Abstract
Background
Hyperkalemia (serum potassium >5.0 mEq/L) may be caused by reduced kidney function and drugs affecting the renin-angiotensin-aldosterone system and is often present in patients with chronic kidney disease (CKD).
Objective
To quantify the burden of hyperkalemia in US Medicare fee-for-service and commercially insured populations using real-world claims data, focusing on prevalence, comorbidities, mortality, medical utilization, and cost.
Methods
A descriptive, retrospective claims data analysis was performed on patients with hyperkalemia using the 2014 Medicare 5% sample and the 2014 Truven Health Analytics MarketScan Commercial Claims and Encounter databases. The starting study samples required patient insurance eligibility during ≥1 months in 2014. The identification of hyperkalemia and other comorbidities required having ≥1 qualifying claims in 2014 with an appropriate International Classification of Diseases, Ninth Revision, Clinical Modification diagnosis code in any position. To address the differences between patients with and without hyperkalemia, CKD subsamples were analyzed separately. Mortality rates were calculated in the Medicare sample population only. The claims were grouped into major service categories; the allowed costs reflected all costs incurred by each cohort divided by the total number of member months for that cohort.
Results
The prevalence of hyperkalemia in the Medicare and commercially insured samples was 2.3% and 0.09%, respectively. Hyperkalemia was associated with multiple comorbidities, most notably CKD. The prevalence of CKD in the Medicare and the commercially insured members with hyperkalemia was 64.8% and 31.8%, respectively. After adjusting for CKD severity, the annual mortality rate for Medicare patients with CKD and hyperkalemia was 24.9% versus 10.4% in patients with CKD without hyperkalemia. The allowed costs in patients with CKD and hyperkalemia in the Medicare and commercially insured cohorts were more than twice those in patients with CKD without hyperkalemia. Inpatient care accounted for >50% of costs in patients with CKD and hyperkalemia.
Conclusion
Hyperkalemia is associated with substantial clinical and economic burden among US commercially insured and Medicare populations.
Keywords: chronic kidney disease, commercially insured, comorbidities, cost, fee for service, hyperkalemia, Medicare, mortality, prevalence, utilization
Potassium is a cation in the human body that helps to facilitate important physiologic functions, including cellular metabolism, glycogen and protein synthesis, and the maintenance of electrical action potentials across cell membranes.1 More than 98% of the potassium in the body is located inside of cells, mostly in muscle cells. In healthy individuals, serum potassium concentration is maintained at normal levels (3.5–5.0 mEq/L), regardless of dietary potassium intake. Normal serum potassium levels are maintained through a balance of potassium intake and excretion, as well as a balance between intracellular and extracellular potassium levels. Approximately 90% of the daily intake of potassium is excreted in the urine; the remainder is excreted in stool.
Hyperkalemia, which is defined as an elevated serum potassium level (ie, >5.0 mEq/L), may be caused by a reduction in the renal excretion of potassium or an intracellular-to-extracellular shift in potassium that results from various acute clinical conditions. Although the kidney can adjust to a reduced number of nephrons and maintain normokalemia under steady-state conditions, it lacks the ability to respond to acute increases in potassium load and to adequately excrete potassium in patients with chronic kidney disease (CKD); the result in both cases is hyperkalemia.2 In addition, the use of drugs that inhibit the renin-angiotensin-aldosterone system (RAAS) in patients with CKD and other chronic conditions further increases serum potassium levels and exacerbates the risk for hyperkalemia.3–5 At present, RAAS inhibitors are recommended by clinical guidelines for several conditions, including heart failure,5 CKD with proteinuria,6 and diabetes with nephropathy.7 Thus, these agents are widely used in circumstances that predispose patients to hyperkalemia.
The current treatment options for patients with chronic hyperkalemia or for those at risk for chronic hyperkalemia are very limited, and no specific guidelines are available in the United States related to the treatment of hyperkalemia. In fact, for the duration of our study, sodium polystyrene sulfonate (SPS) was the only existing specific treatment option for patients with chronic hyperkalemia. The most applicable current guideline, the 2012 Kidney Disease: Improving Global Outcomes, recommends the use of appropriate medication and diet for the prevention and treatment of hyperkalemia.8
Improving the treatment of hyperkalemia requires a better understanding of its clinical and economic burden, but the epidemiologic, utilization, and cost parameters have not been analyzed in large populations. The broad point is well-established in the medical literature, that the tendency toward hyperkalemia is persistent under certain disease states and/or with the use of certain medications.2–5,8–14 However, hyperkalemia itself may be episodic.2,3,10,15,16
Furthermore, identifying hyperkalemia using administrative data has shortcomings; in particular, the condition may not be appropriately or accurately documented or coded.4,17 Prevalence rates have been shown to vary with the definition of hyperkalemia that is used, the population being studied, the design of the study, and the data source.2,4,11,17,18 As a result of the challenges associated with identifying hyperkalemia, its prevalence has not been clearly established and may be underreported.
Studies have shown that hyperkalemia is associated with an increased risk for mortality and an increased use of hospital resources. A recent study showed that hyperkalemia was associated with a higher hospitalization rate and increased mortality in patients with CKD who were not undergoing dialysis.11 Another study showed that, in patients with cardiovascular disease (CVD) who were taking antihypertensive drugs, hyperkalemia was associated with increased all-cause mortality and an increased hospitalization rate.13
In a retrospective, observational study, patients who had hyperkalemia at the onset of critical care had an increase in all-cause mortality at 30 days.19 In another observational study of patients with severe hyperkalemia (potassium level ≥6.5 mEq/L), 68.6% of patients required emergency hospitalization, and the inpatient mortality rate was 30.7%.20
KEY POINTS
-
▸
Few treatment options and no specific guidelines are available for the treatment of hyperkalemia in patients with chronic conditions.
-
▸
This retrospective, claims-based analysis is the first study about the cost implications of hyperkalemia in patients with CKD who have Medicare or commercial insurance.
-
▸
The mortality rate was more than double in Medicare patients with CKD and hyperkalemia than in patients with CKD but without hyperkalemia (24.9% vs 10.4%).
-
▸
Hospitalization rate was much higher in patients with CKD and hyperkalemia than in those without hyperkalemia among Medicare patients as well as those with commercial insurance.
-
▸
The PPPM treatment costs were 5-fold higher in Medicare patients with CKD and hyperkalemia ($5645) than in the total Medicare population ($1035).
-
▸
In commercially insured patients, the PPPM costs were 15 times higher in patients with CKD and hyperkalemia than in the total population.
-
▸
Hyperkalemia places substantial clinical and economic burdens on patients with CKD.
In patients with acute myocardial infarction, those who had hyperkalemia had higher mortality during a follow-up period that averaged 3.58 years compared with patients with normokalemia.21 However, data on cost, including spending by service type, are lacking in the medical literature. Nonetheless, identifying the distribution of hyperkalemia burden has important implications for healthcare providers, payers, and patients.
Our study utilized real-world claims data to quantify the burden of hyperkalemia among US commercially insured members and fee-for-service (FFS) Medicare beneficiaries, focusing on prevalence, comorbidities, mortality, medical utilization, and cost.
Methods
We performed a descriptive, retrospective claims data analysis of patients with hyperkalemia using the 2014 Medicare 5% sample and the 2014 Truven Health Analytics MarketScan Commercial Claims and Encounter databases (hereafter MarketScan). The Medicare sample, which contains Medicare enrollment data and all FFS Medicare Part A and Part B paid claims, provides a statistically balanced sample of Medicare FFS beneficiaries. The 2014 MarketScan database contains enrollment data and all paid claims for approximately 47 million commercially insured lives covered by the benefit plans of large employers, health plans, and government and public organizations nationwide.
The claims in both data sets include various codes (diagnosis, procedure, revenue, and diagnosis-related group codes) and site-of-service information. The enrollment data in both data sets include beneficiary age and monthly eligibility status; the Medicare enrollment data also include the monthly status of HMO enrollment, eligibility type (aged nondual, aged dual, disabled, and end-stage renal disease), and date of death. Prescription drug claims are available in the MarketScan database but not in the Medicare sample.
Study Samples
The study samples consisted of all patients with ≥1 months of eligibility in 2014 from the Medicare 5% (Medicare) sample and the MarketScan (commercially insured) sample. The patients in the Medicare sample were required to have Medicare Part A and Part B eligibility enrollment and could not be enrolled in an HMO plan during any of the months of eligibility. The patients in the commercially insured sample were required to have pharmacy coverage, and contributors with capitated and high-deductible health plans were excluded.
Because patients with hyperkalemia may have higher rates of CKD and patients with CKD may have higher costs and mortality, additional analyses of only the patients with CKD were conducted by CKD stage. This allowed for analysis of the incremental costs of hyperkalemia after risk adjustment for CKD stage, thereby reducing the risk for potential bias in comparisons of healthcare resource utilization, costs, and mortality between patients with and without hyperkalemia.
Identification of Diseases and Mortality
Patients with hyperkalemia were identified as those with ≥1 qualifying claims in 2014 that were coded in any position with an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis code of 276.7 (ie, hyperkalemia could be the primary or secondary diagnosis). Qualifying claims included facility and professional claims representing in-person encounters with a medical professional. In the analysis of the commercially insured population, patients with ≥1 prescription drug claims with a National Drug Code for SPS were considered to have hyperkalemia (see Appendix at www.AHDBonline.com for a list of National Drug Codes for SPS and for the percentage of patients with hyperkalemia who were identified through each qualifying claim type).
Comorbidities were defined by having ≥1 qualifying claims coded in any position with ICD-9-CM diagnosis codes for hypertension (401.0–402.91, 404.0–405.99), chronic obstructive pulmonary disease (491.0–492.8, 493.20–493.22, 496), heart failure (398.91, 402.01, 402.11, 402.91, 404.xx, 428.xx), end-stage renal disease (585.6), stage I CKD (585.1), stage II CKD (585.2), stage III CKD (585.3), stage IV CKD (585.4), stage V CKD (585.5), and unspecified CKD (585.9).
Diabetes was identified using the standard criteria that were set forth in the Healthcare Effectiveness Data and Information Set (HEDIS), a standard measurement set used most notably as part of accreditation and reporting packages for health plans and other entities. The HEDIS criteria required ≥1 acute inpatient claims or 1 emergency department claim or 2 other qualifying claims coded with diabetes (ICD-9-CM code 250.xx) in the Medicare sample and ≥1 diabetes prescription drug claims in the commercially insured sample.
The mortality rate in the Medicare sample was identified using the eligibility file, which includes the date of death. The cause of death is not available from Medicare claims or eligibility data. The MarketScan database does not include the date of death, so we were unable to ascertain the mortality rate for hyperkalemia in the commercially insured sample.
Identification of Procedures, Drugs, and Costs
The claims were grouped into major service categories for the total samples, as well as for the group of patients with hyperkalemia using the Milliman Health Cost Guidelines grouper, which is based on various codes (Healthcare Common Procedure Coding System, Current Procedural Terminology, ICD-9-CM diagnosis and procedure, revenue, site of service, and diagnosis-related group codes).
The major service categories included inpatient, emergency department, skilled nursing facility, physician office visits, outpatient, other professional (ie, services not included in the inpatient, skilled nursing facility, or physician office visit categories and costs for durable medical equipment, ambulance, and prosthetics), other services (ie, home health and hospice), and prescription drugs.
The MarketScan database includes prescription drug costs, whereas the Medicare sample does not include Medicare Part D prescription drug costs. The allowed costs included payment to providers plus patient cost-sharing. The per-member per-month or per-patient per-month (PPPM) costs reflected all costs for the respective sample divided by the total number of member months for that sample.
Statistical Methods
The analysis was performed using SAS software, version 9.3 (SAS Institute, Inc; Cary, NC). The numbers and proportions were calculated for healthcare utilization measures, such as the admission rate. The univariate descriptive statistics included the mean and median for continuous variables (eg, age, and per-member per-month costs, and PPPM costs) and the relative frequencies for categorical variables (eg, sex and diagnosis).
Analyses based on the CKD sample were conducted at each CKD stage. In addition, to address the differences in the distribution of patients across the CKD stages that could affect healthcare resource utilization, cost, and mortality differences, a summary of all patients with CKD was constructed, weighting the results for each stage by the proportion of patients with hyperkalemia in that stage (ie, the adjustment reweighted the population with CKD without hyperkalemia to have the same CKD severity distribution as the population with CKD and hyperkalemia).
Results
In the FFS Medicare population, 1,674,010 beneficiaries met the study inclusion criteria; of these, 39,056 beneficiaries were identified with hyperkalemia (prevalence, 2.3%; Table 1).
Table 1.
Study Sample Characteristics and Allowed Costs
| Characteristics | Medicare patients | Commercial insurance patients |
|---|---|---|
| Total population, N | 1,674,010 | 31,236,403 |
| Allowed PMPM cost, $ | 1034.68 | 438.11 |
| Average age, yrs | 70.3 | 32.1 |
| Female, % | 55.0 | 51.3 |
| Mortality rate, % | 4.3 | N/A |
| Comorbidity prevalence rate in the total population | ||
| Hyperkalemia, % | 2.333 | 0.090 |
| Ages 0–17 yrs, % | N/A | 0.012 |
| Ages 18–64 yrs, % | N/A | 0.116 |
| Diabetes, % | 21.5 | 3.6 |
| CKD, % | 11.3 | 0.4 |
| Heart failure, % | 9.7 | 0.2 |
| Hypertension, % | 61.9 | 11.0 |
| COPD, % | 13.1 | 0.7 |
| Patients with hyperkalemia, N | 39,056 | 28,002 |
| Allowed PPPM cost, $ | 5644.77 | 7400.74 |
| Allowed PMPM cost, $ | 124.07 (12.0% of total) | 7.09 (1.6% of total) |
| Average age, yrs | 72.9 | 49.1 |
| Female, % | 51.9 | 44.3 |
| Mortality rate, % | 23.6 | N/A |
| Comorbidity prevalence rate in patients with hyperkalemia | ||
| Diabetes, % | 54.2 | 38.3 |
| CKD, % | 64.8 | 31.8 |
| Heart failure, % | 47.6 | 12.2 |
| Hypertension, % | 90.9 | 62.4 |
| COPD, % | 36.4 | 7.9 |
CKD indicates chronic kidney disease; COPD, chronic obstructive pulmonary disease; N/A, not available; PMPM, per-member per-month; PPPM, per-patient per-month.
Source: Milliman's analysis of 2014 Medicare 5% sample data and MarketScan medical claims data.
In the total commercially insured sample, 31,236,403 individuals met the study inclusion criteria; of these, 28,002 individuals were identified as having hyperkalemia (prevalence, 0.09%).
The prevalence of several serious conditions (ie, CKD, hypertension, and diabetes) was markedly higher in patients with hyperkalemia than in the total Medicare and total commercially insured populations. In the total Medicare population and in Medicare patients with hyperkalemia, the prevalence of CKD was 11.3% and 64.8%, respectively. In the total commercially insured population and in commercially insured patients with hyperkalemia, the prevalence of CKD was 0.4% and 31.8%, respectively. The mortality rate was approximately 5.5 times higher in Medicare patients with hyperkalemia than in the total Medicare population (23.6% vs 4.3%, respectively).
The average allowed PPPM cost was 5 times higher in Medicare patients with hyperkalemia than in the total Medicare population ($5645 vs $1035, respectively) and 15 times higher in commercially insured patients with hyperkalemia than in the total commercially insured sample.
Because the prevalence of CKD was significantly higher in patients with hyperkalemia compared with all Medicare and commercially insured patients (64.8% vs 11.3%, respectively, and 31.8% vs 0.4%, respectively), we compared the cost, hospital inpatient admissions, and mortality for patients with CKD who had or did not have hyperkalemia.
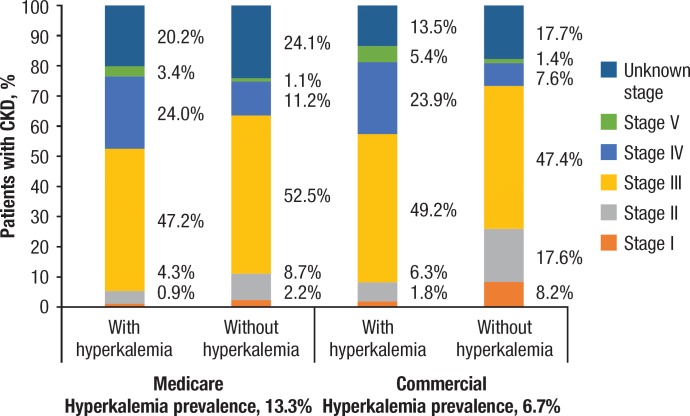
In our study, the prevalence of hyperkalemia in patients with CKD in Medicare and in commercially insured patients was 13.3% and 6.7%, respectively (Figure 1).
Figure 1. Patients with CKD, by Severity Level, with and without Hyperkalemiaa.
aPercentages may not add up to 100% because of rounding.
CKD indicates chronic kidney disease.
Source: Milliman's analysis of 2014 Medicare 5% sample data and MarketScan medical claims data.
In the Medicare and the commercially insured samples, patients with CKD plus hyperkalemia had a higher proportion of stage IV or stage V CKD and a lower proportion of stage I or stage II CKD than patients with CKD without hyperkalemia. Because of this finding, in our analyses of all patients with CKD, we performed severity adjustment for the group without hyperkalemia to achieve the same CKD severity weighting in the 2 groups.
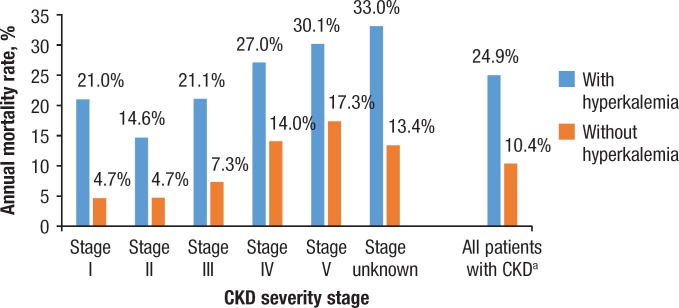
Within each CKD stage, mortality was higher for Medicare patients with hyperkalemia than for those without hyperkalemia (Figure 2). Furthermore, after adjusting for CKD severity, the annual mortality rate in Medicare patients with CKD was higher in those with hyperkalemia than in those without hyperkalemia (24.9% vs 10.4%, respectively). The commercial database does not contain mortality data.
Figure 2. Annual Mortality Rate in Medicare Patients with CKD with and without Hyperkalemia.
aOverall annual mortality rate in the hyperkalemia and nonhyperkalemia populations, after adjusting for CKD severity.
CKD indicates chronic kidney disease.
Source: Milliman's analysis of 2014 Medicare 5% sample data.
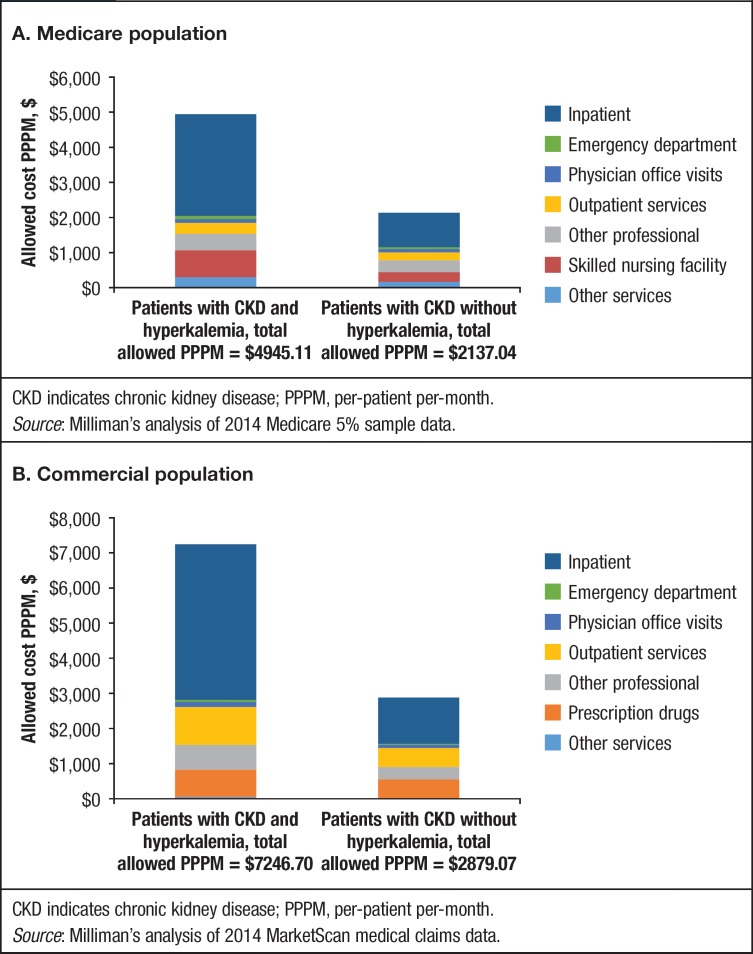
In an examination of cost of CKD, within each disease stage, patients with hyperkalemia had consistently higher costs than patients without hyperkalemia in the Medicare and the commercially insured populations (Table 2). Our calculations also showed that CKD severity–adjusted PPPM costs in Medicare patients with and without hyperkalemia were $4945 and $2137, respectively (difference, $2808). Such costs in commercially insured patients with CKD with and without hyperkalemia were $7247 and $2879, respectively (difference, $4368).
Table 2.
Allowed Per-Patient Per-Month Cost of CKD
| CKD severity stage | Medicare allowed PPPM cost, $ | Commercial allowed PPPM cost, $ | ||
|---|---|---|---|---|
| with hyperkalemia | without hyperkalemia | with hyperkalemia | without hyperkalemia | |
| Stage I | 4896 | 1509 | 5544 | 1508 |
| Stage II | 4571 | 1513 | 6052 | 1696 |
| Stage III | 4552 | 1842 | 6658 | 2488 |
| Stage IV | 5043 | 2525 | 6843 | 3703 |
| Stage V | 5491 | 2819 | 6442 | 3392 |
| Unknown stage | 5803 | 2450 | 11,332 | 3395 |
| All patients with CKDa | 4945 | 2137 | 7247 | 2879 |
PPPM cost in the hyperkalemia and nonhyperkalemia populations after adjusting for CKD severity.
CKD indicates chronic kidney disease; PPPM, per-patient per-month.
Source: Milliman's analysis of 2014 Medicare 5% sample data and MarketScan medical claims data.
Inpatient care was the main driver of cost in patients with CKD plus hyperkalemia in the Medicare and the commercially insured samples. In Medicare patients with CKD, inpatient care accounted for approximately 59% and 46% of the total spending for those with and without hyperkalemia, respectively. Similarly, in commercially insured patients with CKD, inpatient care accounted for approximately 61% and 43% of the total spending for those with and without hyperkalemia, respectively. Figure 3 presents the cost summary, stratified by service category for patients with CKD with and without hyperkalemia in the Medicare and the commercially insured samples.
Figure 3. Cost Summary for Patients with CKD with and without Hyperkalemia (CKD Severity Adjusted).
CKD indicates chronic kidney disease; PPPM, per-patient per-month.
Source: Milliman's analysis of 2014 Medicare 5% sample data.
CKD indicates chronic kidney disease; PPPM, per-patient per-month.
Source: Milliman's analysis of 2014 MarketScan medical claims data.
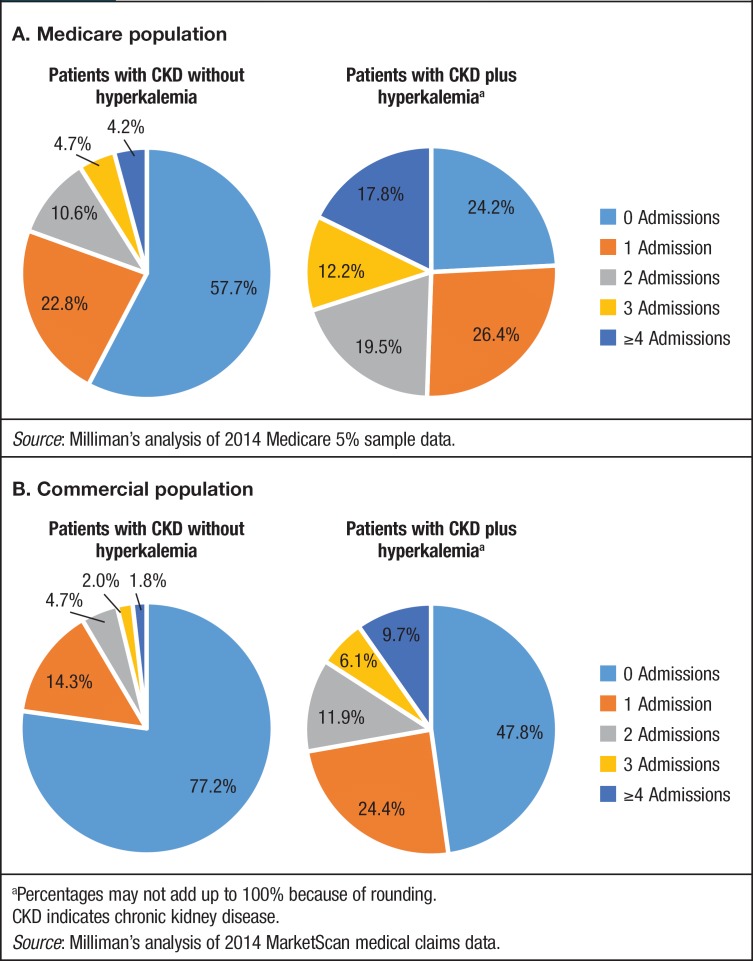
After adjusting for CKD severity, the proportion of patients with CKD in the Medicare sample who had ≥1 hospitalizations in 2014 was 75.8% for those with hyperkalemia versus 42.3% for those without hyperkalemia; in the commercially insured sample, these rates were 52.2% and 22.8%, respectively (Figure 4).
Figure 4. Hospital Admissions Incurred in Patients with CKD and with or without Hyperkalemia in 2014 (CKD Severity Adjusted).
Source: Milliman's analysis of 2014 Medicare 5% sample data.
aPercentages may not add up to 100% because of rounding.
CKD indicates chronic kidney disease.
Source: Milliman's analysis of 2014 MarketScan medical claims data.
Furthermore, the proportion of Medicare patients with CKD with and without hyperkalemia who had ≥4 admissions in 2014 was 17.8% versus 4.2%, respectively, and the proportion of patients with CKD with and without hyperkalemia in the commercially insured sample who had ≥4 admissions in 2014 was 9.7% versus 1.8%, respectively.
Discussion
In this descriptive, retrospective claims data analysis, we sought to examine the burden of hyperkalemia in US Medicare FFS and commercially insured populations by focusing on the prevalence of hyperkalemia and mortality rates, as well as on medical utilization and costs associated with hyperkalemia. To our knowledge, this is the first study to analyze healthcare utilization and cost in a large insured population from more than 1 payer or 1 institution.
The prevalence of hyperkalemia in our study was 2.3% among Medicare patients and 0.09% in commercially insured patients. Of note, compared with the prevalence rates in the medical literature, both rates were low. For example, in a retrospective analysis of >2 million records from 245,808 veterans with ≥1 hospitalizations and ≥1 measurements of serum potassium in fiscal year 2005, hyperkalemic events were documented in 3.2% of the records.18 Notably, the adjusted rate of hyperkalemia was higher in patients with CKD than in those without CKD among patients receiving RAAS inhibitors (7.67 vs 2.30 per 100 patient-months, respectively; P <.001) and in those who did not receive treatment with RAAS inhibitors (8.22 vs 1.77 per 100 patient-months, respectively; P <.001).18
A retrospective study of 1227 male veterans with CKD reported that 515 (42%) of them had ≥1 serum potassium levels of >5.3 mEq/L during a follow-up period of up to 20 years.22 Another retrospective study showed that among 5171 adults with possible CKD who started angiotensin-converting enzyme (ACE) inhibitor therapy between 1998 and 2006 at an HMO, 145 (2.8%) patients had hyperkalemia during the first 90 days of treatment.23 Another prospective analysis of 1038 patients with stage II to stage V CKD who were not undergoing dialysis showed that the prevalence of hyperkalemia increased from 2% to 42% as kidney function declined; the overall prevalence in this population was 17%.14 In reviews of randomized controlled trials in patients with CKD, the incidence of hyperkalemia has been shown to vary between 0.7% and 39.1%, depending on the definition of hyperkalemia and the subpopulation characteristics.2,3
It is likely that the results from our study, because they are based on claims data, underestimate the prevalence of hyperkalemia. A study assessing the difference in prevalence based on how it was defined showed that hyperkalemia defined by laboratory values was reported in 70 per 1000 person-years (7.4% of patients with a median follow-up of 5.5 months), whereas hyperkalemia defined by ICD-9-CM codes was reported in 9 per 1000 person-years (1.1% with a median follow-up of 6.6 months).17
Our findings are consistent with those in the medical literature that shows that hyperkalemia is associated with multiple comorbidities. Specifically, we found that in the Medicare and the commercially insured patients, the prevalence of CKD, diabetes, heart failure, and hypertension was higher in patients with hyperkalemia. A retrospective analysis showed that the odds of hyperkalemia were 57% higher in patients with ≥2 comorbid conditions (defined by the Charlson Comorbidity Index criteria) compared with those with no comorbidities.18 Another study showed that in patients with hyperkalemia, approximately 20.1% also had advanced CKD, 52.8% had diabetes, 53.3% had coronary artery disease, and 12.6% had peripheral vascular disease; furthermore, advanced CKD was a significant predictor of hyperkalemia in patients with CVD, which was defined as the presence of hypertension and heart failure.13
In a sample of 7653 patients receiving treatment for hypertension, individuals with low and high serum potassium levels (3.0–3.5 mEq/L and 5.1–5.9 mEq/L, respectively) had a significantly greater risk for CVD events than did those with middle-range levels (3.5–5.1 mEq/L).24 Multivariate-adjusted hazard ratios (HRs) from Cox models were 2.6 (95% confidence interval [CI], 1.5–4.4) in the low serum potassium group and 1.7 (95% CI, 1.0–2.7) in the high serum potassium group, with the middle serum potassium group used as reference.24 Among 1679 individuals who regularly took diuretics, the HRs were 4.3 (95% CI, 2.4–7.9) and 6.7 (95% CI, 2.8–15.9) in the low and high serum potassium groups, respectively. Neither low nor high serum potassium level was significantly associated with outcome events in patients who were not regularly using diuretics.24
Hyperkalemia is associated with increased resource utilization, particularly inpatient hospitalization. In our study, hyperkalemia was identified based on an inpatient claim in more than 66% of patients in the Medicare population and in approximately 50% of patients in the commercially insured population. In a retrospective study of medical records of patients with CKD, hyperkalemia was shown to be associated with an increased risk for hospitalization.11 Another study reported that the rate of hospital admission in patients with hyperkalemia who received ACE inhibitors more than doubled (from 1.2 per 1000 in early 1999 to 2.8 per 1000 by late 2001; P <.001) after publication of data from the RALES (Randomized Aldactone Evaluation Study) trial showing the benefits of spironolactone in patients with severe heart failure.25 In our study, we also found that in Medicare and commercially insured patients, the inpatient readmission rate was higher in patients with CKD plus hyperkalemia than in patients with CKD without hyperkalemia.
We also found that the mortality rate in the Medicare sample with hyperkalemia was markedly higher than that in the total Medicare population (23.5% vs 4.3%, respectively). Similarly, our analysis showed that the mortality rates in Medicare patients with CKD with and without hyperkalemia were 24.2% vs 9.4%, respectively. These results are consistent with those from a number of other studies. One study based on the medical records of more than 55,000 patients with CKD showed a correlation between hyperkalemia and the risk for death.11 Compared with patients with normal serum potassium (4.5–5.0 mEq/L), patients with a serum potassium level of 5.5 to 5.9 mEq/L had a 1.5-times higher adjusted mortality rate, and patients with a serum potassium level of ≥6.0 mEq/L had an adjusted mortality incidence rate that was 3.31 times higher.11
In a retrospective observational study of 39,705 adults receiving inpatient critical care, hyperkalemia was associated with higher all-cause mortality 30 days after the initiation of critical care.19 In a study of 15,803 patients with CVD who received antihypertensive drugs, a hyperkalemic event was a predictor of all-cause mortality (odds ratio, 1.56; 95% CI, 1.30–1.88).13 In a study of patients with severe hyperkalemia, the in-hospital mortality rate was 30.7%, which was strongly correlated with the difference between serum potassium levels at admission and the level at its highest point (odds ratio, 1.83; P <.001).20 In a retrospective study of 1924 patients diagnosed with acute myocardial infarction, the mortality risk over a 3-year follow-up period was greater in those with hyperkalemia than normokalemia during hospitalization (HR, 4.78 for potassium ≥5.0 mEq/L).21 A study of 1227 male veterans with CKD who were not on dialysis showed that the relationship between serum potassium and all-cause mortality over the course of up to 20 years followed a U-shaped curve, with the lowest mortality associated with a serum potassium level of 4.5 mEq/L, and higher mortality associated with either hypokalemia or hyperkalemia.22
Our cost calculations are based on information for all patients with documentation of hyperkalemia on a medical claim. Notably, we found that the average allowed PPPM cost was 5 times higher in the Medicare sample with hyperkalemia versus the total Medicare population and 15 times higher in the commercially insured sample with hyperkalemia versus the total commercially insured population. Our calculations also showed that CKD severity–adjusted PPPM costs in patients with hyperkalemia in the Medicare and the commercially insured populations were more than double than those for patients without hyperkalemia. The main driver of these cost differences was inpatient care. Nonetheless, payers should be aware of the increased spending in all the various service categories for patients with CKD with hyperkalemia versus patients without this comorbidity.
Limitations
We acknowledge several study limitations. First, the prevalence of hyperkalemia was based on claims data, which likely underestimated the true prevalence rate.
Second, mortality data are not available in the MarketScan database, and Medicare Part D pharmacy data are not available in the Medicare 5% sample.
Third, in our comparison of patients with CKD with and without hyperkalemia, we adjusted for CKD severity but not for other variables. If other variables are systematically associated with hyperkalemia, then it is possible that we have overestimated the contribution of hyperkalemia to mortality and costs.
Fourth, our conclusions regarding the relationship of CKD disease stage to the prevalence of hyperkalemia in the CKD population subset was limited, because the “unknown” CKD stage accounted for between 13.5% and 24.1% of the total population.
Conclusion
Using paid claims data, our analysis shows that hyperkalemia is associated with substantial clinical and economic burden in the US Medicare and commercially insured populations. Our findings pertaining to hyperkalemia-related prevalence, mortality, and resource utilization add value to the existing medical literature; furthermore, ours is the first study to analyze the cost implications of hyperkalemia in large patient populations.
Specifically, our analysis shows that costs in commercially insured and Medicare patients with hyperkalemia, including in a subset of patients with CKD, are markedly higher than the costs for patients without hyperkalemia. These new cost-related insights have important economic implications for payers, patients, and providers, and may help to underscore the need for improved treatment options in at-risk patients, specifically in those with chronic comorbidities.
Author Disclosure Statement
Ms Fitch, Mr Engel, and Dr Blumen are employees of Milliman, which received funding for this study from ZS Pharma. Dr Woolley is an employee of ZS Pharma.
Source of Funding
Funding for this study was provided by ZS Pharma.
Contributor Information
Kathryn Fitch, Principal, Milliman, New York, NY.
J. Michael Woolley, Executive Director, ZS Pharma, San Mateo, CA.
Tyler Engel, Associate Actuary, Milliman.
Helen Blumen, Principal, Milliman.
References
- 1. Chaitman M, Dixit D, Bridgeman MB. Potassium-binding agents for the clinical management of hyperkalemia. P T. 2016; 41: 43–50. [PMC free article] [PubMed] [Google Scholar]
- 2. Kovesdy CP. Management of hyperkalaemia in chronic kidney disease. Nat Rev Nephrol. 2014; 10: 653–662. [DOI] [PubMed] [Google Scholar]
- 3. Lazich I, Bakris GL. Prediction and management of hyperkalemia across the spectrum of chronic kidney disease. Semin Nephrol. 2014; 34: 333–339. [DOI] [PubMed] [Google Scholar]
- 4. Raebel MA. Hyperkalemia associated with use of angiotensin-converting enzyme inhibitors and angiotensin receptor blockers. Cardiovasc Ther. 2012; 30: e156–e166. [DOI] [PubMed] [Google Scholar]
- 5. Yancy CW, Jessup M, Bozkurt B, et al; for the American College of Cardiology Foundation; American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2013; 62: e147–e239. [DOI] [PubMed] [Google Scholar]
- 6. Stevens PE, Levin A; for the Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group Members. Evaluation and management of chronic kidney disease: synopsis of the Kidney Disease: Improving Global Outcomes 2012 Clinical Practice Guideline. Ann Intern Med. 2013; 158: 825–830. [DOI] [PubMed] [Google Scholar]
- 7. American Diabetes Association. 9. Microvascular complications and foot care. Diabetes Care. 2016; 39(suppl 1): S72–S80. [DOI] [PubMed] [Google Scholar]
- 8. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease. Kidney Int Suppl (2011). 2012; 2: 337–414. [Google Scholar]
- 9. Vardeny O, Claggett B, Anand I, et al; for the Randomized Aldactone Evaluation Study (RALES) Investigators. Incidence, predictors, and outcomes related to hypo- and hyperkalemia in patients with severe heart failure treated with a mineralocorticoid receptor antagonist. Circ Heart Fail. 2014; 7: 573–579. [DOI] [PubMed] [Google Scholar]
- 10. Lee JH, Kwon YE, Park JT, et al. The effect of renin-angiotensin system blockade on renal protection in chronic kidney disease patients with hyperkalemia. J Renin Angiotensin Aldosterone Syst. 2014; 15: 491–497. [DOI] [PubMed] [Google Scholar]
- 11. Luo J, Brunelli SM, Jensen DE, Yang A. Association between serum potassium and outcomes in patients with reduced kidney function. Clin J Am Soc Nephrol. 2016; 11: 90–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Heerspink HJ, Gao P, de Zeeuw D, et al. The effect of ramipril and telmisartan on serum potassium and its association with cardiovascular and renal events: results from the ONTARGET trial. Eur J Prev Cardiol. 2014; 21: 299–309. [DOI] [PubMed] [Google Scholar]
- 13. Jain N, Kotla S, Little BB, et al. Predictors of hyperkalemia and death in patients with cardiac and renal disease. Am J Cardiol. 2012; 109: 1510–1513. [DOI] [PubMed] [Google Scholar]
- 14. Moranne O, Froissart M, Rossert J, et al; for the NephroTest Study Group. Timing of onset of CKD-related metabolic complications. J Am Soc Nephrol. 2009; 20: 164–171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mushiyakh Y, Dangaria H, Qavi S, et al. Treatment and pathogenesis of acute hyperkalemia. J Community Hosp Intern Med Perspect. 2012; 1(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lederer E, Alsauskas ZC, Mackelaite L, Nayak V. Hyperkalemia. Medscape; Updated January 11, 2016. http://emedicine.medscape.com/article/240903-overview#showall. Accessed April 20, 2016. [Google Scholar]
- 17. Urbine TF, Schwenke DC, Wu WC, Dev S. ICD9 coding of hyperkalemia greatly underestimates incidence of lab-defined hyperkalemia in veterans with heart failure. J Card Fail. 2013; 19(8 suppl): S32. [Google Scholar]
- 18. Einhorn LM, Zhan M, Hsu VD, et al. The frequency of hyperkalemia and its significance in chronic kidney disease. Arch Intern Med. 2009; 169: 1156–1162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. McMahon GM, Mendu ML, Gibbons FK, Christopher KB. Association between hyperkalemia at critical care initiation and mortality. Intensive Care Med. 2012; 38: 1834–1842. [DOI] [PubMed] [Google Scholar]
- 20. An JN, Lee JP, Jeon HJ, et al. Severe hyperkalemia requiring hospitalization: predictors of mortality. Crit Care. 2012; 16: R225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Choi JS, Kim YA, Kim HY, et al. Relation of serum potassium level to long-term outcomes in patients with acute myocardial infarction. Am J Cardiol. 2014; 113: 1285–1290. [DOI] [PubMed] [Google Scholar]
- 22. Hayes J, Kalantar-Zadeh K, Lu JL, et al. Association of hypo- and hyperkalemia with disease progression and mortality in males with chronic kidney disease: the role of race. Nephron Clin Pract. 2012; 120: c8–c16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Johnson ES, Weinstein JR, Thorp ML, et al. Predicting the risk of hyperkalemia in patients with chronic kidney disease starting lisinopril. Pharmacoepidemiol Drug Saf. 2010; 19: 266–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Cohen HW, Madhavan S, Alderman MH. High and low serum potassium associated with cardiovascular events in diuretic-treated patients. J Hypertens. 2001; 19: 1315–1323. [DOI] [PubMed] [Google Scholar]
- 25. Juurlink DN, Mamdani MM, Lee DS, et al. Rates of hyperkalemia after publication of the Randomized Aldactone Evaluation Study. N Engl J Med. 2004; 351: 543–551. [DOI] [PubMed] [Google Scholar]