, a substantial proportion of women do not deliver at health facilities, thereby jeopardizing their health and that of their babies. Previous research has identified various characteristics that are associated with the type of place where women give birth. For example, women’s education level is positively associated with the likelihood of an in-facility delivery.1–4 Similarly, women from better-off households are more likely than other women to deliver their babies at health facilities.3–9 Cultural norms,10 religion8 and the influence of household and community members11 may play important roles. Aside from the individual, household and community characteristics that may shape access to maternal and child health services, the characteristics of health care institutions and especially the quality of care that women perceive or experience are associated with women’s decision to deliver at a health facility.4,10–14
While some women may choose not to deliver at a clinic, opting instead for the assistance of nonprofessional providers in their communities, many are unable to reach a facility in time because of distance or the cost or unavailability of transportation.15 Indeed, spatial inequalities in access to delivery care services have been noted as a major determinant of place of delivery.3,4,6,9,10,16–18 Finally, the physical accessibility of maternal and child health facilities may vary throughout the year depending on rainfall, though the empirical evidence is inconsistent. For example, a Zambian study found a higher likelihood of institutional deliveries during a dry season than during a rainy season,15 whereas no association was apparent in Ghana.18
Most studies exploring the correlates of place of child delivery have focused on settings in which only a small share of births occur at health facilities. However, thanks to concerted government efforts supported by international assistance, many areas in less developed countries in Sub-Saharan Africa and elsewhere have witnessed considerable progress in institutional coverage of births.19 In these transitional settings, the main theoretical and policy concern is to understand the barriers that may hinder the continued improvement in and eventual universalization of access to facility-based deliveries.
This study seeks to unpack the notion of access by examining the relative importance of institutional, spatial and seasonal variables associated with place of delivery in one such transitional setting—rural southern Mozambique. Although the study area is typical of many resource-limited rural settings in Sub-Saharan Africa, it is also characterized by relatively high coverage of institutional deliveries. Our study therefore adds to the literature by focusing on an increasingly common type of setting in which a large majority of child births occur in facilities but a substantial minority do not.
SETTING
Mozambique is a nation of 27 million in southeast Africa with a gross national income of US$600 per capita.20 The study area is located in the south of the country and comprises rural parts of four contiguous districts of Gaza province with a total area of 15,500 square kilometers and a population of 650,000. The setting is largely monoethnic and patrilineal. The mainstay of the local economy is subsistence agriculture. Low and unpredictable agricultural yields, the scarcity of nonagricultural employment opportunities and the proximity of South Africa (Mozambique’s substantially more developed neighbor) have all contributed to a large-scale out-migration of male laborers.21 The total fertility rate in Gaza province is 5.3 children per woman,22 and the prevalence of HIV among adults is about 25%.23
Maternal and child health care and other reproductive and sexual health care services for rural women are provided through a network of clinics run by the Ministry of Health. All of the clinics offer maternal and child health care services as well as HIV prophylaxis and treatment completely free of charge. Most women may receive antenatal care and have deliveries in a clinic of their choice, but some, depending on the assessed risk level of their pregnancy, may be referred to a clinic that offers more sophisticated care. Ensuring that all births take place at maternity clinics is an important priority for local health authorities. To that effect, almost all maternity clinics have an “expectant mother home,” which is typically a rustic facility where women can stay while waiting for labor to start. A pregnant woman’s stay at such a facility is free of charge, but she and her family must supply their own food and take care of whatever other nonmedical needs she has. Our field observations suggest that expectant mother homes are underutilized because of the need to provide food and other supplies to the pregnant woman, and because a prolonged stay removes the woman from home care and other productive activities in which local women typically engage until the day of delivery.24 Nonetheless, compared with many other parts of Mozambique and of rural Sub-Saharan Africa, the area has a considerable penetration of maternal and child health services; the vast majority of pregnant women receive at least one antenatal consultation, and a high share of births take place in health facilities. Yet, despite considerable progress in provision of maternal and child health services and continuing efforts to ensure universal institutional deliveries, a substantial fraction of births still occur outside the clinic walls.
RESEARCH QUESTIONS AND HYPOTHESES
Guided by the growing programmatic interest in barriers to universalization of safe and skilled facility-based child delivery services, our primary interest here is to understand the spatial, seasonal and institutional reasons why, in a setting where institutional deliveries are increasingly common, a substantial minority of women continue to deliver their babies outside of health facilities. Accordingly, we define our outcome as out-of-facility delivery; because almost all such deliveries take place at home, hereafter we also refer to them as “home births.” From the literature, we assume that the distance between individuals’ homes and clinics providing maternal and child health services should have significant influence on their use of such services, regardless of other factors. We hypothesize that women who live in close proximity to a greater number of clinics are less likely than other women to have a home delivery, all other things being equal (Hypothesis 1). We also consider distance from residence to towns. Because infrastructure—especially that related to roads, transportation and communication systems—typically is more developed closer to urban areas, we hypothesize that greater proximity to towns is negatively associated with the probability of a home delivery, regardless of other characteristics (Hypothesis 2).
With respect to seasonality, we distinguish between months of high precipitation and those of low precipitation. Precipitation may be a proxy for ease of physical access to health facilities; for example, heavy rains can make roads impassable.15 Such rains also can impair the functioning of health facilities.13 Furthermore, precipitation correlates with the demand for women’s labor: Local agricultural activities rely almost exclusively on women’s labor, and their activities are much more intense during the rainy season than during the dry season. For these reasons, we hypothesize that births that take place during months when precipitation and agricultural activity are highest are more likely to occur outside of clinics than are births that take place during months of low precipitation and low agricultural intensity (Hypothesis 3).
For the institutional dimension, we investigate whether the probability of a home birth is associated with the characteristics of the clinic where a pregnant woman received antenatal care and with the woman’s experience of that care. We hypothesize that receiving antenatal care at clinics that are better equipped and provide a greater array of services is associated with a reduced likelihood of home birth (Hypothesis 4). Because antenatal care builds and reflects a woman’s connection with the health sector, we also hypothesize that the more antenatal visits a woman has, the less likely she is to deliver outside a health facility (Hypothesis 5). Next, by connecting the spatial perspective with an institutional one, we argue that consistent use of the nearest health facility (rather than use of multiple facilities) for antenatal care should strengthen a pregnant woman’s connection with formal health services; accordingly, we hypothesize that women who receive most of their antenatal care at the nearest maternal and child health clinic are less likely to have a home birth than those whose antenatal care takes place primarily at more distant facilities (Hypothesis 6). Finally, we want to account for exposure to the expanding HIV services in the study area; HIV testing and counseling, which for women is done mainly during antenatal visits, may further underscore for women the importance of formal health care and thus strengthen their motivation for giving birth in a clinic. We use HIV testing experience as a proxy for exposure to HIV services, and anticipate that women who have an HIV test prior to the focal birth are less likely than other women to have that birth outside a health facility (Hypothesis 7).
DATA AND METHODS
Data
We used data from the 2009 wave of a population-based longitudinal survey called “Childbearing in a Setting of High HIV Prevalence and Rapid ART Rollout.” In 2006, for the survey’s first wave, 1,680 married women aged 18–40 were selected through multistage probability sampling in 56 villages of four contiguous districts of Gaza province in southern Mozambique. Within each district, villages were selected with probability proportional to size. About 30 women in each village were then chosen to be interviewed. The women were reinterviewed in 2009. The retention rate between survey waves for surviving women was 86%, and the participation rate in both waves exceeded 95%. Women who could not be reinterviewed in the second wave because they had migrated outside of the study area (typically to South Africa) or died were replaced through random sample refreshment. In both waves, the survey collected detailed information on women’s and their households’ demographic and socioeconomic characteristics, as well as pregnancy and birth histories for each respondent. Geographic coordinates of participants’ residences were also recorded. The analytic sample consisted of the 1,373 women in a marital union (either formalized or not) who had had a birth in the five years preceding the survey and had had at least one antenatal consultation before that birth.
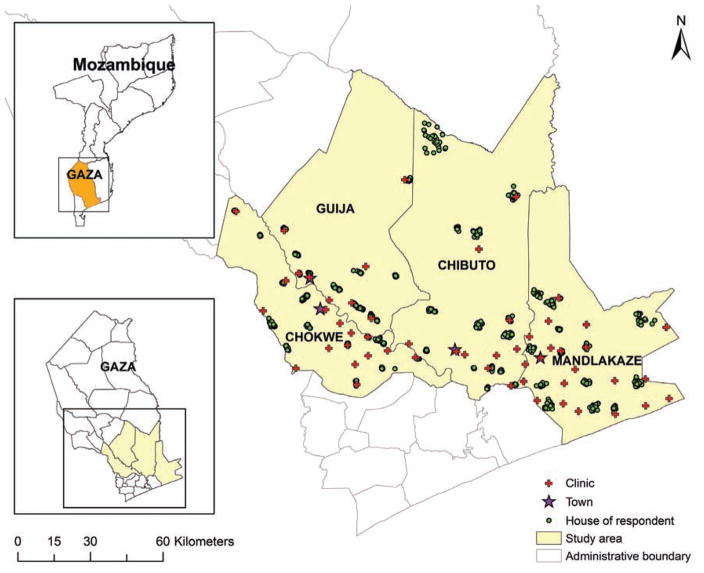
We complement the women’s survey with data from a roughly concurrent survey of all 53 maternal and child health clinics in the four districts. For this survey, staff members (usually nurses) at each clinic were interviewed about the types of maternal and child health services provided, the number and characteristics of patients, and challenges in the provision of services. In addition, monthly statistics were collected from each clinic on antenatal care, deliveries, prevention of mother-to-child HIV transmission and other services. Figure 1 shows the location of survey respondents’ houses and of the maternal and child health clinics in the study area. Note that the surveyed villages and clinics are predominantly concentrated in the southern part of the study area, reflecting the distribution of its population.
FIGURE 1.
Locations of survey respondents’ residences and maternal and child health clinics, Gaza province, Mozambique, 2009
METHODS
The study employs a combination of exploratory spatial data analysis (ESDA) and geographic information systems (GIS) techniques with confirmatory logistic regression. ESDA and GIS are used to explore spatial variations and patterns of home deliveries and to identify variables associated with place of delivery, which are then tested as covariates in multilevel logistic regression models.
First, we used desktop mapping as a straightforward way to represent and visualize spatial information and to explore the general spatial distribution within the survey area of participating women’s most recent delivery. For this analysis, survey data are used to construct covariates that are aggregated at the community level and then mapped in a GIS environment to examine regional variation in place of delivery. In addition, we illustrate the spatial pattern of institutional child deliveries using lines connecting each residence to the relevant clinic of delivery, and compute the distances between residences and clinics. The GIS-based visualizations, mapping and computations are performed using ArcGIS 10.
Next, we employed ESDA to investigate spatial patterns of institutional and noninstitutional delivery. ESDA is a collection of techniques to describe and visualize spatial patterns by graphic and map-based visualization and to facilitate hypothesis formulation and testing.25,26 In this study, the spatial scan statistics based on probability models are used to explore spatial clustering of out-of-facility deliveries. Typically, a cluster in health research represents a group of individuals with unusually high or low rates of a medical condition or outcome of interest.27,28 In this study, we define a cluster as a group of surveyed women that has a significantly high or low rate of out-of-clinic child delivery. We identify such clusters using a spatial scan statistic that employs a predefined window (circular or elliptical) with variable size that scans over the study area. We use the Bernoulli model proposed by Kulldorff29 for binary data, as the outcome has two possible values (out-of-clinic vs. in-clinic delivery). The spatial scan statistics are calculated using SaTScan software. Finally, we fit a multilevel multivariate logistic regression to investigate associations between the place of delivery and the theoretically relevant covariates. As noted earlier, the regression analysis is limited to women who had had at least one antenatal consultation prior to their last delivery (more than 98% of the sample), thus excluding women who were completely disconnected from the formal health care sector during their last pregnancy. Also, the few women who were outside the study area during their last pregnancy and had their antenatal consultations in clinics other than those covered in the clinic survey are excluded from the analysis because we do not have information on the location of or services provided by those clinics. The outcome of interest is whether the woman’s last delivery took place outside a health facility (home delivery).
To test our hypotheses regarding the relationship between spatial, seasonal and institutional characteristics and place of delivery, we define three corresponding groups of predictors. The spatial dimension is represented by two covariates: number of clinics within a 10-kilometer radius of the respondent’s residence and distance from the respondent’s residence to the nearest town (district headquarters). The first covariate, selected on the basis of the results of the descriptive spatial analysis, captures access to health care services; the second measures proximity to more economically developed areas in the study region.
To examine possible seasonal variation in the likelihood of out-of-clinic deliveries, we try two slightly different approaches. First, we use data obtained from Mozambique’s National Meteorological Service on the amount of precipitation in millimeters for the month of last birth. Because the meteorological service does not report precipitation for each of the four districts, we use data for the larger areas that include or are closest to respondents’ homes. Rather than use a continuous specification, we subdivide the distribution into four quartiles and create four dummy variables, ranked on the basis of average amount of precipitation (the first and fourth quartiles correspond to the lowest and highest levels of precipitation, respectively). This approach guards against likely imprecision in the rainfall data and also allows for exploring nonlinearity in the association between precipitation and place of delivery. If a woman could not name the month of her last child’s birth (2% of cases), we imputed the modal month for that year.
Instead of monthly precipitation, the second approach uses the type of season in which the birth took place. We use three dummy variables that classify births according to whether they occurred from April to October (generally the dry season, when the intensity of agricultural activities is low), from November to March (typically the rainy, high-intensity agricultural season) or at an unknown time (i.e., the respondent did not remember the month of birth). This approach, though admittedly cruder than the one based on monthly precipitation, permits taking into account not just rainfall but also the socioeconomic dimension of seasonality. Because the association between distance and place of birth may differ between the rainy and dry seasons, we also explore the data for possible interactions between measures of distance and seasonality.
Finally, the institutional experience dimension is represented by four variables. The first three—whether a woman had an HIV test prior to the focal birth; the number of antenatal consultations she had during the focal pregnancy; and whether more than half of those consultations took place in the nearest clinic—are based on information from women’s reports and serve as proxies for their encounters with reproductive health services. The fourth variable, the service quality of the clinic where most of the woman’s antenatal consultations occurred, is measured on a scale from 1 to 4, and is constructed on the basis of such clinic characteristics as number of staff, size and characteristics of facility, and whether it received support from any non-governmental organizations; additional details are available elsewhere.30 The information on clinic characteristics that is used to compute the service quality score was collected through the previously mentioned survey of clinics and is available only starting in 2008. For births before 2008, we extrapolate these characteristics to the previous three years, on the assumption that clinic characteristics did not change substantially during that period.
We are interested in the potential effects of space, season and institutional exposure net of individual and household characteristics. Accordingly, we include a battery of relevant control variables. The regression models adjust for women’s age and parity, because older women and those with a larger number of children could feel more comfortable than younger, lower-parity women about having a delivery without professional assistance. Whether a woman had ever experienced a reproductive loss (miscarriage or stillbirth) prior to the focal birth is a proxy for her awareness of risks of unsafe delivery. We control for women’s educational level (in years) because previous research has demonstrated that more educated women are less likely than others to give birth outside of health facilities. If use of health care services is related to household resources, then women living in more affluent households will be less likely than those living in poorer households to have a home delivery. We therefore adjust for household material conditions using a scale of 1 to 4 constructed on the basis of household ownership of such items as a radio, bicycle, motorcycle and automobile. We also adjust for two characteristics of respondents’ marriages. Women married to labor migrants may be less likely than their peers to reach a health facility, because their husband may not be around to help. Likewise, women in a polygynous marriage may receive less support from their husband than do monogamously married women (although, alternatively, the presence of co-wives may facilitate delegation of child care and of household and productive duties, thus enabling women to travel to health facilities). Finally, we include a dichotomous variable that separates women who are affiliated with an organized religion from those who are not; the encouragement and support of coreligionists may increase the likelihood of a woman’s reaching a clinic for delivery. Although the analysis looks at births that occurred up to five years before the survey, we assume that individual and household characteristics did not change substantially during that period.
We start the regression analysis with a baseline model that includes only individual and household characteristics as predictors. We then add institutional experience, spatial characteristics and season (represented either by the precipitation dummies or the dummies for the season of birth). We also examine the data for substantively meaningful interactions. At the exploratory stage, we tested various specifications of covariates (e.g., continuous vs. categorical; different classification of categorical variables); the specifications used in the presented analyses are those that are both contextually meaningful and provide the best fit for the data.
A random-intercept approach is employed in all models to account for shared unobserved characteristics due to respondents’ clustering within villages. For all models we test for multicollinearity to ensure that the covariates are not highly correlated; the results of these tests are not shown but are available from the authors. All models are fitted using the xtlogit routine in STATA 14.
RESULTS
Descriptive Statistics
Table 1 describes the individual, household, institutional, spatial and seasonal characteristics associated with deliveries that occurred at a health facility or outside a health facility. Mean age did not differ between women who had their last delivery at a clinic and those who had it outside a clinic. Women who had institutional deliveries had fewer children prior to the reference birth (3.2 vs. 3.5) and were somewhat better educated than women with home deliveries (3.2 vs. 2.6 years). Women in both categories had similarly high levels of polygamous marriages and participation in organized religion, but the proportion whose husbands migrated for work was slightly higher among those with institutional deliveries (42% vs. 37%). Women who delivered at health facilities also tended to live in somewhat better-off households.
TABLE 1.
Characteristics associated with in-facility and out-of-facility deliveries, Gaza province, Mozambique, 2004–2009
| Characteristic | In-facility(N = 972) | Out-of-facility (N = 401) |
|---|---|---|
| Women | ||
| Age (yrs.) | 29.6 | 29.9 |
| No. of previous children | 3.2 | 3.5 |
| Education (yrs.) | 3.2 | 2.6 |
| % in polygamous marriage | 20.9 | 20.2 |
| % whose husband migrates for work | 41.7 | 36.9 |
| Household material status score‡ | 2.1 | 1.9 |
| % belongs to an organized religion | 93.4 | 90.8 |
| % had reproductive loss before last delivery | 24.7 | 26.4 |
| Institutional experience | ||
| No. of antenatal consultations before delivery | 4.2 | 4.1 |
| % had most antenatal consultations at nearest clinic | 70.8 | 55.6 |
| % had an HIV test during or before year of delivery | 50.6 | 48.4 |
| Service quality score of primary antenatal clinic§,‡ | 2.4 | 2.7 |
| Spatial | ||
| No. of clinics within 10 km of woman’s home | 2.0 | 1.8 |
| Distance from woman’s village to nearest town (km) | 23.7 | 20.4 |
| Seasonal | ||
| % of deliveries occurred during rainy or high agricultural season | 35.2 | 41.9 |
On a scale from 1 to 4.
Refers to clinic where woman had most of her antenatal consultations.
Notes: All values are means unless otherwise indicated. Sample includes only each woman’s last delivery. km=kilometers.
In both categories, women had had an average of four antenatal consultations, and about half had been tested for HIV prior to the focal birth. However, the proportion who had received most prenatal care at their nearest clinic was much higher among women with institutional deliveries than among those with home births (71% vs. 56%). Interestingly, the clinics where women with institutional deliveries had most of their antenatal consultations had lower service quality scores, on average, than did the clinics where women with noninstitutional deliveries received most of their antenatal care (2.4 vs. 2.7). Overall, about 85% of the sample had at least one clinic within 10 kilometers of their residence (not shown); the average number was slightly higher among women with institutional births than among women with home births. Women who had had institutional deliveries lived farther from towns, on average, than did women who had delivered their baby at home. Finally, the proportion of deliveries that took place during the rainy season was higher for home births than for institutional births (42% vs. 35%).
Exploratory Spatial Analysis
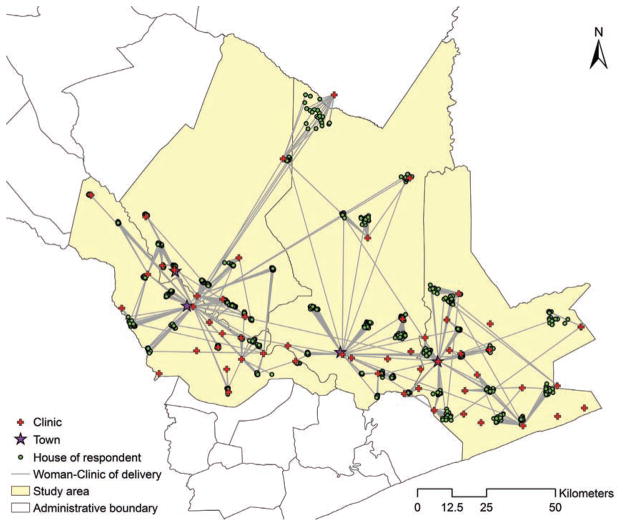
More than two-thirds (71%) of women in the sample had had their last deliveries at a maternal and child health clinic, illustrating the relatively high institutional coverage in the study area. Figure 2 shows the locations of clinics where women had their most recent deliveries. It is clear from the map that women did not necessarily deliver at the closest clinic and that women from the same village often gave birth in different clinics. Also, some clinics, especially the four larger clinics located in towns (district headquarters), attracted more women than did other clinics.
FIGURE 2.
Location of clinic of delivery and place of residence for survey respondents whose last delivery took place in a maternal and child health clinic, Gaza province, Mozambique, 2004–2009
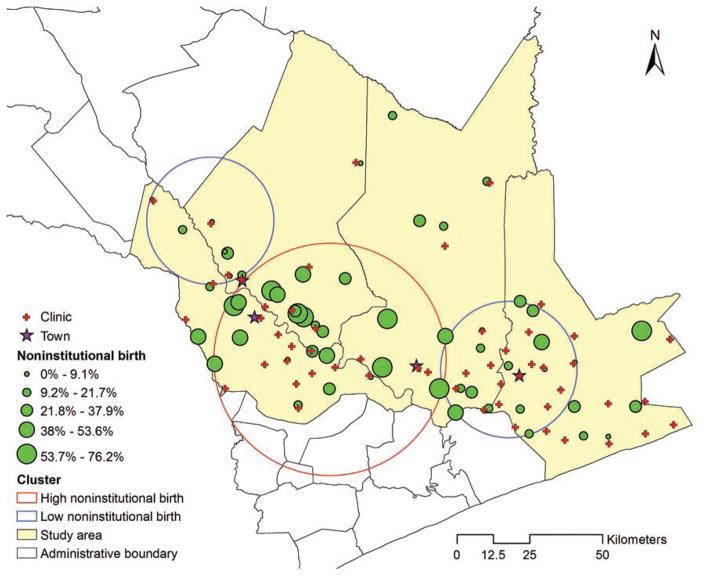
Figure 3 shows the spatial variation across the study area in the proportion of deliveries that occurred at home. Each community (village) is represented by a green dot whose size indicates the proportion of deliveries that occurred at home among surveyed women in that community. It is evident that women living in the northern part of the study area (i.e., in more remote and less economically developed villages) were the most likely to have had their last births in clinics, and similar patterns can be observed in the western and eastern parts of the study area. In contrast, home deliveries were most common among respondents living in the middle south. The results obtained from the spatial scan statistics further describe the clusters with significantly high or significantly low rates of institutional deliveries, which are indicated by red and blue circles, respectively. Two low-value clusters were identified, one in the east (where 9% of deliveries occurred at home, compared with the average value of 29%) and the other in the west (where 17% of deliveries occurred at home). A high-value cluster was in the middle south (where 41% of deliveries took place at home).
FIGURE 3.
Proportion of births that occurred outside of facilities, Gaza province, Mozambique, 2004–2009
Notably, the villages in the high-rate cluster in the middle south are close to many local clinics; they generally are also close to district headquarters, paralleling the pattern in the descriptive comparisons presented in Table 1. These findings may seem counterintuitive, given the conventional assumption that home deliveries should be more common in more remote areas. While ESDA produces intriguing insights into spatial patterns of delivery service utilization, it does not allow for a formal test of the relative importance of spatial factors. This formal test is accomplished with multivariate regression analysis.
Multivariate Regression Analysis
Table 2 displays the results of three random-intercept multivariate logistic regression models examining the probability that women had their most recent delivery outside a health facility. As a reminder, only married women who had at least one antenatal consultation during the focal pregnancy and whose pregnancy ended in a live birth are included in this analysis. We start with a model that includes only individual- and household-level variables. Model 2A adds the spatial, temporal and institutional measures; Model 2B includes the same predictors, but replaces the rainfall dummies with the dummies for the agricultural season of birth.
TABLE 2.
Coefficients (and standard errors) from random-intercept logistic regression analysis assessing relationship between selected characteristics and home delivery at last birth, Gaza province, Mozambique, 2004–2009
| Characteristic | Model 1 | Model 2A | Model 2B |
|---|---|---|---|
| Women | |||
| Age (yrs.) | −0.026 (0.017) | −0.028 (0.017)† | −0.029 (0.017)† |
| No. of previous children | 0.161 (0.059)** | 0.167 (0.060)** | 0.172 (0.060)** |
| Education (yrs.) | −0.055 (0.032)† | −0.048 (0.032) | −0.047 (0.032) |
| Polygamous marriage | −0.016 (0.171) | −0.007 (0.172) | −0.020 (0.172) |
| Husband migrates for work | −0.078 (0.143) | −0.062 (0.144) | −0.060 (0.144) |
| Household material status score | −0.193(0.071)** | −0.195 (0.071)** | −0.199 (0.071)** |
| Belongs to an organized religion | −0.238 (0.255) | −0.284 (0.258) | −0.275 (0.258) |
| Had reproductive loss before last delivery | 0.082 (0.157) | 0.087 (0.158) | 0.086 (0.158) |
| Institutional experience | |||
| No. of antenatal consultations before delivery | na | −0.033 (0.037) | −0.026 (0.037) |
| Had most antenatal consultations at nearest clinic | na | −0.045 (0.224) | −0.061 (0.224) |
| Had HIV test during or before year of delivery | na | −0.167 (0.143) | −0.197 (0.143) |
| Service quality score of primary antenatal clinic | na | 0.034 (0.124) | 0.036 (0.124) |
| Spatial | |||
| No. of clinics within 10 km of woman’s home | na | −0.277 (0.113)** | −0.273 (0.112)* |
| Distance from woman’s village to nearest town (km) | na | −0.031 (0.012)** | −0.031 (0.012)** |
| Seasonal | |||
| Monthly rainfall (ref=1st quartile) | |||
| 2nd quartile | na | 0.258 (0.192) | na |
| 3rd quartile | na | 0.183 (0.196) | na |
| 4th quartile | na | 0.364 (0.109)† | na |
| Season (ref=dry/low agricultural) | |||
| Rainy/high agricultural | na | na | 0.364 (0.141)** |
| Unknown | na | na | 0.455 (0.438) |
| Intercept | −0.060 (0.516) | 1.171 (0.819) | 1.220 (0.811) |
| Level-two variance | 1.130 (0.151)** | 1.036 (0.153)** | 1.032 (0.152)** |
| Model chi-square | 24.3** | 39.8** | 42.8** |
p<.05.
p<.01
p<.10.
Notes: na=not applicable. km=kilometers. ref=reference category.
In Model 1, the likelihood of having a home birth significantly increased with parity. As in the bivariate comparisons, a woman’s likelihood of having given birth outside a clinic rose with greater educational attainment, but this association was only marginally significant (p<.10). Household material status was significantly associated with place of delivery: Net of other factors, women living in more affluent households were less likely than poorer women to have a home birth. Marital characteristics, religious affiliation and prior reproductive complications were not associated with place of delivery.
Model 2A adds the three blocks of predictors of interest. In the spatial block, the number of maternal and child health clinics within a 10-kilometer radius was strongly and negatively associated with the likelihood of a home delivery (coefficient, −0.28), supporting Hypothesis 1. At the same time, contrary to Hypothesis 2—but in congruence with the earlier observed spatial patterns—distance to town was negatively associated with home deliveries (coefficient, −0.03); the equivalent odds ratio is 0.97, indicating that with every additional kilometer of distance between a woman’s village and the nearest town, the odds of having had a home birth decreased by 3%, which added up to a non-negligible cumulative magnitude as distance between residence and nearest town grew. Model 2A also includes the dummies for rainfall. Compared with births that occurred in the lowest-precipitation months, those that occurred during the highest-precipitation months were more likely to take place at home, though this association fell just short of statistical significance (p<.06).
In Model 2B, the rainfall dummy variables are replaced with dummies for agricultural season; the model fit statistic suggests that this specification provides a slightly better fit to the data. This model shows that births that occurred during the agriculturally intensive months were more likely to take place outside of clinics than those occurring in the lower agricultural season. The coefficient (0.36) is equivalent to an odds ratio of 1.44, indicating that the odds of a home delivery among women who gave birth during the high agricultural season were 44% higher than those of women who gave birth during the rest of the year. Hypothesis 3 is therefore supported. We explored the data for possible interactive associations between space and time, but no significant patterns emerged, paralleling the findings by Gabrysch et al.13 Thus, the associations of distance and season with place of delivery were additive rather than interactive.
The service quality scale score of the clinic where most of a woman’s antenatal consultations took place was not associated with home births. Thus, Hypothesis 4 is not supported. Similarly, none of the three proxies for reproductive care experience—number of antenatal consultations, whether a woman had most of her antenatal care in the nearest clinic and whether she had had an HIV test—were associated with place of delivery. Hypotheses 5, 6 and 7 are therefore not supported.
The addition of spatial and temporal characteristics in Models 2A and 2B did not alter the associations of parity and household material conditions with place of delivery: Both remained highly statistically significant. The association of mother’s education, already rather small in magnitude and only marginally significant in the previous model, were not statistically significant. Conversely, the negative, nonsignificant coefficient for age became marginally significant. As in Model 1, none of the other control variables were significantly associated with the likelihood of having an out-of-facility delivery.
The level-two (community-level) variance was statistically significant in all three models, indicating that women living in the same village shared similar patterns in place of delivery even after the covariates included in the model were taken into account. This correlation may be attributable to such characteristics as unmeasured spatial factors (e.g., access to public transportation or the quality of roads), unmeasured characteristics of local clinics, or the communication and social influence of neighbors. The significant intracommunity correlation suggests the need for further research on this issue.
DISCUSSION
Although the study area represents a relatively developed part of rural Mozambique—it has a fairly dense network of health facilities, and women have nearly universal access to at least some antenatal care—almost 30% of all births in the area still occur outside of health facilities and without professional obstetric care. Our analyses offer some instructive insights into the multidimensional factors that may contribute to the persistence of noninstitutional deliveries.
The analyses detected no net associations between the proxies for women’s experiences with maternal and child health care—the place or the number of antenatal consultations, whether most of those consultations took place at the nearest clinic, exposure to HIV testing and counseling, and the service quality of the clinic where antenatal consultations took place—and place of delivery. This result parallels conclusions of a recent study in rural Ghana in which a clinic’s capacity to provide maternal services was not associated with utilization.18 We should again acknowledge, however, that that we do not have individualized measures of women’s encounters with maternal and child health clinics. Qualitative research in Sub-Saharan Africa, including Mozambique, suggests that women often avoid health facilities for maternal delivery because of the poor treatment they receive from clinic staff.31,32 Also, quality of care is very difficult to measure accurately,10,33 and the results might have been different had we had more refined quality-of-service indicators.
In contrast to institutional experience, the spatial dimension proved highly relevant to place of child delivery. The analyses clearly indicate that the greater the number of clinics within a reasonable travel distance of a woman’s residence, the more likely she was to deliver her child at one of them. Yet, intriguingly, we found that women living in communities located closer to towns (district headquarters) were, other things being equal, less likely than those who lived further away to deliver their babies at health facilities. This pattern first emerged in the bivariate comparisons and in the spatial exploration of the village-level clustering of noninstitutional births, and was confirmed in the multivariate regression model. The negative association between distance to town and the probability of home delivery was robust to a different specification of the model, thus excluding the possibility of multicollinearity. Finally, we detected the predicted association between season of birth and the likelihood of home delivery. The association was marginally significant when seasonality was measured as the amount of precipitation, but was highly statistically significant when we dichotomized time of birth as rainy season versus dry season.
We should note that our data do not contain information on reasons for noninstitutional deliveries. An underlying assumption in the literature on place of delivery is that most women would prefer to give birth in a health facility, and that out-of-clinic births happen because of constraints on achieving those preferences. In some instances, however, this may not be the case. For example, the positive net association between parity and the likelihood of delivering a child outside a clinic might reflect higher-parity women’s experiences of child delivery and lower perceived need for professional birth assistance.11,33 Yet, at the same time, elevated child-care demands on higher-parity women may undermine their ability to reach a health facility in time for delivery. Likewise, heavy rains can disrupt transportation or make walking paths impassable; however, perhaps more important, the rainy season is also the time when rural women are most involved in agricultural activities and the opportunity costs of missing even a few days of work while waiting at the clinic’s expectant mother home for labor to start may be particularly high.
Another potential contributor to the persistence of noninstitutional deliveries is what can be described as the inertia of the health care system. A generation ago, when the number of health facilities was much smaller and their outreach was much more limited, national health authorities invested heavily in training traditional midwives. At the time, equipping community-based informal providers with knowledge and skills for safer home child delivery looked like the most cost-effective way to reduce the incidence of life-threatening complications of noninstitutional births. Ironically, the success of that earlier approach may now be slowing the spread of current efforts: Some of the traditional midwifes who continue to practice the skills they were once made to learn may offer pregnant women a convenient and trustworthy alternative to an institutional delivery, despite the authorities’ efforts to discourage home births. Although we do not have systematic data to support this argument, our community-based observations point to its plausibility, while evidence from other settings in Mozambique and elsewhere confirm the importance of women’s trust in traditional birth attendants.31–33 Interestingly, our observations also suggest that traditional midwives are particularly active in villages located relatively close to towns, which may help to shed light on the counterintuitive association between place of delivery and distance to nearest town detected in our statistical test.
Several additional limitations of the analysis must be acknowledged. Although the overwhelming majority of pregnant women in the study site had received at least one antenatal consultation, the few who had not and were excluded from the analysis may have been different from the majority with respect to some characteristics. Euclidean distance between residence and clinic and between village and town does not take into account population density, proximity to roads, availability and frequency of transportation, or walking paths; unfortunately, information on these characteristics was not available. The time of day when women go into labor may also affect the place of birth; for instance, women who go into labor at daybreak may be more likely to reach a clinic to give birth than women whose labor starts between dusk and dawn, when no transportation is available and walking may be unsafe. We were not able to adjust our analyses for this variable because of data constraints.
In sum, more specialized data are needed to explore in depth women’s motivations for the choice of delivery location as well as the spatial, temporal and institutional barriers that may constrain that choice. However, even in the absence of such detailed data, our study provides important insights to guide future directions in data collection and analysis. Even more important, perhaps, our study offers valuable guidance to current efforts aimed at assuring universal institutional deliveries in Sub-Saharan Africa and elsewhere in the global south. As our findings suggest, to be successful these efforts must be multidimensional. Continued endeavors to improve physical access to clinics in more remote, harder-to-reach areas are necessary. Yet, interventions beyond the health care system may be required to further reduce the level of out-of-facility births. If the demands on women’s time, along with their economic insecurities, represent major barriers to institutional delivery, these challenges are difficult to address through the health care system alone. Instead, more holistic interventions to improve women’s livelihoods should be a necessary complement to expanding their access to health facilities.
Acknowledgments
The authors gratefully acknowledge the support of the Eunice Kennedy Shriver National Institute of Child Health and Human Development (grants R21HD048257, R01HD058365 and R01HD058365–03S1) for data collection.
Contributor Information
Victor Agadjanian, Professor, Department of Sociology, University of Kansas, Lawrence, KS, USA.
Jing Yao, Lecturer, School of Social and Political Sciences, University of Glasgow, UK.
Sarah R. Hayford, Associate professor, Department of Sociology and Institute for Population Research, Ohio State University, Columbus, OH, USA
References
- 1.Elo IT. Utilization of maternal health-care services in Peru: the role of women’s education. Health Transition Review. 1992;2(1):49–69. [PubMed] [Google Scholar]
- 2.Raghupathy S. Education and the use of maternal health care in Thailand. Social Science & Medicine. 1996;43(4):459–471. doi: 10.1016/0277-9536(95)00411-4. [DOI] [PubMed] [Google Scholar]
- 3.Wagle RR, Sabroe S, Nielsen BB. Socioeconomic and physical distance to the maternity hospital as predictors for place of delivery: an observation study from Nepal. BMC Pregnancy and Childbirth. 2004;4(1):8. doi: 10.1186/1471-2393-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moyer CA, Mustafa A. Drivers and deterrents of facility delivery in sub-Saharan Africa: a systematic review. Reproductive Health. 2013;10(1):40. doi: 10.1186/1742-4755-10-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dalal K, et al. Economic empowerment of women and utilization of maternal delivery care in Bangladesh. International Journal of Preventive Medicine. 2012;3(9):628–636. [PMC free article] [PubMed] [Google Scholar]
- 6.Jain AK, Sathar ZA, ul Haque M. The constraints of distance and poverty on institutional deliveries in Pakistan: evidence from georeference-linked data. Studies in Family Planning. 2015;46(1):21–39. doi: 10.1111/j.1728-4465.2015.00013.x. [DOI] [PubMed] [Google Scholar]
- 7.Idris SH, Gwarzo UMD, Shehu AU. Determinants of place of delivery among women in a semi-urban settlement in Zaria, Northern Nigeria. Annals of African Medicine. 2006;5(2):68–72. [Google Scholar]
- 8.Nwakoby BN. Use of obstetric services in rural Nigeria. Journal of the Royal Society of Health. 1994;114(3):132–136. doi: 10.1177/146642409411400304. [DOI] [PubMed] [Google Scholar]
- 9.Pathak PK, Singh A, Subramanian SV. Economic inequalities in maternal health care: prenatal care and skilled birth attendance in India, 1992–2006. PLoS ONE. 2010;5(10):e13593. doi: 10.1371/journal.pone.0013593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seljeskog L, Sundby J, Chimango J. Factors influencing women’s choice of place of delivery in rural Malawi—an explorative study. African Journal of Reproductive Health. 2006;10(3):66–75. [PubMed] [Google Scholar]
- 11.Amooti-Kaguna B, Nuwaha F. Factors influencing choice of delivery sites in Rakai district of Uganda. Social Science & Medicine. 2000;50(2):203–213. doi: 10.1016/s0277-9536(99)00275-0. [DOI] [PubMed] [Google Scholar]
- 12.Hounton S, et al. Accessibility and utilisation of delivery care within a Skilled Care Initiative in rural Burkina Faso. Tropical Medicine & International Health. 2008;13(Suppl 1):44–52. doi: 10.1111/j.1365-3156.2008.02086.x. [DOI] [PubMed] [Google Scholar]
- 13.Kruk ME, et al. Women’s preferences for place of delivery in rural Tanzania: a population-based discrete choice experiment. American Journal of Public Health. 2009;99(9):1666–1672. doi: 10.2105/AJPH.2008.146209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bohren MA, et al. Facilitators and barriers to facility-based delivery in low- and middle-income countries: a qualitative evidence synthesis. Reproductive Health. 2014;11(1):71. doi: 10.1186/1742-4755-11-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gabrysch S, et al. The influence of distance and level of care on delivery place in rural Zambia: a study of linked national data in a geographic information system. PLoS Medicine. 2011;8(1):e1000394. doi: 10.1371/journal.pmed.1000394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Johnson FA, Padmadas SS, Brown JJ. On the spatial inequalities of institutional versus home births in Ghana: a multilevel analysis. Journal of Community Health. 2009;34(1):64–72. doi: 10.1007/s10900-008-9120-x. [DOI] [PubMed] [Google Scholar]
- 17.Kumar S, Dansereau EA, Murray CJL. Does distance matter for institutional delivery in rural India? Applied Economics. 2014;46(33):4091–4103. [Google Scholar]
- 18.Masters SH, et al. Travel time to maternity care and its effect on utilization in rural Ghana: a multilevel analysis. Social Science & Medicine. 2013;93:147–154. doi: 10.1016/j.socscimed.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 19.Diamond-Smith N, Sudhinaraset M. Drivers of facility deliveries in Africa and Asia: regional analyses using the Demographic and Health Surveys. Reproductive Health. 2015;12 doi: 10.1186/1742-4755-12-6. Art. 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The World Bank. Mozambique. 2014 http://data.worldbank.org/country/mozambique.
- 21.de Vletter F. Migration and development in Mozambique: poverty, inequality and survival. Development Southern Africa. 2007;24(1):137–153. [Google Scholar]
- 22.Ministério da Saúde. Moçambique Inquérito Demográfico e de Saúde 2011. Maputo, Mozambique, and Calverton, MD, USA: Ministério da Saúde, Instituto Nacional de Estatística and ICF International; 2013. [Google Scholar]
- 23.Ministério da Saúde, Inquérito Nacional de Prevalência, Riscos Comportamentais e Informação sobre o HIV e SIDA em Moçambique (INSIDA) 2009: Relatório Final. Maputo, Mozambique: Ministério da Saúde; 2010. [Google Scholar]
- 24.Ruiz MJ, et al. Barriers to the use of maternity waiting homes in indigenous regions of Guatemala: a study of users’ and community members’ perceptions. Culture, Health & Sexuality. 2013;15(2):205–218. doi: 10.1080/13691058.2012.751128. [DOI] [PubMed] [Google Scholar]
- 25.Anselin L. Exploratory spatial data analysis and geographic information systems. In: Painho M, editor. New Tools for Spatial Analysis. Luxembourg: Eurostat; 1994. pp. 45–54. [Google Scholar]
- 26.Murray AT. Quantitative geography. Journal of Regional Science. 2010;50(1):143–163. [Google Scholar]
- 27.Rogerson PA, Yamada I. Statistical Detection and Surveillance of Geographic Clusters. Boca Raton, FL, USA: Chapman & Hall/CRC Press; 2009. [Google Scholar]
- 28.Jacquez GM. Spatial cluster analysis. In: Fotheringham S, Wilson J, editors. The Handbook of Geographic Information Science. Malden, MA, USA: Blackwell Publishing; 2008. pp. 395–416. [Google Scholar]
- 29.Kulldorff M. A spatial scan statistic. Communications in Statistics—Theory and Methods. 1997;26(6):1481–1496. [Google Scholar]
- 30.Yao J, Murray A, Agadjanian V. A geographical perspective on access to sexual and reproductive health care for women in rural Mozambique. Social Science & Medicine. 2013;96:60–68. doi: 10.1016/j.socscimed.2013.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chapman RR. Family Secrets: Risking Reproduction in Central Mozambique. Nashville, TN, USA: Vanderbilt University Press; 2010. [Google Scholar]
- 32.Izugbara C, Ezeh A, Fotso JC. The persistence and challenges of homebirths: perspectives of traditional birth attendants in urban Kenya. Health Policy and Planning. 2009;24(1):36–45. doi: 10.1093/heapol/czn042. [DOI] [PubMed] [Google Scholar]
- 33.Gabrysch S, Campbell OMR. Still too far to walk: literature review of the determinants of delivery service use. BMC Pregnancy and Childbirth. 2009;9 doi: 10.1186/1471-2393-9-34. Art. 34. [DOI] [PMC free article] [PubMed] [Google Scholar]