Abstract
Objective
To evaluate long-term radiographic and functional outcomes between dynamic hip screw (DHS) and proximal femoral nail antirotation (PFNA) fixation for treatment of osteoporotic type 31-A1 intertrochanteric femoral fractures (IFFs) among elderly patients
Methods
A retrospective comparative study was carried out. Follow-up was performed at 1, 3, 6, 9, and 12 months postoperatively and yearly thereafter. The primary outcome was the radiographic outcome, and the secondary outcome was the functional outcome.
Results
A significant difference in radiographic complications was observed between the DHS group (n = 45, 40.2%) and PFNA group (n = 15, 13.6%). The risk of femoral shaft fracture after implant removal at the 1-year follow-up was increased by 0.9% (n = 1) and 6.3% (n = 7) in the PFNA and DHS groups, respectively. This difference persisted with rates of 3.6% (n = 4) and 12.5% (n = 14) at the final follow-up. Additionally, significant differences were present in the Harris hip score at each visit.
Conclusion
Our results indicate that PFNA yields better outcomes than DHS fixation among elderly patients with osteoporotic type 31-A1 IFFs.
Keywords: Intertrochanteric fracture, radiographic complication, proximal femoral nail antirotation, dynamic hip screw, Harris hip score
Introduction
Dynamic hip screw (DHS) fixation and proximal femoral nail antirotation (PFNA) fixation are both frequently used to treat intertrochanteric femoral fractures (IFFs).1–3 In China, the percentage of IFFs treated with these two implant techniques increased from 9% in 2010 to 35% in 2015.4,5
According to the literature, the complication rate after open reduction and internal fixation or closed reduction and internal fixation (CRIF) of IFFs [AO Foundation/Orthopaedic Trauma Association (AO/OTA) type 3.1 A1.1-1.3] is comparatively low relative to that after fixation with other implants. However, a low postoperative Harris hip score (HHS), cut-out, and migration of the femoral neck screw occasionally occur regardless of whether PFNA or DHS fixation was used. A low postoperative HHS and high radiographic complication rate after undergoing PFNA or DHS fixation for type 31-A1 IFFs mostly occur among elderly patients with osteoporosis.6,7 Moreover, no long-term studies have yet assessed which device is more appropriate for the treatment of type 31-A1 IFFs among elderly patients with osteoporosis. Numerous randomized clinical trials have demonstrated no statistically significant difference in short-term functional and radiographic outcomes between the two devices in the management of IFFs (AO/OTA type 3.1 A1.1-3.3, stable or unstable).8,9 Aros et al.1 reported the outcomes of 143 elderly patients with osteoporosis who underwent DHS or PFNA fixation for IFFs and found a 6% incidence of radiographic complications at the 1-year follow-up evaluation. A meta-analysis involving 669 IFFs revealed a radiographic complication rate of <10%, and the postoperative HHSs were satisfactory among elderly patients with osteoporosis at the 2-year follow-up evaluation.10 Overall, the rate of radiographic complications after CRIF of PFNA- or DHS-treated IFFs was comparable to that after other treatments, and the HHS was acceptable.2,11 Nevertheless, no empirical study based on long-term data supports this conclusion.
The purpose of this study was to compare the long-term radiographic and functional outcomes between DHS and PFNA fixation in the treatment of IFFs (AO/OTA type 3.1 A1). The hypothesis was that DHS fixation would have poorer radiographic and worse functional outcomes than PFNA fixation.
Patients and methods
The study was approved by the institutional ethics review board of the First Affiliated Hospital of Sun Yat-sen University, and an exemption for informed consent was obtained from the Investigational Ethical Review Board. From March 2007 to December 2011, 413 elderly patients with osteoporosis (413 hips) with type 31-A1 IFFs were first treated with a PFNA device (Smith & Nephew, Memphis, TN, USA) or a DHS (Synthes, West Chester, PA, USA). The inclusion criteria were as follows: age of 60 to 92 years, a freshly closed type 31-A1 IFF, undergoing CRIF, a bone mineral density T-score of ≤ −2.5 at the femoral neck, the ability to walk independently without aids before the fracture, surgery performed an average of 3 days (range, 1–6 days) after admission, use of a DHS (standard screw/blade; Synthes) or PFNA device (240 or 300 mm in length, 11 or 12 mm in diameter, 125° or 130° collodiaphyseal angle; Smith & Nephew), and removal of the internal fixation device within 1 year. The exclusion criteria were as follows: pathological fractures or metastatic disease, ipsilateral lower-limb surgery or a contralateral IFF, follow-up of < 3 years, bone-active medication use, poly-trauma, severe osteoarthritis, an American Society of Anesthesiologists (ASA) physical status of V, cognitive dysfunction, mental illness, and refusal to participate.
Major baseline characteristics, including sex, age, IFF side, bone mineral density, body mass index, ASA physical status, AO/OTA fracture type, injury operation interval, quality of reduction, and duration of follow-up are shown in Table 1. The postoperative HHS and major postoperative radiographic outcomes [lateral cortex fracture, limb shortening (>2.5 cm), varus collapse, screw cut-out (penetration of the superior aspect of the femoral head from screw migration) secondary to the “Z” effect, and femoral shaft fracture after implant removal] were evaluated at 1, 3, 6, 9, and 12 months postoperatively and yearly thereafter.
Table 1.
Patient characteristics in both groups
| Variable | PFNAa (n = 110) | DHSb (n = 112) | P-value |
|---|---|---|---|
| Sex, male/female | 40/70 | 45/67 | 0.559* |
| Age, years | 74.34 ± 8.18 | 75.16 ± 8.80 | 0.471* |
| BMI, kg/m2 | 24.94 ± 1.99 | 25.34 ± 1.38 | 0.081* |
| BMD | –3.90 ± 0.66 | –3.76 ± 0.75 | 0.152* |
| Side, left/right | 56/54 | 60/52 | 0.691* |
| AO/OTA fracture type | 0.648* | ||
| 31A1.1 | 32 | 36 | |
| 31A1.2 | 48 | 42 | |
| 31A1.3 | 30 | 34 | |
| ASA physical status | 0.863* | ||
| I | 32 | 27 | |
| II | 36 | 39 | |
| III | 30 | 32 | |
| IV | 12 | 14 | |
| Injury operation interval | 0.912* | ||
| <24 h | 19 | 22 | |
| 24–48 h | 44 | 46 | |
| 48–72 h | 34 | 30 | |
| >72 h | 13 | 14 | |
| Quality of reduction | 0.510* | ||
| Good | 66 | 72 | |
| Acceptable | 44 | 40 | |
| Poor | 0 | 0 | |
| Follow-up, months | 37.97 ± 1.60 | 38.20 ± 1.90 | 0.343* |
Data are presented as number of patients or mean ± standard deviation.
No statistically significant values.
PFNA: proximal femoral nail antirotation; DHS: unconventional dynamic hip screw; ASA: American Society of Anesthesiologists; BMI: body mass index; BMD: bone mineral density; aSmith & Nephew, Memphis, TN, USA; bSynthes, West Chester, PA, USA
All patients received a dose of the antibiotic teicoplanin (Aventis Pharma, Kings Hill, UK) half an hour before surgery. All surgeries were carried out under spinal anesthesia. Closed reduction of all IFFs was attained under fluoroscopic guidance. All surgeries were finished at our institution by experienced orthopedists. The surgical procedures were based on standard protocols for either PFNA or DHS fixation, as recommended by the device manufacturers and as previously described by Mereddy et al.18 for PFNA fixation and Little et al.11 for DHS fixation. The correct implant position and the tip–apex distance (TAD) were controlled postoperatively using X-ray. The radiographs were attained immediately after surgery (Figures 1, 2).
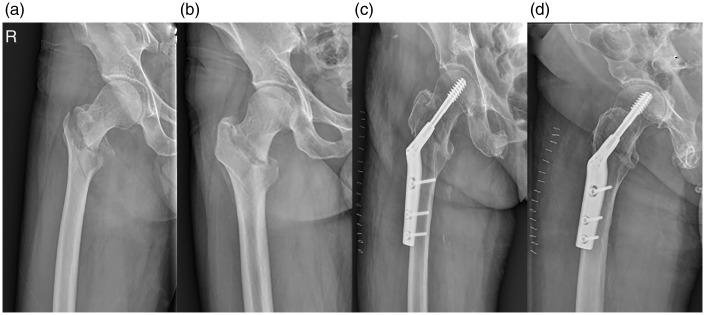
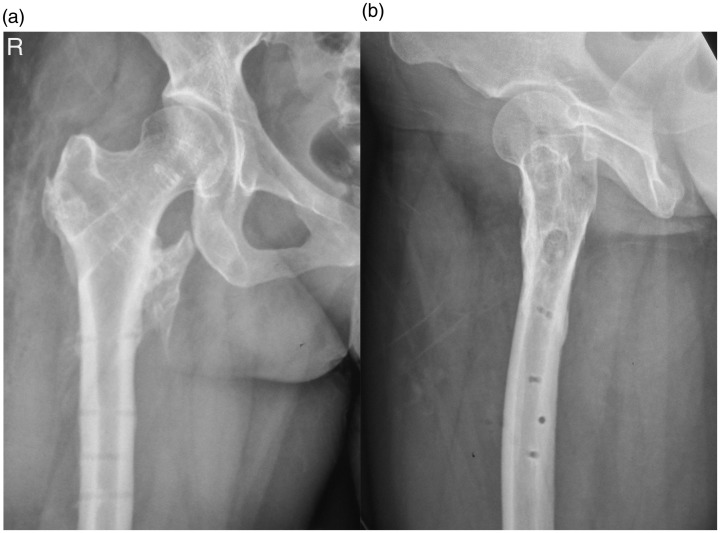
Figure 1.
Anteroposterior and lateral X-ray views of an osteoporotic patient with an intertrochanteric femoral fracture (AO/OTA 31-A1) of the right hip (a, b). Postoperative anteroposterior and lateral X-ray views of the same patient undergoing dynamic hip screw fixation of an osteoporotic intertrochanteric femoral fracture of the right hip (c, d).
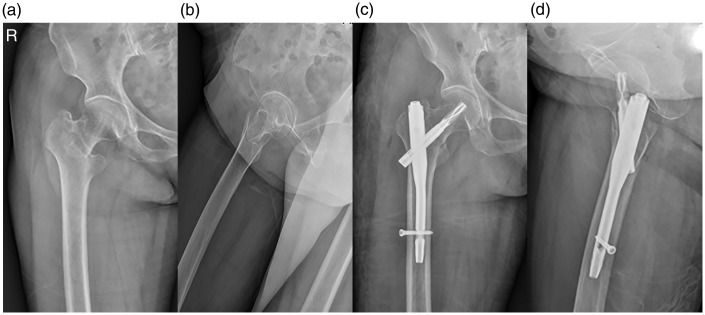
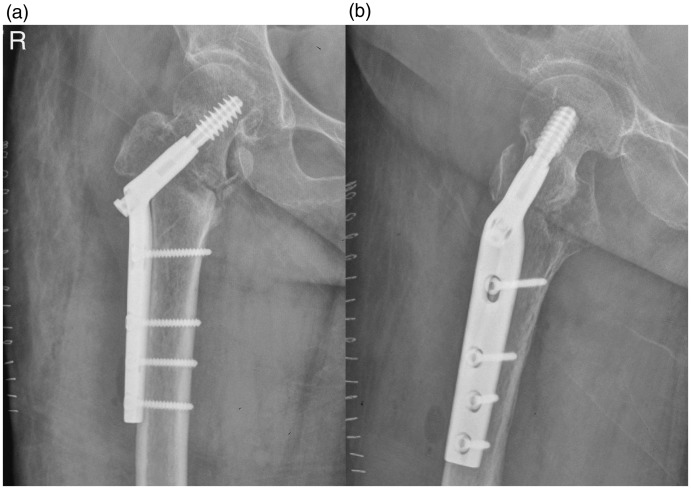
Figure 2.
Anteroposterior and lateral X-ray views of an osteoporotic patient with an intertrochanteric femoral fracture (AO/OTA 31-A1) of the right hip (a, b). Postoperative anteroposterior and lateral X-ray views of the same patient undergoing proximal femoral nail antirotation fixation of an osteoporotic intertrochanteric femoral fracture of the right hip (c, d).
A low-molecular-weight heparin (enoxaparin sodium; Clexane 4000 AXa IU; AVENTIS, Shanghai, China) was injected once a day for 7 days, starting at admission. Each patient additionally received prophylactic antibiotics (cefazolin sodium pentahydrate, 2.0 g; Baomanbio, Shanghai, China) twice a day for 3 days, starting the day before surgery.
After surgery, the rehabilitation protocol was identical for the two groups. Continuous passive motion (CPM, Smith & Nephew, Memphis, Tennessee) was managed by a physiotherapist three times a day starting the day after surgery if the patient was capable. The weight-bearing protocol for all patients was the same: out-of-bed activity with axillary crutches on postoperative day 7, touch weight-bearing ambulation on postoperative day 10, partial weight-bearing ambulation on postoperative day 14, and full weight-bearing ambulation after bone union was proven by X-ray.
Between 11 and 12 months after surgery, removal of the internal fixation device was performed in patients with infection, long-term pain, intolerance, or allergy. The procedure details (antibiotics, antithrombotic drugs, anesthesia, surgery, wound care, and postoperative rehabilitation) were essentially the same as in the first operation. On postoperative day 3, the patients were encouraged to engage in partial weight-bearing ambulation. All of the patients were discharged with full weight-bearing ambulation approximately 7 days (range, 5–8 days) after surgery.
All statistical analyses were performed using SPSS Statistics version 22 (IBM Corp., Armonk, NY, USA). All continuous data are expressed as mean ± standard deviation (SD). Quantitative variables were analyzed using Student’s t-test, and categorical variables were analyzed using the χ2 test or Fisher’s exact test where appropriate. All tests were two-tailed. The level of significance was set at P < 0.05 for all statistical analyses.
Results
Comparison of baseline data
A total of 104 patients met the exclusion criteria, and another 47 patients refused to participate, leaving 262 patients (262 hips) eligible for the study. During the follow-up, 35 patients refused to continue participating in the study. Two patients died of gas poisoning, and three patients died of cerebral hemorrhage, unexplained cardiac arrest, and a car accident. Consequently, 222 patients (222 primary operations; PFNA, n = 110; DHS, n = 112) were enrolled in the final evaluation (Figure 3). The patients comprised 96 men and 126 women. No significant sex-related difference was present between the two groups. The average age was 74.34 years (range, 60–92 years; SD, 8.18) in the PFNA group and 75.16 years (range, 60–91 years; SD, 8.80) in the DHS group (Table 1). No significant between-group differences were present in the baseline data or mortality rates (Table 3).
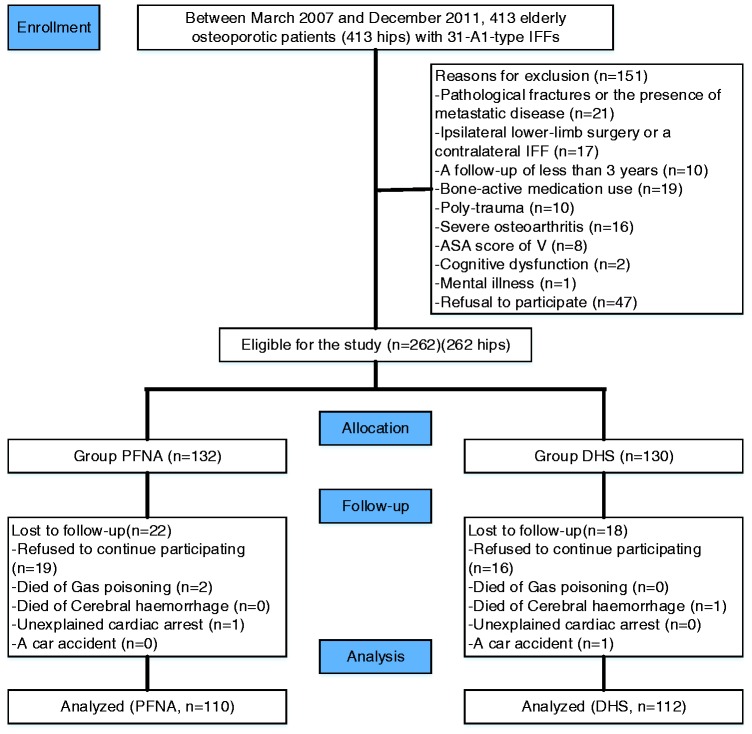
Figure 3.
Flow diagram demonstrating methods for identification of studies assessing the treatment of osteoporotic type 31-A1 intertrochanteric femoral fractures in elderly patients using either proximal femoral nail antirotation or dynamic hip screw fixation and reasons for exclusion.
Table 3.
Main results of the study
| Variable | PFNAa (n = 110) | DHSb (n = 112) | P-value |
|---|---|---|---|
| Radiographic complications | 15 (13.6) | 45 (40.2) | |
| Patients affected | 11 (10.0) | 39 (34.8) | 0.000* |
| Femoral shaft fracture after implant removal | 4 | 14 | 0.016* |
| Lateral cortex fracture | 1 | 7 | 0.033* |
| Limb length discrepancy (>2.5 cm) | 0 | 5 | 0.025* |
| Malunion | 3 | 1 | 0.304 |
| Nonunion | 1 | 0 | 0.495 |
| Varus collapse | 0 | 6 | 0.014* |
| Heterotopic ossification | 3 | 2 | 0.636 |
| Screw cut-out | 0 | 4 | 0.045* |
| Implant failure | 0 | 5 | 0.025* |
| Aseptic loosening | 0 | 1 | 1.000 |
| Osteolysis with well-fixed implants | 3 | 0 | 0.078 |
| Wound infection | 2 | 2 | 0.985 |
| Mortality | 0 | 0 | 1.000 |
| Reoperation | 6 (5.5) | 24 (21.4) | 0.000* |
Data are presented as n or n (%).
Statistically significant values.
PFNA: proximal femoral nail antirotation; DHS: unconventional dynamic hip screw; aSmith & Nephew, Memphis, TN, USA; bSynthes, West Chester, PA, USA
Comparison of functional outcomes
Both groups demonstrated variations in the postoperative HHS from postoperative month 1 to the last follow-up at an average of 37.97 and 38.20 months for the PFNA and DHS groups, respectively.
During the first 3 postoperative months and after postoperative month 12, the HHS in the PFNA group was higher than that in the DHS group; however, from postoperative months 6 to 9, the HHS in the PFNA group was lower than that in the DHS group. From postoperative month 12 to the final follow-up, the HHS in the PFNA group was higher than that in the DHS group. At the final follow-up, the average postoperative HHS was 76.86 (range, 54–92) in the PFNA group, which was better than that in the DHS group (73.36; range, 52–92). The results were excellent in 47 patients (PFNA, n = 31 and DHS, n = 16; P = 0.029), good in 133 patients (PFNA, n = 79 and DHS, n = 54; P = 0.000), fair in 9 patients (PFNA, n = 4 and DHS, n = 5), and poor in 33 patients (PFNA, n = 12 and DHS, n = 21). The main results are shown in Table 2.
Table 2.
Harris hip scores in the two groups at 1, 3, 6, 9, 12, 15, 18, 21, 24, 27, 30, 33, and 36 months postoperatively and at the final follow-up
| Variable | PFNAa (n = 110) | DHSb (n = 112) | P-value |
|---|---|---|---|
| 1 month postoperatively | 71.78 ± 2.38 | 70.93 ± 1.90 | 0.003* |
| 3 months postoperatively | 80.29 ± 2.69 | 79.31 ± 1.69 | 0.001* |
| 6 months postoperatively | 81.42 ± 2.86 | 84.78 ± 3.48 | 0.000* |
| 9 months postoperatively | 82.55 ± 2.52 | 83.46 ± 2.46 | 0.008* |
| 12 months postoperatively# | 79.57 ± 1.95 | 78.54 ± 2.17 | 0.000* |
| 15 months postoperatively | 82.90 ± 2.14 | 81.38 ± 2.33 | 0.000* |
| 18 months postoperatively | 84.76 ± 2.68 | 82.58 ± 2.30 | 0.000* |
| 21 months postoperatively | 83.03 ± 2.40 | 81.79 ± 2.66 | 0.000* |
| 24 months postoperatively | 84.89 ± 2.62 | 82.06 ± 3.14 | 0.000* |
| 27 months postoperatively | 81.00 ± 3.62 | 77.17 ± 2.36 | 0.000* |
| 30 months postoperatively | 74.36 ± 4.39 | 73.23 ± 3.99 | 0.000* |
| 33 months postoperatively | 76.07 ± 5.17 | 73.46 ± 4.01 | 0.000* |
| 36 months postoperatively | 76.63 ± 5.81 | 74.13 ± 5.35 | 0.001* |
| Final follow-up | 76.86 ± 7.50 | 73.36 ± 10.29 | 0.004* |
Harris hip scores are presented as mean ± standard deviation.
*Statistically significant values; #After removal of the internal fixation.
PFNA: proximal femoral nail antirotation; DHS: unconventional dynamic hip screw; aSmith & Nephew, Memphis, TN, USA; bSynthes, West Chester, PA, USA
Comparison of radiographic outcomes
Statistically significant differences in radiographic outcomes were present between the two groups, including the incidence of femoral shaft fracture after implant removal, lateral cortex fracture, limb shortening (>2.5 cm), varus collapse, screw cut-out (penetration of the superior aspect of the femoral head from screw migration) secondary to the “Z” effect, and implant failure. There were no statistically significant differences in the remaining observations between the two groups (Table 3).
In the PFNA group, the radiographic complication rate was 13.6% (15/110 patients). In total, 15 radiographic complications in 11 patients were observed in the PFNA group (Figure 4), including a femur shaft fracture after implant removal, lateral cortex fracture, malunion, nonunion, heterotopic ossification, and osteolysis with well-fixed implants. In the DHS group, radiographic complications were significantly more common (Figures 5, 6, 7). A radiographic complication rate of 40.2% (45/112 patients) was present in the DHS group, which was significantly higher than that in the PFNA group (13.6%; 15/110 patients; P = 0.000). Remarkably, the increased risk of femoral shaft fracture after implant removal at the 1-year follow-up was 0.9% (n = 1) and 6.3% (n = 7) in the PFNA and DHS groups, respectively (P = 0.033). This difference remained over time, with rates of 3.6% (n = 4) and 12.5% (n = 14) at the last follow-up (P = 0.016).
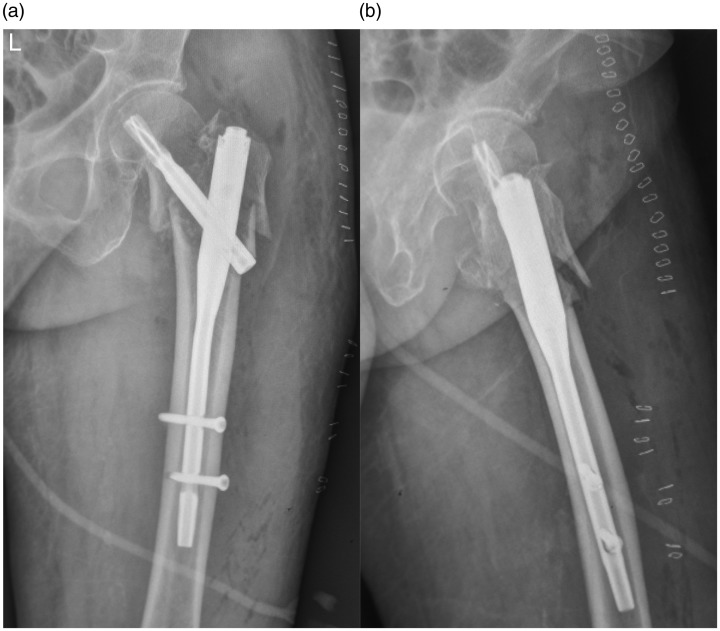
Figure 4.
Plain radiographs demonstrating a left intertrochanteric femoral fracture fixed with proximal femoral nail antirotation fixation. Subsequent follow-up radiographs at 9 months demonstrate multiple fractures of the proximal part of the femur.
Figure 5.
Plain radiographs demonstrating a right intertrochanteric femoral fracture fixed with dynamic hip screw fixation. Follow-up radiographs at 12 months demonstrate heterotopic ossification.
Figure 6.
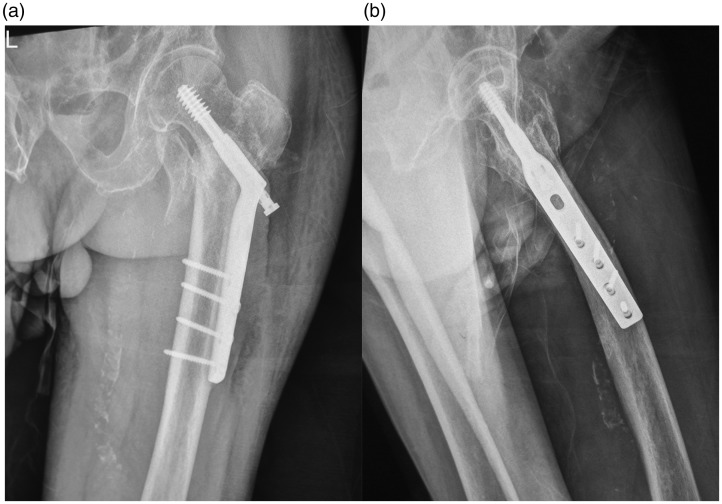
Plain radiographs demonstrating a right intertrochanteric femoral fracture fixed with dynamic hip screw fixation. Follow-up radiographs at 12 months demonstrate a lateral cortex fracture and lag screw cut-out.
Figure 7.
Plain radiographs demonstrating a left intertrochanteric femoral fracture fixed with dynamic hip screw fixation. Subsequent follow-up radiographs at 9 months demonstrate that the lag screw is backing out with proximal fragments (lateral cortex fracture and lesser trochanter).
Discussion
In the current long-term study, significant differences were observed in terms of lateral cortex fracture, limb shortening, varus collapse, screw cut-out (penetration of the superior aspect of the femoral head from screw migration), femoral shaft fracture after implant removal, and postoperative HHS. These results are inconsistent with some previously published studies that revealed no significant differences in radiographic outcomes and the postoperative HHS between PFNA and DHS fixation of type 31-A1 IFFs.2,1,8 Additionally, our results differ from some studies that concluded that PFNA fixation had no significant advantage over DHS fixation for stable IFFs.14,15 However, most previous studies have documented that PFNA implants are superior to DHS implants in terms of early weight-bearing (i.e., a reduced time to first weight-bearing). A prospective study by Saudan et al.14 that included 206 elderly osteoporotic patients with type 31-A1 IFFs stabilized with either PFNA or DHS fixation revealed a significant difference in radiographic complications in both groups. However, Mavrogenis et al.16 performed a retrospective study of 7643 operations to stabilize simple two-part IFFs (AO/OTA type A1) using either a DHS (n = 6355) or a PFNA implant (n = 1288) and reported that the PFNA implant resulted in more radiographic complications and a poorer HHS. In a meta-analysis of 8 randomized clinical trials assessing PFNA and DHS fixation among 1276 elderly osteoporotic patients with IFFs (AO/OTA type 3.1 A1.1-1.3),17 5 trials inferred that the PFNA implant was the optimal fixation device, 2 reported that the DHS was better, and 1 failed to show superiority of one implant over the other. Nevertheless, in a randomized study of PFNA versus DHS fixation involving 43,659 elderly osteoporotic patients with type 31-A1 IFFs, Mereddy et al.18 reported that patients treated with a PFNA implant had higher rates of revision surgery during the first postoperative year than those treated with a DHS implant (7.2% vs. 5.5%, respectively). In addition, Zou et al.8 assessed PFNA and DHS fixation for the treatment of osteoporotic type 31-A1 IFFs and demonstrated no significant difference in terms of implant-related complications and the postoperative HHS.
Type 31-A1 IFFs account for 12% to 33% of all IFFs at our institution. The choice of an optimal implant is of prime importance among elderly osteoporotic patients with type 31-A1 IFFs. Although no long-term comparisons of radiographic complications and the postoperative HHS have been made among elderly osteoporotic patients with type 31-A1 IFFs, the treatment for such IFFs in these patients has been associated with a mechanical complication rate of 0% to 24%.19,20 Ozkayin et al.21 confirmed a 23% radiographic complication rate with a PFNA implant and a 30% complication rate with a DHS implant. Radcliff et al.22 noted a 22% radiographic complication rate among 14 patients who underwent PFNA fixation. Sahin et al.23 compared 35 patients who underwent DHS fixation and 32 who underwent PFNA fixation and reported a radiographic complication rate of 24% and 15%, respectively. Kanakaris et al.8 demonstrated that when patients with type 31-A1 IFFs had osteoporosis, DHS fixation had a tendency to result in more radiographic complications than PFNA. In previously published literature, DHS fixation has been documented to have a radiographic complication rate ranging from 10% to 25%.24 Nevertheless, whether osteoporosis or bone loss was predominant among the elderly patients with type 31-A1 IFFs in the present study is unclear.31 To the best of our knowledge, our series of 222 elderly patients with osteoporosis is the largest study to date to assess PFNA and DHS fixation for management of type 31-A1 IFFs. Most previous studies tended to ignore type 31-A1 IFFs among elderly patients with osteoporosis, which has resulted in a lack of research among these patients and a greater tendency to encounter a deteriorating postoperative HHS together with an increased risk of radiographic complications.16,25–27 Consequently, it is crucial to achieve a near-anatomic reduction and maintain it until union. Unfortunately, this is often difficult to achieve in elderly osteoporotic patients with type 31-A1 IFFs because intraoperative and postoperative collapse or fracture may occur; this increases the difficulty of the operation because osteoporotic type 31-A1 IFFs are at high risk of instability, without regard to type 31-A2/A3 IFFs. In addition, according to our previous experience, we do not hesitate to choose a DHS implant for type 31-A1 IFFs and believe that DHS fixation is the optimal choice for such a fracture. This is because cortical contact is present after reduction of type 31-A1 IFFs, without a gap medially, posteriorly, or laterally.28,29 This contact can prevent fracture displacement secondary to the pull of the iliopsoas, gluteus medius, and short external rotator muscles on the proximal fragment30; varus collapse; retroversion; future deformity; or nonunion when a force is transmitted to the fracture line. Nevertheless, in osteoporotic type 31-A1 IFFs, femoral shaft fracture after implant removal is prone to occur secondary to the excessive stress shielding or concentration in patients who have undergone DHS fixation. Furthermore, rupture of the lateral wall while inserting the implant could convert a stable IFF into an unstable IFF. Under these circumstances, applying a DHS device could further increase this risk despite good reduction and satisfactory fixation. However, this can be avoided by applying a PFNA implant or a smaller-diameter DHS.31 In the present study, DHS fixation was related to radiographic complications such as limb shortening, varus collapse, screw cut-out, and femoral shaft fracture after implant removal. Limb shortening was observed more frequently in association with DHS fixation. The application of a locking plate cannot easily prevent limb shortening in patients with osteoporotic type 31-A1 IFFs. Such patients who have undergone stabilization with a short locking plate will have an increased risk of jamming the screw, which further increases the risk of toggling of the screws within the head and resultant cut-out.32 In contrast, a PFNA device could, to some extent, maintain reduction until bony union with a lower risk of radiographic complications because it can decrease concentrated stress. However, in osteoporotic type 31-A1 IFFs stabilized using a PFNA implant, the radiographic complications mentioned above could also occur. Moreover, long PFNA implants have shown better results than short PFNA implants in previous studies. For this reason, the challenge in treating elderly osteoporotic patients with type 31-A1 IFFs is not only to achieve satisfactory reduction and fixation but also to attain healing.
In the current study, the rate of re-fracture (femoral shaft fracture after implant removal) was slightly higher than that in some previous studies. The majority of the re-fractures occurred after implant removal. In contrast to other studies,33,2,23 we noted a three-times-higher risk of re-fracture when applying DHS fixation. The reason for this appears to be excessive stress shelter in osteoporotic IFFs. Although weight-bearing was delayed in patients who underwent DHS fixation, stress shelter and bone loss associated with the cover part of the locking plate were inevitable until a fracture occurred. Furthermore, in DHS fixation, more screw holes can result in greater stress concentrations and high strain, which may cause a subsequent re-fracture after cyclic loading despite the fact that no fracture occurred during fixation. In addition, the working length of the DHS in elderly osteoporotic patients could also have a potential effect on the stiffness, gap motion, and resistance to fatigue.8 We conclude that among elderly osteoporotic patients with type 31-A1 IFFs, increasing the implant length at the level of the fracture line enables a larger area of stress distribution on the locking plate and decreases the stress at the fracture site. PFNA fixation appears to be superior because it disperses and reduces the concentrated stress secondary to the biomechanical characteristics of the intramedullary fixation and controllable TAD. The superior TAD in patients who have undergone PFNA fixation does have a tendency to reduce the re-fracture rate, and we note that applying the guide device to the PFNA can ensure that the TAD remains in a reasonable range, especially on lateral radiographs. Because the guide device is only part of the PFNA process, the procedure of nailing will in fact empower surgeons to achieve an improved PFNA position and thereby reduce the risk of uneven distribution of biomechanics.34,16,22
To our knowledge, no other studies to date have reported such a difference in the re-fracture rate between these two implants. Our study was retrospective, and some parameters of the perioperative procedure were not available, such as blood loss, operative time, and fluoroscopy exposure time. Future prospective studies should include these parameters, although variables requiring analysis will need to be further evaluated. A long intramedullary nail and/or a long DHS is currently recommended for use in elderly osteoporotic patients with type 31-A1 IFFs. In addition, patient- and surgeon-related confounders may have existed in the present study, and we might not have addressed every potential confounding variable in our analyses.
In conclusion, our study revealed a higher rate of radiographic complications in association with DHS than PFNA fixation among osteoporotic type 31-A1 IFFs in elderly patients. In addition, DHS fixation had poorer performance in terms of the postoperative HHS than did PFNA fixation during the first 3 months postoperatively and after 12 months postoperatively. Based on these findings, we conclude that the PFNA device is a better implant than the DHS for elderly osteoporotic patients with 31-A1 IFFs. Although this study had several limitations, our results appear to be consistent with those of other studies. From a macroscopic perspective, PFNA fixation as a whole has become a safer procedure, although it remains an expensive implant and may be less cost-effective at this point.
Declaration of conflicting interest
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Aros B, Tosteson ANA, Gottlieb DJ, et al. Is a sliding hip screw or IM nail the preferred implant for intertrochanteric fracture fixation? Clin Orthop Relat Res 2008; 466: 2827–2832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avakian Z, Shiraev T, Lam L, et al. Dynamic hip screws versus proximal femoral nails for intertrochanteric fractures. ANZ J Surg 2012; 82: 56–59. [DOI] [PubMed] [Google Scholar]
- 3.Garg B, Marimuthu K, Kumar V, et al. Outcome of short proximal femoral nail antirotation and dynamic hip screw for fixation of unstable trochanteric fractures. A randomised prospective comparative trial. Hip Int 2011; 21: 531–536. [DOI] [PubMed] [Google Scholar]
- 4.Goffin JM, Pankaj P, Simpson AH, et al. Does bone compaction around the helical blade of a proximal femoral nail antirotation (PFNA) decrease the risk of cut-out? A subject-specific computational study. Bone Joint Res 2013; 2: 79–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Guerra MT, Pasqualin S, Souza MP, et al. Functional recovery of elderly patients with surgically-treated intertrochanteric fractures: preliminary results of a randomised trial comparing the dynamic hip screw and proximal femoral nail techniques. Injury 2014; 45: S26–S31. [DOI] [PubMed] [Google Scholar]
- 6.Huang X, Leung F, Xiang Z, et al. Proximal femoral nail versus dynamic hip screw fixation for trochanteric fractures: a meta-analysis of randomized controlled trials. Scientific World J 2013; 2013: 805805–805805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hwang JH, Oh JK, Han SH, et al. Mismatch between PFNa and medullary canal causing difficulty in nailing of the pertrochanteric fractures. Arch Orthop Trauma Surg 2008; 128: 1443–1446. [DOI] [PubMed] [Google Scholar]
- 8.Kanakaris NK, Tosounidis TH, Giannoudis PV. Nailing Intertrochanteric Hip Fractures: Short Versus Long; Locked Versus Nonlocked. J Orthop Trauma 2015; 29(Suppl 4): S10–S16. [DOI] [PubMed] [Google Scholar]
- 9.Kazemian GH, Manafi AR, Najafi F, et al. Treatment of intertrochanteric fractures in elderly highrisk patients: Dynamic hip screw vs. external fixation. Injury 2014; 45: 568–572. [DOI] [PubMed] [Google Scholar]
- 10.Kim JW, Kim TY, Ha YC, et al. Outcome of intertrochanteric fractures treated by intramedullary nail with two integrated lag screws: a study in Asian population. Indian J Orthop 2015; 49: 436–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Little NJ, Verma V, Fernando C. A prospective trial comparing the Holland nail with the dynamic hip screw in the treatment of intertrochanteric fractures of the hip. J Bone Joint Surg Br 2008; 90: 1073–1078. [DOI] [PubMed] [Google Scholar]
- 12.Ma J, Xing D, Ma X, et al. The percutaneous compression plate versus the dynamic hip screw for treatment of intertrochanteric hip fractures: a systematic review and meta-analysis of comparative studies. Orthop Traumatol Surg Res 2012; 98: 773–783. [DOI] [PubMed] [Google Scholar]
- 13.Ma KL, Wang X, Luan FJ, et al. Proximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: a meta-analysis. Orthop Traumatol Surg Res 2014; 100: 859–866. [DOI] [PubMed] [Google Scholar]
- 14.Matre K, Havelin LI, Gjertsen JE, et al. Intramedullary nails result in more reoperations than sliding hip screws in two-part intertrochanteric fractures. Clin Orthop Relat Res 2013; 471: 1379–1386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matre K, Vinje T, Havelin LI, et al. TRIGEN INTERTAN intramedullary nail versus sliding hip screw a prospective, randomized multicenter study on pain, function, and complications in 684 patients with an intertrochanteric or subtrochanteric fracture and one year of follow-up. J Bone Joint Surg Am 2013; 95: 200–208. [DOI] [PubMed] [Google Scholar]
- 16.Mavrogenis AF, Panagopoulos GN, Megaloikonomos PD, et al. Complications after hip nailing for fractures. Orthopedics 2016; 39: e108–e116. [DOI] [PubMed] [Google Scholar]
- 17.Menezes DF, Gamulin A, Noesberger B. Is the proximal femoral nail a suitable implant for treatment of all trochanteric fractures? Clin Orthop Relat Res 2005; 439: 221–227. [DOI] [PubMed] [Google Scholar]
- 18.Mereddy P, Kamath S, Ramakrishnan M, et al. The AO/ASIF proximal femoral nail antirotation (PFNA): A new design for the treatment of unstable proximal femoral fractures. Injury 2009; 40: 428–432. [DOI] [PubMed] [Google Scholar]
- 19.Niu E, Yang A, Harris AH, et al. Which fixation device is preferred for surgical treatment of intertrochanteric hip fractures in the united states? a survey of orthopaedic surgeons. Clin Orthop Relat Res 2015; 473: 3647–3655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Oken OF, Soydan Z, Yildirim AO, et al. Performance of modified anatomic plates is comparable to proximal femoral nail, dynamic hip screw and anatomic plates: Finite element and biomechanical testing. Injury 2011; 42: 1077–1083. [DOI] [PubMed] [Google Scholar]
- 21.Ozkayin N, Okcu G, Aktuglu K. Intertrochanteric femur fractures in the elderly treated with either proximal femur nailing or hemiarthroplasty: a prospective randomised clinical study. Injury 2015; 46(Suppl 2): S3–S8. [DOI] [PubMed] [Google Scholar]
- 22.Radcliff TA, Regan E, Cowper Ripley DC, et al. Increased use of intramedullary nails for intertrochanteric proximal femoral fractures in veterans affairs hospitals a comparative effectiveness study. J Bone Joint Surg Am 2012; 94: 833–840. [DOI] [PubMed] [Google Scholar]
- 23.Sahin O, Demirors H, Akgun R, et al. Dynamic hip screw versus proximal femoral nail for treatment of trochanteric hip fractures: an outcome analyses with a minimum 2 years of follow-up. Eur J Orthop Surg Traumatol 2012; 22: 473–480. [Google Scholar]
- 24.Said GZ, Farouk O, El-Sayed A, et al. Salvage of failed dynamic hip screw fixation of intertrochanteric fractures. Injury 2006; 37: 194–202. [DOI] [PubMed] [Google Scholar]
- 25.Saudan M, Lubbeke A, Sadowski C, et al. Pertrochanteric fractures: Is there an advantage to an intramedullary nail? A randomized, prospective study of 206 patients comparing the dynamic hip screw and proximal femoral nail. J Orthop Trauma 2002; 16: 386–393. [DOI] [PubMed] [Google Scholar]
- 26.Seyhan M, Turkmen I, Unay K, et al. Do PFNA devices and Intertan nails both have the same effects in the treatment of trochanteric fractures? A prospective clinical study. J Orthop Sci 2015; 20: 1053–1061. [DOI] [PubMed] [Google Scholar]
- 27.Shen L, Zhang Y, Shen Y, et al. Antirotation proximal femoral nail versus dynamic hip screw for intertrochanteric fractures: A meta-analysis of randomized controlled studies. Orthop Traumatol Surg Res 2013; 99: 377–383. [DOI] [PubMed] [Google Scholar]
- 28.Weiser L, Ruppel AA, Nuechtern JV, et al. Extra- vs. intramedullary treatment of pertrochanteric fractures: a biomechanical in vitro study comparing dynamic hip screw and intramedullary nail. Arch Orthop Trauma Surg 2015; 135: 1101–1106. [DOI] [PubMed] [Google Scholar]
- 29.Xu YZ, Geng DC, Mao HQ, et al. A comparison of the proximal femoral nail antirotation device and dynamic hip screw in the treatment of unstable pertrochanteric fracture. J Int Med Res 2010; 38: 1266–1275. [DOI] [PubMed] [Google Scholar]
- 30.Raviraj A, Anand A, Chakravarthy M, et al. Proximal femoral nail antirotation (PFNA) for treatment of osteoporotic proximal femoral fractures. Eur J Orthop Surg Traumatol 2012; 22: 301–305. [Google Scholar]
- 31.Yu W, Zhang X, Zhu X, et al. A retrospective analysis of the InterTan nail and proximal femoral nail anti-rotation-Asia in the treatment of unstable intertrochanteric femur fractures in the elderly. J Orthop Surg Res 2016; 11: 10–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang K, Zhang S, Yang J, et al. Proximal femoral nail vs. Dynamic hip screw in treatment of intertrochanteric fractures: a meta-analysis. Med Sci Monit 2014; 20: 1628–1633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhou Z, Zhang X, Tian S, et al. Minimally invasive versus conventional dynamic hip screw for the treatment of intertrochanteric fractures in older patients. Orthopedics 2012; 35: E244–E249. [DOI] [PubMed] [Google Scholar]
- 34.Zou J, Xu Y, Yang H. A comparison of proximal femoral nail antirotation and dynamic hip screw devices in trochanteric fractures. J Int Med Res 2009; 37: 1057–1064. [DOI] [PubMed] [Google Scholar]