Abstract
Purpose
Patients’ understanding of their illness is key for making informed treatment decisions, yet studies suggest an association between prognostic awareness and worse quality of life (QOL) and mood among patients with advanced cancer. We sought to explore the relationships among prognostic awareness, coping, QOL, and mood in patients with newly diagnosed, incurable cancer.
Methods
We assessed patients’ self-reported health status and treatment goal (Prognosis and Treatment Perceptions Questionnaire), coping (Brief COPE), QOL (Functional Assessment of Cancer Therapy-General), and mood (Hospital Anxiety and Depression Scale) within 8 weeks of incurable lung or GI cancer diagnosis. We used linear regression to examine associations and interaction effects among patients’ health status and treatment goal, coping strategies, QOL, and mood.
Results
Patients who reported a terminally ill health status had worse QOL (unstandardized coefficient [B] = −6.88; P < .001), depression (B = 1.60; P < .001), and anxiety (B = 1.17; P = .007). Patients who reported their oncologist’s treatment goal was “to cure my cancer” had better QOL (B = 4.33; P = .03) and less anxiety (B = −1.39; P = .007). We observed interaction effects between self-reported health status and treatment goal and certain coping strategies. Specifically, subgroup analyses showed that greater use of positive reframing was related to better QOL (B = 2.61; P < .001) and less depression (B = −0.78; P < .001) among patients who reported a terminally ill health status. Active coping was associated with better QOL (B = 3.50; P < .001) and less depression (B = −1.01; P < .001) among patients who acknowledged their oncologist’s treatment goal was not “to cure my cancer.”
Conclusion
Prognostic awareness is related to worse QOL and mood in patients with newly diagnosed, incurable cancer; however, the use of certain coping strategies may buffer these relationships. Interventions to improve patients’ prognostic awareness should seek to cultivate more adaptive coping strategies in order to enhance QOL and mood.
INTRODUCTION
Patients with advanced cancer prefer that their oncologists disclose their assessment of their prognosis, yet data suggest that most patients inaccurately perceive their illness as curable.1-3 In addition, patients and their oncologists often report discordant illness perceptions, with patients reporting a more optimistic assessment of their prognosis.4 Nonetheless, patients with an accurate prognostic understanding of their illness are better able to make informed treatment decisions and to prepare for the future.3,5-7 Of importance, research suggests that patient-clinician communication about prognosis does not take away patients’ hope but, rather, improves end-of-life care, such as enabling patients to die in their preferred setting and ensuring bereavement support for their family.8-10 Thus, improving patient-clinician communication about illness and prognosis is a priority for enhancing the quality of care for patients with cancer.
Despite the need for improved communication regarding prognosis, prior research has demonstrated that patients with advanced cancer who have accurate prognostic awareness are more likely to experience worse quality of life (QOL), mood symptoms, and survival.1-3,6,11,12 However, to date, studies have primarily been correlational in design, which limited the interpretation of the direction of these relationships. For example, patients with advanced cancer who have greater symptom burden and worse QOL may simply be more accurate in their assessment of their disease status and prognosis compared with those with better QOL. In contrast to these correlational studies, a randomized trial of early palliative care integrated with oncology care demonstrated that patients who were assigned to the intervention were more likely to develop or maintain accurate prognostic awareness over time, as well as to report improved QOL and depression symptoms, compared with those who received oncology care alone.13,14 Thus, to help reconcile findings from prior studies and to develop strategies that effectively enhance patients’ prognostic awareness, further research is needed to elucidate the complex relationships between prognostic awareness, QOL, and mood.
Moreover, factors such as the use of certain coping strategies may influence the relationships between patients’ prognostic awareness and their QOL and mood.15-24 After a diagnosis of incurable cancer, patients must cope with numerous stressors, including the need to make urgent treatment decisions, manage adverse effects of the diagnosis and treatment, and tolerate uncertainty regarding their future.25-30 The manner in which patients cope with their life-threatening illness likely influences their prognostic awareness and experience with their illness.31 For example, some coping strategies may allow patients to better acknowledge the terminal nature of their illness, whereas other coping mechanisms may hinder their ability to tolerate prognosis discussions.32 In addition, research has demonstrated that certain coping strategies may be more adaptive than others with regard to patients’ QOL and mood.15,18,33 Strategies such as acceptance coping positively correlate with patients’ QOL and mood, whereas denial and self-blame negatively correlate with these outcomes.15-18,33 However, little is known about the interaction between patients’ use of coping strategies and their prognostic awareness, QOL, and mood.
In the current study, we used baseline data from patients with newly diagnosed, incurable cancer to investigate associations and explore interaction effects among patients’ prognostic awareness, coping strategies, QOL, and mood. We studied two constructs of prognostic awareness by assessing patients’ self-reported health status and treatment goal. On the basis of prior research, we hypothesized that patients with a more accurate understanding of their health status and treatment goal would report worse QOL and mood, yet their use of certain coping strategies would moderate these relationships.1,12
METHODS
Study Design
We approached patients who were within 8 weeks of diagnosis with incurable cancer to participate in a randomized trial of early palliative care integrated with oncology care versus oncology care alone. Although the parent trial sought to evaluate the effect of early integrated palliative care, the current study uses data before patient random assignment and before the start of the intervention.34 After informed consent, participants completed baseline assessments before random assignment and notification of study arm allocation. The Dana-Farber/Harvard Cancer Care institutional review board approved the study protocol.
Patient Selection
The sample included patients from Massachusetts General Hospital Cancer Center with a confirmed diagnosis of incurable lung or noncolorectal GI cancer with the following characteristics: diagnosis within the previous 8 weeks, not receiving treatment with curative intent, an Eastern Cooperative Oncology Group performance status of 0 to 2, age ≥ 18 years, no prior therapy for metastatic disease, planned to receive care at Massachusetts General Hospital, and could read and respond to questions in English or with minimal assistance from family or an interpreter. We excluded patients who were already receiving palliative care services, those who needed immediate referral to palliative care or hospice, or those who had significant psychiatric or other comorbid disease, which the treating clinician believed prohibited informed consent or study participation.
Study Measures
Sociodemographic and clinical factors.
Study participants completed a baseline demographic questionnaire to report their race, ethnicity, religion, relationship status, education, presence of dependent children, and annual income. We reviewed electronic health records to obtain participants’ age, sex, Eastern Cooperative Oncology Group performance status, and cancer diagnosis, stage, and therapy.
QOL.
We used the Functional Assessment of Cancer Therapy-General (FACT-G; version 4) to assess QOL.35 The FACT-G contains 27 items with subscales that measure well-being during the past week across four domains: physical, functional, emotional, and social. Higher scores indicate better QOL.
Depression and anxiety.
To assess depression and anxiety symptoms, patients completed the Hospital Anxiety and Depression Scale (HADS).36 The 14-item HADS questionnaire contains two 7-item subscales that measure depression and anxiety symptoms during the past week. Scores on each subscale range from 0 to 21. Higher scores indicate greater distress.
Coping strategies.
To evaluate patients’ use of certain coping strategies, we administered the 28-item Brief COPE questionnaire. The 28-item Brief COPE questionnaire measures 14 coping strategies using two items for each strategy.37 To minimize questionnaire burden, we solicited feedback from our research and palliative care teams about the coping strategies that were most likely to be influenced by our early palliative care intervention. We chose to exclude items such as self-distraction, substance use, and venting, and limited our evaluation to seven coping strategies that were deemed most relevant for the study: emotional support, positive reframing, active coping, acceptance, self-blame, denial, and behavioral disengagement. Scores for each coping strategy range from 2 to 8, with higher scores reflecting greater use of that specific strategy.
Patient-reported health status and treatment goal.
We used the Prognosis and Treatment Perceptions Questionnaire—a survey previously developed to assess patients’ prognostic understanding.12 The Prognosis and Treatment Perceptions Questionnaire asks patients about their primary treatment goal, their oncologist’s primary treatment goal, and their current medical status. Specifically, we asked participants to report the primary goal of their current cancer treatment from the following mutually exclusive options: “to lessen my suffering as much as possible,” “for me and/or my family to be able to keep hoping,” “to make sure I have done everything,” “to extend my life as long as possible,” “to cure my cancer,” “to help cancer research,” or “other.” Using the same response options, we asked participants to report their oncologist’s primary goal of their current cancer treatment. For both questions, we categorized responses as either “to cure my cancer” or “not to cure my cancer,” consistent with prior studies.12,38 We asked participants to describe their current health status by choosing from the following mutually exclusive options: “relatively healthy,” “relatively healthy and terminally ill,” “seriously ill and not terminally ill,” or “seriously ill and terminally ill.” Consistent with prior research, we categorized responses as either “terminally ill” or “not terminally ill.”12
Statistical analysis.
We used descriptive statistics to evaluate the frequencies, means, and standard deviations of study variables. To examine associations between patients’ self-reported health status and treatment goal and their QOL and mood, we used linear regression. To determine the presence of an interaction between patients’ self-reported health status and treatment goal and their use of certain coping strategies (measured continuously), we used linear regression with QOL and mood (measured continuously) as outcomes. Specifically, we created an interaction term (health status [1, terminally ill; 0, not terminally ill] × coping strategy [continuous variable]; treatment goal [1, to cure my cancer; 0, not to cure my cancer] × coping strategy [continuous variable]) and included this term, along with both interaction components, as predictors in the models. In all models, we adjusted for variables that were significantly different across groups (Appendix Tables A1 and A2, online only). For each statistically significant interaction (P < .05), we performed analyses within the health status and treatment goal subgroups.39 To adjust for multiple testing in subgroup analyses, we corrected the α level by using the Bonferroni method (α = .05/20 = .0025). In addition to available case analyses, we used multiple imputations for missing observations to ensure consistent results. In our multiple imputation approach, we used characteristics—age, sex, relationship status, education, cancer type, and presence of dependent children—to build a regression model to impute missing data with 100 imputations. We used SPSS for Windows version 20 (SPSS, Chicago, IL) for statistical analyses.
RESULTS
Participant Sample
Of 480 eligible patients between May 2011 and July 2015, 350 (72.9%) enrolled in the study. As shown in Table 1, participants (mean age ± standard deviation, 64.9 ± 10.9 years) were primarily white (92.3%), married (69.7%), and educated beyond high school (62.6%). Approximately one half were female (46.0%) and had lung cancer (54.6%).
Table 1.
Baseline Characteristics of Study Participants (N = 350)

Patient-Reported Health Status and Treatment Goal
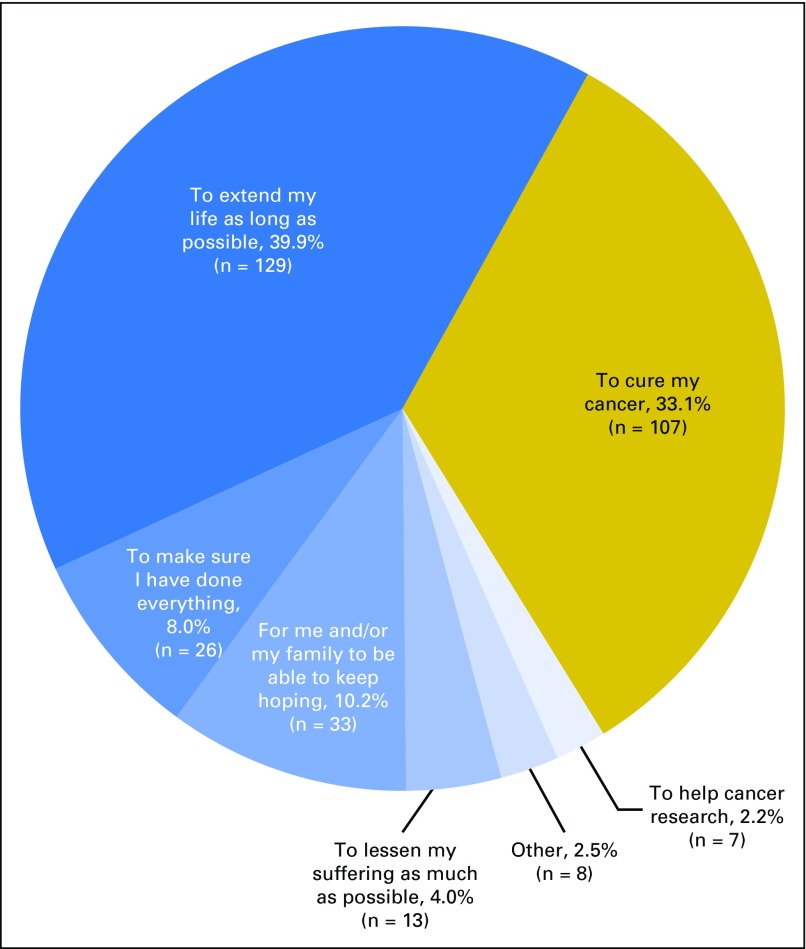
Nearly one half of participants (49.4%) reported their current health status as “terminally ill” (Fig 1). Approximately one third (33.1%) reported their primary treatment goal was “to cure my cancer” (Fig 2). Yet within this subgroup who reported their primary treatment goal was “to cure my cancer,” 44.9% acknowledged that their oncologist’s goal was not “to cure my cancer.” Among all participants, 22.8% reported that their oncologist’s primary treatment goal was “to cure my cancer” (Fig 3).
Fig 1.
Patient report of his or her current health status. Displays patient responses to the question, “How would you describe your current medical status?”
Fig 2.
Patient report of his or her primary goal of current cancer treatment. Displays patient responses to the question, “If you had to choose one, what would you say is your primary goal of your current cancer treatment?”
Fig 3.
Patient report of his or her oncologist’s primary goal of current cancer treatment. Displays patient responses to the question, “If you had to choose one, what would you say is your oncologist’s primary goal of your current cancer treatment?”
Relationship Between Patient-Reported Health Status and Treatment Goal, QOL, and Mood
Patient report of a terminally ill health status was associated with worse QOL (unstandardized coefficient [B], −6.88; standard error [SE], 1.63; 95% CI, −10.08 to −3.68; P < .001) as well as greater depression (B, 1.60; SE, 0.43; 95% CI, 0.74 to 2.45; P < .001) and anxiety (B, 1.17; SE, 0.43; 95% CI, 0.32 to 2.01; P = .007). A patient report that his or her primary treatment goal was “to cure my cancer” was not significantly associated with QOL (B, 2.79; SE, 1.79; 95% CI, −0.74 to 6.31; P = .12), depression (B, −0.27; SE, 0.47; 95% CI, −1.21 to 0.66; P = .56), or anxiety (B, −0.72; SE, 0.46; 95% CI, −1.62 to 0.19; P = .12); however, a patient report that his or her oncologist’s primary treatment goal was “to cure my cancer” was associated with better QOL (B, 4.33; SE, 2.00; 95% CI, 0.41 to 8.26; P = .03) and lower anxiety (B, −1.39; SE, 0.51; 95% CI, −2.40 to −0.38; P = .007), but not with depression (B, −0.68; SE, 0.53; 95% CI, −1.72 to 0.36; P = .20).
Interactions Between Patient-Reported Health Status and Treatment Goal and Coping Strategies
We found interactions between a patient report of a terminally ill health status and the use of certain coping strategies for QOL and mood outcomes. For QOL (FACT-G), we observed significant interactions between a report of a terminally ill health status and positive reframing (B, −1.87; SE, 0.88; 95% CI, 0.13 to 3.60; P = .04) and denial coping (B, −2.35; SE, 1.00; 95% CI, −4.33 to −0.38; P = .02). For HADS-Depression, we found interactions between a patient report of a terminally ill health status and positive reframing (B, −0.47; SE, 0.23; 95% CI, −0.93 to −0.02; P = .04) and behavioral disengagement coping (B, 1.30; SE, 0.53; 95% CI, 0.27 to 2.33; P = .01). For HADS-Anxiety, we found significant interactions between a patient report of a terminally ill health status and positive reframing (B, −0.66; SE, 0.24; 95% CI, −1.13 to −0.19; P = .006) and emotional support coping (B, −1.04; SE, 0.49; 95% CI, −2.01 to −0.08; P = .03). We obtained similar results in our models that used multiple imputations (Appendix Tables A3 and A4, online only).
To interpret these interactions, we conducted subgroup analyses of the associations between these coping strategies and patients’ QOL and mood outcomes by patient report of a terminally ill health status (Table 2). These analyses demonstrated that positive reframing coping was associated with better QOL and mood outcomes among patients who reported a terminally ill health status, but not consistently in those who did not acknowledge their terminal illness. Within the subgroup that reported a terminally ill health status, we found that behavioral disengagement correlated with greater depression, whereas emotional support correlated with less anxiety.
Table 2.
Relationship Between Patients’ Use of Coping Strategies and Their Quality of Life and Mood Outcomes by Patient Report of Their Current Health Status

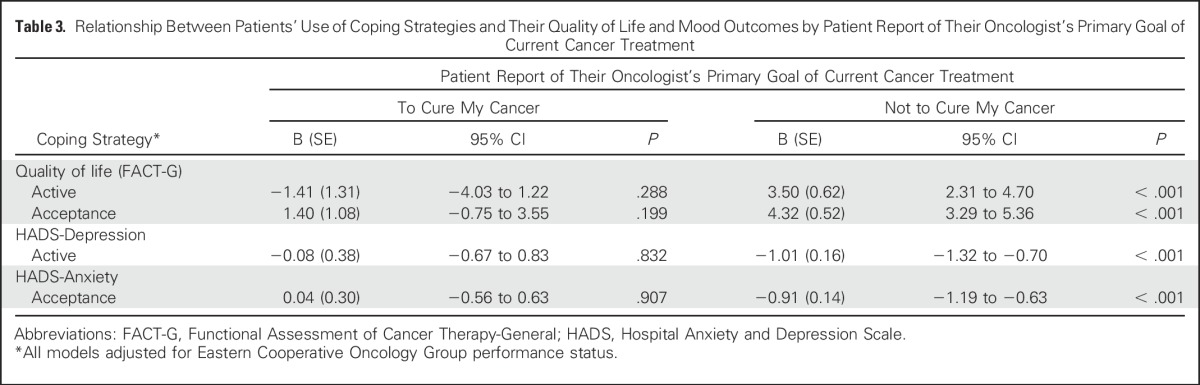
We also identified interactions between a patient report of his or her oncologist’s primary treatment goal and use of certain coping strategies for QOL and mood outcomes. With QOL (FACT-G), we found significant interactions between a patient report of his or her oncologist’s treatment goal and use of active (B, −4.78; SE, 1.47; 95% CI, −7.68 to −1.88; P = .001) and acceptance coping (B, −2.81; SE, 1.18; 95% CI, −5.13 to −0.49; P = .02). For HADS-Depression, we found an interaction between a patient report of his or her oncologist’s treatment goal and active coping (B, 1.02; SE, 0.39; 95% CI, 0.25 to 1.78; P = .009). For HADS-Anxiety, we observed a significant interaction between a patient report of his or her oncologist’s treatment goal and acceptance coping (B, 0.97; SE, 0.32; 95% CI, 0.34 to 1.61; P = .003).
Given these interactions, we conducted subgroup analyses of the associations between these coping strategies and patients’ QOL and mood outcomes by patient report of his or her oncologist’s treatment goal (Table 3). Among patients who acknowledged that their oncologist’s primary treatment goal was not “to cure my cancer,” the use of active coping was associated with better QOL and less depression. In addition, acceptance coping correlated with better QOL and less anxiety among patients who reported that their oncologist’s primary treatment goal was not “to cure my cancer.”
Table 3.
Relationship Between Patients’ Use of Coping Strategies and Their Quality of Life and Mood Outcomes by Patient Report of Their Oncologist’s Primary Goal of Current Cancer Treatment
We did not observe additional significant interactions between patients’ self-reported health status and treatment goal and any remaining coping styles. We also did not find significant interactions between patient report of his or her primary treatment goal and any coping strategies for QOL and mood outcomes.
DISCUSSION
We investigated the relationships between patients’ prognostic awareness, coping strategies, QOL, and mood. Using two constructs of prognostic awareness—patient-reported health status and treatment goal—we found that a substantial proportion of patients reported inaccurate prognostic understanding. More than one half of patients indicated that their current health status was not terminal and nearly one third noted that their primary treatment goal was “to cure my cancer.” Patients with an accurate understanding of their health status and treatment goal reported worse QOL and mood. Of note, we observed interaction effects between patients’ use of certain coping strategies and the relationships among their self-reported health status and treatment goal, QOL, and mood. Collectively, these findings provide important new evidence that patients’ coping strategies represent a key factor that may influence the relationship between patients’ prognostic awareness and their QOL and mood.
Subgroup analyses revealed that the significant relationships between patients’ use of certain coping strategies and their QOL and mood existed primarily among patients with accurate prognostic understanding. For example, among patients who accurately reported a terminally ill health status, positive reframing correlated with better QOL and less depression. Similarly, active coping was associated with better QOL and less depression among patients who accurately reported that their oncologist’s primary treatment goal was not to cure their cancer. Clinically, our findings suggest that use of adaptive coping behaviors, such as positive reframing (eg, looking for something good in what is happening), active coping (eg, taking action to try to make the situation better), acceptance (eg, accepting the reality of the fact that it happened), and seeking emotional support, provide a means for enhancing QOL and mood among patients who accurately acknowledge their poor prognosis. Future interventions designed to improve patients’ prognostic understanding should seek to foster the use of adaptive coping skills in this population.
Of interest, we discovered a lack of concordance between patients’ report of their own primary treatment goal and their report of their oncologist’s goal. Although prior studies have demonstrated patient-oncologist prognostic discordance, few have evaluated patients’ perceptions of their oncologists’ treatment goal.4,41 We found that among patients who reported their own treatment goal was to cure their cancer, nearly one half acknowledged that their oncologist’s goal differed. This discordance between patients’ understanding for themselves versus their perceptions of their oncologists’ treatment goal may reflect the presence of cognitive and emotional dissonance.42 When asked to report their primary treatment goal, patients may actually be reporting their hopes or wishes, rather than their true understanding. This disconnect may also reflect patients’ difficulty responding to questions regarding their treatment goal. Many patients may endorse that their goal or wish is to be cured, even if they simultaneously understand their cancer is incurable. Future studies that involve patients’ understanding of their illness should consider the potential role of cognitive dissonance and the need to ask patients about their prognostic awareness in various ways to gain deeper insight into their true understanding.
To our knowledge, our work represents the largest study to date to highlight that patients who acknowledge their poor prognosis report worse QOL and mood. A more comprehensive understanding of the associations among patients’ understanding of their health status and treatment goal, QOL, and mood can be instrumental in clarifying their prognostic awareness and helping them cope with the physical and psychological effects of their terminal illness; understanding how prognostic awareness can influence patients’ decision-making and approach to end-of-life care; and in identifying ways to foster prognostic awareness while enhancing patients’ QOL and mood.
Our study has several limitations. First, we conducted this study at an academic cancer center in a relatively homogenous sample; thus, our findings may not generalize to other, more diverse populations in different geographic areas. Second, we lack information about patient-clinician communication and, therefore, cannot distinguish the amount or quality of information provided to patients about their cancer. Finally, our study design allows us to comment on associations, but we cannot state the directionality of these relationships. In addition, our cross-sectional design prohibits our ability to determine how these relationships change over time. Future research should include longitudinal assessments with audio-recorded visits to provide objective information about prognostic disclosure and the effect of patient-clinician communication on patients’ prognostic awareness, coping strategies, QOL, and mood.
Our study provides novel insights into the relationships between patients’ prognostic awareness and their QOL and mood. We discovered interaction effects with patients’ use of certain coping strategies on these relationships, which underscores the importance of promoting the use of more adaptive coping strategies, particularly among patients with accurate prognostic understanding. Efforts to cultivate more adaptive coping among patients when disclosing prognosis include assessing patients’ prognostic understanding and coping mechanisms, determining their readiness and clinical urgency, and delivering prognostic information that is tailored to their needs.43,44 Future research is needed to develop and test interventions to enhance patients’ prognostic awareness and to support effective end-of-life decision-making. Such efforts would ideally address patients’ QOL and psychosocial needs while facilitating the use of more adaptive coping behaviors.
Appendix
Table A1.
Characteristics of Study Participants by Patient Report of Their Current Health Status

Table A2.
Characteristics of Study Participants by Patient Report of Their Oncologist’s Primary Goal of Current Cancer Treatment

Table A3.
Interactions Between Coping and Patient Report of Their Current Health Status Using Available Case Analyses and Multiple Imputations

Table A4.
Interactions Between Coping and Patient Report of Their Oncologist’s Primary Goal of Current Cancer Treatment Using Available Case Analyses and Multiple Imputations

Footnotes
Supported by US National Institutes of Health National Institute of Nursing Research Grant No. R01-NR012735 (J.S.T.) and National Cancer Institute Grant No. K24-CA181253 (J.S.T.).
AUTHOR CONTRIBUTIONS
Conception and design: Ryan D. Nipp, Joseph A. Greer, Areej El-Jawahri, Lara Traeger, Juliet C. Jacobsen, Emily R. Gallagher, Elyse R. Park, David P. Ryan, Vicki A. Jackson, William F. Pirl, Jennifer S. Temel
Administrative support: Emily R. Gallagher, Jennifer S. Temel
Collection and assembly of data: Ryan D. Nipp, Joseph A. Greer, Areej El-Jawahri, Samantha M. Moran, Emily R. Gallagher, David P. Ryan, William F. Pirl, Jennifer S. Temel
Data analysis and interpretation: Ryan D. Nipp, Joseph A. Greer, Areej El-Jawahri, Samantha M. Moran, Lara Traeger, Jamie M. Jacobs, Juliet C. Jacobsen, Emily R. Gallagher, David P. Ryan, William F. Pirl, Jennifer S. Temel
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Coping and Prognostic Awareness in Patients With Advanced Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/jco/site/ifc.
Ryan D. Nipp
No relationship to disclose
Joseph A. Greer
No relationship to disclose
Areej El-Jawahri
No relationship to disclose
Samantha M. Moran
No relationship to disclose
Lara Traeger
No relationship to disclose
Jamie M. Jacobs
No relationship to disclose
Juliet C. Jacobsen
No relationship to disclose
Emily R. Gallagher
No relationship to disclose
Elyse R. Park
No relationship to disclose
David P. Ryan
Stock or Other Ownership: MPM Capital
Honoraria: UpToDate, Research to Practice
Consulting or Advisory Role: MPM Capital
Patents, Royalties, Other Intellectual Property: McGraw Hill chapter royalties, Johns Hopkins University Press
Vicki A. Jackson
No relationship to disclose
William F. Pirl
No relationship to disclose
Jennifer S. Temel
Research Funding: Pfizer (Inst)
REFERENCES
- 1.Greer JA, Pirl WF, Jackson VA, et al. : Perceptions of health status and survival in patients with metastatic lung cancer. J Pain Symptom Manage 48:548-557, 2014 [DOI] [PubMed] [Google Scholar]
- 2.Weeks JC, Catalano PJ, Cronin A, et al. : Patients’ expectations about effects of chemotherapy for advanced cancer. N Engl J Med 367:1616-1625, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Epstein AS, Prigerson HG, O’Reilly EM, et al. : Discussions of life expectancy and changes in illness understanding in patients with advanced cancer. J Clin Oncol 34:2398-2403, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gramling R, Fiscella K, Xing G, et al. : Determinants of patient-oncologist prognostic discordance in advanced cancer. JAMA Oncol 2:1421-1426, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Steinhauser KE, Christakis NA, Clipp EC, et al. : Preparing for the end of life: Preferences of patients, families, physicians, and other care providers. J Pain Symptom Manage 22:727-737, 2001 [DOI] [PubMed] [Google Scholar]
- 6.Steinhauser KE, Christakis NA, Clipp EC, et al. : Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA 284:2476-2482, 2000 [DOI] [PubMed] [Google Scholar]
- 7.Steinhauser KE, Clipp EC, McNeilly M, et al. : In search of a good death: Observations of patients, families, and providers. Ann Intern Med 132:825-832, 2000 [DOI] [PubMed] [Google Scholar]
- 8.Lundquist G, Rasmussen BH, Axelsson B: Information of imminent death or not: Does it make a difference? J Clin Oncol 29:3927-3931, 2011 [DOI] [PubMed] [Google Scholar]
- 9.Smith TJ, Dow LA, Virago E, et al. : Giving honest information to patients with advanced cancer maintains hope. Oncology (Williston Park) 24:521-525, 2010 [PubMed] [Google Scholar]
- 10.Zhang B, Wright AA, Huskamp HA, et al. : Health care costs in the last week of life: Associations with end-of-life conversations. Arch Intern Med 169:480-488, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Curtis JR, Back AL, Ford DW, et al. : Effect of communication skills training for residents and nurse practitioners on quality of communication with patients with serious illness: A randomized trial. JAMA 310:2271-2281, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.El-Jawahri A, Traeger L, Park ER, et al. : Associations among prognostic understanding, quality of life, and mood in patients with advanced cancer. Cancer 120:278-285, 2014 [DOI] [PubMed] [Google Scholar]
- 13.Temel JS, Greer JA, Muzikansky A, et al. : Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 363:733-742, 2010 [DOI] [PubMed] [Google Scholar]
- 14.Temel JS, Greer JA, Admane S, et al. : Longitudinal perceptions of prognosis and goals of therapy in patients with metastatic non-small-cell lung cancer: Results of a randomized study of early palliative care. J Clin Oncol 29:2319-2326, 2011 [DOI] [PubMed] [Google Scholar]
- 15.Brunault P, Champagne AL, Huguet G, et al. : Major depressive disorder, personality disorders, and coping strategies are independent risk factors for lower quality of life in non-metastatic breast cancer patients. Psychooncology 25:513-520, 2016 [DOI] [PubMed] [Google Scholar]
- 16.Costanzo ES, Lutgendorf SK, Rothrock NE, et al. : Coping and quality of life among women extensively treated for gynecologic cancer. Psychooncology 15:132-142, 2006 [DOI] [PubMed] [Google Scholar]
- 17.Kershaw T, Northouse L, Kritpracha C, et al. : Coping strategies and quality of life in women with advanced breast cancer and their family caregivers. Psychol Health 19:149-156, 2004 [Google Scholar]
- 18.Nipp RD, El-Jawahri A, Fishbein JN, et al. : The relationship between coping strategies, quality of life, and mood in patients with incurable cancer. Cancer 122:2110-2116, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller SM: Monitoring versus blunting styles of coping with cancer influence the information patients want and need about their disease. Implications for cancer screening and management. Cancer 76:167-177, 1995 [DOI] [PubMed] [Google Scholar]
- 20.Philip EJ, Merluzzi TV, Zhang Z, et al. : Depression and cancer survivorship: Importance of coping self-efficacy in post-treatment survivors. Psychooncology 22:987-994, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roberts N, Czajkowska Z, Radiotis G, et al. : Distress and coping strategies among patients with skin cancer. J Clin Psychol Med Settings 20:209-214, 2013 [DOI] [PubMed] [Google Scholar]
- 22.Aguado Loi CX, Baldwin JA, McDermott RJ, et al. : Risk factors associated with increased depressive symptoms among Latinas diagnosed with breast cancer within 5 years of survivorship. Psychooncology 22:2779-2788, 2013 [DOI] [PubMed] [Google Scholar]
- 23.Horney DJ, Smith HE, McGurk M, et al. : Associations between quality of life, coping styles, optimism, and anxiety and depression in pretreatment patients with head and neck cancer. Head Neck 33:65-71, 2011 [DOI] [PubMed] [Google Scholar]
- 24.Kitano A, Yamauchi H, Hosaka T, et al. : Psychological impact of breast cancer screening in Japan. Int J Clin Oncol 20:1110-1116, 2015 [DOI] [PubMed] [Google Scholar]
- 25.Teunissen SC, Wesker W, Kruitwagen C, et al. : Symptom prevalence in patients with incurable cancer: A systematic review. J Pain Symptom Manage 34:94-104, 2007 [DOI] [PubMed] [Google Scholar]
- 26.Barbera L, Seow H, Howell D, et al. : Symptom burden and performance status in a population-based cohort of ambulatory cancer patients. Cancer 116:5767-5776, 2010 [DOI] [PubMed] [Google Scholar]
- 27.Mack JW, Weeks JC, Wright AA, et al. : End-of-life discussions, goal attainment, and distress at the end of life: Predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol 28:1203-1208, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brundage MD, Davidson JR, Mackillop WJ: Trading treatment toxicity for survival in locally advanced non-small cell lung cancer. J Clin Oncol 15:330-340, 1997 [DOI] [PubMed] [Google Scholar]
- 29.Hirose T, Yamaoka T, Ohnishi T, et al. : Patient willingness to undergo chemotherapy and thoracic radiotherapy for locally advanced non-small cell lung cancer. Psychooncology 18:483-489, 2009 [DOI] [PubMed] [Google Scholar]
- 30.Nipp RD, Zullig LL, Samsa G, et al. : Identifying cancer patients who alter care or lifestyle due to treatment-related financial distress. Psychooncology 25:719-725, 2016 [DOI] [PubMed] [Google Scholar]
- 31.Hopman P, Rijken M: Illness perceptions of cancer patients: Relationships with illness characteristics and coping. Psychooncology 24:11-18, 2015 [DOI] [PubMed] [Google Scholar]
- 32.Jacobsen J, Thomas Jd, Jackson VA: Misunderstandings about prognosis: An approach for palliative care consultants when the patient does not seem to understand what was said. J Palliat Med 16:91-95, 2013 [DOI] [PubMed] [Google Scholar]
- 33.Hagan TL, Fishbein JN, Nipp RD, et al. : Coping in patients with incurable lung and gastrointestinal cancers: A validation study of the Brief COPE. J Pain Symptom Manage 53:131-138, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Temel JS, Greer JA, El-Jawahri A, et al. : Effects of early integrated palliative care in patients with lung and GI cancer: A randomized clinical trial. J Clin Oncol 35:834-841, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cella DF, Tulsky DS, Gray G, et al. : The Functional Assessment of Cancer Therapy scale: Development and validation of the general measure. J Clin Oncol 11:570-579, 1993 [DOI] [PubMed] [Google Scholar]
- 36.Zigmond AS, Snaith RP: The hospital anxiety and depression scale. Acta Psychiatr Scand 67:361-370, 1983 [DOI] [PubMed] [Google Scholar]
- 37.Carver CS: You want to measure coping but your protocol’s too long: Consider the Brief COPE. Int J Behav Med 4:92-100, 1997 [DOI] [PubMed] [Google Scholar]
- 38.Nipp RD, El-Jawahri A, Fishbein JN, et al. : Factors associated with depression and anxiety symptoms in family caregivers of patients with incurable cancer. Ann Oncol 27:1607-1612, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang R, Ware JH: Detecting moderator effects using subgroup analyses. Prev Sci 14:111-120, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bennett DA: How can I deal with missing data in my study? Aust N Z J Public Health 25:464-469, 2001 [PubMed] [Google Scholar]
- 41.Weeks JC, Cook EF, O’Day SJ, et al. : Relationship between cancer patients’ predictions of prognosis and their treatment preferences. JAMA 279:1709-1714, 1998 [DOI] [PubMed] [Google Scholar]
- 42.Draycott S, Dabbs A: Cognitive dissonance. 1: An overview of the literature and its integration into theory and practice in clinical psychology. Br J Clin Psychol 37:341-353, 1998 [DOI] [PubMed] [Google Scholar]
- 43.Jackson VA, Jacobsen J, Greer JA, et al. : The cultivation of prognostic awareness through the provision of early palliative care in the ambulatory setting: a communication guide. J Palliat Med 16:894-900, 2013 [DOI] [PubMed] [Google Scholar]
- 44.Back AL, Arnold RM: Discussing prognosis: “How much do you want to know?” talking to patients who are prepared for explicit information. J Clin Oncol 24:4209-4213, 2006 [DOI] [PubMed] [Google Scholar]