Abstract
Immature or semi-mature dendritic cells (DCs) represent tolerogenic maturation stages that can convert naive T cells into Foxp3+ induced regulatory T cells (iTreg). Here we found that murine bone marrow-derived DCs (BM-DCs) treated with cholera toxin (CT) matured by up-regulating MHC-II and costimulatory molecules using either high or low doses of CT (CThi, CTlo) or with cAMP, a known mediator CT signals. However, all three conditions also induced mRNA of both isoforms of the tolerogenic molecule cytotoxic T lymphocyte antigen 2 (CTLA-2α and CTLA-2β). Only DCs matured under CThi conditions secreted IL-1β, IL-6 and IL-23 leading to the instruction of Th17 cell polarization. In contrast, CTlo- or cAMP-DCs resembled semi-mature DCs and enhanced TGF-β-dependent Foxp3+ iTreg conversion. iTreg conversion could be reduced using siRNA blocking of CTLA-2 and reversely, addition of recombinant CTLA-2α increased iTreg conversion in vitro. Injection of CTlo- or cAMP-DCs exerted MOG peptide-specific protective effects in experimental autoimmune encephalomyelitis (EAE) by inducing Foxp3+ Tregs and reducing Th17 responses. Together, we identified CTLA-2 production by DCs as a novel tolerogenic mediator of TGF-β-mediated iTreg induction in vitro and in vivo. The CT-induced and cAMP-mediated up-regulation of CTLA-2 also may point to a novel immune evasion mechanism of Vibrio cholerae.
Introduction
It is well accepted that DCs play a central role in the induction of adaptive immune responses as well as in the maintenance of peripheral tolerance [1,2]. DCs are able to sense a wide array of pathogens and mount an appropriate T helper cell response through the expression of pattern-recognition receptors such as Toll-like receptors [3]. Naive CD4+ T cells can differentiate into a variety of CD4+ T cell subsets characterized by the cytokine produced: Th1 cells secrete predominately IFN-γ, Th2 cells release IL-4, IL-5 and IL-13 and Th17 cells typically produce IL-17 [4]. Although the contribution of DCs for CD4+ T cell polarization is under debate [5,6] several DC-derived mechanisms have been described to significantly direct Th cell phenotypes. Depending on the stimulus DCs change their maturation status by up-regulating surface expression of MHC-II and co-stimulatory molecules and by producing a defined set of cytokines to optimally induce distinct Th cell responses [7–9].
Adaptive immune responses are also characterized by the activation and differentiation of CD4+ regulatory T cells (Tregs). They consist of pre-existing thymus-derived, natural Tregs (nTregs) or are induced from naive CD4+ T cells in the periphery (iTregs). Both allow effector cell responses against pathogens but help to terminate these responses at later time points and prevent auto-reactive T cells from autoimmune attack [10–12]. While effector CD4+ T cell responses are characterized by their subsequent polarization into Th1, Th2, Th9 or Th17 subsets, fulfilling specific tasks in defending from viruses, intracellular and extracellular bacteria or fungi, the transcriptional regulation of the differentiation of Tregs from naive T cells or during polarized effector Th1 or Th2 responses for counter-regulation is still less well understood [13–15]. The induction of effector and regulatory T cells has been followed also for the balance between Th17 and Foxp3+ iTregs [16]. In this setting IL-6 plays a pivotal role in determining whether in the presence of TGF-β alone Foxp3+ iTregs will develop or in the combined activity of TGF-β plus IL-6 a Th17 response will be raised. Although DCs essentially influence Th17 cell polarization or iTreg induction, most of these studies did not address the DC subset, DC maturation state or by which molecular mechanisms DCs can act in a tolerogenic way [15].
Our previous work indicated how LPS- or TNF-matured DCs could induce polarized Th1 or Th2 CD4+ T cell responses, respectively [17]. In this context we also tested CT since it had been reported as an adjuvant that favored Th2 immunity [18–20]. However, also the induction of Th17 responses [21,22] or regulatory Foxp3- IL-10+ Treg cells [23] but not Th1 effector cells [24] have been described for CT. In vivo experiments indicated that the route of application and the use of CT versus its subunit B alone (CTB) could decisively direct immunogenicity or tolerogenicity of model antigens conjugated to CT or CTB. The oral route of CTB administration appears as dominantly tolerogenic showing induction of Foxp3+ and Foxp3- Tregs in mice [25]. Consequently, CTB-peptide conjugates have been tested in studies with patients suffering from Behcet's diesease and demonstrated substantial benefit [26]. However, the molecular mechanisms how CT or CTB induce Tregs are not known.
While immature DCs have been found to act as tolerogenic DCs via induction of T cell anergy or regulatory T cells [27], we found in addition that DCs matured with TNF reached only a semi-mature state and resembled tolerogenic steady state migratory DCs [28,29]. This enables them convert MOG peptide-specific naive T cells into IL-10-producing Foxp3- Tr1 cells in the EAE model [30]. In contrast, DCs reaching a fully mature state after LPS treatment resulting in strong inflammatory cytokine production and inducing Th1 immunity enhanced EAE symptoms [17,30]. The phenomenon of semi-maturation was later confirmed by global transcriptional analyses and showed that TNF-DCs initially instructed a Th2-like response that was converted into a Tr1 response after repeated injections [17].
Here we show that high doses of cholera toxin (CThi) do not induce TNF-like semi-maturation nor LPS-like DC full maturation, but a CT-specific gene expression profile of full maturation promoting Th17 immunity. In contrast, low doses of CT (CTlo) or its known intracellular mediator cAMP induced a semi-mature DC state, but distinct from TNF. CThi-, CTlo- or cAMP-mediated DC maturation were unique by induction of the tolerogenic molecule CTLA-2.
The CTLA-2 protein was first identified in murine activated cytotoxic T cells and mast cells [31]. The mouse carries two protein isoforms CTLA-2α and -2β, which are 90% identical [32] and have been described as inhibitors of the endolysosomal cysteine protease cathepsin L [33,34]. However, also a cathepsin L-independent function of CTLA-2 has been reported [35]. CTLA-2β seems to play an important role during embryogenesis since the respective homozygote gene-deficient mice show complete pre-weaning lethality (http://www.mousephenotype.org/data/genes/MGI:88555). In adult animals CTLA-2 mRNA expression was found preferentially in cells of immune-privileged organs such as murine brain cells [36], uterus [37], placenta [38], retinal pigment epithelial cells [39] and corneal endothelial cells [40]. It appears that CTLA-2α contributes to the immune privilege of the eye by promoting activation of TGF-β and thus, supporting local Foxp3+ iTreg generation [39,41]. Hence, we hypothesized that CTLA-2 expression in DCs might serve tolerogenic functions.
Here we established that CT and cAMP induce CTLA-2 in DCs. Subsequently, CTLA-2 acts as a tolerogenic molecule by promoting TGF-β dependent Foxp3+ Treg generation in vitro. Furthermore, CTlo- and cAMP-treated DCs, which are unable to secrete Th17-polarizing cytokines, induce in vivo tolerance in the EAE model. Our data further suggest a CTLA-2-specific immune evasion mechanism by Vibrio cholerae. This mechanism may be further exploited to study CTLA-2-mediated immunosuppression in other autoimmune models, allergies or transplantation.
Results
Cholera toxin- and cAMP-matured DCs express CTLA-2α and β
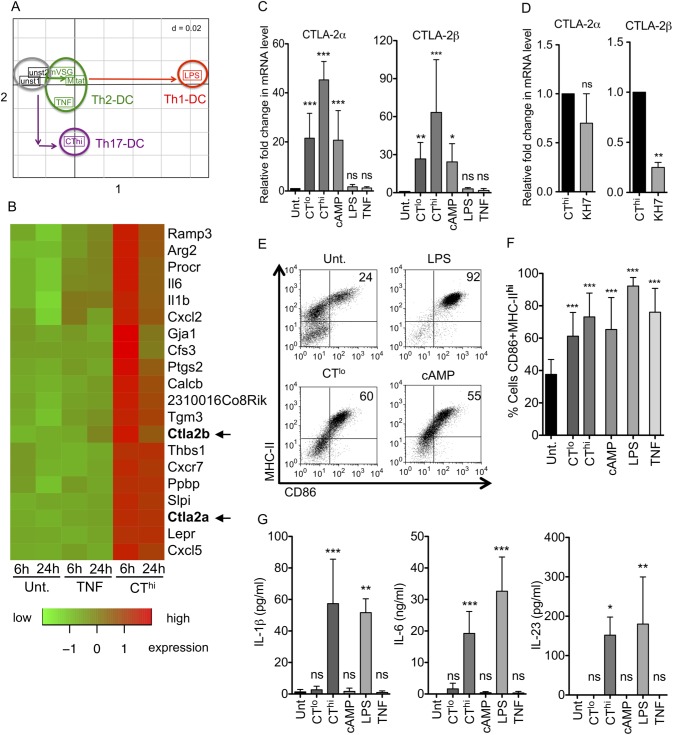
Previous work in our laboratory intended to identify gene expression profiles of LPS- or TNF-matured bone marrow-derived DCs (BM-DCs) for induction of Th1 or Th2 responses, respectively [17]. Here we compared the effects of CT on the gene expression profiles of murine BM-DCs with the previously identified profile. A principal component analysis confirmed that Th1- and Th2-inducing DCs show a gene signature clearly different from DCs treated with high doses of 1 μg/ml CT (termed CThi) (Fig 1A) and potentially indicating a Th17-inducing gene signature as suggested by others [42]. Among the top 25 genes regulated after 6 or 24h of CThi stimulation CTLA-2α and CTLA-2β were specifically up-regulated which was not observed with untreated or TNF matured DCs (Fig 1B) or by LPS or Trypanosoma-derived variant-specific surface glycoproteins (VSGs) stimulation [17]. Thus, CTLA-2α and CTLA-2β induction by CT in DCs is unique for CT and has not been reported before.
Fig 1. CT and cAMP induces both CTLA-2α and -2β during DC maturation.
BM-DCs were differentially matured with the indicated stimuli for 16h unless otherwise specified. (A) Principal component analysis comparing untreated BM-DCs, DCs matured for 6h with the Th2-inducing stimuli TNF, the Trypanosoma brucei antigens Mitat or mVSG, and the Th1-inducing LPS from our previous study [17] with CThi (1 μg/ml) matured Th17-inducing DCs investigated in this study. (B) Heat map displaying the top 25 genes regulated in DCs after CThi or TNF stimulation compared with untreated DCs. Data show single time point values of a single microarray. (C) Densitometric analysis of CTLA-2α and -2β expression levels determined by RT-sqPCR normalized to β-actin and relative to untreated control for n = 4 experiments; CTlo (0.1 μg/ml). (D) CThi stimulation of BM-DCs ± the cAMP inhibitor KH7 before RT-sqPCR normalized to β-actin of n = 3 independent and pooled experiments. (E) DC maturation analysis by flow cytometry of CD86 and MHC-II on CD11c positive cells. (F) Statistical evaluation of D with respect to untreated control for n = 5 experiments. (G) IL-1β, IL-6 and IL-23 secretion by differentially stimulated DCs measured by ELISA n = 3 experiments. Statistical analysis was performed with respect to untreated control. Error bars represent mean ± SD. One Way ANOVA, Dunnett post-test. *p<0.05, **p<0.01, ***p<0.001, ns: not significant. For D, student's t test, n = 3, *p<0.05.
Next we tested whether the induction of CTLA-2 by CT was dose-dependent and which down-stream mediator would account for the CT effect. CT is internalized by the cells via the GM1 ganglioside and once inside the cells, subunit A of the CT complex leads to activation of adenylate cyclase and an ensuing elevation in cyclic AMP (cAMP) levels, which triggers a wide spectrum of intracellular signaling events [43]. Therefore, we used a cell membrane-permeable analog of cAMP, 8-CPT-cAMP (referred from now on simply as cAMP). The cAMP concentration of 100μM correlated with 0.1μg/ml CT for CTLA-2α and CTLA-2β induction and DC surface marker expression as revealed by dose titration experiments (not shown). The specific upregulation of both CTLA-2α and CTLA-2β mRNA was observed independent of using different doses of CT such as high doses of 1 μg/ml (CThi) or low doses of 0.1 μg/ml (CTlo) or by its intracellular mediator cAMP, but not other stimuli could be confirmed by sqPCR (Fig 1C). To test whether CTLA-2α/β induction by CT required cAMP, the adenylate cyclase inhibitor KH7 was added during CThi stimulation of BM-DCs. While CTLA-2α showed only a trend of reduced mRNA levels, the reduction of CTLA-2β was significant (Fig 1D), indicating that cAMP is indeed the signaling intermediate of CT, at least for CTLA-2β induction. While CThi and CTlo as well as cAMP treatments of BM-DCs induced the expression of surface maturation markers (Fig 1D and 1E), only CThi-DCs were found to secrete IL-1β, IL-6 and IL-23 (Fig 1G). As expected, LPS induced both surface markers and cytokines similar to CThi (Fig 1F and 1G). TNF treatment led to a semi-mature phenotype, up-regulating maturation markers but lacking cytokine production (Fig 1F and 1G), similar to the treatment under CTlo or cAMP conditions. Thus, the gene expression profile of CThi-DCs predicts the induction of Th17 cells and is different from Th1- and Th2-inducing DCs. All three conditions of CThi-DCs, CTlo-DCs or cAMP-DCs induced CTLA-2α and CTLA-2β mRNA that may predict a contribution to Treg induction.
CThi-DCs favor Th17 responses while CTlo- or cAMP-DCs induce CTLA-2-dependent Foxp3+ iTreg conversion in vitro
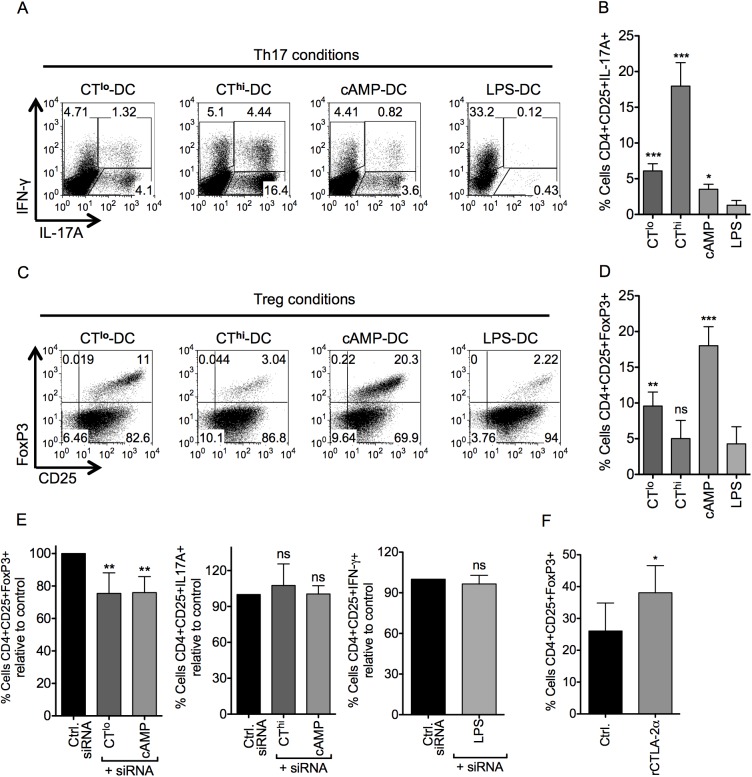
After having analyzed the maturation profile of CT- or cAMP-matured DCs, we wanted to determine the type of CD4+ T helper/Treg cell response that would be induced by these differentially matured DCs. CT- or cAMP-treated DCs were co-cultured with OT-II T cells in the presence of Th17-polarizing cytokines (TGF-β + IL-6) or under Treg conversion conditions (TGF-β). CThi-DCs clearly induced a Th17 profile in polarization assays while CTlo- and cAMP-DCs showed a much lower Th17 conversion (Fig 2A and 2B). LPS-DCs induced Th1 cells even under Th17 polarizing conditions, indicating that IL-12 production may overrule the Th17 conditions (Fig 2A and 2B). Under Treg conversion conditions LPS- and CThi-matured BMDC were unable to generate CD4+CD25+Foxp3+ T cells (iTreg), while CTlo or cAMP-DCs clearly favored Foxp3 expression (Fig 2C and 2D). Of note, the generation of Foxp3+ Tregs was strictly dependent on the addition of exogenous TGF-β (not shown). Although CThi-DCs induced the expression of CTLA-2α/β similar to cAMP-DCs, the observed results indicate that the Th17 polarizing effects by IL-1β, IL-6 and IL-23 [44] dominate over the CTLA-2-mediated effects on Treg conversion.
Fig 2. CTlo- or cAMP-DCs enhance TGF-β dependent Foxp3+ iTreg conversion via CTLA-2 in vitro.
OT-II T cells were co-cultured with C57BL/6 BM-DCs matured with the indicated stimuli (CTlo 0.1 μg/ml; CThi 1 μg/ml; cAMP 100 μM; LPS 0.1 μg/ml) in the presence of (100 ng/ml) OVA327-339 peptide and TGF-β (2 ng/ml) + IL-6 (20 ng/ml) for Th17 polarizing conditions or TGF-β (2 ng/ml) for iTreg conversion conditions. (A) After 5 days cells were re-stimulated for 6 h with 30 ng/ml PMA + 1 μg/ml ionomycin in the presence of 5 μg/ml brefeldin A + 2μM monensin and IL-17A and IFN-γ producing OT-II cells were analyzed by flow cytometry in a CD4+Vβ5+ gate. (B) Statistics of A with respect to LPS-DCs used as negative control for n = 5 experiments. (C) After 5 days cells were analyzed by flow cytometry for Foxp3 and CD25 expression in a CD4+Vβ5+ gate. (D) Statistics of C with respect to LPS-DCs used as negative control for n = 5 experiments. (E) OT-II naïve T cells were co-cultured with BM-DCs first transfected with 5 μM siRNA against CTLA-2, scrambled siRNA or mock-electroporated (pooled controls) and then, treated with different stimuli. Graphs represent changes in the frequency of iTreg (n = 7), Th17 (n = 6) and Th1 (n = 3) normalized to control. Numbers inside each dot plot represent the cell frequency in each quadrant. Error bars represent mean ± SD. One Way ANOVA, Dunnett post-test. *p<0.05, **p<0.01, ***p<0.001, ns: not significant. (F) C57BL/6 naïve CD4+CD25- T cells were cultured in the presence of TGF-β plus recombinant CTLA-2α. After 3 days cells were analyzed by flow cytometry for Foxp3 and CD25 expression in a CD4+ gate (n = 6). Error bars represent mean ± SD. Two-tailed paired Student’s t test. *p<0.05.
To assess if these observations were indeed prompted by CTLA-2, we performed in vitro T cell polarizations assays blocking CTLA-2α/β in DCs by siRNA. The results indicate that inhibition of CTLA-2α/β in both CTlo- and -cAMP-matured DCs led to an impaired capacity to convert naïve T cells into iTregs, but had no effects on Th17 or Th1 polarization (Fig 2E). Likewise, addition of recombinant CTLA-2α into an anti-CD3 antibody mediated-Treg assay significantly increased the frequency of iTregs in the presence of TGF-β (Fig 2F).
Taken together, these results suggest that CTlo- and -cAMP-matured DCs enhance the TGF-β dependent conversion of naïve T cells toward iTreg supported by CTLA-2α/β. Under CThi conditions the effect of CTLA-2α/β seems to be outcompeted by the production of Th17 polarizing cytokines IL-1β, IL-6 and IL-23 by the DCs.
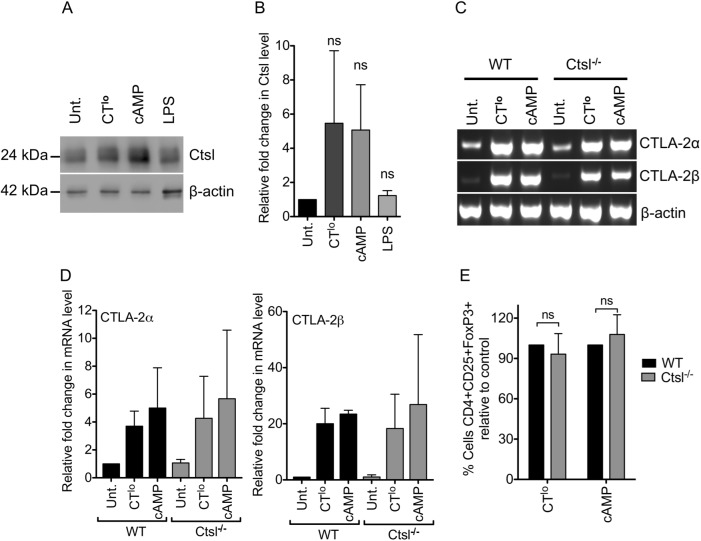
Cathepsin L expression is not required in CT/cAMP-DCs for iTreg conversion
Since both CTLA-2α/β molecules have been described to inhibit cathepsin L (ctsl) [33,34] we tested whether deficiency of cathepsin L in CT-DCs would influence the CTLA-2-mediated Treg conversion. Western blot analysis revealed that cathepsin L, the substrate of CTLA-2α/β, was induced to a similar extent when DCs were treated with CT or cAMP but not using LPS (Fig 3A and 3B), indicating that substrate and inhibitor are induced under the same conditions. However, DCs derived from Ctsl-/- mice stimulated with CT and cAMP could induce the expression of CTLA-2α and -2β mRNA to the same level as WT DCs (Fig 3C and 3D). When WT or Ctsl-/- DCs treated with CTlo or cAMP were used in a Treg conversion assay, they were similarly able to generate iTregs (Fig 3E). This indicates that cathepsin L expression in CT/cAMP-treated DCs does not influence iTreg conversion and also suggests that CTLA-2α/β might promote iTreg conversion independently of its interaction with DC-derived cathepsin L.
Fig 3. Cathepsin L expression in CT/cAMP-DCs does not influence iTreg conversion.
(A) BM-DCs were differentially matured with the indicated stimuli for 10 h (CTlo 0.1 μg/ml; cAMP 100 μM; LPS 0.1 μg/ml). Total cell lysates were analyzed for mature Ctsl protein content by Western Blot. One representative experiment is shown. (B) Densitometric analysis of Western blot data of 3 mice per group from 3 independent experiments performed like the one shown in A, normalized to β-actin and relative to untreated control. (C) BM-DCs were stimulated with CTlo or cAMP for 4 h. CTLA-2α and -2β mRNA expression was determined by RT-sqPCR, representative experiment, (D) Densitometric analysis of mRNA data of 3 mice per group from 3 independent experiments performed like the one shown in C, normalized to β-actin and relative to WT untreated control. (E) OT-II T cells were co-cultured with WT or Ctsl-/- BM-DCs-treated with CTlo or cAMP for 4 h in the presence of 100 ng/ml OVA327-339 peptide and 2 ng/ml TGF-β. After 5 days cells were analyzed by flow cytometry for Foxp3 and CD25 expression in a CD4+Vβ5+ gate. Data represent the change in the frequency of iTreg conversion using Ctsl-/- DCs normalized to WT DCs of n = 5 experiments. Error bars represent mean ± SD. (B) One Way ANOVA, Dunnett post-test. (E) Two-tailed Student’s t test. ns: not significant.
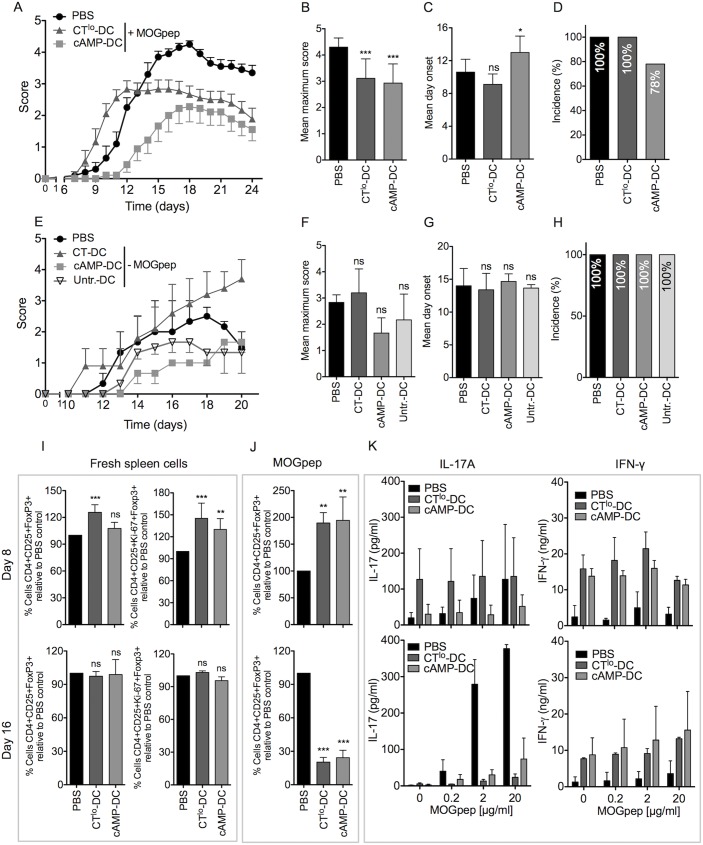
Both CTlo and cAMP-treated DCs are protective in EAE
Since CTlo- and cAMP-DCs exerted dominantly tolerogenic functions in vitro by inducing Tregs supported by CTLA-2, we tested if the injection of CTlo- and cAMP-DCs loaded with the auto-immunogenic peptide MOG would be able to prevent EAE, using the same protocol as we applied before for tolerogenic and semi-mature TNF-stimulated DCs [17,30]. Three i.v. injections of either DC type were given to each mouse at days -7, -5, -3, before EAE was induced at day 0. While CTlo-DCs showed an elevated clinical score at early time points the late disease score and the maximum score remained lower than that of the PBS-treated control group without influencing the day of onset or incidence (Fig 4A to 4D). The clinical score of animals injected with cAMP-DCs appeared both delayed and lower with changes in the day of onset and reduced incidence (Fig 4A to 4D). Control mice injected with CTlo- and cAMP-DCs that were not pulsed with MOG peptide as well as mice injected with untreated-DC (immature) did not show significant differences in day onset, in the maximum score or in the incidence of the disease compare with PBS-treated mice, indicating the requirement for MOG peptide loaded on the CTlo/cAMP-DC (Fig 4E to 4H).
Fig 4. Both CTlo and cAMP-matured DCs are protective in EAE.
(A) CTlo (0.1 μg/ml) or cAMP (100 μM) treated BM-DCs loaded with 40 μg/ml MOG35-55 peptide were injected i.v. at days -7, -5, -3 (2×106/mouse) before MOG-specific EAE induction at d0. Control mice received PBS injections. Average disease scores were monitored for a total of 10 mice per group from two independent experiments. Error bars represent mean ± SEM. (B), (C) and (D) Statistical analyses of different other clinical parameters derived from A. Error bars represent mean ± SD of pooled results from n = 10 mice. (E) CTlo (0.1 μg/ml), cAMP (100 μM) treated BM-DCs or untreated BM-DCs were injected i.v. at days -7, -5, -3 (2×106/mouse) before MOG-specific EAE induction at d0. Control mice received PBS injections. Average disease scores were monitored for a total of 6 mice per group of two independent experiments. Error bars represent mean ± SEM. (F), (G) and (H) Statistical analyses of different other clinical parameters derived from E. Error bars represent mean ± SD of pooled results from n = 6 mice. (I) Spleen cells of EAE mice treated like in A were analyzed 8 or 16 days after EAE induction for their Foxp3+ Treg relative frequencies or Ki67+ proliferating Foxp3+ Treg frequencies. (J) Like in I, but the spleen cells were re-stimulated with 10 μg/ml MOG35-55 peptide and then the relative frequencies of Treg expansion were determined after 5 days. (K) Like in I, but splenocytes were re-stimulated with graded concentrations of MOG35-55 peptide and after 3 days their supernatants analyzed by ELISA for IL-17A and IFN-γ production. (I-K) Error bars represent mean ± SD of pooled results from n = 6 mice. One Way ANOVA, Dunnett post-test. *p<0.05, **p<0.01, ***p<0.001, ns: not significant.
When the splenic Treg population was analyzed before the onset (d8) and around the peak of disease (d16), increased frequencies of total and proliferating CD4+CD25+Foxp3+ were observed only at d8, but not at d16 in animals injected with CTlo- and cAMP-DCs (Fig 4I). Re-stimulation of spleen cells with MOG peptide indicated also a higher frequency of MOG-specific Treg in the CTlo- and cAMP-DC treated groups (Fig 4J) but hardly any MOG-specific IL-17A and IFN-γ at day 8 (Fig 4K). This picture dramatically changed at day 16, where those animals protected from EAE by the treated-DC injections showed lower frequencies of Tregs, a complete abrogation of MOG-specific IL-17A production and partially elevated levels of IFN-γ in the spleen (Fig 4J and 4K). Together these data suggest that injections of MOG-loaded CTlo- and cAMP-DCs partially protect mice from clinical EAE symptoms. The observed expansion of MOG-specific Foxp3+ Tregs before the onset of the disease correlates with the inhibition of MOG-specific Th17 cell development while not suppressing the IFN-γ response.
Discussion
Besides the accepted central roles of DCs to initiate T cell activation, to instruct polarized T helper cell responses and to control T cell tolerance, the molecular basis underlying these polarizing events are much less clear. Here we found that the CT, a pathogen product that would naturally be secreted by Vibrio cholerae bacteria, exerts two types of instructive signals on DCs differentially influencing CD4+ T cell polarization. DCs treated under CThi conditions secrete the Th17-polarizing cytokines IL-1β, IL-6 and IL-23 but also CTLA-2, a molecule that has so far not been identified to be produced by DCs. CTLA-2α expression in retinal pigment epithelial cells has been found to contribute to the immune privilege in the eye by induction of Foxp3+ Tregs [39]. Lowering the dose of CT or treating with the intracellular downstream signal mediator cAMP results in a weaker DC maturation characterized by the up-regulation of surface maturation markers and the production of CTLA-2, but lacked the production of Th17 polarizing cytokines. As a result CThi-DCs induced preferentially Th17 responses, while CTlo-DCs promoted TGF-β dependent Treg conversion from naive T cells similar to what had been found in the eye.
While the polarization of CD4+ T cells into all known Th cell subsets depends on cytokine signals, different groups seem to exist that are linked to each other by counter-regulation. It appears that polarized Th1 and Th2 induction are linked, as well as the induction of Th17 and Foxp3+ Tregs. For induction of Th1 immunity the production of IL-12p70 has been defined as a clear Th1 polarizing signal [45], while other data indicate that the signal strength for T cells such as with high doses of antigen also favors Th1 polarization [46–48]. On the other hand, Th2 induction may just require the absence of IL-12p70 or lower doses of antigen [17,49,50] or IL-4 produced by innate cells [51–53]. In contrast, TGF-β is critically involved to promote both Th17 and Foxp3+ Tregs, while additional production of IL-1β, IL-6 and IL-23 shift the balance towards Th17 cells and retinoic acid towards Tregs [54]. Since Th17 and Treg generation are linked, it is tempting to speculate whether cholera bacteria may exploit this link by balancing Th17 immunity with Treg tolerance through induction of CTLA-2 production by DCs.
Our microarray data also indicated an induction of Ctla2a and Ctla2b by CT, which could be confirmed by sqPCR. The induction of CTLA-2 was unique to CT and cAMP and not observed for TNF or LPS or as previously shown for two different Trypanosoma antigens [17]. Lowering the dose of CT or using its intracellular signaling molecules cAMP for DC treatment abrogated DC cytokine production, whereas the surface marker maturation and the production of CTLA-2 were maintained. While LPS-DCs failed to exert tolerogenic functions in the Treg conversion assays in vitro, CTlo- and cAMP-DC clearly showed TGF-β induced Treg conversion that was partially dependent on CTLA-2.
While the injection of tolerogenic DCs represents a therapeutic option for clinical application in transplantation and autoimmunity, their stable tolerogenicity is required to avoid secondary maturation and thereby shifting to immunogenic DC phenotypes [55,56]. Our data indicate that tolerogenic DC maturation under CTlo and cAMP conditions may easily switch to an immunogenic DC maturation when CT doses increase. Thus, the identification and application of defined molecular mediators of DC tolerance such as CTLA-2 may be advantageous over the treatment with whole tolerogenic DC. Although a large variety of DC subsets treated in different ways have been tested to achieve suppression or tolerance in animal models, the molecular basis of their tolerogenicity is often much less clear. Here we found that CTLA-2 production by DCs cooperates with TGF-β to convert and expand Tregs. It will be interesting to further investigate tolerogenic functions of CTLA-2 secreting DCs or the CTLA-2 molecule alone for their therapeutic potential as exemplified here in the EAE model.
Along this line cAMP-treated DCs may offer new possibilities to generate human tolerogenic DCs. For this, the interesting question remains if there is a human counterpart for mouse CTLA-2. Although a homologous gene has not been identified in human, one known CTLA-2 binding partner is murine cathepsin L. The murine cathepsin L molecule has a lower protein sequence homology and identity with human cathepsin L as compared to human cathepsin V [57] and both, murine cathepsin L and human cathepsin V, show similar tissue expression pattern and functional activity for invariant chain degradation [58]. Therefore, a functional homologue of murine CTLA-2 may exist in human DCs, but potentially as an interaction partner of cathepsin V.
Previous work suggested that a semi-mature stages of DCs such as achieved with TNF may still allow tolerogenic functions on CD4+ T cells when injected repetitively into mice [28]. Key features of this semi-maturation were their upregulation of MHC-II and costimulatory molecules such as CD80, CD86 or CD40 but the failure to secrete cytokines. The phenotype of semi-mature BM-DCs generated in vitro is highly similar to steady state migratory DCs that transport self-antigens to the lymph nodes, where they tolerize CD4+ T cells by converting them into Foxp3+ Tregs [29,59]. Here we found that semi-mature CTlo- and cAMP-DCs appear with a partially similar, but also distinct phenotype and CThi-DCs with some similarities in the transcriptional gene signature as compared to semi-mature TNF-DCs. Our previous data suggested that TNF-DCs showed a weak inflammatory gene signature that led to polarization of CD4+ T cells into a Th2 response that, upon repetitive stimulation, shifted toward tolerogenic IL-10+ Tr1 cells [17,30]. Here we find that CThi-DCs showed a similar inflammatory gene expression profile (Il1b, Il6, Ptgs2 = COX2) and the production of Th17 promoting cytokines IL-1β, IL-6 and IL-23 by ELISA.
Studies with a fusion protein of rCTLA-2α bound to an IgG molecule did not indicate a direct binding of CTLA-2 to other immune cells (unpublished data). For CTLA-2β dimerization formation has been described [33] that may also be required to exert its tolerogenic functions including potential binding to a hypothetical cell surface receptor of the TGF-β family, similar to other TGF-β signaling enhancers such as activin A [60]. These data may point to an interaction of CTLA-2 dimers with TGF-βR family members or promoting conversion of latent TGF-β to active TGF-β to enhance the observed Treg conversion [61,62]. The proteolytic cleavage of latent TGF-β from murine and rat fibroblast cell lines by cathepsin D [63] or human latent TGF-β by cathepsin B [64,65] into its active form has been described before. Human cathepsin L can degrade the single-chain isoform of cathepsin D [66]. It is conceivable that CTLA-2 as a cathepsin L inhibitor may promote TGF-β indirectly via cathepsin D. However, in our experiments Ctsl-/- DCs were able to convert Tregs to a similar extent as observed with WT DCs. It remains to be tested whether CTLA-2 directly interferes with cathepsin D or other molecules to promote latent TGF-β conversion.
CT has been proposed as a vaccine adjuvant. Different routes of administration have been tested to work successfully, including subcutaneous [67], epicutaneous [68] and oral administration [69]. Nasal application in animals with EAE ameliorated their clinical scores [70]. The adjuvant effect of intravenously injected CT was dependent on DCs residing in the marginal zone [71]. However, microbes that are well adapted to their hosts allow a balanced immune response that enables microbial control and host survival, but also counter-regulatory immune evasion mechanisms that prevent complete microbial elimination. The use of microbial substances as vaccine adjuvants may be counteracted by unwanted immune evasion strategies from the respective microbe. Several immune evasion strategies have been described for Vibrio cholerae, however not the induction of CTLA-2 [72]. Thus the tolerogenic effects observed by CTLA-2 activity may represent a novel mechanism of immune evasion mediated by CT.
Conclusion
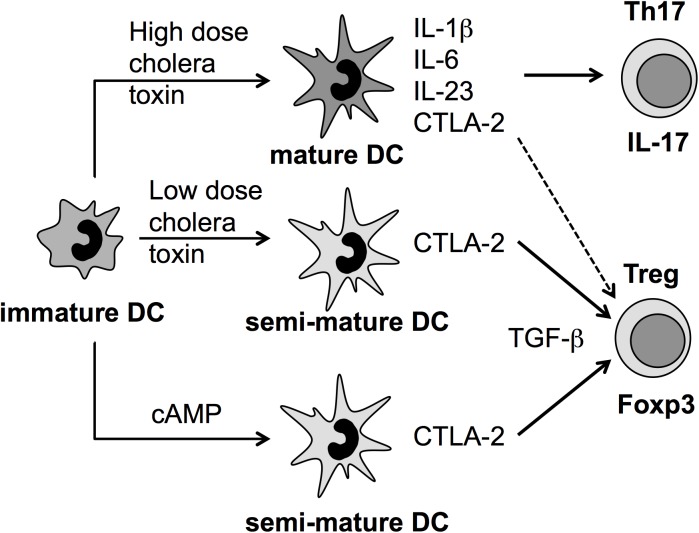
Here we show that the tolerogenic molecule CTLA-2 can be produced by DCs after stimulation with CT. High doses of CT induce Th17 polarizing cytokines and thereby favoring the polarization into this T cell subset. Low doses of CT or its mediator cAMP induce a DC semi-mature state characterized by the upregulation of surface MHC II and costimulatory molecules in the absence of pro-inflammatory cytokine secretion. In addition and thereby different from the semi-mature TNF-DC phenotype, both treatments also induce the expression of CTLA-2, which cooperates with TGF-β for the conversion of Foxp3+ regulatory T cells (Fig 5). Thus, CTLA-2 molecules may represent promising candidates for further studies to treat autoimmune diseases, but also to better understand immune evasion of cholera bacteria.
Fig 5. Model on the differential effects of CT and cAMP on DC-directed induction of Th17 or Foxp3+ Treg cells.
Immature DCs treated with high (CThi) or low (CTlo) doses of cholera toxin or its known secondary mediator cAMP induced partial DC maturation measured as upregulation of MHC II- and costimulatory molecules such as CD86. CTlo-DCs and cAMP-DCs produced no pro-inflammatory cytokines (semi-mature DCs) but instead the tolerogenic molecule CTLA-2. Under Treg polarizing conditions in vitro, using naive TCR-transgenic CD4+ T cells, CTLA-2 produced by CTlo-DCs and cAMP-DCs supports the TGF-β mediated conversion into Foxp3+ Tregs. In contrast, CThi-DCs also released CTLA-2 but additionally the Th17-polarizing cytokines IL-1β, IL-6 and IL-23 (mature DCs). Consequently CThi-DCs mainly generated Th17 cells in vitro. In vivo, a polyclonal repertoire of T cells triggered by CTlo-DCs and cAMP-DCs results in both Th17 and Tregs activation pointing to competing effects at early or late time points in the EAE model.
Materials and methods
Animals
The animal experimetns have been permitted by and were controlled through the Regierung von Unterfranken, AZ55.2–2531.01-52/14. C57BL/6 (Charles River), OT-II (kindly provided by F. Carbone, Melbourne), OT-II/Rag1-/- mice (RAG1-/- from JAX mice) and cathepsin L-/- (Ctsl-/-) mice [73] were bred under pathogen-free conditions in our facilities. All animal experiments were performed using age- and sex-matched animals. The mice were sacrificed by CO2 inhalation according to approved standard operating procedures. For EAE experiments, the animals were immunized or pertussis toxin-injected according to approved standard operating procedures.
Flow cytometry
Surface staining: performed at 4°C using PBS supplemented with 0.1% BSA and 0.1% sodium azide (FACS buffer). mAbs were purchased from BioLegend, unless otherwise indicated. Pacific Blue-conjugated mAb: anti-CD4 (GK1.5). FITC-conjugated mAbs: anti-MHC-II (M5/114.15.2, BD Biosciences), anti-CD86 (GL1), anti-Vβ5.1 and 5.2 TCR (MR9-4). PE-conjugated mAbs: anti-MHC-II (M5/114.15.2), anti-CD86 (GL1), anti-CD25 (PC61), anti-Vβ5.1 and 5.2 TCR (MR9-4). APC-conjugated mAbs: anti-CD11c (N418), anti-CD25 (PC61). PerCP/Cy5.5-conjugated mAb: anti-CD4 (GK1.5). PE/Cy7- conjugated mAb: anti-CD25 (PC61). Fc receptors were blocked by pre-incubating the cells with 10% of supernatant from 2.4G2 hybridoma (anti-Fc-γ-RII/III; ATCC) prior to staining. Intracellular staining: cells were fixed using 2% formaldehyde, permeabilized with perm buffer (0.5% saponin in FACS buffer) and stained at 4°C using the following Abs in perm buffer: anti-IFN-γ-FITC (XMG1.2), anti-IL-17A-PE (TC11-18H10; BD Biosciences). Nuclear staining of Foxp3 and Ki67: performed using the eBioscience anti-mouse Foxp3 staining set according to the manufacturer’s instructions. Anti-Foxp3-Alexa Fluor 647 (150D) and anti-Ki67-PE or Alexa Fluor 647 (16A8) antibodies were used. Samples were measured in LSRII flow cytometer (BD Biosciences) and data were analyzed with FlowJo software v8.7 (TreeStar).
Generation of BM-DCs
Murine BM-DCs were generated as previously described [74]. Briefly, bone marrow precursor cells were obtained by perfusion from femur and tibias of C57BL/6 mice and seeded in petri dishes (100 mm, Greiner) at 3×106 cells/dish in 10 ml of complete medium: RPMI 1640 (Sigma) supplemented with 10% heat-inactivated FCS (GIBCO), 100 U/ml penicillin (Sigma), 100 μg/ml streptomycin (Sigma), 2 mM L-glutamine (Sigma) and 50 μM β-mercaptoethanol (Sigma-Aldrich). To induce the differentiation to DCs, the medium was additionally supplemented with 10% of a supernatant obtained from the X-63 cell line transfected with the GM-CSF murine gene [75]. The cells were culture at 37° C, 7% CO2. On day 3 of culture, 10 mL of complete RPMI medium supplemented with 10% GM-CSF-containing supernatant was added. On day 6, 10 ml of the medium was removed and fresh medium was added as at day 3. In some cases (EAE), the cells were fed again at day 8.
CTLA-2 induction in BM-DCs and cAMP inhibition
Day 8 BM-DCs were cultured in complete medium at 1×106 cells/ml in the presence of 10% GM-CSF-containing supernatant without (untreated) or with different stimuli: 0.1 μg/ml cholera toxin (Sigma-Aldrich) as low dose (CTlo), 1 μg/ml cholera toxin as high dose (CThi), 100 μM 8-CPT-cAMP (cAMP, Proteinkinase.biz), 0.1 μg/ml LPS (from E. coli, Sigma-Aldrich) and 500 U/ml TNF-α (Peprotech). The adenylate cyclase inhibitor KH7 (TOCRIS) was used at 100 μM to inhibit cAMP. Total RNA was extracted from DCs using TRIzol® reagent (Invitrogen-Life Technologies) according to the manufacturer’s instructions. cDNA was synthesized using BioScript™ Reverse Transcriptase (Bioline). The relative mRNA levels of both CTLA-2α and β was determined by sqPCR using the following primers: CTLA-2αF, 5’-CTTCAGTGCTGTCTTCCTGCTCAT-3’;
CTLA-2αR, 5’-TTACTCTGGCTGAGCCCTTCCA-3’;
CTLA-2βF, 5’-GGACAACAAAGTTCTGGTTTCTATCTG-3’;
CTLA-2βR, 5’-AACTGTTACTCTGGCTGAGCCCTT-3’;
β-actinF, 5’-CCTAGGCACCAGGGTGTGAT-3’;
β-actinR, 5’CTCTTTGATGTCACGCACGATTTC-3’. The PCR products were separated by electrophoresis using a 2% agarose gel. The bands were visualized by staining with ethidium bromide. Amplicons were quantified by densitometry using ImageJ v1.48 software [76] upon normalizing using a β-actin control.
For microarray analysis bone marrow precursor cells were depleted of T and B cells using anti-CD90.2 and anti-CD19 magnetic beads (Miltenyi Biotec), respectively. Day 8 BM-DCs were stimulated as mentioned above and total RNA was extracted. Samples were prepared and microarray analysis performed as previously described [17]. RNA integrity and comparability between samples was tested using a BioAnalyzer (Agilent). RNA integrity numbers were between 9,8 and 10.
Cytokine production by BMDC
The supernatants of matured BM-DCs were collected and centrifuged at 10,000×g for 10 min prior to measurement. IL-1β, IL-6 (both BD Biosciences) and IL-23 (eBioscience) production were determined by ELISA. Absorbance was detected using the SpectraMax Plus 384 Microplate Reader (Molecular Devices).
In vitro Th17 and Th1 differentiation
Single cell suspension from lymph nodes (LNs) of OT-II mice were obtained by gently mashing and passing through a 70 μm cell strainer. 1×105 bulk cells were co-cultured in round bottom 96-well plates together with 2×104 day 8 BM-DCs treated for 4 h with different stimuli as indicated, in the presence of 100 ng/ml OVA peptide327-339 (Charité-Berlin), 2 ng/ml porcine TGF-β1 (R&D Systems), 20 ng/ml rmIL-6 (ImmunoTools) for Th17 differentiation or 100 ng/ml OVA peptide327-339, 5 ng/ml IL-12 (Peprotech) in the case of Th1 polarization. After 5 days at 37°C and 7% CO2 in 200 μl of IMDM medium supplemented as RPMI, the cells were harvested, counted and re-stimulated at 1×106/ml in complete IMDM with 30 ng/ml PMA (Sigma-Aldrich) and 1 μg/ml Ionomycin (Sigma-Aldrich). After 1 h of stimulation 5 μg/ml Brefeldin (Sigma-Aldrich) and 2 μM Monensin (Sigma) were added without washing and further incubated for 5 hours. IL-17A and IFN-γ production were measured by flow cytometry staining as mentioned above.
In vitro Treg conversion assays
Naïve CD4+CD25- T cells were obtained from spleen and LN of OT-II mice. After erythrocyte lysis, total CD4+ cells were negatively selected using the CD4+ EasySep kit (StemCell Technologies) according to manufacturer’s instructions. Then, CD4+CD25- cells were acquired after magnetic isolation of CD4+ cells using the CD25 microBeads kit (Miltenyi). 2×104 naïve T cells were co-cultured in round bottom 96-well plates together with day 8 BM-DCs treated for 4 h with different stimuli as described above, in the presence of 100 ng/ml OVA peptide327-339 and 2 ng/ml porcine TGF-β1. The cells were cultured in 200 μl of complete RPMI medium at 37° C, 7% CO2. The conversion of naïve T cells towards iTreg was analyzed after 5 days by Foxp3 staining.
For polyclonal Treg conversion assay, naïve CD4+CD25- T cells were negatively selected as before from spleen and lymph nodes of C57BL/6 mice. 3–5×105 naïve T cells were cultured in 24-well plates pre-coated overnight at 4° C with 5 μg/ml of anti-CD3 antibody (clone 145.2C11) in the presence of 1 ng/ml porcine TGF-β1 and 500 U/ml rhIL-2 (Novartis) and with or without 10 μg/ml of recombinant CTLA-2α. The cells were cultured in 1 ml of complete RPMI medium at 37° C, 5% CO2. The conversion of naïve T cells towards iTreg was analyzed after 3 days by Foxp3 staining.
Knockdown of CTLA-2 with small interfering RNA (siRNA)
CTLA-2α and β expression in day 8 stimulated BM-DCs was blocked using four different duplex of siRNAs (customer made, Invitrogen-Life Technologies) targeting the CTLA-2 coding sequence. siRNAs were delivered into BM-DCs as previously described [77] with some modifications: BM-DCs (4×106) and siRNAs (final concentration 5 μM) were prepared each one in 100 μl of serum- and phenol red-free Opti-MEM® medium (Gibco). Then, BM-DCs were electroporated with the siRNAs in 4-mm electroporation cuvettes (Peqlab) at room temperature using the Gene Pulser Xcell (Bio-Rad). Pulse conditions were 400 V, 6 ms, 150 μF. Immediately after the pulse, an equivalent volume of complete RPMI medium was added and the electroporated cells were allow to stand for 1 h at 37° C, 7% CO2. The cells were washed with complete RPMI medium and treated for 4 h with diverse stimuli as indicated prior the co-culture with OT-II T cells for Th17, Th1 or Treg differentiation.
The sequences of siRNAs used to target CTLA-2α and β coding sequences at different sites were used alone or mixed (maintaining a final concentration of 5 μM) with similar results. A mouse scramble siRNA was used as a control (Ambion-Life Technologies). The efficiencies of knockdown were calculated by setting the scramble control as 100% and revealed 66±17.7 for CTLA-2a and 76±10.7 for CTLA-2b. (as % decrease). The sequences of siRNAs used were the following:
127s, 5’-AUAGUCUGCAUUGUGUGCCTT-3’;
127a, 5’-GGCACACAAUGCAGACUAUTT-3’;
202s, 5’-GGAUAAUGAGUGGAAAGAATT-3’;
202a, 5’- UUCUUUCCACUCAUUAUCCTT-3’;
213s, 5’-UUCGUCUUCCAUUCUUUCCTT-3’,
213a, 5’-GGAAAGAAUGGAAGACGAATT-3’;
495s, 5’-GCUUGACUGGUAACAAUAUTT-3’,
495a, 5’-AUAUUGUUACCAGUCAAGCTT-3’.
Production of recombinant CTLA-2α
Total RNA was extracted from CThi-treated DCs and first-strand synthesis of cDNA was performed using Moloney Murine Leukemia Virus Reverse Transcriptase, RNase H Minus, Point Mutant polymerase (Promega) according to manufacturer’s instructions. Phusion High-Fidelity polymerase (New England biolabs) was used for second strand cDNA synthesis and PCR amplification. The primers used were:
CTLA-2a-a, 5’-TTACCAGTCAAGCCACAGCTGTTACTCTGGC-3’;
NdeCTLA-2a-alphas, 5’-AACCATATGATGGTTTCTATCTGTGAACAGAAGCTGC-3’.
The PCR product was gel purified using GenElute Gel Extraction Kit (Sigma-Aldrich) according to the manufacturer’s instruction. The amplicon was cloned into the vector pSC-B-amp/kan (Stratagene) following manufacturer’s instructions and verified by nucleotide sequencing. The CTLA-2α encoding sequences were excised and inserted in the mammalian expression vector pcDNA3.1+ (Invitrogen) and into a bacterial expression vector following an N-terminal His tag (BioLegend). The resulting plasmids were sequenced.
Bacterial expression of recombinant CTLA-2α was induced with 1 mM isopropyl-β-D-thiogalactopyranoside (IPTG) when OD600 had reached 0.6 and expression was continued for ~3 hours at 37°C. Cell were lysed in 20 mM Tris (pH 7.5) and 300 mM NaCl. His-tagged CTLA-2α was purified by affinity chromatography using HisTrap FF columns (GE Healthcare) and eluted in, with 300 mM imidazole. The eluted fractions were dialyzed overnight at 4°C against a buffer composed of 20 mM Tris and 100 mM NaCl. The His-tag was removed by factor X cleavage and the CTLA-2α was purified by reverse His-tag purification. The protein was then further purified by Superdex 200 chromatography in PBS buffer. Endotoxin removal was performed using Cellufine ET-clean S (JNC Corporation) following manufacture's instruction.
Western blot of cathepsin L
Day 8 BM-DCs were treated for 10 h with different stimuli as indicated and the presence of CathL was evaluated by Western blot (SDS-PAGE). The cells were washed with PBS and resuspended in sodium acetate buffer (100 mM sodium acetate, 1 mM EDTA, 0.05% Brij35) at 107 cells/ml. Cell lysates were prepared by freeze-thaw cycles (liquid nitrogen-37° C, three times) and protein concentration was determined using a microplate bicinchoninic acid (BCA) protein assay kit (Thermo Scientific). 10 μg of protein were loaded per lane, separated by SDS-PAGE (12% polyacrylamide gels) and transferred to PVDF membranes. The membranes were blocked overnight at 4° C in 10% non-fat milk and for CathL detection a biotinylated anti-mCathL (R&D Systems) was used followed by incubation with HRP-conjugated streptavidin (Thermo Scientific). The membranes were developed using chemoluminescent HRP substrate (Millipore) and visualized using the FluorChem Q imager (Alpha Innotech). As loading control, the membranes were stripped by incubation with buffer containing 62.5 mM Tris HCl pH 6.7, 2% SDS and 0.8% (v/v) β-mercaptoethanol for 20 min at 70° C. The membranes were then washed with PBS plus 0.1% tween buffer, and blocked overnight at 4° C. β-actin was detected using anti-m-β-Actin (Sigma-Aldrich) as the primary antibody followed by incubation with biotinylated goat anti-mIgG1 (Abcam) and HRP-streptavidin. The membranes were developed and visualized as described above. The images were analyzed by densitometry using ImageJ v1.48 software [76] normalizing regarding β-actin control.
Experimental autoimmune encephalomyelitis (EAE)
Days 6, 8 and 10-BM-DCs were treated for 4 h with CTlo and cAMP in the presence (or not) of 40 μg/ml of MOG35-55 peptide (MEVGWYRSPFSRVVHLYRNGK; Charité-Berlin). 2×106 matured-DCs were injected intravenously into age- and sex-matched C57BL/6 mice at days -7, -5 and -3 before the induction of EAE. Control mice received no DC treatment. The disease was induced as described before [30] with some modifications. 20 μg of MOG35-55 peptide were injected subcutaneously in the rear flank in 50 μl of complete Freund’s adjuvant (Sigma-Aldrich) enriched with 10 mg/ml M. tuberculosis (H37 RA, Difco/BD). In addition, 100 ng/mouse of Pertussis toxin (List Biological Laboratories) were injected i.p. at days 0 and 2 of EAE induction. Mice were monitored daily for clinical disease symptoms according to the following scale: 0 = no disease; 1 = tail weakness; 2 = full tail paralysis; 3 = hind limp paralysis; 4 = hind limp and back paralysis; 5 = fore limp paralysis or moribund or death.
The frequency and activation state of Treg were measured in freshly isolated and in re-stimulated splenocytes of mice after 8 and 16 days of EAE induction. In the latter case, the cells were cultured for 5 days at 1×106/ml in BioWhittaker™HL-1™ (Lonza) free serum medium in the presence of 10 μg/ml MOG35-55 peptide. Additionally, splenocytes were re-stimulated for 3 days at 2×106/ml in BioWhittaker™HL-1™ with graded concentration of MOG35-55 peptide to measure IL-17 and IFN-γ production in the supernatants by ELISA (R&D Systems and BD Biosciences, respectively). The supernatants were collected and centrifuged at 10,000×g for 10 min prior to measurement.
Statistical analysis
Data are presented as the mean ± SD, except for the EAE score, where SEM is displayed. The data were analyzed utilizing Student t-test or One-way Anova using Dunnett post-test using Graph Pad Prism™ software. Significance level was defined as *p<0.05, **p<0.01, *** p<0.001.
Acknowledgments
We thank Eliana Ribechini, Sarah Potter and Iris Gonzales Leal for their help with experiments, Carsten Wiethe for his help in generating the vector and the Graduate School of Life Sciences (GSLS), Heidrun Moll and Thomas Hünig for their support of the project. We also thank Thomas Herrmann for generating a fusion protein of rCTLA-2α bound to an IgG molecule.
Abbreviations
- CT
cholera toxin
- DC
dendritic cell
- iTreg
CD4+CD25+Foxp3+ T cells
- Ctsl
cathepsin L
- MS
multiple sclerosis
- EAE
experimental autoimmune encephalomyelitis
Data Availability
All microarray files are available from the GEO database (accession number GSE79274).
Funding Statement
This publication was funded by the German Research Foundation (DFG) and the University of Wuerzburg in the funding programme Open Access Publishing. The Stibet program of the DAAD and the collaborative research centre TR52 of the DFG provided support in the form of salaries for author CSV, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of this author are articulated in the ‘author contributions’ section.
References
- 1.Steinman RM, Hawiger D, Nussenzweig MC (2003) Tolerogenic dendritic cells. Annu Rev Immunol 21: 685–711. doi: 10.1146/annurev.immunol.21.120601.141040 [DOI] [PubMed] [Google Scholar]
- 2.Banchereau J, Palucka AK (2005) Dendritic cells as therapeutic vaccines against cancer. Nat Rev Immunol 5: 296–306. doi: 10.1038/nri1592 [DOI] [PubMed] [Google Scholar]
- 3.Akira S, Takeda K (2004) Functions of toll-like receptors: lessons from KO mice. C R Biol 327: 581–589. [DOI] [PubMed] [Google Scholar]
- 4.Zhu J, Yamane H, Paul WE (2010) Differentiation of effector CD4 T cell populations (*). Annu Rev Immunol 28: 445–489. doi: 10.1146/annurev-immunol-030409-101212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Min B, Paul WE (2008) Basophils: in the spotlight at last. Nat Immunol 9: 223–225. doi: 10.1038/ni0308-223 [DOI] [PubMed] [Google Scholar]
- 6.Phythian-Adams AT, Cook PC, Lundie RJ, Jones LH, Smith KA, et al. (2010) CD11c depletion severely disrupts Th2 induction and development in vivo. J Exp Med 207: 2089–2096. doi: 10.1084/jem.20100734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kapsenberg ML (2003) Dendritic-cell control of pathogen-driven T-cell polarization. Nat Rev Immunol 3: 984–993. doi: 10.1038/nri1246 [DOI] [PubMed] [Google Scholar]
- 8.Moser M, Rock KM (2000) Dendritc cell regulation of TH1-TH2 development. Nat Immunol 1: 199–205. doi: 10.1038/79734 [DOI] [PubMed] [Google Scholar]
- 9.Kalinski P, Hilkens CM, Wierenga EA, Kapsenberg ML (1999) T-cell priming by type-1 and type-2 polarized dendritic cells: the concept of a third signal. Immunol Today 20: 561–567. [DOI] [PubMed] [Google Scholar]
- 10.Ohkura N, Kitagawa Y, Sakaguchi S (2013) Development and maintenance of regulatory T cells. Immunity 38: 414–423. doi: 10.1016/j.immuni.2013.03.002 [DOI] [PubMed] [Google Scholar]
- 11.Wing K, Sakaguchi S (2010) Regulatory T cells exert checks and balances on self tolerance and autoimmunity. Nat Immunol 11: 7–13. doi: 10.1038/ni.1818 [DOI] [PubMed] [Google Scholar]
- 12.Gregori S, Goudy KS, Roncarolo MG (2012) The cellular and molecular mechanisms of immuno-suppression by human type 1 regulatory T cells. Front Immunol 3: 30 doi: 10.3389/fimmu.2012.00030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.O'Garra A, Vieira PL, Vieira P, Goldfeld AE (2004) IL-10-producing and naturally occurring CD4+ Tregs: limiting collateral damage. J Clin Invest 114: 1372–1378. doi: 10.1172/JCI23215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Garra A, Vieira P (2007) T(H)1 cells control themselves by producing interleukin-10. Nat Rev Immunol 7: 425–428. doi: 10.1038/nri2097 [DOI] [PubMed] [Google Scholar]
- 15.Pletinckx K, Döhler A, Pavlovic V, Lutz MB (2011) Role of dendritic cell maturity/costimulation for generation, homeostasis and suppressive activity of regulatory T cells. Frontiers in Immunology 2 (article 39) 1–15. doi: 10.3389/fimmu.2011.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Littman DR, Rudensky AY (2010) Th17 and regulatory T cells in mediating and restraining inflammation. Cell 140: 845–858. doi: 10.1016/j.cell.2010.02.021 [DOI] [PubMed] [Google Scholar]
- 17.Pletinckx K, Stijlemans B, Pavlovic V, Laube R, Brandl C, et al. (2011) Similar inflammatory DC maturation signatures induced by TNF or Trypanosoma brucei antigens instruct default Th2-cell responses. Eur J Immunol 41: 3479–3494. doi: 10.1002/eji.201141631 [DOI] [PubMed] [Google Scholar]
- 18.Marinaro M, Staats HF, Hiroi T, Jackson RJ, Coste M, et al. (1995) Mucosal adjuvant effect of cholera toxin in mice results from induction of T helper 2 (Th2) cells and IL-4. J Immunol 155: 4621–4629. [PubMed] [Google Scholar]
- 19.Su SB, Silver PB, Wang P, Chan CC, Caspi RR (2004) Cholera toxin prevents Th1-mediated autoimmune disease by inducing immune deviation. J Immunol 173: 755–761. [DOI] [PubMed] [Google Scholar]
- 20.Gagliardi MC, Sallusto F, Marinaro M, Langenkamp A, Lanzavecchia A, et al. (2000) Cholera toxin induces maturation of human dendritic cells and licences them for Th2 priming. Eur J Immunol 30: 2394–2403. doi: 10.1002/1521-4141(2000)30:8<2394::AID-IMMU2394>3.0.CO;2-Y [DOI] [PubMed] [Google Scholar]
- 21.Lee JB, Jang JE, Song MK, Chang J (2009) Intranasal delivery of cholera toxin induces th17-dominated T-cell response to bystander antigens. PLoS One 4: e5190 doi: 10.1371/journal.pone.0005190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Datta SK, Sabet M, Nguyen KP, Valdez PA, Gonzalez-Navajas JM, et al. (2010) Mucosal adjuvant activity of cholera toxin requires Th17 cells and protects against inhalation anthrax. Proc Natl Acad Sci U S A 107: 10638–10643. doi: 10.1073/pnas.1002348107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lavelle EC, McNeela E, Armstrong ME, Leavy O, Higgins SC, et al. (2003) Cholera toxin promotes the induction of regulatory T cells specific for bystander antigens by modulating dendritic cell activation. J Immunol 171: 2384–2392. [DOI] [PubMed] [Google Scholar]
- 24.Braun MC, He J, Wu CY, Kelsall BL (1999) Cholera toxin suppresses interleukin (IL)-12 production and IL-12 receptor beta1 and beta2 chain expression. J Exp Med 189: 541–552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sun JB, Czerkinsky C, Holmgren J (2010) Mucosally induced immunological tolerance, regulatory T cells and the adjuvant effect by cholera toxin B subunit. Scand J Immunol 71: 1–11. doi: 10.1111/j.1365-3083.2009.02321.x [DOI] [PubMed] [Google Scholar]
- 26.Stanford M, Whittall T, Bergmeier LA, Lindblad M, Lundin S, et al. (2004) Oral tolerization with peptide 336–351 linked to cholera toxin B subunit in preventing relapses of uveitis in Behcet's disease. Clin Exp Immunol 137: 201–208. doi: 10.1111/j.1365-2249.2004.02520.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pletinckx K, Dohler A, Pavlovic V, Lutz MB (2011) Role of dendritic cell maturity/costimulation for generation, homeostasis, and suppressive activity of regulatory T cells. Front Immunol 2: 39 doi: 10.3389/fimmu.2011.00039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lutz MB, Schuler G (2002) Immature, semi-mature and fully mature dendritic cells: which signals induce tolerance or immunity? Trends Immunol 23: 445–449. [DOI] [PubMed] [Google Scholar]
- 29.Lutz MB (2012) Therapeutic potential of semi-mature dendritic cells for tolerance induction. Front Immunol 3: 123 doi: 10.3389/fimmu.2012.00123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Menges M, Rossner S, Voigtlander C, Schindler H, Kukutsch NA, et al. (2002) Repetitive injections of dendritic cells matured with tumor necrosis factor alpha induce antigen-specific protection of mice from autoimmunity. J Exp Med 195: 15–21. doi: 10.1084/jem.20011341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Denizot F, Brunet JF, Roustan P, Harper K, Suzan M, et al. (1989) Novel structures CTLA-2 alpha and CTLA-2 beta expressed in mouse activated T cells and mast cells and homologous to cysteine proteinase proregions. European journal of immunology 19: 631–635. doi: 10.1002/eji.1830190409 [DOI] [PubMed] [Google Scholar]
- 32.Brunet JF, Denizot F, Golstein P (1988) A differential molecular biology search for genes preferentially expressed in functional T lymphocytes: the CTLA genes. Immunol Rev 103: 21–36. [DOI] [PubMed] [Google Scholar]
- 33.Delaria K, Fiorentino L, Wallace L, Tamburini P, Brownell E, et al. (1994) Inhibition of cathepsin L-like cysteine proteases by cytotoxic T-lymphocyte antigen-2 beta. J Biol Chem 269: 25172–25177. [PubMed] [Google Scholar]
- 34.Kurata M, Hirata M, Watabe S, Miyake M, Takahashi SY, et al. (2003) Expression, purification, and inhibitory activities of mouse cytotoxic T-lymphocyte antigen-2alpha. Protein Expr Purif 32: 119–125. doi: 10.1016/S1046-5928(03)00222-5 [DOI] [PubMed] [Google Scholar]
- 35.Zhang L, Yun H, Murray F, Lu R, Wang L, et al. (2011) Cytotoxic T lymphocyte antigen-2 alpha induces apoptosis of murine T-lymphoma cells and cardiac fibroblasts and is regulated by cAMP/PKA. Cell Signal 23: 1611–1616. doi: 10.1016/j.cellsig.2011.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Luziga C, Nakamura O, Deshapriya RM, Usui M, Miyaji M, et al. (2008) Dendritic and axonal localization of cytotoxic T-lymphocyte antigen-2 alpha protein in mouse brain. Brain Res 1204: 40–52. doi: 10.1016/j.brainres.2008.01.067 [DOI] [PubMed] [Google Scholar]
- 37.Campo M, Rice E, Kasik J (1996) There is an increase in expression of the cytotoxic T-lymphocyte antigen-2 alpha gene during pregnancy. Am J Obstet Gynecol 174: 1605–1607. [DOI] [PubMed] [Google Scholar]
- 38.Deussing J, Kouadio M, Rehman S, Werber I, Schwinde A, et al. (2002) Identification and characterization of a dense cluster of placenta-specific cysteine peptidase genes and related genes on mouse chromosome 13. Genomics 79: 225–240. doi: 10.1006/geno.2002.6696 [DOI] [PubMed] [Google Scholar]
- 39.Sugita S, Horie S, Nakamura O, Futagami Y, Takase H, et al. (2008) Retinal Pigment Epithelium-Derived CTLA-2α Induces TGFβ-Producing T Regulatory Cells. The Journal of Immunology 181: 7525–7536. [DOI] [PubMed] [Google Scholar]
- 40.Sugita S, Yamada Y, Horie S, Nakamura O, Ishidoh K, et al. (2011) Induction of T regulatory cells by cytotoxic T-lymphocyte antigen-2α on corneal endothelial cells. Invest Ophthalmol Vis Sci 52: 2598–2605. doi: 10.1167/iovs.10-6322 [DOI] [PubMed] [Google Scholar]
- 41.Sugita S, Horie S, Nakamura O, Maruyama K, Takase H, et al. (2009) Acquisition of T regulatory function in cathepsin L-inhibited T cells by eye-derived CTLA-2alpha during inflammatory conditions. Journal of immunology 183: 5013–5022. [DOI] [PubMed] [Google Scholar]
- 42.Lee J-B, Jang J-E, Song MK, Chang J (2009) Intranasal delivery of cholera toxin induces th17-dominated T-cell response to bystander antigens. PloS one 4: e5190 doi: 10.1371/journal.pone.0005190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Haan LD, Hirst TR (2004) Cholera toxin: A paradigm for multi-functional engagement of cellular mechanisms (Review). Mol Membr Biol 21: 77–92. doi: 10.1080/09687680410001663267 [DOI] [PubMed] [Google Scholar]
- 44.Korn T, Bettelli E, Oukka M, Kuchroo VK (2009) IL-17 and Th17 Cells. Annual review of immunology 27: 485–517. doi: 10.1146/annurev.immunol.021908.132710 [DOI] [PubMed] [Google Scholar]
- 45.Heufler C, Koch F, Stanzl U, Topar G, Wysocka M, et al. (1996) Interleukin-12 is produced by dendritic cells and mediates T helper 1 development as well as interferon-gamma production by T helper 1 cells. Eur J Immunol 26: 659–668. doi: 10.1002/eji.1830260323 [DOI] [PubMed] [Google Scholar]
- 46.O'Garra A, Gabryšová L, Spits H (2011) Quantitative events determine the differentiation and function of helper T cells. Nat Immunol 12: 288–294. doi: 10.1038/ni.2003 [DOI] [PubMed] [Google Scholar]
- 47.Lutz MB (2013) How quantitative differences in dendritic cell maturation can direct Th1/Th2-cell polarization. Oncoimmunology 2: e22796 doi: 10.4161/onci.22796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van Panhuys N, Klauschen F, Germain RN (2014) T-cell-receptor-dependent signal intensity dominantly controls CD4(+) T cell polarization In Vivo. Immunity 41: 63–74. doi: 10.1016/j.immuni.2014.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Langenkamp A, Messi M, Lanzavecchia A, Sallusto F (2000) Kinetics of dendritic cell activation: impact on priming of TH1, TH2 and nonpolarized T cells. Nat Immunol 1: 311–316. doi: 10.1038/79758 [DOI] [PubMed] [Google Scholar]
- 50.Iezzi G, Scotet E, Scheidegger D, Lanzavecchia A (1999) The interplay between the duration of TCR and cytokine signaling determines T cell polarization. Eur J Immunol 29: 4092–4101. doi: 10.1002/(SICI)1521-4141(199912)29:12<4092::AID-IMMU4092>3.0.CO;2-A [DOI] [PubMed] [Google Scholar]
- 51.Yoshimoto T, Yasuda K, Tanaka H, Nakahira M, Imai Y, et al. (2009) Basophils contribute to T(H)2-IgE responses in vivo via IL-4 production and presentation of peptide-MHC class II complexes to CD4+ T cells. Nat Immunol 10: 706–712. doi: 10.1038/ni.1737 [DOI] [PubMed] [Google Scholar]
- 52.Liang HE, Reinhardt RL, Bando JK, Sullivan BM, Ho IC, et al. (2012) Divergent expression patterns of IL-4 and IL-13 define unique functions in allergic immunity. Nat Immunol 13: 58–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Roediger B, Weninger W (2015) Group 2 innate lymphoid cells in the regulation of immune responses. Adv Immunol 125: 111–154. doi: 10.1016/bs.ai.2014.09.004 [DOI] [PubMed] [Google Scholar]
- 54.Weaver CT, Hatton RD (2009) Interplay between the TH17 and TReg cell lineages: a (co-)evolutionary perspective. Nat Rev Immunol 9: 883–889. doi: 10.1038/nri2660 [DOI] [PubMed] [Google Scholar]
- 55.Thomson AW, Turnquist HR, Zahorchak AF, Raimondi G (2009) Tolerogenic dendritic cell-regulatory T-cell interaction and the promotion of transplant tolerance. Transplantation 87: S86–90. doi: 10.1097/TP.0b013e3181a2dcec [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hilkens CMU, Isaacs JD, Thomson AW (2010) Development of dendritic cell-based immunotherapy for autoimmunity. Int Rev Immunol 29: 156–183. doi: 10.3109/08830180903281193 [DOI] [PubMed] [Google Scholar]
- 57.Brömme D, Li Z, Barnes M, Mehler E (1999) Human cathepsin V functional expression, tissue distribution, electrostatic surface potential, enzymatic characterization, and chromosomal localization. Biochemistry 38: 2377–2385. doi: 10.1021/bi982175f [DOI] [PubMed] [Google Scholar]
- 58.Tolosa E, Li W, Yasuda Y, Wienhold W, Denzin LK, et al. (2003) Cathepsin V is involved in the degradation of invariant chain in human thymus and is overexpressed in myasthenia gravis. J Clin Invest 112: 517–526. doi: 10.1172/JCI18028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Azukizawa H, Dohler A, Kanazawa N, Nayak A, Lipp M, et al. (2011) Steady state migratory RelB+ langerin+ dermal dendritic cells mediate peripheral induction of antigen-specific CD4+ CD25+ Foxp3+ regulatory T cells. Eur J Immunol 41: 1420–1434. doi: 10.1002/eji.201040930 [DOI] [PubMed] [Google Scholar]
- 60.Abe Y, Minegishi T, Leung PC (2004) Activin receptor signaling. Growth Factors 22: 105–110. [DOI] [PubMed] [Google Scholar]
- 61.Todorovic V, Rifkin DB (2012) LTBPs, more than just an escort service. J Cell Biochem 113: 410–418. doi: 10.1002/jcb.23385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shi M, Zhu J, Wang R, Chen X, Mi L, et al. (2011) Latent TGF-β structure and activation. Nature 474: 343–349. doi: 10.1038/nature10152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Lyons RM, Keski-Oja J, Moses HL (1988) Proteolytic activation of latent transforming growth factor-beta from fibroblast-conditioned medium. J Cell Biol 106: 1659–1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Somanna A, Mundodi V, Gedamu L (2002) Functional analysis of cathepsin B-like cysteine proteases from Leishmania donovani complex. Evidence for the activation of latent transforming growth factor beta. J Biol Chem 277: 25305–25312. doi: 10.1074/jbc.M203034200 [DOI] [PubMed] [Google Scholar]
- 65.Kasabova M, Joulin-Giet A, Lecaille F, Gilmore BF, Marchand-Adam S, et al. (2014) Regulation of TGF-beta1-driven differentiation of human lung fibroblasts: emerging roles of cathepsin B and cystatin C. J Biol Chem 289: 16239–16251. doi: 10.1074/jbc.M113.542407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wille A, Gerber A, Heimburg A, Reisenauer A, Peters C, et al. (2004) Cathepsin L is involved in cathepsin D processing and regulation of apoptosis in A549 human lung epithelial cells. Biol Chem 385: 665–670. doi: 10.1515/BC.2004.082 [DOI] [PubMed] [Google Scholar]
- 67.Apte SH, Redmond AM, Groves PL, Schussek S, Pattinson DJ, et al. (2013) Subcutaneous cholera toxin exposure induces potent CD103⁺ dermal dendritic cell activation and migration. Eur J Immunol 43: 2707–2717. doi: 10.1002/eji.201343475 [DOI] [PubMed] [Google Scholar]
- 68.Olvera-Gomez I, Hamilton SE, Xiao Z, Guimaraes CP, Ploegh HL, et al. (2012) Cholera toxin activates nonconventional adjuvant pathways that induce protective CD8 T-cell responses after epicutaneous vaccination. Proc Natl Acad Sci USA 109: 2072–2077. doi: 10.1073/pnas.1105771109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Gustafsson T, Hua YJ, Dahlgren MW, Livingston M, Johansson-Lindbom B, et al. (2013) Direct interaction between cholera toxin and dendritic cells is required for oral adjuvant activity. Eur J Immunol 43: 1779–1788. doi: 10.1002/eji.201242867 [DOI] [PubMed] [Google Scholar]
- 70.Yura M, Takahashi I, Terawaki S, Hiroi T, Kweon MN, et al. (2001) Nasal administration of cholera toxin (CT) suppresses clinical signs of experimental autoimmune encephalomyelitis (EAE). Vaccine 20: 134–139. [DOI] [PubMed] [Google Scholar]
- 71.Grdic D, Ekman L, Schön K, Lindgren K, Mattsson J, et al. (2005) Splenic marginal zone dendritic cells mediate the cholera toxin adjuvant effect: dependence on the ADP-ribosyltransferase activity of the holotoxin. J Immunol 175: 5192–5202. [DOI] [PubMed] [Google Scholar]
- 72.Rothenbacher FP, Zhu J (2014) Efficient responses to host and bacterial signals during Vibrio cholerae colonization. Gut Microbes 5: 120–128. doi: 10.4161/gmic.26944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Roth W, Deussing J, Botchkarev VA, Pauly-Evers M, Saftig P, et al. (2000) Cathepsin L deficiency as molecular defect of furless: hyperproliferation of keratinocytes and pertubation of hair follicle cycling. FASEB J 14: 2075–2086. doi: 10.1096/fj.99-0970com [DOI] [PubMed] [Google Scholar]
- 74.Lutz MB, Kukutsch N, Ogilvie ALJ, Rößner S, Koch F, et al. (1999) An advanced culture method for generating large quantities of highly pure dendritic cells from mouse bone marrow. Journal of Immunological Methods 223: 77–92. [DOI] [PubMed] [Google Scholar]
- 75.Zal T, Volkmann a, Stockinger B (1994) Mechanisms of tolerance induction in major histocompatibility complex class II-restricted T cells specific for a blood-borne self-antigen. The Journal of experimental medicine 180: 2089–2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Abràmoff MD, Magalhães PJ, Ram SJ (2004) Image processing with imageJ. Biophotonics International 11: 36–41. [Google Scholar]
- 77.Van Meirvenne S, Straetman L, Heirman C, Dullaers M, De Greef C, et al. (2002) Efficient genetic modification of murine dendritic cells by electroporation with mRNA. Cancer gene therapy 9: 787–797. doi: 10.1038/sj.cgt.7700499 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All microarray files are available from the GEO database (accession number GSE79274).