Abstract
Objective
To compare the effects of saddle, lumbar epidural and caudal blocks on anal sphincter tone using anorectal manometry.
Methods
Patients undergoing elective anorectal surgery with regional anaesthesia were divided randomly into three groups and received a saddle (SD), lumbar epidural (LE), or caudal (CD) block. Anorectal manometry was performed before and 30 min after each regional block. The degree of motor blockade of the anal sphincter was compared using the maximal resting pressure (MRP) and the maximal squeezing pressure (MSP).
Results
The study analysis population consisted of 49 patients (SD group, n = 18; LE group, n = 16; CD group, n = 15). No significant differences were observed in the percentage inhibition of the MRP among the three regional anaesthetic groups. However, percentage inhibition of the MSP was significantly greater in the SD group (83.6 ± 13.7%) compared with the LE group (58.4 ± 19.8%) and the CD group (47.8 ± 16.9%). In all groups, MSP was reduced significantly more than MRP after each regional block.
Conclusions
Saddle block was more effective than lumbar epidural or caudal block for depressing anal sphincter tone. No differences were detected between lumbar epidural and caudal blocks.
Keywords: Anorectal surgery, saddle block, caudal block, lumbar epidural block, anal sphincter tone, anorectal manometry
Introduction
Surgical procedures for haemorrhoids and other minor anorectal disorders account for a large proportion of elective ambulatory surgery.1 Anorectal surgery requires deep anaesthesia because the region is innervated by multiple nerves and it is a reflexogenic zone.2 Although each method has its advantages and drawbacks, saddle, lumbar epidural, and caudal blocks are regional anaesthetic techniques considered well tolerated and reliable for anorectal surgery.3–5
Several methods have been introduced in an attempt to quantify motor blockade but they have limited practicability and are unfeasible in some clinical situations6 such as evaluating anal muscle tone.3 The degree of motor block associated with regional anaesthesia has traditionally been assessed using the Bromage scale or modified Bromage scale.7,8 However, the information obtained by observing the movements of the muscles included in this scale (i.e., hip, knee, and foot) does not accurately reflect the motor blockade that affects the anal muscle. Often in clinical practice, the anaesthesiologist or surgeon, test anorectal motor block by palpating the patient’s anus but it is difficult to quantify the degree of motor blockade using this subjective method.5
Epidural local anaesthesia does not produce anaesthetic effects uniformly across the spinal segments.9 One of the factors that can affect the blockade is the size of the nerve root. For example, the large size of the L5 and S1 nerve roots may cause resistance to the local anaesthetic effect.10 Interestingly, it has been reported that the sensory blockade of S3 is easier than that of S1 and as rapid as that of L2 in a lumbar epidural block.11 Moreover, the same study concluded that the efficacy of a lumbar epidural block is comparable with a caudal block.11 However, the authors evaluated motor blockade using the Bromage scale and did not quantify the anal motor block. To our knowledge, no objective investigation has compared saddle, lumbar epidural and caudal blocks in a prospective, randomized study. The lack of a comparative study and adequate information on the potency of paralysing the anal sphincter with these regional anaesthetic techniques prompted us to examine if significant differences in anal motor block existed using the three different methods. Anorectal manometry, with the use of a continuous water perfusion system, was used to assess the tone of the anal sphincter muscles.
Patients and methods
Study design and patient population
The prospective, randomized, comparative study took place in the Department of Anaesthesiology and Pain Medicine, Kangwon National University Hospital, Gangwon-Do, Republic of Korea between 05 December 2013 and 27 June 2014. Adult patients, aged 16–65 years, scheduled for elective anal surgery with regional anaesthesia and American Society of Anaesthesiologists physical status I or II were eligible for the study.12 Exclusion criteria were as follows: (i) a known allergy to local anaesthetics; (ii) the presence of a neuromuscular disorder; (iii) contraindications to regional anaesthesia; (iv) morbid obesity (i.e., body mass index > 30 kg/m2).
A computer-generated random number table was used to assign patients to one of the following three regional anaesthetic groups: saddle (SD), lumbar epidural (LE), or caudal (CD). The study was approved by the Institutional Review Board of Kangwon National University Hospital (Ref: Imsang 07–05) and all patients provided written informed consent prior to enrolment.
Anaesthetic procedures
Patients did not receive any premedication. Electrocardiograms, heart rate and oxygen saturation were monitored before the block and thereafter continuously throughout the study.
In the SD group, the subarachnoid space was entered using a 25-gauge Quinke spinal needle (Insung, Seoul, Korea) at the L3–4 interspace with the patient in the sitting position. After confirming the free flow of cerebrospinal fluid, 1 ml of 0.5% bupivacaine (5 mg) in 8% glucose solution (Marcain; AstraZeneca, Södertälje, Sweden) was administered. The patient remained in the sitting position for 5 min after the local anaesthetic injection. Subsequently, the patient was moved to the supine position.
For the LE and CD groups, the anaesthetic solution was lidocaine-epinephrine-bicarbonate (20 ml of lidocaine 2% plus epinephrine [1:200 000] plus 2 ml of sodium bicarbonate 8.4%, which was added immediately before administration). In the LE group, the epidural space was identified using an 18-gauge Tuohy needle (Perifix®; B Braun, Melsungen, Germany) with its bevel facing caudally via the midline approach at the L4–5 interspace using the loss-of-resistance-to-air technique. Subsequently, a 22-gauge multi-orifice catheter was placed 3 cm into the epidural space in the lateral position. After taping the catheter and filter, 3 ml of 2% lidocaine with epinephrine (1: 200 000) were administered via the epidural catheter as a test dose. If no evidence of intravascular or subarachnoid injection appeared, an additional 12 ml of the anaesthetic solution was injected through the catheter over 1 min. In the CD group, the patients were placed in the lateral position and an 18-gauge Tuohy needle was inserted into the caudal space through the sacrococcygeal ligament. If no blood or cerebrospinal fluid was aspirated, a caudal injection of 15 ml of the anaesthetic solution was given through the needle. All patients in the LE and CD groups were moved into supine position following the anaesthetic injection and remained in the supine position for 20 min. To avoid inter-operator variability, one staff anaesthesiologist (S.S.K.) performed all of the blocks.
In all patients, the level of sensory analgesia was evaluated on the torso and lower extremity at 5-min intervals for 30 min after injecting the local anaesthetic. The anatomical landmarks and correlated dermatome levels were standardized for testing as follows: the umbilicus (T10), inguinal crease (L1), anterior thigh (L2), medial knee (L3), medial malleolus (L4), the dorsum web between first and second toe (L5), the lateral heel (S1), and the medial popliteal fossa (S2). The assessment was based on the loss of cold sensation to a cotton wool swab soaked in absolute alcohol by an independent assessor blinded to the anaesthetic treatment group.
Anal intraluminal pressure measurements
Anal intraluminal pressure was evaluated using water perfused anorectal manometry pre-block and post-block. The pre-block assessment was performed 1–2 h before regional anaesthesia and the post-block assessment was taken 30 min after regional anaesthesia.13 The patients had no bowel preparation before manometry. The anal sphincter pressures were measured using a 3-lumen, water-perfused catheter and pneumohydraulic capillary infusion system (R3B & PIP4-4; Mui Scientific, Mississauga, Ontario, Canada) connected to a computerized software program (MMS Database; Medical Measurement Systems, Enschede, The Netherlands). The catheter had three ports spaced 0.5 cm apart for the two proximal holes and each lumen was perfused with sterile degassed water at 0.1 ml/min. The sphincter was identified using the slow station pull-through technique.14 For the pre-block measurement, the location of the catheter was verified using the pressure increase observed during pull-through and during a voluntary squeeze and the same position was used for the post-block measurement. After the patient was comfortable and the manometric trace had stabilized, the recording was started. The patient was then instructed to contract the anal sphincter maximally for 15 s on three separate occasions 1 min apart and the average value of 3 consecutive measurements was taken for the analysis. While relaxing and squeezing, the maximal resting (MRP) and squeezing (MSP) pressures of the anus were observed. The amount of inhibition caused by anaesthesia (i.e., the pressure drop in the anal canal) was expressed as the percentage of the resting and squeezing pressures. The percentage inhibition for MRP or MSP was calculated as follows:
All anorectal manometry measurements were performed by a fully trained independent physician blinded to the anaesthetic procedures. To ensure study blindness, the area from the lumbar vertebrae to the sacrococcygeal ligament was covered with the cotton gauze. All procedures and measurements were performed in the same manometric study room.
After the manometric measurements were taken, all patients were moved to operating room and anal surgery was undertaken with the patient in the prone position. During the operation, the patients were sedated with intravenous administration of midazolam (1–3 mg).
Statistical analyses
The sample size was based on estimates from our pilot study in which the mean percentage inhibition of the MRP was 21.2, 31.3, and 29.2% for saddle, lumbar epidural, and caudal blocks, respectively. The standard deviation was 8.6%. Therefore, approximately 45 patients (15 in each group) were required to achieve 80% power to detect a difference of 10% inhibition of MRP among the means using one-way analysis of variance (ANOVA) at the 0.05 significance level. For the same variables, an expected difference of 8% inhibition of MSP generated a similar sample size. Patients with inadequate blockade after the administration of local anaesthetic were recorded as failures and excluded from the post-anaesthetic evaluation. To allow for drop-outs, a sample size of at least 18 patients per group was chosen.
All statistical analyses were performed using the SPSS® statistical package, version 19.0 (SPSS Inc., Chicago, IL, USA) for Windows®. Differences among the groups were analysed using one-way ANOVA or nonparametric Kruskal–Wallis test, as appropriate. Manometric data among the groups were compared using ANOVA and if significant results were obtained the post hoc Scheffé test was used.15 Within-group comparisons were made using the paired t-test. P-values < 0.05 were considered statistically significant.
Results
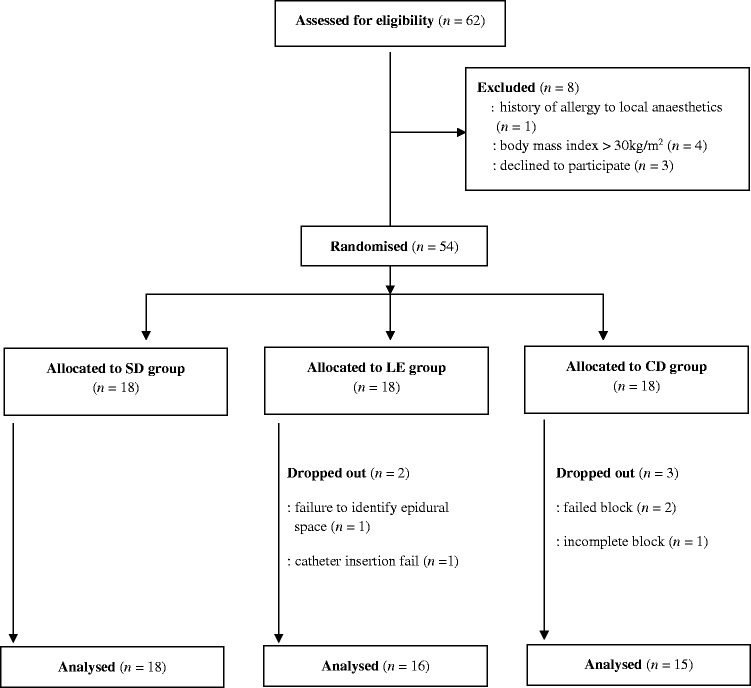
Of the 62 patients who were assessed for eligibility, 54 were randomized to one of the three regional anaesthesia groups. Reasons for exclusion are shown in Figure 1. In the LE group, the lumbar epidural technique was successful in all but two patients (failure to identify epidural space and catheter insertion failure) and in the CD group three patients (failed block in two patients and incomplete block in one patient) had to be excluded from the analysis. Therefore, the study analysis population consisted of 49 patients (SD group, n = 18; LE group, n = 16; CD group, n = 15). No statistically significant differences were detected among the three groups in terms of age, height, weight or sex distribution (Table 1). The anaesthesia level in the LE group was statistically significantly higher than in the SD and CD groups (P < 0.01 for both comparisons) (Table 1). All the operations were performed successfully without any need for additional intervention or analgesics.
Figure 1.
Flow diagram showing patient numbers at various stages in the prospective, randomized, comparative study of the effects of saddle (SD), lumbar epidural (LE) and caudal (CD) blocks on anal sphincter pressure.
Table 1.
Clinical and demographic characteristics of patients (n = 49) who participated in this study to compare the effects of saddle, lumbar epidural and caudal blocks on anal sphincter tone.
| Regional anaesthesia group |
|||
|---|---|---|---|
| Saddle block (n = 18) | Lumbar epidural block (n = 16) | Caudal block (n = 15) | |
| Age, years | 35.8 ± 18.7 | 37.9 ± 18.1 | 39.8 ± 13.4 |
| Height, cm | 164.1 ± 9.5 | 161.7 ± 8.8 | 163.0 ± 7.3 |
| Weight, kg | 62.1 ± 10.1 | 64.5 ± 8.2 | 63.3 ± 9.0 |
| Male/female | 10/8 | 9/7 | 7/8 |
| Diagnosis† | |||
| Haemorrhoids | 9 | 8 | 7 |
| Anal fissure | 6 | 5 | 5 |
| Anal fistula | 4 | 6 | 4 |
| Anaesthesia level | L1 (T10–L2) | T11 (T8–L1)* | L2 (T12–L3) |
Data are presented as mean ± SD or n of patients. Anaesthesia level is shown as median (range).
Some patients had two or more preoperative anal diseases.
P < 0.01 compared with groups SD and CD; nonparametric Kruskal–Wallis test.
No statistically significant differences were observed in the pre-block MRP and MSP values among the three regional anaesthetic groups (Tables 2 and 3). However, within each group, the values for MRP and MSP after regional block had decreased significantly compared with the pre-block values (P < 0.05 for all comparisons).
Table 2.
Maximal resting anal pressure measured by anorectal manometry pre- and post-block with regional anaesthesia.
| Maximal resting pressure |
|||
|---|---|---|---|
| Saddle block (n = 18) | Lumbar epidural block (n = 16) | Caudal block (n = 15) | |
| Pre-block, mmHg | 79.7 ± 14.3 | 77.2 ± 20.3 | 74.7 ± 14.3 |
| Post-block, mmHg | 61.5 ± 17.7* | 50.7 ± 19.6* | 54.1 ± 21.3* |
| Mean difference, mmHg | 19.2 (8.7–29.8) | 22.3 (6.9–37.8) | 20.9 (5.9–36.0) |
Values are the mean ± SEM. Mean differences are the mean (95% confidence interval).
P < 0.05 compared with pre-block in each group; paired t-test.
Table 3.
Maximal squeezing anal pressure measured by anorectal manometry pre- and post-block with regional anaesthesia.
| Maximal squeezing pressure |
|||
|---|---|---|---|
| Saddle block (n = 18) | Lumbar epidural block (n = 16) | Caudal block (n = 15) | |
| Pre-block, mmHg | 85.1 ± 29.8 | 93.2 ± 38.0 | 86.7 ± 33.7 |
| Post-block, mmHg | 16.6 ± 11.7* | 40.8 ± 19.6* | 45.1 ± 18.4* |
| Mean difference, mmHg | 70.4 (42.2–98.6) | 54.4 (32.8–75.9) | 40.1 (17.4–57.5) |
Values are the mean ± SEM. Mean differences are the mean (95% confidence interval).
P < 0.05 compared with pre-block in each group; paired t-test.
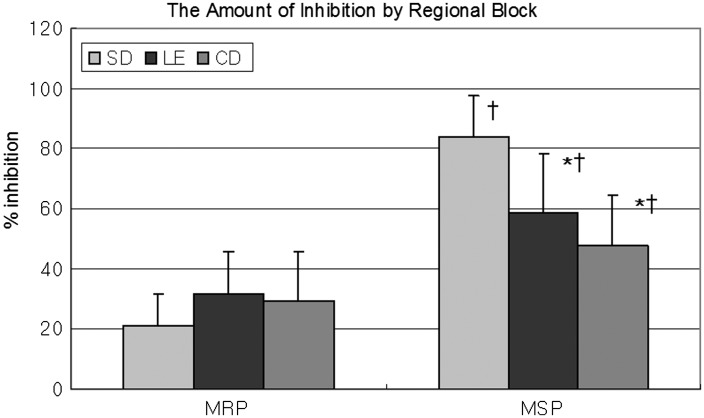
The mean ± SEM percentage inhibitions of MRP with regional block were 21.2 ± 10.5%, 31.4 ± 14.1%, and 29.2 ± 16.4% in the SD, LE, and CD groups, respectively (Figure 2). Although there were no statistically significant differences between groups in the percentage inhibition of MRP, the percentage inhibition of MSP was significantly greater in the SD group (83.6 ± 13.7%) compared with the LE group (58.4 ± 19.8%) and the CD group (47.8 ± 16.9%) (P < 0.05 for both comparisons) (Figure 2). No difference was observed between the LE and CD groups. For all groups, the percentage inhibition in MSP after each regional block was significantly greater than for the MRP (P < 0.05 for all comparisons) (Figure 2).
Figure 2.
Percentage inhibition of maximum resting pressure (MRP) and maximum squeezing pressure (MSP) measured by anorectal manometry following regional anaesthetic block. The amount of inhibition caused by the regional anaesthesia (i.e., the pressure drop in the anal canal) was expressed as the percentage of the resting and squeezing pressures. Values are mean ± SEM. *P < 0.05 compared with the SD group, †P < 0.05 compared with MRP. SD, saddle block; LE, lumbar epidural block; CD, caudal block.
Discussion
Anorectal manometry is a simple, non-invasive and reproducible method of measuring luminal pressures within the anal canal.16 The technique is now widely used as a surrogate measure of anal sphincter tone.16,17 The MRP in the anal canal is at its highest level when the patient is at rest. The resting tone of the internal anal sphincter contributes 85% to the MRP and the resting tone of the external anal sphincter 15%.11 The MSP in the anal canal is at its highest pressure during squeezing and starts from a baseline represented by the maximal resting tone. The MSP is related to the activity of the striated sphincters (i.e., the external sphincter and the puborectalis muscle).
The principal finding of this study was that saddle block was the most effective technique for decreasing MSP. In addition, the reductions in MSP following lumbar epidural or caudal block were similar. Also, the decrease in MRP was similar for all types of anaesthetic technique. These current findings support the results of a study that found surgeons who were blinded to the anaesthetic method rated spinal anaesthesia better than epidural anaesthesia for minor non-obstetric surgery.18
The complex innervation of the anal zone (i.e., autonomic versus spinal) may explain the differences that this present study found between the regional anaesthetics in the anorectal manometry results. The internal anal sphincter is under autonomic control via sympathetic innervation from the hypogastric plexus, which initiates tonic contraction, and via sacral parasympathetic fibres that mediate anorectal muscle relaxation. The external sphincter, which is supplied by the inferior rectal branch of the internal pudendal nerve and the perineal branch of the fourth sacral nerve, is under voluntary control.19 The decrease in the MRP after each block is probably due to sympathetic blockade. Therefore, the difference that this current study observed between the reductions in MSP and MRP may have been the result of partial, incomplete sympathetic blockade. In this present study, the level of analgesia ranged from T10 to L2 (SD group), T8 to L1 (LE group) and T12 to L3 (CD group). Considering the innervation of this region and the sensory level that was observed with each block, partial sympathetic blockade of the hypogastric plexus was a probable cause for the differences that were found between the regional anaesthetics in this study.
With a spinal block, sympathetic blockade is present two or three levels above the level of the sensory blockade, whereas with an epidural block the level of sympathetic blockade is the same as, or lower than the sensory block.9 The hypogastric plexus contracts the internal anal sphincter and receives its sympathetic innervation from preganglionic fibres, which have their cell bodies in the lower thoracic and upper lumbar segments.20 Another possible explanation for the differences that were found with the three regional anaesthetics in the anorectal manometry results in the present study is incomplete sympathetic blockade that might happen in the dermatomal segments when analgesia is present. For example, one study showed that despite a blockade sufficient for surgical anaesthesia, it was difficult to achieve a complete sympathetic blockade with a spinal or epidural block using clinical doses of local anaesthetics.21
Although caudal block is widely used for anorectal surgery, its success rate has been reported to be only 70–80%.22–24 Despite a highly experienced staff anaesthesiologist performing the procedure in the present study, three of the 18 caudal blocks were unsuccessful. Caudal block failure is often related to anatomic variations of the bony sacrum and the soft tissues over the bone, which include displacement of the hiatus, narrowing of the sacral canal, and ossification of the sacrococcygeal membrane that can occur especially in the elderly.25 In addition, following caudal entry to the epidural space, the cephalad spread of the drug may be limited by minor bony obstructions that will result in the blockade of limited segments.25
In our institute, saddle block is the most commonly performed regional anaesthetic technique for anal surgery, since it provides rapid-onset, dense block and usually takes a short time to perform.26 Caudal block is used as an alternative to saddle block in cases where dural puncture is to be avoided (e.g., patients with a history of post-dural puncture headache, increased intracranial pressure). However, as mentioned previously, caudal block in adults is often difficult because of anatomical variability. Also, we noted that the sacral spread of anaesthetic following the lumbar epidural block was sufficient to block sacral segments for anal surgery. Therefore, lumbar epidural block rather than caudal block may be a better choice in cases where saddle block cannot be used.
The present study had several limitations. First, the exact level of sympathetic blockade was not checked and although measuring the level would have provided more detail, it was not the primary objective of the study. Moreover, there is some debate concerning the evaluative methods for sympathetic blockade.27–30 Secondly, the direction of the epidural catheter was not confirmed radiologically. One study showed that the initial injection of a local anaesthetic solution through a caudally oriented epidural catheter results in a large spread of anaesthesia through the sacral area.31 Although the bevel of the epidural needle was placed caudally, it did not ensure caudal advance. However, another study showed that the injection of a local anaesthetic solution through a lumbar epidural catheter oriented caudally resulted in a faster onset and superior quality of anaesthesia in comparison with a cephalad-oriented catheter in ankle surgery (operating site innervated mainly by S1), but not in haemorrhoidectomy (by S3–5).32 This interesting difference between the two aforementioned studies implies that although more anaesthetic pooled in the sacral area with the caudally oriented lumbar epidural catheter, sensory analgesia with a lumbar epidural block for the area innervated by the sacral nerve (excluding S1, the blockade of which is often delayed due to the larger size of this root8) is not affected by the direction of spread of the local anaesthetic.31,32 In this present study, it remains unclear as to whether the direction of the epidural catheter affected manometric changes within the LE group. Theoretically, we would suggest that more caudal spread of the local anaesthetic with a caudally directed catheter should result in a difference in the degree of motor blockade in the lower sacral area. Finally, different local anaesthetics were used in the three treatment groups; hyperbaric bupivacaine was used for spinal anaesthesia and lidocaine for the LE and CD groups. A significantly higher motor blockade has been reported with lidocaine than with bupivacaine.30 However, the focus of this present study was to make a clinically oriented comparison of the three anaesthetic techniques in a normal clinical practice setting. In addition, several case reports and animal studies have suggested that spinal lidocaine may result in a greater incidence of neurological complications compared with other local anaesthetics.33,34
In conclusion, this prospective, randomized, comparative study used anorectal manometry to demonstrate that saddle block was more effective than lumbar epidural or caudal block for depressing anal sphincter tone. No differences were detected between the lumbar epidural and caudal blocks.
Declaration of conflicting interests
The authors declare that there are no conflicts of interest.
Funding
This work was supported by a 2014 Kangwon National University research grant (no. 120140659).
References
- 1.Li S, Coloma M, White PF, et al. Comparison of the costs and recovery profiles of three anesthetic techniques for ambulatory anorectal surgery. Anesthesiology 2000; 93: 1225–1230. [DOI] [PubMed] [Google Scholar]
- 2.Erdman AG. Concise anatomy for anaesthesia, Cambridge, UK: Cambridge University Press, 2001. [Google Scholar]
- 3.Davies SJ, Paech MJ, Welch H, et al. Maternal experience during epidural or combined spinal-epidural anesthesia for cesarean section: a prospective, randomized trial. Anesth Analg 1997; 85: 607–613. [DOI] [PubMed] [Google Scholar]
- 4.Karaman S, Akercan F, Akarsu T, et al. Comparison of the maternal and neonatal effects of epidural block and of combined spinal-epidural block for Caesarean section. Eur J Obstet Gynecol Reprod Biol 2005; 121: 18–23. [DOI] [PubMed] [Google Scholar]
- 5.Verghese ST, Mostello LA, Patel RI, et al. Testing anal sphincter tone predicts the effectiveness of caudal analgesia in children. Anesth Analg 2002; 94: 1161–1164. [DOI] [PubMed] [Google Scholar]
- 6.Graham AC, McClure JH. Quantitative assessment of motor block in labouring women receiving epidural analgesia. Anaesthesia 2001; 56: 470–476. [DOI] [PubMed] [Google Scholar]
- 7.Breen TW, Shapiro T, Glass B, et al. Epidural anesthesia for labor in an ambulatory patient. Anesth Analg 1993; 77: 919–924. [DOI] [PubMed] [Google Scholar]
- 8.Bromage PR. Epidural analgesia, Philadelphia: WB Saunders, 1978. [Google Scholar]
- 9.Cousins MJ, Veering BT. Epidural neural blockade. In: Cousins MJ, Bridenbaugh PO. (eds). Neural blockade in clinical anesthesia and management of pain, 3rd ed Philadelphia: JB Lippincott, 1998, pp. 243–321. [Google Scholar]
- 10.Hogan Q. Size of human lower thoracic and lumbosacral nerve roots. Anesthesiology 1996; 85: 37–42. [DOI] [PubMed] [Google Scholar]
- 11.Arakawa M, Aoyama Y, Ohe Y. Block of the sacral segments in lumbar epidural anaesthesia. Br J Anaesth 2003; 90: 173–178. [DOI] [PubMed] [Google Scholar]
- 12.American Society of Anesthesiologists®. ASA PHYSICAL STATUS CLASSIFICATION SYSTEM. Last approved by the ASA House of Delegates on October 15, 2014, https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system (2014, assessed 12 September 2016).
- 13.Lin JK. Anal manometric studies in hemorrhoids and anal fissures. Dis Colon Rectum 1989; 32: 839–842. [DOI] [PubMed] [Google Scholar]
- 14.Sainio P, Husa A. A prospective manometric study of the effect of anal fistula surgery on anorectal function. Acta Chir Scand 1985; 151: 279–288. [PubMed] [Google Scholar]
- 15.McHugh ML. Multiple comparison analysis testing in ANOVA. Biochem Med (Zagreb) 2011; 21: 203–209. [DOI] [PubMed] [Google Scholar]
- 16.Bharucha AE, Seide B, Fox JC, et al. Day-to-day reproducibility of anorectal sensorimotor assessments in healthy subjects. Neurogastroenterol Motil 2004; 16: 241–250. [DOI] [PubMed] [Google Scholar]
- 17.Karoui S, Boubaker J and Filali A. Technical aspects and indications of anorectal manometry. Tunis Med 2005; 83: 315–319 [Article in French, English abstract]. [PubMed]
- 18.Flaatten H, Felthaus J, Larsen R, et al. Postural post-dural puncture headache after spinal and epidural anaesthesia. A randomised, double-blind study. Acta Anaesthesiol Scand 1998; 42: 759–764. [DOI] [PubMed] [Google Scholar]
- 19.Nivatvongs S, Gordon PH. Surgical anatomy. In: Gordon PH, Nivatvongs S. (eds). Principles and practice of surgery for the colon, rectum, and anus, St. Louis: Quality Medical, 1992, pp. 3–37. [Google Scholar]
- 20.Waldman SD. Pain review. 2nd ed, Philadelphia: Elsevier Health Sciences; 2009.
- 21.Stevens RA, Beardsley D, White JL, et al. Does spinal anesthesia result in a more complete sympathetic block than that from epidural anesthesia? Anesthesiology 1995; 82: 877–883. [DOI] [PubMed] [Google Scholar]
- 22.White A, Derby R, Wynne G. Epidural injections for the diagnosis and treatment of low-back pain. Spine 1980; 5: 78–86. [DOI] [PubMed] [Google Scholar]
- 23.Price C, Rogers P, Prosser A, et al. Comparison of the caudal and lumbar approaches to the epidural space. Annals Rheum Dis 2000; 59: 879–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Stitz M, Sommer H. Accuracy of blind versus fluoroscopically guided caudal epidural injection. Spine 1999; 24: 1371–1376. [DOI] [PubMed] [Google Scholar]
- 25.Willis R. Caudal epidural blockade. In: Cousins MJ, Bridenbaugh PO. (eds). Neural blockade in clinical anesthesia and management of pain, 3rd ed Philadelphia: Lippincott-Raven, 1998, pp. 323–342. [Google Scholar]
- 26.Ng K, Parsons J, Cyna AM, et al. Spinal versus epidural anaesthesia for caesarean section. Cochrane Database Syst Rev 2004; 2: CD003765–CD003765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chamberlain DP, Chamberlain BD. Changes in skin temperature of the trunk and their relationship to sympathetic blockade during spinal anesthesia. Anesthesiology 1986; 65: 139–143. [DOI] [PubMed] [Google Scholar]
- 28.Gibbons JD. Non-parametric methods for quantitative analysis, 2nd ed Columbus: American, 1988. [Google Scholar]
- 29.Greene NM, Brull SJ. Physiology of spinal anesthesia, 4th ed Baltimore: Lippincott Williams and Wilkins, 1993, pp. 21–40. [Google Scholar]
- 30.Greene NM. The area of differential spinal block during spinal anesthesia with hyperbaric tetracaine. Anesthesiology 1958; 19: 45–50. [DOI] [PubMed] [Google Scholar]
- 31.Asato F, Hirakawa N, Araki K, et al. A technique for obtaining successful sacral spread with continuous lumbar epidural anesthesia. Anesth Analg 1990; 70: 662–664. [DOI] [PubMed] [Google Scholar]
- 32.Chou WY, Hsu CJ, Cheng JT, et al. Anesthetic effect of epidural anesthesia with cephalad or caudad catheterization for ankle surgery or hemorrhoidectomy. Acta Anaesthesiol Scand 2005; 49: 406–410. [DOI] [PubMed] [Google Scholar]
- 33.Johnson ME. Potential neurotoxicity of spinal anesthesia with lidocaine. Mayo Clin Proc 2000; 75: 921–932. [DOI] [PubMed] [Google Scholar]
- 34.Sakura S, Kirihara Y, Muguruma T, et al. The comparative neurotoxicity of intrathecal lidocaine and bupivacaine in rats. Anesth Analg 2005; 101: 541–547. [DOI] [PubMed] [Google Scholar]