Abstract
Objective
The overall intubation conditions after tracheal intubation with remifentanil, propofol, and sevoflurane at 1.0 minimum alveolar concentration (MAC) are worse than with rocuronium at 0.45 mg/kg. Therefore, we compared the intubation conditions and laryngeal morbidity (vocal cord injuries, hoarseness, and sore throat) with sevoflurane at 1.2 and 1.4 MAC versus 1.0 MAC.
Methods
In this prospective clinical trial, 90 patients were randomized to 3 groups: the sevoflurane 1.0, 1.2, and 1.4 MAC groups. At 3 min, tracheal intubation was performed and the patients’ intubation conditions were assessed. The vocal cords were examined for injury by videolaryngoscopy. Additionally, the incidence and severity of laryngeal morbidity were compared between women and men.
Results
Acceptable intubation conditions were seen in 72% of the patients without significant differences between the groups. Overall, vocal cord injuries (oedema) occurred in three (4%) patients. Women reported sore throat more often than men (51% vs. 21%, respectively).
Conclusions
Intubation conditions were not improved with higher sevoflurane concentrations. The incidence and severity of sore throat were greater in women than men.
Trial registration: ClinicalTrials.Gov: NCT 01896245
Keywords: Sevoflurane, remifentanil, intubation conditions, sore throat, laryngeal injury, sex
Introduction
Neuromuscular blocking agents (NMBAs) are not used in up to 25% of tracheal intubations in Germany and Denmark.1–3 In 2014, we found that tracheal intubation with propofol, remifentanil, and sevoflurane (Sevo) at 1.0 minimum alveolar concentration (MAC) and tracheal intubation with propofol, remifentanil, and rocuronium at 0.45 mg/kg produced comparable intubation conditions at the vocal cords;4 moreover, these two techniques had comparable side effects including arterial hypotension and vocal cord injuries. The overall intubation conditions, however, were better with rocuronium than Sevo.4
In the present study, we hypothesized that higher concentrations of Sevo would improve the overall intubation conditions. We again studied the incidence and severity of vocal cord injuries. Furthermore, we studied sex-related differences in laryngeal morbidity (vocal cord injuries, hoarseness, and sore throat) when using Sevo for tracheal intubation.
Methods
In total, 90 patients planned to undergo tracheal intubation for otologic surgery were randomized into 3 groups. The Sevo 1.0 MAC, 1.2 MAC, and 1.4 MAC groups received Sevo with a MAC of 1.0, 1.2, and 1.4, respectively. The primary outcome measure was the intubation conditions assessed during tracheal intubation.5 The secondary outcome measures were the number of intravenous administrations of ephedrine and the incidence and severity of laryngeal morbidity (hoarseness, sore throat, and vocal cord injuries); videolaryngoscopy was performed before and after surgery to assess vocal cord injuries. In addition, we compared the incidence and severity of laryngeal morbidity between women and men.
Ethics approval and registration
This study was performed at the Rostock University Medical Center from May 2013 to June 2014. Ethical approval was obtained from the Institutional Review Committee (A 2013-0039). The study was registered at ClinicalTrials.Gov with the number NCT 01896245.
Inclusion and exclusion criteria and randomization
After providing informed consent, the patients were randomized according to an online randomization program.6 Patients aged 18 to 80 years with an American Society of Anesthesiologists physical status of I to III who were planned to undergo tracheal intubation for otologic surgery in our Department of Otorhinolaryngology, Head and Neck Surgery were included in the study. Patients were excluded if they had a difficult airway, such as a mouth opening of <3.5 cm. Other exclusion criteria were surgery of the larynx and hoarseness before surgery.
Induction and maintenance of anaesthesia
Before general anaesthesia, all patients received midazolam at 7.5 mg orally. All patients also received dexamethasone at 4.0 mg intravenously (IV) and ondansetron at 4.0 mg IV to prevent postoperative nausea and vomiting
Induction of anaesthesia was performed according to the following standardized procedure.4 The patients’ lungs were ventilated with 100% oxygen at a fresh gas flow rate of 8 L/min. Remifentanil was continuously administered at 0.30 µg/kg/min for 3 min; propofol was then administered at 2.0 mg/kg, and patients in the Sevo 1.0, 1.2, and 1.4 MAC groups received Sevo at concentrations of 3.0%, 4.0%, and 5.0%, respectively. The individual MAC value was calculated from the age of the patient using software integrated with the Primus® anaesthetic machine (Draeger Medical Germany, Lübeck, Germany). After 3 min, when the end-tidal concentration of Sevo reached 1.0, 1.2, or 1.4 MAC and remained stable for 20 s, tracheal intubation was performed by the same anaesthesiologist in all patients. We used Ring-Adair-Elwyn tubes (Mallinckrodt®; Covidien, Dublin, Ireland); men and women received tracheal tubes with an inner diameter of 8.0 and 7.0 mm, respectively. The cuff pressure was measured and adjusted continuously to <25 cmH2O by a cuff pressure monitor.
Maintenance of anaesthesia was standardized as follows: all patients received propofol at 4.0 to 6.0 mg/kg/h and remifentanil at 0.30 µg/kg/min. During tracheal intubation and during the whole surgical procedure, neuromonitoring was performed with the BIS Vista® brain monitoring system (Aspect Medical Systems, Norwood, MA, USA); during surgery, the aim was to achieve a bispectral index (BIS) of 40 to 50. Ephedrine (10.0 mg IV) was given if the systolic arterial pressure decreased to <100 mmHg.
Intubation and extubation conditions
Intubation conditions were assessed according to the Good Clinical Research Practice guidelines (Table 1).5 Extubation conditions were also assessed (Table 1).4 Additionally, the following intubation variables were assessed: Cormack–Lehane grade, number of intubation attempts, and time required for tracheal intubation (time in seconds from the initial insertion of the laryngoscope into the patient’s mouth until blocking of the cuff).
Table 1.
Intubation and extubation conditions.
| Intubation/extubation scores |
|||
|---|---|---|---|
| Clinically acceptable |
Clinically unacceptable |
||
| Variable | Excellent | Good | Poor |
| Intubation conditions Laryngoscopy | |||
| Jaw relaxation | Relaxed | Not fully | Poor |
| Resistance to laryngoscope | None | Slight | Active |
| Vocal cords | |||
| Position | Abducted | Intermediate | Closed |
| Movement | None | Moving | Closing |
| Reaction to tube insertion or cuff inflation | |||
| Movement of limbs | None | Slight | Vigorous |
| Coughing | None | Slight | Sustained |
| Extubation conditions | |||
| Reaction to tube removal | |||
| Movement of limbs | None | Slight | Vigorous |
| Coughing | None | Slight | Sustained |
Intubation conditions: excellent = all qualities are excellent; good = all qualities are excellent or good; poor = any quality is poor. Excellent and good intubation conditions are summarized as clinically acceptable conditions.5
Extubation conditions: excellent = all qualities are excellent; good = all qualities are excellent or good; poor = any quality is poor.4
Laryngeal morbidity
Videolaryngoscopic findings were analysed by an otolaryngologist blinded to the patients’ therapy arm. Videolaryngoscopy was performed 1 day before surgery and 1 day after surgery on the ward. The otolaryngologist compared the videolaryngoscopic findings before induction of anaesthesia with the findings after surgery. Vocal cord injuries were defined as oedema and haematoma formation at the vocal folds. In addition, slight changes such as localized minimal oedema and erythema were assessed. Hoarseness and sore throat were assessed by an anaesthesiologist in the post-anaesthesia care unit and daily up to 3 days after surgery (Appendix).7,8
Sex-related differences in laryngeal morbidity
The incidence and severity of vocal cord injuries, hoarseness, and sore throat were compared between men and women in the Sevo 1.0, 1.2, and 1.4 MAC groups.
Statistical analysis
Statistical analysis was performed with SigmaStat® 3.5 (Systat Software Inc., San Jose, CA, USA). Our primary endpoint was the overall intubation conditions. We performed a sample size calculation, which revealed that we needed 90 patients (30 patients for each group) to detect a statistically significant difference between groups; we assumed that 70% of the patients in the Sevo 1.0 MAC group had acceptable intubation conditions (excellent and good intubation conditions together) and an increase of 25% in the Sevo 1.4 MAC group (α = 0.05, 1−ß = 0.08). Demographic data were analysed with the t-test or Mann–Whitney U-test. Intubation conditions, laryngeal morbidity, and the number of intravenous administrations of ephedrine were compared between the groups using the χ2 test, Fisher’s exact test, or Kruskal–Wallis analysis of variance.
Results
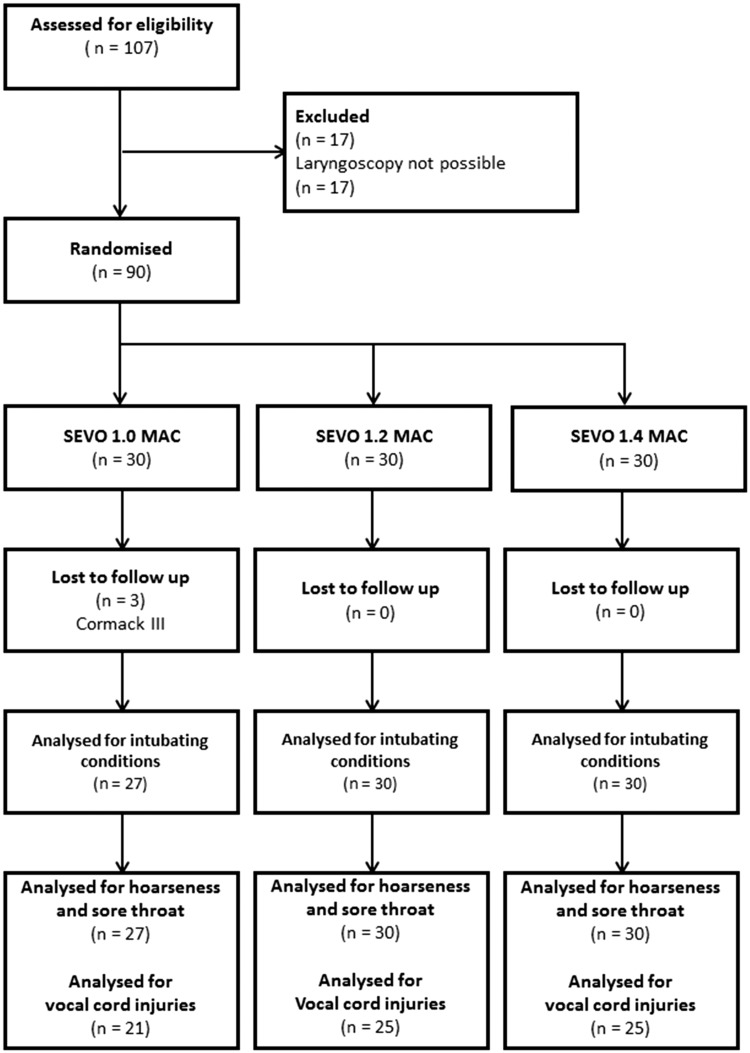
Three patients were excluded (all in the Sevo 1.0 MAC group) because of a Cormack–Lehane grade 3 laryngoscopic view (Figure 1). The patients’ characteristics and duration of anaesthesia were comparable between the groups (Table 2). Intravenous ephedrine was administered to 64% of all patients; the rate was higher in the 1.2 and 1.4 MAC groups, but the difference was not statistically significant (Table 3).
Figure 1.
Flow chart of patient distribution. Laryngoscopy after surgery was not possible in 16 patients.
Table 2.
Patient characteristics and duration of anaesthesia.
| Sevo 1.0 MAC (n = 27) | Sevo 1.2 MAC (n = 30) | Sevo 1.4 MAC (n = 30) | p | |
|---|---|---|---|---|
| Age (years) | 49 ± 15 | 54 ± 16 | 49 ± 18 | 0.39 |
| Height (cm) | 169 ± 10 | 171 ± 10 | 172 ± 8 | 0.60 |
| Weight (kg) | 77 ± 19 | 76 ± 16 | 84 ± 17 | 0.16 |
| Body mass index (kg/m2) | 26.0 (23.9–29.6) | 26.1 (23.4–28.3) | 28.0 (23.9–30.9) | 0.20 |
| ASA physical status I/II/III | 6/20/1 | 7/18/5 | 1/25/4 | 0.09 |
| Duration (min) | 110 (89–130) | 100 (70–154) | 85 (69–139) | 0.59 |
Values are presented as mean ± standard deviation, number, or median (25th and 75th quartiles). Duration = duration of anaesthesia. Sevo, sevoflurane; MAC, minimum alveolar concentration; ASA, American Society of Anesthesiologists.
Table 3.
Concentration of sevoflurane, intubation variables, and ephedrine administration.
| Sevo 1.0 MAC (n = 27) | Sevo 1.2 MAC (n = 30) | Sevo 1.4 MAC (n = 30) | p | |
|---|---|---|---|---|
| Concentration of Sevo (%) | 1.9 (1.7/2.1) | 2.2 (1.8/2.3) | 2.8 (2.1/3.4) | <0.001 |
| Cormack grade 1/2 | 12/15 | 7/23 | 9/21 | 0.22 |
| Attempts (n) 1/2/3 | 23/3/1 | 27/2/1 | 28/2/0 | 0.80 |
| Time for intubation (s) | 26 (20–34) | 22 (20–34) | 23 (22–31) | 0.83 |
| Ephedrine (n) | 15 (56) | 23 (77) | 18 (60) | 0.21 |
Values are presented as median (25th and 75th quartiles), number, or number (%). Attempts = attempts at intubation; Ephedrine = number of administrations of intravenous ephedrine required to treat arterial hypotension. Sevo, sevoflurane; MAC, minimum alveolar concentration.
Intubation and extubation conditions
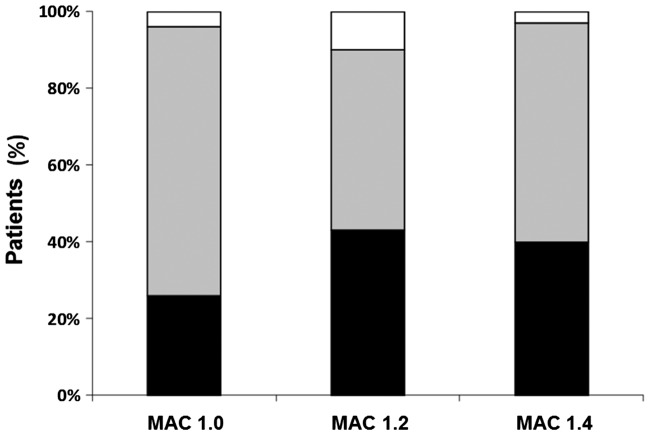
In 63 (72%) patients, the intubation conditions were clinically acceptable (excellent and good intubation conditions together) without significant differences between the groups (Table 4). The subscore for the vocal cords (position and movement of the vocal cords) during tracheal intubation, however, was excellent or good in 82 (94%) patients (Figure 2). The extubation conditions were comparable between the groups (data not shown).
Table 4.
Intubation conditions.
| Sevo 1.0 MAC (n = 27) | Sevo 1.2 MAC (n = 30) | Sevo 1.4 MAC (n = 30) | p | |
|---|---|---|---|---|
| Overall score | 2/16/9 | 1/21/8 | 4/19/7 | 0.43 |
| Subscore for vocal cords | 7/19/1 | 13/14/3 | 12/17/1 | 0.39 |
| - Position | 10/17/0 | 20/10/0 | 14/16/0 | 0.07 |
| - Movement | 13/13/1 | 18/9/3 | 19/10/1 | 0.48 |
| Jaw relaxation | 15/8/4 | 21/8/1 | 15/14/1 | 0.24 |
| Resistance to laryngoscope | 13/11/3 | 11/18/1 | 15/14/1 | 0.43 |
| Movement of limbs | 26/1/0 | 30/0/0 | 30/0/0 | 0.32 |
| Coughing | 13/10/4 | 19/6/5 | 17/8/5 | 0.71 |
Values are presented as numbers of patients with intubation scores of excellent/good/poor. Excellent = all qualities are excellent; good = all qualities are excellent or good; poor = any quality is poor. Excellent and good intubating conditions are summarized as clinically acceptable conditions.5 Sevo, sevoflurane; MAC, minimum alveolar concentration.
Figure 2.
Intubation conditions at the vocal cords; patients (%) with excellent (black bars), good (grey bars), and poor intubation conditions (white bars).
Laryngeal morbidity
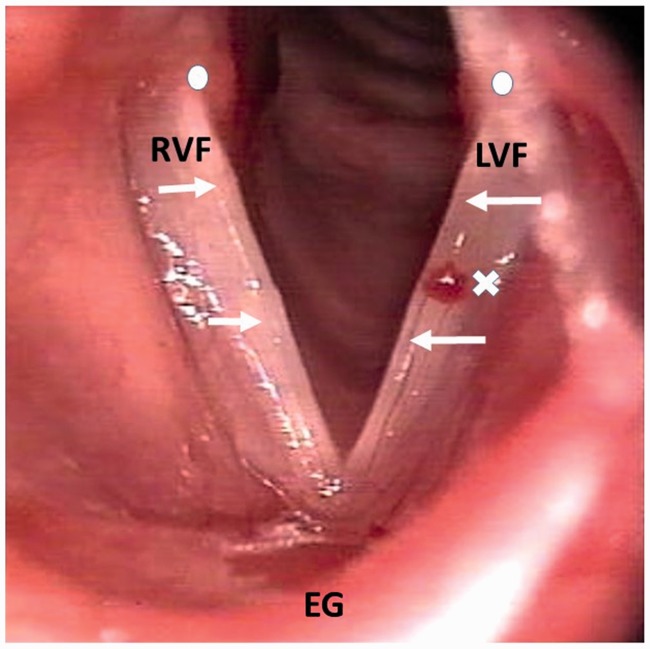
Overall, vocal cord injuries (oedema) occurred in three (4%) patients (no patients in the Sevo 1.0 MAC group, one patient in the Sevo 1.2 MAC group, and two patients in the Sevo 1.4 MAC group) (Figure 3, Table 5). The incidence of hoarseness after surgery was 49% without a significant difference between the study groups. Only one patient developed moderate hoarseness; the other patients developed grade 1 hoarseness (noticed by the patient). Four patients had hoarseness for longer than 1 day, and two patients had hoarseness for 3 days. The incidence of sore throat was 35% without a significant difference between the groups. The severity was comparable between the groups (data not shown).
Figure 3.
Oedema (arrows) and erythema (circles) of both vocal folds at 24 h after surgery. This patient had a pre-existing minimal haemangioma of the left vocal fold (cross). RVF = right vocal fold, LVF = left vocal fold, EG = epiglottis.
Table 5.
Vocal cord injuries and slight changes.
| Sevo 1.0 MAC (n = 21) | Sevo 1.2 MAC (n = 25) | Sevo 1.4 MAC (n = 25) | p | |
|---|---|---|---|---|
| Incidence of injuries | 0.40 | |||
| Oedema | 0 | 1 | 2 | |
| Haematoma | 0 | 0 | 0 | |
| Slight changes | 0.80 | |||
| Localized minimal oedema | 7 | 9 | 11 | |
| Erythema | 6 | 5 | 8 |
Values are presented as number of patients with vocal cord injuries or slight changes. Numbers of patients assessed for vocal cord injuries are summarized in the flow chart in Figure 1.
Sex-related differences in laryngeal morbidity
Vocal cord injuries were assessed in 21 women and 24 men, and no significant differences were noted.
The incidence of hoarseness was comparable between women and men: 21 (48.8%) versus 24 (51.1%), respectively (not statistically significant).
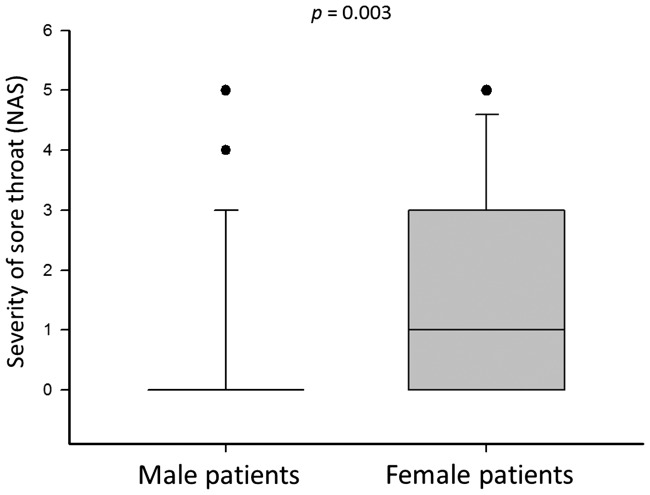
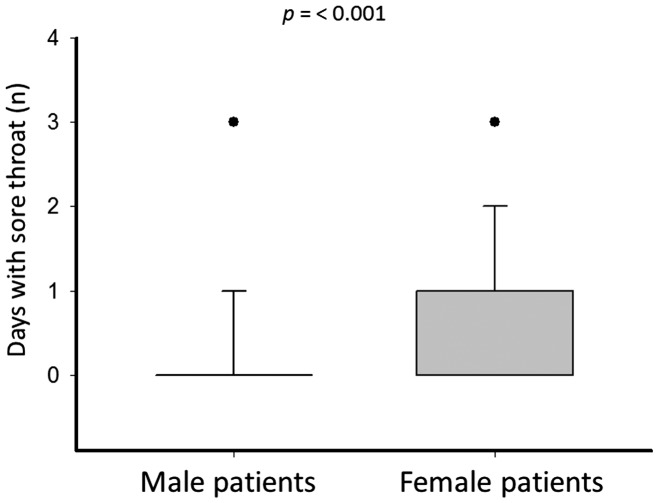
Women reported sore throat significantly more often than men: 22 (51.1%) versus 10 (21.3%) patients, respectively (P = 0.006). The severity of sore throat (numeric analogue scale) and the number of days with sore throat were significantly greater in women than men (Figures 4 and 5).
Figure 4.
Severity of sore throat in women and men. Women and men of the Sevo 1.0, 1.2, and 1.4 MAC groups were pooled. Intensity of sore throat was assessed with a numeric analogue scale ranging from 0 to 10: 0 = no sore throat, 1–3 = mild sore throat, 4–6 = moderate sore throat, 7–9 severe sore throat, and 10 = worst possible sore throat. Box plots show median (line and line within box), quartiles (line and box), 10th and 90th percentiles (error bars), and outlying points. Sevo = sevoflurane, MAC = minimum alveolar concentration.
Figure 5.
Days with sore throat in women and men. Women and men of the Sevo 1.0, 1.2, and 1.4 MAC groups were pooled. Box plots show median (line and upper line of box), quartiles (line and box), 10th and 90th percentiles (error bars), and outlying points. Sevo = sevoflurane, MAC = minimum alveolar concentration.
BIS
The median BIS during tracheal intubation was 27 with no significant difference between the two groups. The BIS was comparable during surgery and tracheal extubation (not statistically significant).
Discussion
Tracheal intubation with propofol at 2.0 mg/kg, remifentanil at 0.30 µg/kg/min, and Sevo at 1.0 MAC, 1.2 MAC, or 1.4 MAC was successful in all patients; the overall intubation conditions, however, were not better with higher concentrations of Sevo. A total of 94% of all patients had excellent or good intubation conditions at the vocal cords. Intravenous ephedrine was given more often in the Sevo 1.2 and 1.4 MAC groups, but the difference was not statistically significant. Therefore, Sevo at 1.0 MAC together with propofol and remifentanil is the preferable concentration for tracheal intubation if NMBAs are not administered. We found a sex-related difference in that the incidence and severity of sore throat after general anaesthesia with Sevo were significantly higher in women than men. This is the first time that this sex-related difference was found when omitting muscle relaxants.
Tracheal intubation without NMBAs is frequently performed in ambulatory surgery because it has clinical advantages. First, the risk of anaphylaxis is reduced because NMBAs are responsible for 69% of all allergic reactions during general anaesthesia.9 Second, postoperative residual curarization, which increases perioperative morbidity and mortality, is omitted.10,11 Third, muscle relaxants are not an obligatory part of total intravenous anaesthesia with propofol and remifentanil.1,2
In 2003, we showed that an induction technique without NMBAs was associated with a higher incidence of hoarseness than an induction technique with NMBAs; additionally, more vocal cord injuries occurred, with a number needed to harm of 2.9.12 In 2010, González Obregón et al.13 showed that addition of Sevo to propofol and remifentanil resulted in an incidence of hoarseness comparable with that in patients receiving rocuronium. In 2014, we confirmed these results and proved that vocal cord injuries were not increased with a muscle relaxant-free induction technique using propofol, remifentanil, and Sevo.4 The addition of Sevo to an induction technique consisting of an opioid and propofol led to acceptable intubation conditions at the vocal cords; thus, Sevo may partially substitute as a muscle relaxant. The overall intubation conditions in the patients receiving Sevo instead of rocuronium, however, were worse than in the patients receiving rocuronium.4
Therefore, we performed the present study to examine whether concentrations higher than 1.0 MAC resulted in better overall intubation conditions. However, the overall intubation conditions were not improved. The BIS during tracheal intubation was comparable between the study groups. Nishiyama14 studied the BIS during administration of different concentrations of Sevo. In that study, when Sevo was increased from 1.0 vol% to 1.5 vol% and subsequently to 2.0 vol%, the BIS decreased; however, the BIS was measured after application of Sevo for 10 min at each concentration.14 In the present study, Sevo was administered for only 3 min; this duration of time might have been too short to affect the BIS. The aim of our study was to examine a realistic induction sequence, and administration of Sevo for 10 min would be too long in the clinical setting.
In another study, Sevo was used alone for tracheal intubation; the dose required for the desired effect in 95% of the population exposed to it was 8.1%.15 When combined with remifentanil at 2.0 µg/kg, the incidence of acceptable intubation conditions was 97%.16 When combined with remifentanil at 1.0 µg/kg followed by 0.25 µg/kg/min, only 2.5 vol% Sevo was necessary.17 In the present study, we administered Sevo not at fixed concentrations but adjusted to the age of the patients. The MAC diminishes with age; the MAC of an 18-year-old patient is twice as high as the MAC of an 80-year-old patient.18 Hence, we used the MAC to standardize the dosage of Sevo relative to the age of the patients.
The incidence of vocal cord injuries in the present study was 4%; in other studies, the incidence varied from 4% to 42% (with NMBAs, up to 27%; without NMBAs, 42%).12,19–22 In 1000 patients, tracheal intubation resulted in haematoma formation at the vocal cords in 45 (4.5%) patients; Kambic and Radsel19 supposed that insufficient relaxation at the vocal cords caused vocal cord injuries. In our study from 2014, laryngeal morbidity was comparable between the Sevo group and the rocuronium group because the subscore for the vocal cords (position and movement of the vocal cords) was comparable.4 In the present study, the intubation conditions at the vocal cords were excellent or good in 94% of the patients. This might explain why we only observed oedema of the vocal cords, but no haematomas.
Hoarseness and sore throat were observed in up to 50% of patients after tracheal intubation in another study.7 We noted hoarseness in 49% of our patients and sore throat in 35%; 87% of our patients, however, developed hoarseness or sore throat only in the post-anaesthesia care unit, and only one patient had sore throat longer than 3 days. Sore throat was observed more often in women than men; moreover, the number of days with sore throat and the severity of sore throat were also greater in women. The odds ratio of sex-related differences in sore throat after general anaesthesia was 1.5 in previous studies23,24; however, muscle relaxants such as succinylcholine were used. Succinylcholine may cause myalgia in the striated pharyngeal muscles.25 No muscle relaxants were used in the present study; therefore, sex-related differences in the perception of pain intensity and in the pharmacodynamics of propofol and remifentanil may be causative.23
Tracheal intubation with propofol, remifentanil, and Sevo was safe, and all tracheal intubations were successful. Nevertheless, induction of anaesthesia without NMBAs may impair the quality of mask ventilation and tracheal intubation.3,26 Therefore, an NMBA as a rescue drug should be available during anaesthetic induction without muscle relaxants.
In conclusion, we have shown that the intubation conditions at the vocal cords were excellent or good in 94% of all patients after propofol at 2.0 mg/kg, remifentanil at 0.30 µg/kg/min, and Sevo at 1.0 MAC. Sevo at 1.2 MAC and 1.4 MAC did not improve the overall intubation conditions. However, we observed a sex-related difference with respect to a higher incidence and severity of sore throat in women than men.
Acknowledgements
No persons other than the authors listed made substantial contributions to the conception and design of the study, acquisition of the data, analysis and interpretation of the data, and preparation of the manuscript.
Appendix: Hoarseness and sore throat
Hoarseness12
Do you have any hoarseness?
If the answer was no, hoarseness was graded as 0 (none); if the answer was yes, hoarseness was graded as follows: 1 = noticed by patient, 2 = obvious to observer, and 3 = aphonia.
Sore throat7
Do you have a sore throat?
Sore throat was assessed with a numeric analogue scale ranging from 0 to 10: 0 = no sore throat, 1–3 = mild sore throat, 4–6 = moderate sore throat, 7–9 = severe sore throat, and 10 = worst possible sore throat.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Eikaas H, Raeder J. Total intravenous anaesthesia techniques for ambulatory surgery. Curr Opin Anaesthesiol 2009; 22: 725–729. [DOI] [PubMed] [Google Scholar]
- 2.Fink H, Geldner G, Fuchs-Buder T, et al. Muscle relaxants in Germany 2005: a comparison of application customs in hospitals and private practices. Anaesthesist 2006; 55: 668–678. [in German, English Abstract]. [DOI] [PubMed] [Google Scholar]
- 3.Lundstrøm LH, Møller AM, Rosenstock C, et al. Avoidance of neuromuscular blocking agents may increase the risk of difficult tracheal intubation: a cohort study of 103,812 consecutive adult patients recorded in the Danish Anaesthesia Database. Br J Anaesth 2009; 103: 283–290. [DOI] [PubMed] [Google Scholar]
- 4.Mencke T, Jacobs RM, Machmueller S, et al. Intubating conditions and side effects of propofol, remifentanil and sevoflurane compared with propofol, remifentanil and rocuronium: a randomised, prospective, clinical trial. BMC Anesthesiol 2014; 14: 39–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fuchs-Buder T, Claudius C, Skovgaard LT, et al. Good clinical research practice in pharmacodynamic studies of neuromuscular blocking agents II: the Stockholm revision. Acta Anaesthesiol Scand 2007; 51: 789–808. [DOI] [PubMed] [Google Scholar]
- 6.Urbaniak GC and Plous S. Research Randomizer 2012. http:/www.randomizer.org.
- 7.McHardy FE, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia 1999; 54: 444–453. [DOI] [PubMed] [Google Scholar]
- 8.Woo P, Colton R, Casper J, et al. Diagnostic value of stroboscopic examination in hoarse patients. J Voice 1991; 5: 231–238. [Google Scholar]
- 9.Laxenaire MC, Mertes PM. Groupe d'Études des Réactions Anaphylactoïdes Peranesthésiques. Anaphylaxis during anaesthesia. Results of a two-year survey in France. Br J Anaesth 2001; 87: 549–558. [DOI] [PubMed] [Google Scholar]
- 10.Arbous MS, Meursing AE, van Kleef JW, et al. Impact of anesthesia management characteristics on severe morbidity and mortality. Anesthesiology 2005; 102: 257–268. [DOI] [PubMed] [Google Scholar]
- 11.Murphy GS, Szokol JW, Marymont JH, et al. Residual neuromuscular blockade and critical respiratory events in the postanesthesia care unit. Anesth Analg 2008; 107: 130–137. [DOI] [PubMed] [Google Scholar]
- 12.Mencke T, Echternach M, Kleinschmidt S, et al. Laryngeal morbidity and quality of tracheal intubation. A randomized controlled trial. Anesthesiology 2003; 98: 1049–1056. [DOI] [PubMed] [Google Scholar]
- 13.González Obregón MP, Rivera Díaz RC, Ordóñez Molina JE, et al. Tracheal intubation quality under remifentanil-propofol with sevoflurane compared with remifentanil-propofol with rocuronium: a randomized double-blind clinical trial. Rev Esp Anestesiol Reanim 2010; 57: 351–356. [in Spanish, English Abstract]. [DOI] [PubMed] [Google Scholar]
- 14.Nishiyama T. Composite-, plain-auditory evoked potentials index and bispectral index to measure the effects of sevoflurane. J Clin Monit Comput 2013; 27: 335–339. [DOI] [PubMed] [Google Scholar]
- 15.Kimura T, Watanabe S, Asakura N, et al. Determination of end-tidal sevoflurane concentration for tracheal intubation and minimum alveolar anesthetic concentration in adults. Anesth Analg 1994; 79: 378–381. [DOI] [PubMed] [Google Scholar]
- 16.Cagiran E, Eyigor C, Balcioglu T, et al. Tracheal intubation in intellectually disabled patients: clinical usefulness of remifentanil and sevoflurane without a muscle relaxant. J Int Med Res 2013; 41: 1632–1638. [DOI] [PubMed] [Google Scholar]
- 17.Cros AM, Lopez C, Kandel T, et al. Determination of sevoflurane alveolar concentration for tracheal intubation with remifentanil, and no muscle relaxant. Anaesthesia 2000; 55: 965–969. [DOI] [PubMed] [Google Scholar]
- 18.Fragen RJ, Dunn KL. The minimum alveolar concentration (MAC) of sevoflurane with and without nitrous oxide in elderly versus young adults. J Clin Anesth 1996; 8: 352–356. [DOI] [PubMed] [Google Scholar]
- 19.Kambic V, Radsel Z. Intubation lesions of the larynx. Br J Anaesth 1978; 50: 587–590. [DOI] [PubMed] [Google Scholar]
- 20.Mencke T, Echternach M, Plinkert PK, et al. Does the timing of tracheal intubation based on neuromuscular monitoring decrease laryngeal injury? A randomized, prospective, controlled trial. Anesth Analg 2006; 102: 306–312. [DOI] [PubMed] [Google Scholar]
- 21.Peppard SB, Dickens JH. Laryngeal injury following short-term intubation. Ann Otol Rhinol Laryngol 1983; 92(4 Pt 1): 327–330. [DOI] [PubMed] [Google Scholar]
- 22.Combes X, Andriamifidy L, Dufresne E, et al. Comparison of two induction regimens using or not using muscle relaxant: impact on postoperative upper airway discomfort. Br J Anaesth 2007; 99: 276–281. [DOI] [PubMed] [Google Scholar]
- 23.Hueppe M, Kemter A, Schmidtke C, et al. Postoperative complaints. Gender differences in expectations, prevalence and appraisal. Anaesthesist 2013; 62: 528–536. [in German, English Abstract]. [DOI] [PubMed] [Google Scholar]
- 24.Myles PS, Hunt JO, Moloney JT. Postoperative minor complications. Anaesthesia 1997; 52: 300–306. [DOI] [PubMed] [Google Scholar]
- 25.Capon LM, Bruce DL, Patel KP, et al. Succinylcholine-induced postoperative sore throat. Anesthesiology 1983; 59: 202–216. [PubMed] [Google Scholar]
- 26.Warters RD, Szabo TA, Spinale FG, et al. The effect of neuromuscular blockade on mask ventilation. Anaesthesia 2011; 66: 163–167. [DOI] [PubMed] [Google Scholar]