Abstract
BACKGROUND
Routine preoperative testing is not recommended for patients undergoing cataract surgery, because testing neither decreases adverse events nor improves outcomes. We sought to assess adherence to this guideline, estimate expenditures from potentially unnecessary testing, and identify patient and health care system characteristics associated with potentially unnecessary testing.
METHODS
Using an observational cohort of Medicare beneficiaries undergoing cataract surgery in 2011, we determined the prevalence and cost of preoperative testing in the month before surgery. We compared the prevalence of preoperative testing and office visits with the mean percentage of beneficiaries who underwent tests and had office visits during the preceding 11 months. Using multivariate hierarchical analyses, we examined the relationship between preoperative testing and characteristics of patients, health system characteristics, surgical setting, care team, and occurrence of a preoperative office visit.
RESULTS
Of 440,857 patients, 53% had at least one preoperative test in the month before surgery. Expenditures on testing during that month were $4.8 million higher and expenditures on office visits $12.4 million higher (42% and 78% higher, respectively) than the mean monthly expenditures during the preceding 11 months. Testing varied widely among ophthalmologists; 36% of ophthalmologists ordered preoperative tests for more than 75% of their patients. A patient’s probability of undergoing testing was associated mainly with the ophthalmologist who managed the preoperative evaluation.
CONCLUSIONS
Preoperative testing before cataract surgery occurred frequently and was more strongly associated with provider practice patterns than with patient characteristics. (Funded by the Foundation for Anesthesia Education and Research and the Grove Foundation.)
Cataract surgery is the most common elective surgery among Medicare beneficiaries, with 1.7 million procedures performed annually.1 It is also very safe, with less than a 1% risk of major adverse cardiac events or death.2 The mean duration of cataract surgery is 18 minutes,3 and virtually all surgical procedures are performed in an ambulatory setting with topical anesthesia.4 However, because patients are typically elderly with multiple coexisting conditions,5,6 physicians frequently order routine preoperative tests because of concerns about patient safety, worries about medicolegal risks, and the perception that other physicians expect preoperative testing.6,7
Despite these common justifications, previous studies have shown that routine preoperative medical testing neither decreases the incidence of adverse events nor improves the outcomes of cataract surgery.5,8–10 Therefore, since 2002, guidelines from multiple specialty societies have deemed routine preoperative testing unnecessary.2,11–15 When there is concern about a patient’s ability to undergo this low-risk surgery, these guidelines recommend a preoperative office visit and examination, with testing as indicated on the basis of the patient’s medical history and physical findings.2,11–15
Historically, preoperative testing was common: a 1993 study, performed before the current guidelines were issued, showed that about half of Medicare beneficiaries had at least one test or office visit within 30 days before cataract surgery.16 In addition, a more recent study showed that the prevalence of preoperative consultations for patients undergoing cataract surgery has been increasing since 199617; however, this research did not address whether preoperative testing has declined with the rising prevalence of preoperative office visits or whether preoperative testing varies among physicians. To assess more recent provider adherence to the guidelines, we analyzed Medicare claims for cataract surgery in 2011 to determine the prevalence of pre-operative testing, the associated costs, the predictors of testing, and the extent of provider-level variation in ordering tests.
METHODS
STUDY OVERSIGHT AND DATA SOURCE
This study was approved by the institutional review board at the University of California, San Francisco. We obtained research identifiable files from the Centers for Medicare and Medicaid Services (CMS) Research Data Distribution Center for Medicare beneficiaries who underwent cataract surgery in 2011. For each beneficiary, we obtained the outpatient file, the carrier file, the Medicare Provider Analysis and Review file, and the Master Beneficiary Summary file representing all claims from January 1, 2010, through December 31, 2011.
STUDY COHORT
Using the outpatient and carrier files, we identified patients undergoing cataract surgery in 2011 on the basis of the Current Procedural Terminology (CPT) codes for cataract surgery (66982, 66983, 66984, 66850, 66920, 66930, and 66940).1 We included patients 66 years of age or older with at least 12 months of Medicare eligibility before surgery who were enrolled in the Medicare fee-for-service program without a concurrent health maintenance organization plan. From a total of 1,004,972 eligible persons, we obtained a random sample of 500,000 beneficiaries. We defined each beneficiary’s index surgery date as the first date of an ophthalmology claim for routine cataract surgery (CPT codes 66982–66984). We did not include beneficiaries who had an International Classification of Diseases, Ninth Revision, code indicating previous cataract surgery (V43.1, V45.61, or 379.31), who had had a cataract surgery claim in 2010, who had had an inpatient hospital stay within 30 days before the index surgery (to avoid misclassification of follow-up testing associated with the inpatient admission as preoperative testing), or who could not be linked to a hospital referral region.
PREDICTOR VARIABLES
The patient characteristics that we examined included age, sex, race, and health status; health status was assessed with the use of the Quan modification of the Charlson comorbidity index (scores on the Charlson comorbidity index range from 0 to 33, with higher scores indicating greater disease burden and increased risk of death within 1 year).18 Health system characteristics were derived with the use of the ophthalmologist’s ZIP Code, hospital referral region,19 and the Rural–Urban Commuting Area Codes.20
IDENTIFICATION OF PREOPERATIVE TESTS
We designated the following tests as possible preoperative tests: complete blood count, chemical analysis, coagulation studies, urinalysis, electrocardiography, echocardiography, cardiac stress tests, chest radiography, and pulmonary-function tests; we also included individual components of standard laboratory panels (listed in Table S1 in the Supplementary Appendix, available with the full text of this article at NEJM.org). Like Steinberg et al.,16 we categorized these tests as routine preoperative tests if they occurred during the preoperative month (i.e., within 30 days before — but not including the day of — the index surgery).
IDENTIFICATION OF PREOPERATIVE OFFICE VISITS
We defined a preoperative office visit as any new or established visit (CPT codes 99201–99205 or 99211–99215) to any general practice, anesthesiology, cardiology, family practice, internal medicine, or geriatric medicine physician, nurse practitioner, or physician assistant within 30 days before the index surgery. Office visits to ophthalmologists or optometrists were excluded.
IDENTIFICATION OF THE TEST-ORDERING PROVIDER AND THE LOCATION OF SURGERY
To assess preoperative testing according to provider, we used the operating ophthalmologist as a proxy for the group of physicians (e.g., the ophthalmologist, primary care physician, and anesthesiologist) who made up the patient’s perioperative care team, because we could not use Medicare claims data to reliably determine the specific physician ordering the test. We refer to the group of physicians who might have ordered a patient’s tests as the “care team,” but we use the term “ophthalmologist” when appropriate for clarity. We ascertained a surgical location for 98.5% of the beneficiaries by identifying an ambulatory surgery center or hospital outpatient department claim in the carrier or outpatient file submitted within 1 day before or after the ophthalmologist-submitted claim.
COSTS
Costs were calculated on the basis of the national limitation amount from the 2011 Clinical Laboratory Fee Schedule21 for laboratory tests. For nonlaboratory tests and office visits, the non-facility price from the 2011 Medicare Physician Fee Schedule was used.22
STATISTICAL ANALYSIS
All statistical analyses were performed with the use of SAS software, version 9.4 (SAS Institute). We calculated the proportion of beneficiaries with preoperative testing or office visits and the associated cost to Medicare. Patient and health system characteristics, including surgical setting, were assessed for patients who did and patients who did not undergo preoperative testing or office visits; chi-square tests were used to assess differences in categorical variables, and Student’s t-tests were used for continuous variables. We calculated the mean number of tests and office visits per beneficiary per month to evaluate changes over time.
For the analysis of variation among ophthalmologists, we identified the percentage of each ophthalmologist’s patients who had preoperative testing or office visits and graphed this result for ophthalmologists who performed five or more surgeries in 2011. Within groups of ophthalmologists stratified according to the rate of preoperative testing, we calculated excess testing in the preoperative month by subtracting the mean number of tests per month during the 11-month baseline period.
To estimate independent predictors of pre-operative testing or office visits, using only beneficiaries with a known surgical location, we created a two-level hierarchical model with the ophthalmologist as a random effect to account for clustering of patients according to ophthalmologist. We included demographic characteristics of the patients, health status, geographic region, surgical setting, and other health system variables as fixed effects. The influence of the ophthalmologist was summarized with the median odds ratio, which is the median ratio of the odds of preoperative testing or office visits between demographically identical patients of equal health status who are the patients of two randomly selected ophthalmologists, with the clusters compared in descending order so that the odds ratios are always 1 or more.23,24 This summary statistic is a function of the estimated variance of the random effect and is directly comparable to odds ratios of fixed-effects variables. To assess the differential contributions to variation in testing attributable to the ophthalmologist, the characteristics of the patient, and the occurrence of an office visit in the preoperative month, we created multiple models of pre-operative testing and calculated C-statistics for each model.
RESULTS
CHARACTERISTICS OF THE STUDY COHORT
Of 440,857 beneficiaries, 232,889 (53%) underwent at least one preoperative test, and 229,832 (52%) had a preoperative office visit. The characteristics of patients who underwent preoperative tests (Table 1, and Table S2 in the Supplementary Appendix) were similar to the characteristics of the patients who had preoperative office visits (Table S3 in the Supplementary Appendix).
Table 1.
Characteristics of the Patients.*
| Characteristic | Preoperative Testing (N = 232,889) | No Preoperative Testing (N = 207,968) |
|---|---|---|
| Age (yr) | 76.5±6.3 | 75.7±6.2 |
| Sex (%) | ||
| Male | 40 | 40 |
| Female | 60 | 60 |
| Race (%)† | ||
| White | 87 | 90 |
| Black | 7 | 6 |
| Other | 6 | 5 |
| Charlson comorbidity index score (%)‡ | ||
| 0–1 | 54 | 69 |
| 2 | 17 | 14 |
| ≥3 | 29 | 17 |
| Health system characteristics (%)§ | ||
| U.S. region | ||
| Northeast | 23 | 10 |
| Midwest | 23 | 25 |
| South | 37 | 46 |
| Mountain west | 4 | 8 |
| Pacific west | 13 | 10 |
| Population density | ||
| Urban | 84 | 81 |
| Rural | 16 | 19 |
| Surgical setting (%) | ||
| Ambulatory surgery center | 64 | 71 |
| Hospital outpatient department | 34 | 28 |
| Unknown | 2 | 1 |
| Preoperative office visit (%) | ||
| Yes | 73 | 28 |
| No | 27 | 72 |
Plus–minus values are means ±SD.
Data on race were obtained from the Master Beneficiary Summary file.
Scores on the Charlson comorbidity index range from 0 to 33, with higher scores indicating greater disease burden and increased risk of death within 1 year.
Additional health system variables included primary care physicians per 100,000 residents, ophthalmologists per 100,000 residents, ophthalmologist annual cataract surgical volume, and Medicare expenditures per beneficiary in the hospital referral region; data on these variables are provided in the Supplementary Appendix.
PREVALENCE AND COST OF PREOPERATIVE TESTING AND OFFICE VISITS
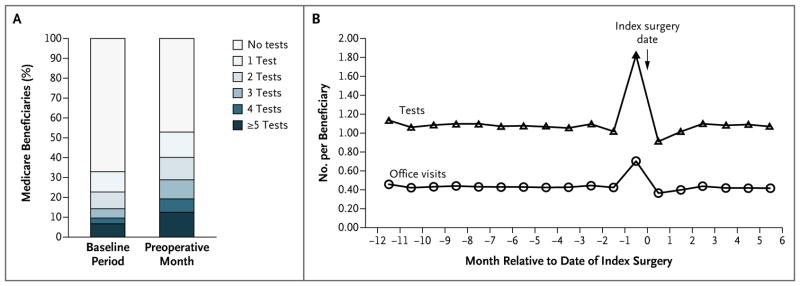
The mean number of tests per beneficiary increased by 66% during the preoperative month, relative to the baseline period, and the mean number of office visits increased by 63%. During the preoperative month, 13% of beneficiaries underwent one test, 11% underwent two, 10% underwent three, 7% underwent four, and 13% underwent five or more. All the percentages were higher than the mean of the monthly percentages during the baseline period (Fig. 1A). Among the 222,741 beneficiaries with 6 months of postoperative follow-up, we found a similar increase in testing and office visits per beneficiary before surgery, followed by a return to baseline levels after surgery (Fig. 1B).
Figure 1. Preoperative Testing during the Preoperative Month as Compared with Baseline.
Panel A shows the percentage of Medicare beneficiaries who underwent testing, stratified according to the number of tests performed. Among all beneficiaries, 13% had one test, 11% had two tests, 10% had three tests, 7% had four tests, and 13% had five or more tests during the preoperative month; the corresponding mean percentages of beneficiaries who had these numbers of tests during the baseline period were 10%, 8%, 5%, 3%, and 7%. The proportion of beneficiaries who did not undergo any testing decreased from 67% during the baseline period to 47% during the preoperative month. We calculated the baseline percentages by averaging the percentage of beneficiaries undergoing the specified number of tests each month over the 11-month baseline period. Panel B shows the mean number of tests and office visits per beneficiary per month. Patients underwent a mean of 1.09 tests per beneficiary per month during the 11-month baseline period, as compared with 1.81 tests per beneficiary in the preoperative month — a 66% increase. Office visits increased by 63%, from 0.43 visits per beneficiary per month during the baseline period to 0.70 visits per beneficiary in the preoperative month. The total number of beneficiaries in the denominator includes all patients in the cohort. The number of tests includes only tests commonly requested for a preoperative evaluation (complete blood count, chemical analysis, coagulation studies, urinalysis, electrocardiography, echocardiography, cardiac stress tests, chest radiography, and pulmonary-function tests). The number of office visits includes only office visits to providers commonly asked to give preoperative clearance (general practice, anesthesiology, cardiology, family practice, internal medicine, and geriatric medicine physicians, nurse practitioners, and physician assistants). Office visits to ophthalmologists or optometrists were not included. Panel B was created with data from the subgroup of beneficiaries with 6 months of follow-up after the index surgery (222,741 patients), to show that testing levels returned to baseline after the index surgery. The percentage of testing and office visits during the baseline period and preoperative month in this subcohort were virtually identical to the results in the full cohort.
A total of 798,150 tests were performed during the preoperative month, at a cost of approximately $16.1 million. Another $28.3 million was spent on 308,397 office visits. Expenditures on testing in the month before surgery were $4.8 million higher and expenditures on office visits $12.4 million higher (42% and 78% higher, respectively) than the mean monthly expenditures during the preceding 11 months (Table S4 in the Supplementary Appendix).
VARIATION AMONG PROVIDERS
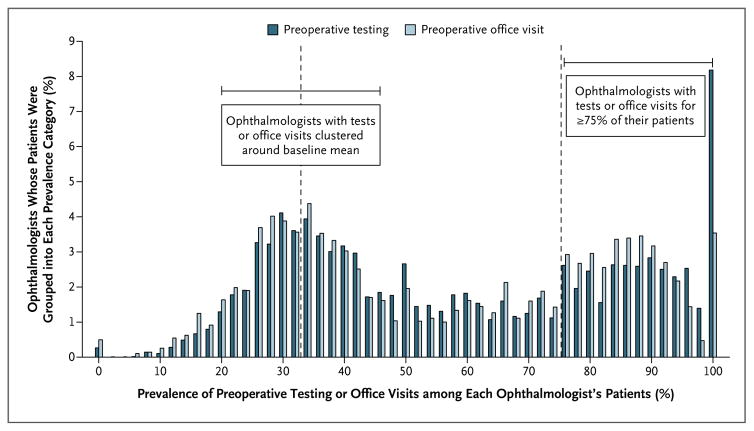
There was substantial variation among ophthalmologists in the use of preoperative testing and office visits (Fig. 2). Of the 9253 ophthalmologists who operated on five or more patients in 2011, more than one third (36%) ordered preoperative testing for 75% or more of their patients, and 8% ordered testing for every patient. This 36% of ophthalmologists collectively treated only 26% of patients, but their patients accounted for 84% of all testing above the baseline mean. The variation in preoperative office visits was similar in magnitude and paralleled that of testing across providers.
Figure 2. Variation among Ophthalmologists in the Prevalence of Preoperative Testing and Office Visits.
Using data on ophthalmologists who performed five or more surgeries in 2011, we graphed the percentage of each ophthalmologist’s patients who underwent testing during the 30 days before index cataract surgery. Of the 9253 ophthalmologists who operated on five or more patients in 2011, more than one third (36%) had 75% or more of their patients undergo preoperative testing, and 8% ordered at least one preoperative test for every patient. The 36% of ophthalmologists who ordered testing for 75% or more of their patients treated only 26% of the total number of patients, but their patients accounted for 84% of all testing above the baseline level of testing. The variation in preoperative office visits was similar in magnitude to the variation in testing, and the use of office visits paralleled that of testing across providers. During the baseline period, the mean monthly prevalence of testing and office visits was 33% and 32%, respectively.
PREDICTIVE MODELS
The ophthalmologist performing the surgery was the strongest predictor of testing, with a median odds ratio of 2.94 (i.e., the odds of testing between two typical ophthalmologists varied by a factor of almost three). As compared with patients undergoing surgery in ambulatory surgery centers, patients undergoing surgery in hospital outpatient departments had higher odds of testing (odds ratio, 1.30) (Table 2) but lower odds of office visits (odds ratio, 0.86) (Table S6 in the Supplementary Appendix).
Table 2.
Characteristics Associated with Preoperative Testing before Cataract Surgery.*
| Characteristic | Baseline Patient Characteristics Only | Ophthalmologist Only | Ophthalmologist plus All Other Variables |
|---|---|---|---|
| Adjusted Odds Ratio (95% CI) | |||
| Age† | 1.19 (1.18–1.20) | — | 1.09 (1.08–1.10) |
|
| |||
| Sex | |||
|
| |||
| Male | Reference | — | Reference |
|
| |||
| Female | 1.04 (1.03–1.05) | — | 1.00 (0.98–1.01) |
|
| |||
| Race | |||
|
| |||
| White | Reference | — | Reference |
|
| |||
| Black | 1.04 (1.01–1.06) | — | 0.97 (0.94–1.00) |
|
| |||
| Other | 1.31 (1.28–1.35) | — | 0.94 (0.91–0.98) |
|
| |||
| Charlson comorbidity index score | |||
|
| |||
| 0–1 | Reference | — | Reference |
|
| |||
| 2 | 1.51 (1.49–1.54) | — | 1.56 (1.53–1.59) |
|
| |||
| ≥3 | 2.20 (2.16–2.23) | — | 2.35 (2.31–2.39) |
|
| |||
| U.S. region | |||
|
| |||
| Pacific west | — | — | Reference |
|
| |||
| Northeast | — | — | 1.74 (1.58–1.90) |
|
| |||
| Midwest | — | — | 0.82 (0.75–0.89) |
|
| |||
| South | — | — | 0.77 (0.71–0.83) |
|
| |||
| Mountain west | — | — | 0.54 (0.48–0.60) |
|
| |||
| Population density | |||
|
| |||
| Urban | — | — | Reference |
|
| |||
| Rural | — | — | 0.86 (0.82–0.90) |
|
| |||
| Primary care physicians per 100,000 residents†‡ | — | — | 1.06 (1.03–1.09) |
|
| |||
| Ophthalmologists per 100,000 residents‡ | — | — | 1.22 (1.19–1.25) |
|
| |||
| Ophthalmologist annual cataract surgical volume† | — | — | 0.97 (0.97–0.98) |
|
| |||
| Medicare expenditures per beneficiary in hospital referral region in 2010 U.S. dollars | |||
|
| |||
| Quartile 1: $6,911–$8,689 | — | — | Reference |
|
| |||
| Quartile 2: $8,691–$9,674 | — | — | 1.06 (0.99–1.14) |
|
| |||
| Quartile 3: $9,693–$10,311 | — | — | 1.03 (0.96–1.11) |
|
| |||
| Quartile 4: $10,341–$13,824 | — | — | 1.23 (1.14–1.33) |
|
| |||
| Surgical setting | |||
|
| |||
| Ambulatory surgery center | — | — | Reference |
|
| |||
| Hospital outpatient department | — | — | 1.30 (1.26–1.34) |
|
| |||
| Ophthalmologist§ | — | 3.40 (3.33–3.47) | 2.94 (2.88–2.99) |
The C-statistic for the area under the receiver-operating-characteristic curve was 0.60 for the model that included baseline patient characteristics only, 0.78 for the ophthalmologist-only model, and 0.80 for the model that included the ophthalmologist plus all other variables. The addition of a variable for the presence or absence of an office visit to the ophthalmologist-only model and the model with all variables resulted in C-statistics of 0.84 and 0.85, respectively. A graphical depiction of these results is provided in the Supplementary Appendix.
Age, primary care physicians per 100,000 residents, and surgical volume were divided by 10 to produce more meaningful odds ratios.
The hospital referral region variables were current as of 2006.
The influence of the ophthalmologist was summarized by the median odds ratio, which is the median ratio of the odds of preoperative testing between demographically identical patients of equal health status who are the patients of two randomly selected ophthalmologists (calculated with the use of the total sample of 10,507 ophthalmologists).
In our models of preoperative testing, discrimination (as measured by the C-statistic), which captures how well the variables included in each model distinguish between patients who undergo preoperative testing and those who do not, ranged from 0.60 to 0.85 (Fig. S1 in the Supplementary Appendix). The model that included only patient baseline characteristics had a C-statistic of 0.60. A model with the ophthalmologist as the only variable had a C-statistic of 0.78. The addition of all other variables from Table 1 (with the exception of preoperative office visit) to the ophthalmologist-only model increased the C-statistic by just 0.02 over the ophthalmologist-only model (Table 2). The addition of a variable for the presence or absence of an office visit to the ophthalmologist-only model and the model that included all variables resulted in C-statistics of 0.84 and 0.85, respectively (Table S5 in the Supplementary Appendix). Similarly, the discrimination of models predicting preoperative office visits improved the most with inclusion of the ophthalmologist variable alone (Table S6 in the Supplementary Appendix). Additional hierarchical models with clustering according to surgical institution showed similar results but slightly less discrimination, as compared with the models with clustering according to ophthalmologist, a finding that reflects the tight linkage between ophthalmologists and institutions; more than 60% of institutions had claims from only one or two ophthalmologists (data not shown).
DISCUSSION
In this national assessment of variation in routine preoperative testing before cataract surgery, we found that more than half of Medicare beneficiaries undergoing cataract surgery underwent at least one preoperative test, despite strong evidence about the lack of benefit of preoperative testing.5,10 This represents a substantial increase in testing over levels during the baseline period and is most likely an unnecessary Medicare expense. Furthermore, our results showed no difference in the prevalence of testing as compared with 20 years ago,16 before the introduction of guidelines stating that routine preoperative testing for cataract surgery was not necessary. These data underscore the fact that publishing evidence-based guidelines alone does not necessarily change individual physician behavior.25,26 This is an important problem, considering that the number of annual cataract surgeries is projected to increase to 4.4 million by 2030, with Medicare paying for more than 80% of cataract surgical procedures in the United States.1
Our predictive models showed that a patient’s health status is associated with testing. However, the ophthalmologist performing the surgery and the occurrence of a preoperative office visit appeared to be more powerful drivers of testing than were the characteristics of the patient. Our results suggest that preoperative testing among patients undergoing cataract surgery is more attributable to the practice patterns of individual physicians than to differences among physicians in the complexity of their patient populations or to physicians ordering tests differentially — on the basis of a patient’s health status — for specific patients within their own practices. In fact, more than one third of ophthalmologists had testing performed in the vast majority (>75%) of their patients, with 8% of ophthalmologists having all their patients undergoing testing. These high testing percentages should not be attributed solely to the ophthalmologist, because the tests could have been requested or ordered by any member of the care team. We cannot determine from our data, however, which physician’s usual practice pattern is driving the use of testing within each care team.
Similarly, we found that more than half the patients in our study had a preoperative office visit and that the operating ophthalmologist was the strongest predictor of having an office visit. Office visits were unexpectedly less likely among patients undergoing surgery in hospital outpatient departments than among patients undergoing surgery at ambulatory surgery centers, although the hospital-based patients had a higher likelihood of undergoing testing. Many hospitals have preoperative clinics run by the hospital anesthesiology department; these clinics generally do not submit claims for the preoperative evaluation separately from the anesthesiologist’s global claim for the anesthesia encounter on the day of surgery. The existence of these clinics and the corresponding absence of these particular office visits from our data set may explain this observation.
It is possible that the continued use of routine preoperative testing is due to physicians responding to external influences. For example, CMS and the Joint Commission both require that a medical history and physical be completed within 30 days before surgery. Although this requirement may explain the high prevalence of preoperative office visits to nonophthalmologist providers, it does not necessarily explain the persistence of routine testing, because neither organization mandates testing.27–30 Moreover, we observed wide variations in the use of both testing and office visits among physicians, which suggests that regulatory requirements are not the primary influence on physician behavior.
It is not known whether preoperative office visits improve outcomes. Additional research could better clarify the value of a medical history and physical examination performed by a provider other than the ophthalmologist before cataract surgery.17,31 If these office visits and the resulting testing do not change outcomes, then efforts to reduce testing could also address ways to reduce office visits.
This study has several limitations. First, the use of a 30-day preoperative window to measure the prevalence and cost of preoperative testing may inadvertently include unrelated tests that were performed during that period. However, the net increase in testing and cost that occurred during the preoperative month relative to the baseline period strongly suggests that most of the additional tests we classified as preoperative tests were being ordered in anticipation of surgery.
Second, we were unable to identify the actual physicians who were primarily responsible for the excess testing performed. Because previous studies have shown that there is variation among care teams with regard to who is requesting and ordering testing,6,7 interventions to reduce testing will need to address all members of the care team. This makes our findings relevant despite this limitation in the data.
Third, our cost estimates were based on payments made by Medicare only. These estimates may not reflect the full cost, because they do not include payments made by the beneficiary or other insurers, nor do they include downstream costs accruing because of follow-up of abnormal results from unnecessary tests. However, the analysis still meets the study objective of providing an estimate of the annual cost to Medicare of routine preoperative testing.
In conclusion, preoperative testing in patients undergoing cataract surgery still occurred frequently in 2011, despite clear guidelines recommending against it. The practice pattern of the physician care team is the primary determinant of whether preoperative testing is performed.
Supplementary Material
Acknowledgments
Supported by grants from the Foundation for Anesthesia Education and Research and the Grove Foundation.
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Schein OD, Cassard SD, Tielsch JM, Gower EW. Cataract surgery among Medicare beneficiaries. Ophthalmic Epidemiol. 2012;19:257–64. doi: 10.3109/09286586.2012.698692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fleisher LA, Beckman JA, Brown KA, et al. ACC/AHA 2007 Guidelines on peri-operative cardiovascular evaluation and care for noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 2002 guidelines on perioperative cardiovascular evaluation for noncardiac surgery) developed in collaboration with the American Society of Echocardiography, American Society of Nuclear Cardiology, Heart Rhythm Society, Society of Cardiovascular Anesthesiologists, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, and Society for Vascular Surgery. J Am Coll Cardiol. 2007;50:1707–32. doi: 10.1016/j.jacc.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 3.Cullen KA, Hall MJ, Golosinskiy A. Ambulatory surgery in the United States, 2006. Natl Health Stat Report. 2009;11:1–25. [PubMed] [Google Scholar]
- 4.Analeyz. Survey of American Society of Cataract Refractive Surgery members. 2011 ( http://www.analeyz.com/AnaleyzASCRS2011.htm)
- 5.Schein OD, Katz J, Bass EB, et al. The value of routine preoperative medical testing before cataract surgery: study of medical testing for cataract surgery. N Engl J Med. 2000;342:168–75. doi: 10.1056/NEJM200001203420304. [DOI] [PubMed] [Google Scholar]
- 6.Bass EB, Steinberg EP, Luthra R, et al. Do ophthalmologists, anesthesiologists, and internists agree about preoperative testing in healthy patients undergoing cataract surgery? Arch Ophthalmol. 1995;113:1248–56. doi: 10.1001/archopht.1995.01100100036025. [DOI] [PubMed] [Google Scholar]
- 7.Brown SR, Brown J. Why do physicians order unnecessary preoperative tests? A qualitative study. Fam Med. 2011;43:338–43. [PubMed] [Google Scholar]
- 8.Lira RP, Nascimento MA, Moreira-Filho DC, Kara-José N, Arieta CE. Are routine preoperative medical tests needed with cataract surgery? Rev Panam Salud Publica. 2001;10:13–7. doi: 10.1590/s1020-49892001000700003. [DOI] [PubMed] [Google Scholar]
- 9.Cavallini GM, Saccarola P, D’Amico R, Gasparin A, Campi L. Impact of preoperative testing on ophthalmologic and systemic outcomes in cataract surgery. Eur J Ophthalmol. 2004;14:369–74. [PubMed] [Google Scholar]
- 10.Keay L, Lindsley K, Tielsch J, Katz J, Schein O. Routine preoperative medical testing for cataract surgery. Cochrane Database Syst Rev. 2012;3:CD007293. doi: 10.1002/14651858.CD007293.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Apfelbaum JL, Connis RT, Nickinovich DG, et al. Practice advisory for preanesthesia evaluation: an updated report by the American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Anesthesiology. 2012;116:522–38. doi: 10.1097/ALN.0b013e31823c1067. [DOI] [PubMed] [Google Scholar]
- 12.American Academy of Ophthalmology. Routine preoperative laboratory testing for patients scheduled for cataract surgery — 2014. ( http://one.aao.org/clinical-statement/routine-preoperative-laboratory-testing-patients-s)
- 13.American Academy of Ophthalmology. Cataract in the adult eye, preferred practice pattern — 2011. doi: 10.1016/j.ophtha.2021.10.006. ( http://one.aao.org/preferred-practice-pattern/cataract-in-adult-eye-ppp--october-2011) [DOI] [PubMed]
- 14.NHS Institute for Innovation and Improvement. Focus on: cataracts. ( http://www.institute.nhs.uk/quality_and_value/high_volume_care/cataracts.html)
- 15.The Royal College of Ophthalmologists. Cataract surgery guidelines. 2010 Sep; ( https://www.rcophth.ac.uk/wp-content/uploads/2014/12/2010-SCI-069-Cataract-Surgery-Guidelines-2010-SEPTEMBER-2010.pdf)
- 16.Steinberg EP, Javitt JC, Sharkey PD, et al. The content and cost of cataract surgery. Arch Ophthalmol. 1993;111:1041–9. doi: 10.1001/archopht.1993.01090080037016. [DOI] [PubMed] [Google Scholar]
- 17.Thilen SR, Treggiari MM, Lange JM, Lowy E, Weaver EM, Wijeysundera DN. Preoperative consultations for medicare patients undergoing cataract surgery. JAMA Intern Med. 2014;174:380–8. doi: 10.1001/jamainternmed.2013.13426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 19.The Dartmouth Institute for Health Policy and Clinical Practice. The Dart-mouth atlas of health care. ( http://www.dartmouthatlas.org)
- 20.WWAMI Rural Health Research Center. Rural-Urban Commuting Area (RUCA) Codes, version 2.0. ( http://depts.washington.edu/uwruca/ruca-data.php)
- 21.Centers for Medicare and Medicaid Services. Medicare clinical laboratory fee schedule. 2011 ( http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ClinicalLabFeeSched/clinlab.html)
- 22.Centers for Medicare and Medicaid Services. Medicare physician fee schedule. 2011 ( http://www.cms.gov/apps/physician-fee-schedule/overview.aspx)
- 23.Larsen K, Merlo J. Appropriate assessment of neighborhood effects on individual health: integrating random and fixed effects in multilevel logistic regression. Am J Epidemiol. 2005;161:81–8. doi: 10.1093/aje/kwi017. [DOI] [PubMed] [Google Scholar]
- 24.Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60:290–7. doi: 10.1136/jech.2004.029454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cabana MD, Rand CS, Powe NR, et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–65. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 26.Timmermans S, Mauck A. The promises and pitfalls of evidence-based medicine. Health Aff (Millwood) 2005;24:18–28. doi: 10.1377/hlthaff.24.1.18. [DOI] [PubMed] [Google Scholar]
- 27.The Joint Commission. Standards FAQ details: content of the history and physical. 2008 Nov 24; ( http://www.jointcommission.org/mobile/standards_information/jcfaqdetails.aspx?StandardsFAQId=35&StandardsFAQChapterId=12)
- 28.The Joint Commission. Standards FAQ details: history and physical for hospital outpatient procedures. 2008 Nov 24; ( http://www.jointcommission.org/standards_information/jcfaqdetails.aspx?StandardsFAQId=93&StandardsFAQChapterId=74)
- 29.Blue Ridge Health. Joint Commission topic: H&P exams for hospital patients. ( http://www.blueridgehealth.org/Story-Joint-Commission4.pdf)
- 30.Centers for Medicare and Medicaid Services. Clarifications to the ambulatory surgical center (ASC) interpretive guidelines — comprehensive medical history and physical (H&P) assessment. ( http://www.cms.gov/Medicare/Provider-Enrollment-and-Certification/SurveyCertificationGenInfo/downloads/SCLetter11_06.pdf)
- 31.Fleisher LA. Preoperative consultation before cataract surgery: are we choosing wisely or is this simply low-value care? JAMA Intern Med. 2014;174:389–90. doi: 10.1001/jamainternmed.2013.12298. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.