Abstract
Cervical hemorrhage due to non-traumatic, spontaneous rupture of the thyroid artery is rare, which usually results from arterial abnormalities or parathyroid or thyroid disorders. This report describes a 72-year-old woman who presented with a sore throat and slight neck swelling. Computed tomography (CT) revealed a large hematoma in the neck and mediastinum, due to extravasation from the major branch of the left superior thyroid artery. A follow-up CT the next day demonstrated that the extravasation had resolved. Subsequent surgery revealed both parathyroid adenoma and multinodular goiter in the resected thyroid gland. A transient elevation of parathyroid hormone occurred immediately after the hemorrhage, suggesting that the hemorrhage may have been related to the parathyroid adenoma. However, ruptured thyroid arteries were not observed on histopathological examination of the resected tissue.
Keywords: Cervical hemorrhage, thyroid artery, parathyroid adenoma, multinodular goiter, computed tomography
Introduction
Non-traumatic rupture of the thyroid arteries is extremely rare (1–9). Several underlying disorders have been described in previous reports of spontaneous thyroid artery rupture, including thyroid artery aneurysm (2,4,6,7,9), parathyroid adenoma (8), and adenomatous thyroid nodule/multinodular goiter (1,9). Spontaneous rupture of the thyroid artery in the absence of an underlying condition has also been reported (3,5). Here, a case of non-traumatic rupture of the major branch of the superior thyroid artery clearly depicted by enhanced neck computed tomography (CT) is reported. A large hematoma was observed around the thyroid gland and in the mediastinum, and clear extravasation from the ruptured thyroid artery was observed on the initial enhanced CT, which was not observed on follow-up enhanced CT the next day.
Case report
A 72-year-old Japanese woman visited a local hospital with a chief complaint of sore throat and slight neck swelling. Plain and enhanced neck CT depicted a large hematoma spreading through the retropharyngeal space, around the thyroid gland (particularly around the left lobe), and in the mediastinum (Fig. 1). Several non-enhanced, low-density areas were observed in the enlarged left lobe of the thyroid gland (Fig. 1); however, a clear hemorrhage or hematoma was not observed in the gland. On enhanced CT, extravasation from the major branch of the left superior thyroid artery was observed around the superior margin of the left lobe (Figs. 1 and 2) and was considered to be responsible for the hemorrhage/hematoma. Based on the diagnosis of arterial hemorrhage around the thyroid gland, the patient was transferred to our hospital for further treatment. Upon admission, her symptoms were stable and she did not complain of dyspnea or severe neck pain. Follow-up enhanced CT and CT angiography (CTA) on the following day did not demonstrate either an aneurysm or the extravasation observed on the initial CT (Fig. 3). Thus, interventional treatment was not pursued. The patient’s serum level of intact parathyroid hormone (PTH) was elevated (>1500 pg/mL) after admission. However, her neck swelling gradually improved and she was discharged one week later. The hematoma in the neck and mediastinum was completely absorbed on follow-up CT four weeks later. Approximately ten weeks after the onset of symptoms, she underwent hemi-thyroidectomy (left lobe). Pathological examination revealed multinodular goiter and parathyroid adenoma in the resected left lobe (Fig. 4). Small hemosiderin deposits were observed in the specimen; however, obvious hematomas were not observed in the parathyroid adenoma or multinodular goiter. No abnormal thin vessel walls or aneurysms were observed in the thyroid arteries; thus, the true point of rupture of the superior thyroid artery was not clear. The patient’s postoperative clinical course was uneventful.
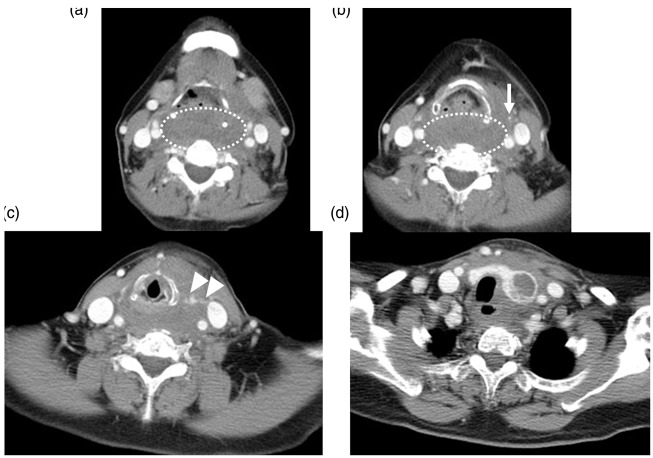
Fig. 1.
Initial enhanced CT. A large hematoma was observed in the retropharyngeal space (dashed oval (a, b)). The left superior thyroid artery is clearly depicted (arrow in (b)), which connects to an extravasation (arrowheads in (c)). The left lobe of the thyroid gland was enlarged and contained unenhanced low-density areas (d). Hematomas were also observed around the left lobe of the thyroid and in the upper mediastinum (d).
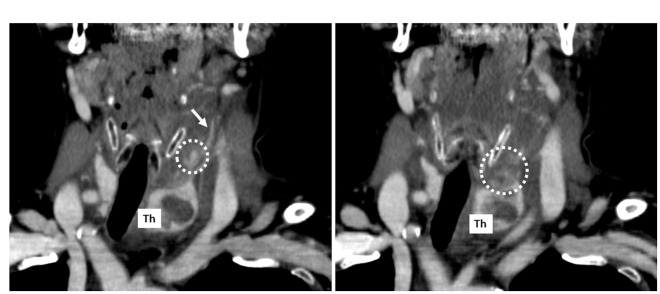
Fig. 2.
Reconstructed coronal images of the initial CT. Connecting the left superior thyroid artery (arrow in (a)), multiple enhanced lesions are observed (dashed oval (a, b)) that are concordant to the extravasations on axial images. Th, thyroid gland (left lobe).
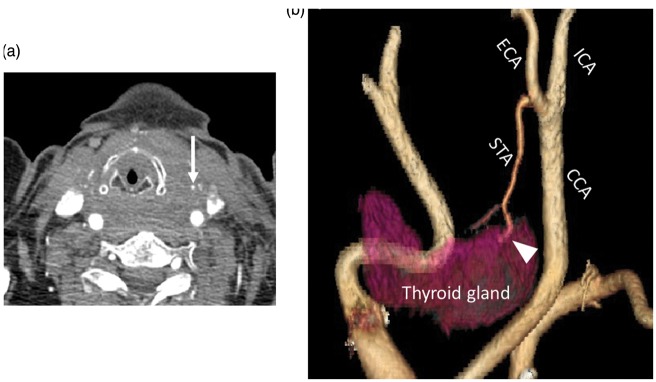
Fig. 3.
Follow-up CT and CTA the following day. The extravasation that was observed on the initial CT disappeared and an apparently normal left superior thyroid was observed (arrow in (a)). On CTA, no aneurysm or dilation was observed around the suspected rupture point (arrowhead in (b)). ICA, internal carotid artery; ECA, external carotid artery; CCA, common carotid artery; STA, superior thyroid artery.
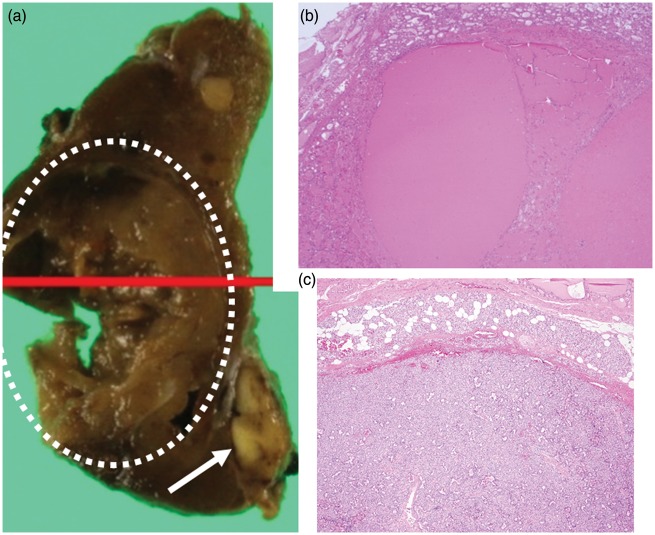
Fig. 4.
Pathological findings of the resected left lobe of the thyroid. On gross pathology, the resected lobe contained multinodular goiter with necrotic/cystic components (dashed oval in (a)). An enlarged parathyroid gland was also observed (arrow in (a)). Microscopically (hematoxylin and eosin, ×40), several follicles were found in the multinodular goiter (b). The enlarged parathyroid gland was diagnosed as an adenoma (c).
Discussion
In the present case, a major branch of the left superior thyroid artery spontaneously ruptured, resulting in a large hematoma spreading through the neck and the mediastinum. Although clear extravasation was observed in the initial enhanced CT, no extravasation was observed on a follow-up CT the next day and the artery did not re-rupture prior to surgical resection. While interventional radiology or emergency surgery are used to treat patients with sudden cervical hemorrhage causing central airway stenosis and dyspnea (1,3,6,7), patients in stable condition may be treated conservatively or with planned surgical interventions (2,4,5). It is unclear if the conservative treatment strategy used in this case can be applied to similar patients. However, our case suggests that spontaneous rupture of the thyroid arteries can occur even without aneurysm and that stable clinical conditions and the absence of aneurysm/continuous arterial bleeding are factors that may help determine treatment options.
While spontaneous rupture of the inferior thyroid artery has previously been reported (4–7), there are limited reports of spontaneous rupture of the superior thyroid artery (1–3). Amadei et al. reported a case of spontaneous rupture of a branch of the superior thyroid artery, which supplied a hyperplastic adenomatous thyroid nodule (1). Kieu et al. reported a case of a ruptured aneurysm of the superior thyroid artery (2) and Stenner et al. reported the spontaneous rupture of the superior thyroid artery in the absence of thyroid gland abnormalities (3). To the best of our knowledge, the present case is the fourth report of a spontaneous rupture of the superior thyroid artery confirmed by enhanced neck CT. Interestingly, all four cases occurred in the context of different backgrounds/abnormalities of the superior thyroid artery or thyroid gland. It is unclear why fewer cases of superior thyroid artery rupture have been reported than cases of inferior thyroid artery rupture. More case reports may help determine if the superior thyroid artery is more robust than the inferior thyroid artery, and therefore less susceptible to spontaneous rupture.
In the present case, the final pathological diagnosis was co-existing multinodular goiter and parathyroid adenoma. Although spontaneous hemorrhage (rupture) of each of these lesions has been reported to cause cervical hematoma (1,8–10), reports describing spontaneous hemorrhage from parathyroid adenoma are more common than those reporting hemorrhage with multinodular goiter or other thyroid abnormalities. In our case, an elevation of intact PTH was observed around the time of hemorrhage, suggesting that the ruptured superior thyroid artery may have been related to the parathyroid adenoma rather than the multinodular goiter.
In conclusion, this spontaneous rupture of a branch of the superior thyroid artery caused temporary extravasation shown on enhanced CT. Parathyroid adenoma and multinodular goiter were found in the resected thyroid specimen, without obvious arterial abnormalities.
Acknowledgments
The authors thank Dr. Fumikiyo Ganaha (Okinawa Prefectural Nanbu Medical Center) and Dr. Joichi Heianna (University of the Ryukyus Hospital) for their important suggestions.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Amadei EM, Benedettini L, Piccin O. Two cases of cervical hemorrhage with upper airway obstruction: a life-threatening condition. Case Rep Med 2014; 2014: 674176–674176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kieu V, Tassone P, Hobbs CG. Successful conservative management of the spontaneous rupture of a superior thyroid artery aneurysm. ANZ J Surg 2012; 82: 371–372. [DOI] [PubMed] [Google Scholar]
- 3.Stenner M, Helmstaedter V, Spuentrup E, et al. Cervical hemorrhage due to spontaneous rupture of the superior thyroid artery: case report and review of the literature. Head Neck 2010; 32: 1277–1281. [DOI] [PubMed] [Google Scholar]
- 4.Coskun ZO, Yavaşi Ö, Durakoglugil T, et al. Acute airway compromise due to ruptured inferior thyroid artery aneurysm. Am J Emerg Med 2015; 33: 1115.e1–3. [DOI] [PubMed] [Google Scholar]
- 5.Hoetzenecker K, Töpker M, Klepetko W, et al. Spontaneous rupture of the inferior thyroid artery resulting in mediastinal hematoma. Interact Cardiovasc Thorac Surg 2010; 11: 209–210. [DOI] [PubMed] [Google Scholar]
- 6.Garrett HE, Heidepriem RW, Broadbent LP. Ruptured aneurysm of the inferior thyroid artery: repair with coil embolization. J Vasc Surg 2005; 42: 1226–1229. [DOI] [PubMed] [Google Scholar]
- 7.Kos X, Henroteaux D, Dondelinger RF. Embolization of a ruptured aneurysm of the inferior thyroid artery. Eur Radiol 2001; 11: 1285–1286. [DOI] [PubMed] [Google Scholar]
- 8.Ilyicheva E. Spontaneous cervical-mediastinal hematoma caused by hemorrhage into parathyroid adenoma: A clinical case. Int J Surg Case Rep 2015; 6C: 214–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chang CC, Chou YH, Tiu CM, et al. Spontaneous rupture with pseudoaneurysm formation in a nodular goiter presenting as a large neck mass. J Clin Ultrasound 2007; 35: 518–520. [DOI] [PubMed] [Google Scholar]
- 10.Tonerini M, Orsitto E, Fratini L, et al. Cervical and mediastinal hematoma: presentation of an asymptomatic cervical parathyroid adenoma: case report and literature review. Emerg Radiol 2004; 10: 213–215. [DOI] [PubMed] [Google Scholar]