Abstract
Extragastrointestinal stromal tumors (EGISTs) are rare tumors that arise outside the digestive tract. We report a case of an EGIST arising in the subcutaneous tissue of the abdominal wall, which at this site can often be misdiagnosed as dermatofibrosarcoma protuberans. The tumor was surgically resected from a 72-year-old male Chinese Han patient, and pathological examination revealed spindle-shaped tumor cells with eosinophilic cytoplasm and an oval nucleus. Immunohistochemically, the tumor cells showed strong cytoplasmic positivity for CD34, c-KIT (CD117), and DOG1. Tests for activating mutations of GISTs showed that the tumor cells carried an in-frame deletion (NP_000213.1:p.Lys550_Gln556del) in exon 11 of c-KIT (CD117). Thus, an EGIST should be considered in patients with abdominal subcutaneous tumors with an epithelioid, spindle-shaped, or mixed morphology. Immunohistochemistry of c-KIT (CD117) and DOG1 and genetic testing for activating mutations are recommended to aid in the differential diagnosis of subcutaneous tumors. In short, although EGISTs are rare in the abdominal subcutaneous tissue, pathologists must be aware of their possibility.
Keywords: Extragastrointestinal stromal tumor, abdominal subcutaneous, dermatofibrosarcoma protuberans, CD34, c-KIT (CD117), DOG1, activating mutation
Introduction
Extragastrointestinal stromal tumors (EGISTs) are morphologically, histologically, and immunophenotypically similar to gastrointestinal stromal tumors (GISTs).1 GISTs are the most common mesenchymal malignancy in the digestive tract.2 However, EGISTs are a rarely reported group of tumors that arise outside the digestive tract, such as from the mesentery, omentum, and retroperitoneum.3,4 EGISTs have also been reported to arise from the pancreas, pelvic cavity, prostate, urinary bladder, and vaginal wall.5–11 To the best of our knowledge, very few EGISTs have been reported in the abdominal wall,12,13 and those in the abdominal subcutaneous tissue are even rarer. Only one case of extra-abdominal subcutaneous metastasis of a GIST has been been reported.14 Dermatofibrosarcoma protuberans (DFSP) is a locally infiltrative tumor of intermediate malignancy with high expression of CD34, and most occur on the trunk, proximal extremities, and head and neck region.15,16 EGISTs in the abdominal subcutaneous tissue are similar to soft tissue sarcomas and DFSPs. Thus, an abdominal subcutaneous soft tissue tumor could easily be misdiagnosed as DFSP. Common immunohistochemical markers used in the differential diagnosis of soft tissue tumors include CD34, alpha smooth muscle actin (SMA), desmin, and S100 protein. In the present case, we achieved a reliable diagnosis of EGIST by adding immunohistochemical staining and genetic testing for c-KIT (CD117) and DOG1.
Case report
A 72-year-old male Chinese Han patient was hospitalized because of prostatic hyperplasia. On admission, the patient had no obvious cause progressive dysuria, gross hematuria, or urinary pain. Physical examination revealed a hard, mobile, painless mass of approximately 6 cm in diameter occupying the abdomen. A computed tomography scan revealed a 6- × 5- × 3-cm heterogeneous mass with a clear boundary in the abdominal wall (Figure 1(a)). Surgical resection of the tumor from the abdominal wall was performed with a clear margin. The patient had a history of surgical repair of a gastric perforation line the stomach, line between the waist dish outstanding lamina decompression, and all the left side of the great saphenous vein high ligation. He had also undergone resection of an abdominal neurilemmoma 3 years previously in the same location. This study was approved by the local institutional review board, and written informed consent was obtained from the patient and family.
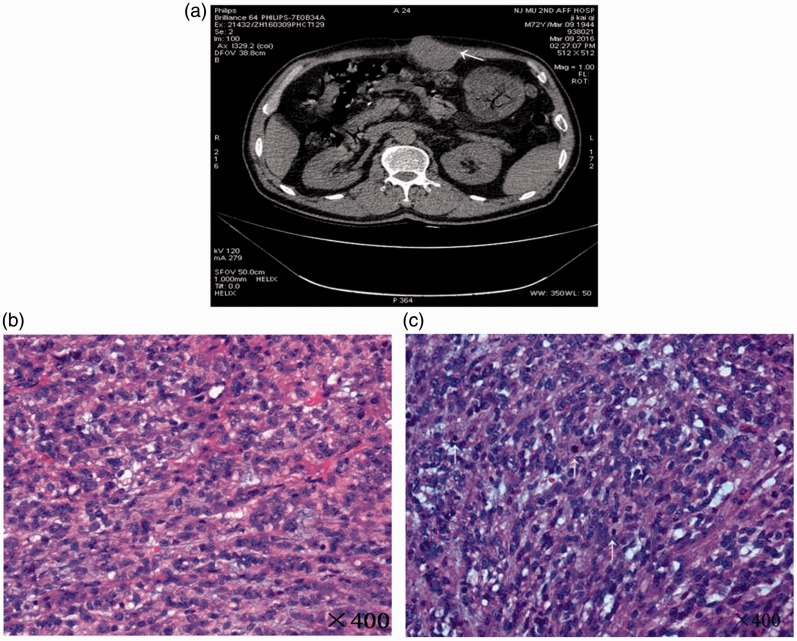
Figure 1.
Abdominal computed tomography scan and examination of hematoxylin- and eosin-stained sections. (a) Computed tomography showed a well-defined heterogeneous mass (white arrow) measuring approximately 6 × 5 × 3 cm in the abdominal subcutaneous tissue. (b) The tumor was mainly composed of spindle cells (magnification, ×400). (c) The tumor had a high mitotic count (>5 per 50 high-power fields) (white arrow).
Histological examination revealed a tumor with interlacing fascicles of spindle-shaped cells with eosinophilic cytoplasm and an oval nucleus (Figure 1(b)). Additionally, >5 mitoses per 50 high-power fields were observed (Figure 1(c)), and infiltration into the surrounding adipose tissue was present. Immunohistochemistry of the tumor cells revealed high Ki67 labeling in the nucleus and positivity for CD34, c-KIT (CD117), and DOG1 and negativity for SMA, desmin, and S-100 (Figure 2(a)–(d)).
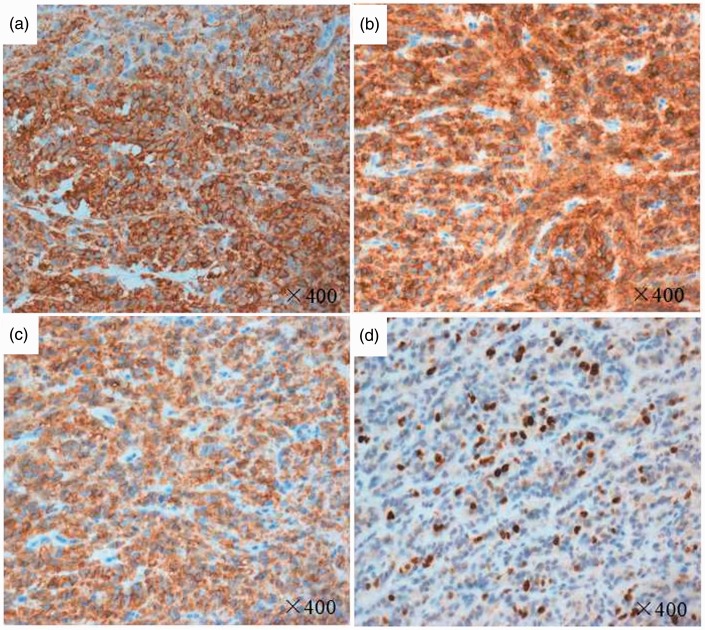
Figure 2.
Immunohistochemical analysis. Immunohistochemical staining showed diffuse strong cytoplasmic positivity for (a) CD34, (b) CD117, and (c) DOG1 and (d) a high Ki-67 labeling index (40%) in the nucleus (magnification, ×400).
Discussion
We have herein reported a rare case involving a 72-year-old man who presented with an abdominal subcutaneous EGIST. The tumor was surgically excised from the abdominal wall. The tumor showed positive staining for CD34 (Figure 2(a)), which often results in misdiagnosis as DFSP. However, we performed a further immunohistochemical analysis and found strong cytoplasmic positive staining for c-KIT (CD117) and DOG1, high Ki67 labeling in the nucleus (Figure 2(b)–(d)), and negative staining for SMA, desmin, and S-100. These markers frequently assist in the differential diagnosis of soft tissue sarcoma.17
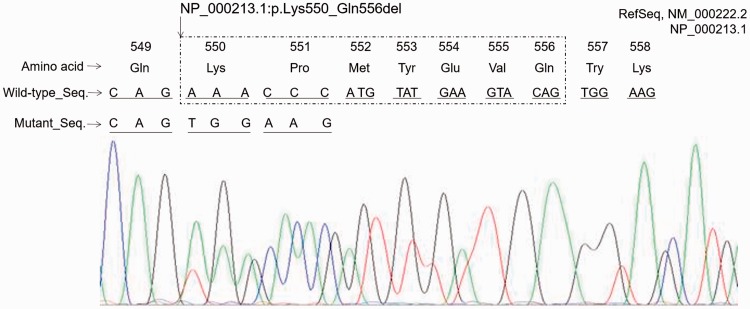
EGISTs exhibit strong cytoplasmic expression of c-KIT (CD117),1 DOG-1,18 and CD341 with negative expression of SMA, desmin, and S-100 protein.1 Thus, EGIST was considered as a differential diagnosis of the tumor in this case. An EGIST is defined as a mesenchymal neoplasm arising from soft tissues outside the gastrointestinal tract.1 Most GISTs contain activating mutations of the c-KIT and PDGFRA genes.19 The mutations in GISTs are usually deletions or insertions residing in exon 11 of the c-KIT gene; less frequently, mutations can be found in exon 9, 13, or 17 of the c-KIT gene or in exon 12 or 18 of the PDGFRA gene. A mutation analysis of these exons of the c-KIT and PDGFRA genes was performed by Sanger sequencing, and we found that the tumor cells harbored an in-frame deletion (NP_000213.1:p.Lys550_Gln556del) in exon 11 of the c-KIT gene (Figure 3). This finding supported the diagnosis of EGIST.
Figure 3.
Genetic analysis. The tumor cells carried an in-frame deletion (NP_000213.1:p.Lys550_Gln556del) in exon 11 of the c-KIT gene.
Most previous studies have shown that EGISTs are derived from the mesentery, omentum, retroperitoneum, pancreas, pelvic cavity, prostate, urinary bladder, and vaginal wall, and most of them are considered to be metastases or a consequence of lost contact with a primary intra-abdominal tumor.3,11,14 In the present case, however, no tumor was found inside or outside of the gastrointestinal tract or retroperitoneum by computed tomography. This implies that the tumor arose neither from a primary GIST in the gastrointestinal tract nor form another primary intra-abdominal tumor. GISTs share features with the interstitial cells of Cajal, which are the putative progenitor cells of GISTs. The abdominal subcutaneous tissue is mesodermal in origin and does not contain interstitial cells of Cajal. However, given that the biological and histopathological features of the tumor cells in the present case were similar to those of GISTs, we speculated that the tumor in the patient’s abdominal wall may have arisen from the ectopic interstitial cells of Cajal during development.
In summary, we have herein reported a rare case involving a 72-year-old man who presented with a primary abdominal subcutaneous EGIST. Such patients presenting with an abdominal subcutaneous tumor have often been diagnosed with DFSP. Thus, both EGISTs and DFSP should be considered as differential diagnoses for tumors in the subcutaneous tissue of the abdominal wall. EGISTs readily relapse and metastasize. The tyrosine kinase inhibitor imatinib is a targeted drug for EGISTs with c-KIT and PDGFRA mutations. DFSP is also a rare borderline malignant or potentially low-grade malignant neoplasm with a high local recurrence rate and low risk of metastasis. The standard therapy for DFSP is wide local excision and radiation. Imatinib was also recently approved for the treatment of unresectable and metastatic DFSP and/or recurrent DFSP.20 Based on these observations, we conclude that routine assessment including immunohistochemical staining and mutation screening for c-KIT and PDGFRA in patients diagnosed with DFSP is recommended to aid in the accuracy of diagnosis and guide treatment decisions.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This work was supported by a special fund from the Second Affiliated Hospital of Nanjing Medical University to Y.W.
References
- 1.Reith JD, Goldblum JR, Lyles RH, et al. Extragastrointestinal (soft tissue) stromal tumors: an analysis of 48 cases with emphasis on histologic predictors of outcome. Mod Pathol 2000; 13: 577–585. [DOI] [PubMed] [Google Scholar]
- 2.Fletcher CD, Berman JJ, Corless C, et al. Diagnosis of gastrointestinal stromal tumors: a consensus approach. Hum Pathol 2002; 33: 459–465. [DOI] [PubMed] [Google Scholar]
- 3.Iqbal N, Sharma A, Iqbal N. Clinicopathological and treatment analysis of 13 extragastrointestinal stromal tumors of mesentery and retroperitoneum. Ann Gastroenterol 2015; 28: 105–108. [PMC free article] [PubMed] [Google Scholar]
- 4.Arabi NA, Musaad AM, Ahmed EE, et al. Primary extragastrointestinal stromal tumour of the whole abdominal cavity, omentum, peritoneum and mesentery: a case report and review of the literature. J Med Case Rep 2014; 8: 337–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reinke DA, Deisch JK, Reinke DD. Gastrointestinal stromal tumor with an unusual presentation as an enlarged prostate gland: a case report and review of the literature. J Gastrointest Oncol 2016; 7(Suppl 1): S71–S74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liu S, Yu Q, Han W, et al. Primary gastrointestinal stromal tumor of the prostate: a case report and literature review. Oncol Lett 2014; 7: 1925–1929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee CH, Lin YH, Lin HY, et al. Gastrointestinal stromal tumor of the prostate: a case report and literature review. Hum Pathol 2006; 37: 1361–1365. [DOI] [PubMed] [Google Scholar]
- 8.Muñoz M, Echeverri C, Ramirez PT, et al. Extragastrointestinal stromal tumor in the rectovaginal septum in an adolescent. Gynecol Oncol Case Rep 2013; 5: 67–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim HH, Koh YS, Park EK, et al. Primary extragastrointestinal stromal tumor arising in the pancreas: report of a case. Surg Today 2012; 42: 386–390. [DOI] [PubMed] [Google Scholar]
- 10.Mekni A, Chelly I, Azzouz H, et al. Extragastrointestinal stromal tumor of the urinary wall bladder: case report and review of the literature. Pathologica 2008; 100: 173–175. [PubMed] [Google Scholar]
- 11.Liu QY, Kan YZ, Zhang MY, et al. Primary extragastrointestinal stromal tumor arising in the vaginal wall: significant clinicopathological characteristics of a rare aggressive soft tissue neoplasm. World J Clin Cases 2016; 4: 118–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kumar AS, Padmini R, Veena G, et al. Extragastrointestinal stromal tumour of the abdominal wall - a case report. J Clin Diagn Res 2013; 7: 2970–2972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alkhatib L, Albtoush O, Bataineh N, et al. Extragastrointestinal Stromal Tumor (EGIST) in the abdominal wall: case report and literature review. Int J Surg Case Rep 2011; 2: 253–255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kroep JR, Bovée JV, van der Molen AJ, et al. Extra-abdominal subcutaneous metastasis of a gastrointestinal stromal tumor: report of a case and a review of the literature. J Cutan Pathol 2009; 36: 565–569. [DOI] [PubMed] [Google Scholar]
- 15.Bogucki B, Neuhaus I, Hurst EA. Dermatofibrosarcoma protuberans: a review of the literature. Dermatol Surg 2012; 38: 537–551. [DOI] [PubMed] [Google Scholar]
- 16.Lemm D, Mügge LO, Mentzel T, et al. Current treatment options in dermatofibrosarcoma protuberans. J Cancer Res Clin Oncol 2009; 135: 653–665. [DOI] [PubMed] [Google Scholar]
- 17.Miettinen M. Immunohistochemistry of soft tissue tumours - review with emphasis on 10 markers. Histopathology 2014; 64: 101–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Espinosa I, Lee CH, Kim MK, et al. A novel monoclonal antibody against DOG1 is a sensitive and specific marker for gastrointestinal stromal tumors. Am J Surg Pathol 2008; 32: 210–218. [DOI] [PubMed] [Google Scholar]
- 19.von Mehren M, Randall RL, Benjamin RS, et al. Gastrointestinal stromal tumors, version 2.2014. J Natl Compr Canc Netw 2014; 12: 853–862. [DOI] [PubMed] [Google Scholar]
- 20.Llombart B, Serra-Guillén C, Monteagudo C, et al. Dermatofibrosarcoma protuberans: a comprehensive review and update on diagnosis and management. Semin Diagn Pathol 2013; 30: 13–28. [DOI] [PubMed] [Google Scholar]