Abstract
Objective
To evaluate the effects of an ultrasound-guided transverse abdominis plane (US-TAP) block used for postoperative pain relief by comparing the efficacy of two different volumes/concentrations of the local anaesthetic bupivacaine in patients undergoing laparoscopic cholecystectomies.
Methods
This randomized study enrolled patients undergoing laparoscopic cholecystectomies. They were randomized to two groups: group A received a 20 ml US-TAP block (50 mg bupivacaine +10 ml saline solution) and group B received a 30 ml US-TAP block (50 mg bupivacaine + 20 ml saline solution). The intraoperative consumption of remifentanil, the requirement for postoperative rescue analgesics, patient satisfaction scores, postoperative complications, and postoperative pain as measured by a visual analogue scale at 20 min, 12 h, and 24 h were recorded.
Results
A total of 60 patients enrolled in the study. There were no differences between the two groups with respect to demographic characteristics, duration of anaesthesia and patient satisfaction scores. The intraoperative consumption of remifentanil, postoperative VAS scores (20 min, 12 h and 24 h) and the requirement for postoperative analgesics were all significantly lower in group B who received a larger volume but a lower concentration of local anaesthetic solution compared with group A.
Conclusion
A US-TAP block can form part of a balanced postoperative analgesic regimen following laparoscopic cholecystectomy.
Keywords: Ultrasound-guided, transverse abdominis plane block, laparoscopic cholecystectomy, postoperative pain
Introduction
The transversus abdominis plane (TAP) block was first defined by Rafi in 2001,1 and it is commonly used in clinical practice as part of the multimodal analgesic therapy after abdominal surgery.2 The TAP block produces a sensorial block via local anaesthetic infiltration, between the internal oblique muscle and transverse abdominis muscle, by targeting the innervating spinal nerves in this plane. This block affects thoracic intercostal nerves 7–12, the ilioinguinal nerve, the iliohypogastric nerve and lumbar nerves 1–3 in the lateral cutaneous branches.2
Although it is known that laparoscopic cholecystectomies are less painful, many patients complain of pain after the operation.3 Several methods have been used to control the postoperative pain after laparoscopic cholecystectomies, such as intravenous patient-controlled analgesia, patient-controlled thoracic epidural analgesia, and the intraperitoneal injection of local anaesthetics.4 In addition, the intraoperative use of low-pressure pneumoperitoneum technics and a warmed air supply can reduce postoperative pain scores.5
Peripheral nerve block can be used as a reliable method to reduce postoperative pain and provide sufficient analgesic management.6 When compared with the conventional TAP block technique, ultrasound-guided TAP (US-TAP) block, which provides direct ultrasonographic visualization of the anatomy during the spreading of the local anaesthetic, could serve as an alternative technique for performing a TAP block. Complications should be minimized by performing the US-TAP block because the precise location of the needle and diffusion of local anaesthetics can be observed directly using this technique.6
This present study evaluated the effects of US-TAP on pain relief by comparing two different volumes and concentrations of the local anaesthetic bupivacaine in patients undergoing laparoscopic cholecystectomies.
Patients and methods
Patient population
This randomized study prospectively enrolled patients with American Society of Anesthesiologists (ASA) physical status I–III,7 aged 18–65 years, undergoing laparoscopic cholecystectomies at the Department of General Surgery, Istanbul Kanuni Sultan Süleyman Research and Training Hospital, Istanbul, Turkey between March 2015 and April 2015. Those patients with cardiac, endocrinological or neurological diseases, those with coagulation disorders, and those with allergies to local anaesthetics, were excluded from the study. Operations that began using the laparoscopic method but were converted to open surgery for a surgical problem were also excluded. The patients were randomly allocated into two groups at study entry using the sealed envelope method: group A was treated with a 20 ml US-TAP block (50 mg bupivacaine + 10 ml saline solution) and group B with a 30 ml US-TAP block (50 mg bupivacaine + 20 ml saline solution). Demographic characteristics were recorded including age, sex and body mass index.
This study was approved by the Istanbul Kanuni Sultan Süleyman Education and Training Hospital Ethics Committee (no. 2015.3.10-7616). Written informed consent was obtained from each patient.
Surgical and anaesthetic procedures
A saline infusion was initiated at 5–7 ml/kg/h for all patients. The induction of general anaesthesia was performed by using 0.05 mg/kg midazolam intravenous (i.v.), 2–3 mg/kg propofol i.v., 2 µg/kg fentanyl i.v. and 0.6 mg/kg rocuronium i.v. Anaesthesia was maintained with remifentanil i.v., which was diluted to 50 µg/ml, started at 0.01–0.02 µg/kg/min and 2–3% sevoflurane and 50/50% O2-N2O mixture (2 ml/min fresh gas flow). Remifentanil doses were increased or decreased according to the patient’s haemodynamic response. During anaesthesia, all patients were ventilated with 6–8 ml/kg tidal volume. The blood pressure was regulated within 20% of the range of the blood pressure measured when entering the operation room by regulating the concentration of remifentanil. In addition, the end tidal carbon dioxide partial pressure was kept within the range of 35 to 40 mmHg. During laparoscopic procedures, pressurized gas insuflation was used for surgical assistance. The pressure of the gas insuflation was within 10–12 mmHg in all patients. Laparoscopic cholecystectomy was undertaken using multiple ports and all patients received laparoscopic cholecystectomy with the same technique and incision size.
When the vital signs were stabilized after endotracheal intubation, the TAP block was performed through the ultrasound-guided method, using a linear high frequency 6–18 MHz ultrasound probe (MyLab™Five; Esaote, Genoa, Italy). The blocks were performed by anaesthesiologists experienced with the technique. First, the external oblique, internal oblique and transverse abdominis muscles were displayed at the plane of the anterior axillary line, between the 12th rib and the iliac crest. A unilateral right-sided TAP block was performed using the in-plane technique, prior to skin incision, with a 21-gauge, 50-mm Stimuplex® A needle (B. Braun, Melsungen, Germany). When the tip of the needle was located in the space between the internal oblique and transverse abdominis muscles, 20 ml (50 mg 0.5% bupivacaine + 10 ml saline solution) or 30 ml (50 mg 0.5% bupivacaine + 20 ml saline solution) was injected gradually, after negative aspiration, under direct ultrasonographic visualization. Performing unilateral block would both save time and could reduce consumption of local anaesthetics.
Surgery was allowed to begin after the TAP block procedure was completed. The total consumption of remifentanil injected during the operation was recorded as the primary outcome. The anaesthesiologist who was an expert in the technique also knew the volume of local anaesthetic solution, but another anaesthesiologist who was blinded to the group allocations managed the patients. As a secondary outcome, the pain score was assessed by a physician who was blinded to the group allocations using a visual analogue scale (VAS: 0 = no pain, 10 = the most severe pain imaginable). At the end of the operation, the first assessment of pain was undertaken at 20 min. After 20 min, the patients were moved from the recovery room to the clinic and the other measurements were performed at 12 h and 24 h after the end of the operation. When the VAS was >7, 25 mg diclofenac sodium i.v. was used as a rescue analgesic. If a patient had a VAS score >7, they were identified as requiring more postoperative analgesic than other patients and the TAP block was considered to have been ineffective.
The patients were visited 24 h after the operation and asked about sensory disturbances due to pain arising from the operation site. They were also asked to rate their satisfaction for pain relief, nausea and vomiting or any disturbances about the operation (0: bad, 1: good, 2: very good). Any occurrence of complications, such as intestinal puncture, bleeding or infection, was also recorded.
Measurement of haemodynamic parameters
Median heart rate, non-invasive mean arterial blood pressure and oxygen saturation were recorded at 0, 5, 15, 30, 45, 60 min after time 0 and then every 30 min thereafter using a CARESCAPE Monitor B450 (GE Healthcare, Piscataway, NJ, USA).
Statistical analyses
All statistical analyses were performed using the SPSS® statistical package, version 17.0 (SPSS Inc., Chicago, IL, USA) for Windows®. Data are presented as mean ± SD or median (range). Data were checked for normal distribution using the SPSS® statistical package. Nonparametric tests (Mann–Whitney U-test and χ2-test) were used because the data were not normally distributed. A P-value < 0.05 was considered statistically significant.
Results
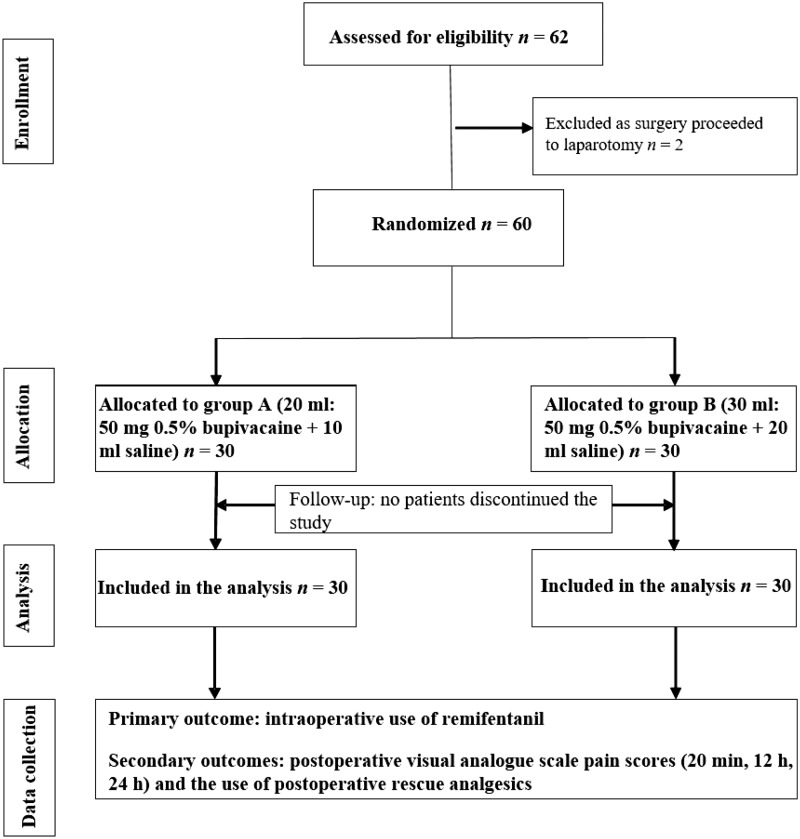
This randomized study enrolled 60 patients who were randomized to group A (n = 30) and group B (n = 30). Figure 1 shows the flow of patients through the study. There were no significant differences in the age, sex distribution, body mass index, duration of anaesthesia and ASA scores between the two groups (Table 1). The duration of surgery was significantly longer in group B compared with group A (P = 0.036).
Figure 1.
Flow diagram showing patient numbers are various stages of this randomized comparative study of the effects on pain relief of two different volumes and concentrations of the local anaesthetic bupivacaine administered via ultrasound-guided transversus abdominis plane block in patients undergoing laparoscopic cholecystectomies.
Table 1.
Baseline clinical, demographic and surgical characteristics of patients undergoing laparoscopic cholecystectomies for which the local anaesthetic bupivacaine was administered via ultrasound-guided transversus abdominis plane block.
| Characteristic | Group A n = 30 | Group B n = 30 |
|---|---|---|
| Age, years | 47.2 ± 13.0 | 46.5 ± 11.5 |
| Sex, female/male | 15/15 | 12/18 |
| Body mass index, kg/m2 | 25.0 ± 1.9 | 25.8 ± 2.1 |
| ASA physical status, I/II | 9/21 | 14/16 |
| Duration of anaesthesia, min | 65.2 ± 18.6 | 74.5 ± 20.6 |
| Duration of surgery, min | 51.7 ± 17.2 | 62.5 ± 20.8* |
Data are presented mean ± SD or n of patients.
P = 0.036 compared with group A; Mann–Whitney U-test.
ASA, American Society of Anesthesiologists.
There were no significant differences in the patient satisfaction scores between the two groups. In group A, three patients (10%) out of 30 selected ‘bad’, 18 (60%) selected ‘good’, and nine (30%) selected ‘very good’. In group B, three patients (10%) out of 30 selected ‘bad’, 10 (33%) selected ‘good’, and 17 (57%) selected ‘very good’. There were no differences in intraoperative haemodynamic parameters between the two groups (Figure 2a, 2b, and 2c). In addition, no statistically significant differences were found between the two groups with regard to the occurrence of side-effects (data not shown).
Figure 2.
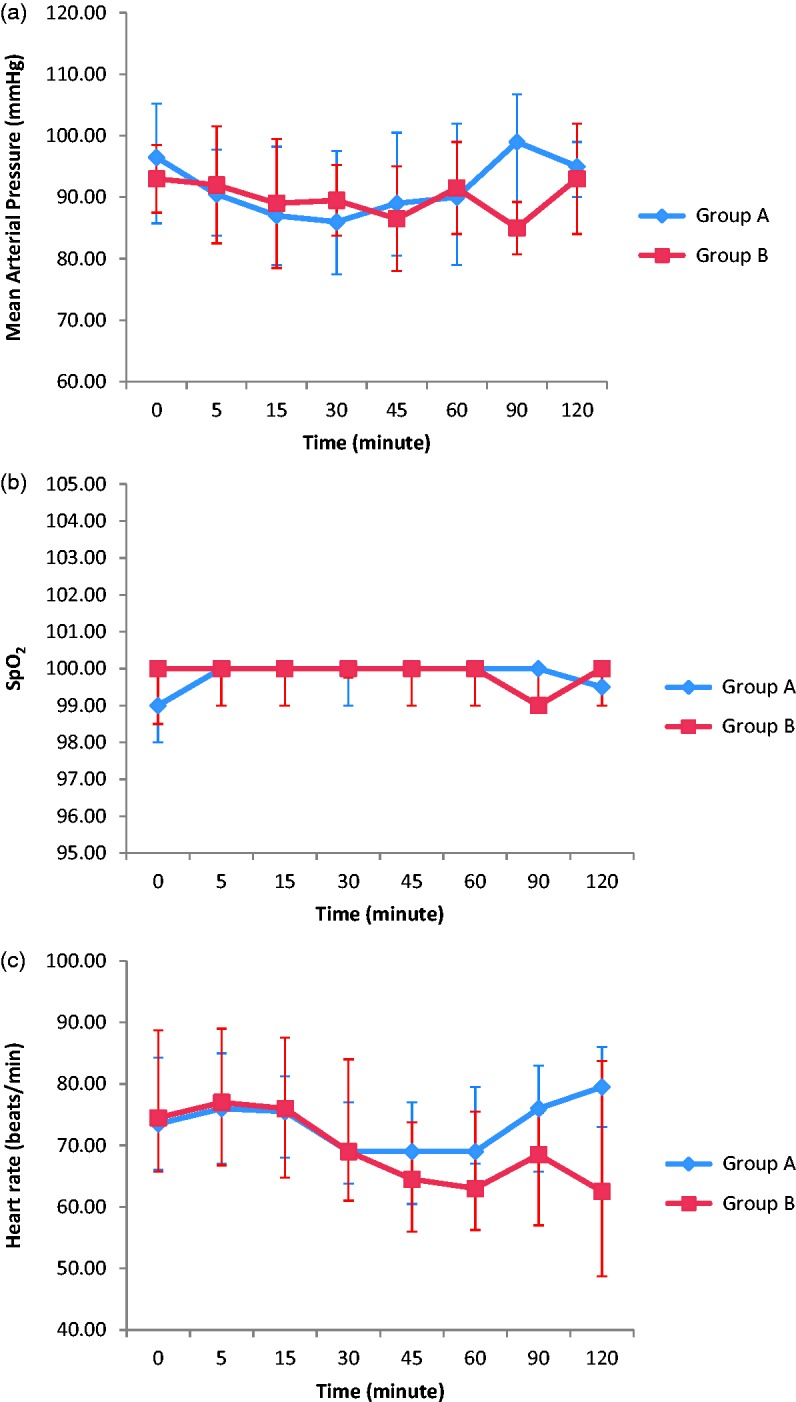
Haemodynamic parameters measured in patients undergoing laparoscopic cholecystectomies for which the local anaesthetic bupivacaine was administered via ultrasound-guided transversus abdominis plane block. (a) Median of mean arterial pressure; (b) median peripheral blood oxygen saturation (SpO2); and (c) median heart rate. Vertical bars show the 25th and 75th percentiles. The colour version of this figure is available at: http://imr.sagepub.com.
The intraoperative consumption of remifentanil was significantly lower in group B compared with group A (P = 0.002) (Table 2). The postoperative VAS scores (20 min, 12 h and 24 h) were significantly lower in group B compared with group A (P < 0.05 for all comparisons). The proportion of patients that required postoperative rescue analgesics was significantly lower in group B compared with group A (14/30 versus 21/30, respectively; P < 0.05).
Table 2.
Intraoperative consumption of remifentanil during surgery and visual analogue scale (VAS) pain scores for patients undergoing laparoscopic cholecystectomies for which the local anaesthetic bupivacaine was administered via ultrasound-guided transversus abdominis plane block.
| Group A n = 30 | Group B n = 30 | Statistical significancea | |
|---|---|---|---|
| Remifentanil dose, µg | 300 (150–500) | 250 (150–500) | P = 0.002 |
| VAS pain score | |||
| 20 min | 2.0 (0–8) | 2.0 (0–4) | P = 0.014 |
| 12 h | 2.5 (0–7) | 1.0 (0–4) | P = 0.003 |
| 24 h | 3.0 (1–7) | 1.0 (0–4) | P < 0.001 |
Data are presented as median (range).
Group A compared with group B; Mann–Whitney U-test.
Discussion
This present study compared two different concentrations of bupivacaine and two different volumes of solutions used for US-TAP blocks to evaluate if this would make a difference in terms of postoperative pain relief in patients undergoing laparoscopic cholecystectomies. Group A received a volume of 20 ml (50 mg 0.5% bupivacaine +10 ml saline solution) and group B received a volume of 30 ml (50 mg 0.5% bupivacaine + 20 ml saline solution). The duration of surgery was significantly longer in group B compared with group A (P = 0.036), but the intraoperative consumption of remifentanil, postoperative VAS scores (20 min, 12 h and 24 h) and requirement for postoperative analgesics were all significantly lower in group B compared with group A (P < 0.05 for all comparisons).
Previous research investigated a ‘pop’ technique in a cadaver study, in which methylene blue was administered and confirmed using a computed tomography scan.2 The ‘pop’ technique has also been described for other regional anaesthetic methods, such as ilioinguinal/iliohypogastric nerve blocks,8 where severe complications, such as colonic puncture, nerve injury or the unpredictable spread of local anaesthetic with a subsequent extension of the motor block, have been reported.9 The direct visualization of all of the anatomical structures, the needle and the spread of the local anaesthetic via US guidance may be associated with an increased margin of safety and optimal block qualities.6 In this present study, the US-TAP block technique was used to avoid any complications associated with the ‘pop’ technique as described previously.2
The use of a TAP block for postoperative analgesia after laparoscopic cholecystectomy has become increasingly popular. A previous study reported that morphine consumption for the first 24 h after the operation in patients who underwent laparoscopic cholecystectomies was significantly reduced by the administration of a US-TAP block using 30 ml of 0.5% bupivacaine (15 ml injected in each side).6
A previous study suggested that TAP block probably only had a small effect on reducing postoperative pain in patients undergoing laparoscopic cholecystectomy.10 In their study, the authors used ultrasound-guided tap blocks with 20 ml 0.5% ropivacaine and they found some beneficial effect in reducing pain with TAP block after laparoscopic cholecystectomy.10 However, very few studies have investigated the effects of a TAP block using different volumes and concentrations of anaesthetic solution. A previous study evaluated the effects of the US-TAP block by comparing the efficacy according to the concentration of levobupivacaine in patients undergoing laparoscopic cholecystectomies.11 In this previous study, the patients undergoing laparoscopic cholecystectomies were randomized into three groups: (i) a control group; (ii) a US-TAP block group that was administered 30 ml of 0.25% levobupivacaine; and (iii) a US-TAP block group that was 30 ml of 0.5% levobupivacaine.11 After the induction of general anaesthesia, a bilateral US-TAP block was performed using an in-plane technique, with 15 ml levobupivacaine injected on each side.11 Their results showed that the US-TAP block with either 30 ml of 0.25% or 30 ml of 0.5% levobupivacaine significantly reduced postoperative pain compared with the control treatment in patients undergoing laparoscopic cholecystectomies.11 Importantly, the study found that the lower concentration could be effective.11 The present study, in which group A received 20 ml of local anaesthetic for US-TAP block and group B received 30 ml of local anaesthetic (i.e. administered at a lower concentration), the intraoperative consumption of remifentanil, postoperative VAS scores (20 min, 12 h and 24 h) and the requirement for postoperative analgesics were all significantly lower in group B compared with group A (P < 0.05 for all comparisons). These current findings suggest that a TAP block performed using US-guided visualization of the spread of the local anaesthetic to the upper part of the abdomen can be an effective treatment for postoperative pain in patients undergoing laparoscopic cholecystectomies. The spread of the local anaesthetic into the fascia that was enabled by using 30 ml of solution was associated with good pain relief in this present study. In our opinion, an anaesthetic solution volume of 20 ml cannot produce effective postoperative pain relief because of its low diffusion capacity.
In the present study, duration of surgery was significantly longer in group B compared with group A. Group B also experienced less postoperative pain and required less postoperative rescue analgesics compared with group A. However, a search of the published literature did not identify any studies that found an association between with the duration of surgery and postoperative pain relief following a TAP block, so in our opinion this was a valuable result. Similar to the present study, previous research found that the total intraoperative consumption of sufentanil was significantly reduced by a TAP block performed with 30 ml of 0.5% bupivacaine compared with no TAP block.6 Similarly, another study showed that a TAP block with 20 ml ropivacaine reduced the amount of remifentanil required during surgery compared with saline.12
In many previous studies of the use of a TAP block in patients undergoing laproscopic cholecystectomy, there were no differences in terms of the haemodynamic parameters and the duration of anaesthesia between the study groups; and no complications were observed.6,11,13 Similarly, there were no differences between the two groups in the present study in terms of demographic characteristics, duration of anaesthesia, haemodynamic parameters and the patient satisfaction scores.
In conclusion, a US-TAP block can form part of a balanced postoperative analgesic regimen following laparoscopic cholecystectomy. A US-TAP block can reduce the amount of opioids used during the operation. Further research is required to investigate the optimal local anaesthetic concentration and volume required to maintain postoperative pain relief.
Declaration of conflicting interests
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Rafi AN. Abdominal field block: a new approach via the lumbar triangle. Anaesthesia 2001; 56: 1024–1026. [DOI] [PubMed] [Google Scholar]
- 2.McDonnell JG, O’Donnell BD, Farrell T, et al. Transversus abdominis plane block: a cadaveric and radiological evaluation. Reg Anesth Pain Med 2007; 32: 399–404. [DOI] [PubMed] [Google Scholar]
- 3.Barczynski M, Herman RM. A prospective randomized trial on comparison of low-pressure (LP) and standard-pressure (SP) pneumoperitoneum for laparoscopic cholecystectomy. Surg Endosc 2003; 17: 533–538. [DOI] [PubMed] [Google Scholar]
- 4.Wills VL, Hunt DR. Pain after laparoscopic cholecystectomy. Br J Surg 2000; 87: 273–284. [DOI] [PubMed] [Google Scholar]
- 5.Mouton WG, Bessell JR, Millard SH, et al. A randomized controlled trial assessing the benefit of humidified insufflation gas during laparoscopic surgery. Surg Endosc 1999; 13: 106–108. [DOI] [PubMed] [Google Scholar]
- 6.El-Dawlatly AA, Turkistani A, Kettner SC, et al. Ultrasound-guided transversus abdominis plane block: description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy. Br J Anaesth 2009; 102: 763–767. [DOI] [PubMed] [Google Scholar]
- 7.American Society of Anesthesiologists. ASA Physical Status Classification System. http://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system (Last approved by the ASA House of Delegates on October 15, 2014).
- 8.van Schoor AN, Boon JM, Bosenberg AT, et al. Anatomical considerations of the pediatric ilioinguinal/iliohypogastric nerve block. Paediatr Anaesth 2005; 15: 371–377. [DOI] [PubMed] [Google Scholar]
- 9.Johr M, Sossai R. Colonic puncture during ilioinguinal nerve block in a child. Anesth Analg 1999; 88: 1051–1052. [DOI] [PubMed] [Google Scholar]
- 10.Petersen PL, Stjernholm P, Kristiansen VB, et al. The beneficial effect of transversus abdominis plane block after laparoscopic cholecystectomy in day-case surgery: a randomized clinical trial. Anesth Analg 2012; 115: 527–533. [DOI] [PubMed] [Google Scholar]
- 11.Ra YS, Kim CH, Lee GY, et al. The analgesic effect of the ultrasound-guided transverse abdominis plane block after laparoscopic cholecystectomy. Korean J Anesthesiol 2010; 58: 362–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kawahara R, Tamai Y, Yamasaki K, et al. The analgesic efficacy of ultrasound-guided transversus abdominis plane block with mid-axillary approach after gynecologic laparoscopic surgery: a randomized controlled trial. J Anaesthesiol Clin Pharmacol 2015; 31: 67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kokulu S, Baki ED, Kacar E, et al. Effect of transversus abdominis plane block on cost of laparoscopic cholecystectomy anesthesia. Med Sci Monit 2014; 20: 2783–2787. [DOI] [PMC free article] [PubMed] [Google Scholar]