Abstract
Objective
To evaluate the effect of dynamic long leg casting in paediatric patients with developmental dysplasia of hip (DDH) diagnosed at 12–18 months.
Methods
The adductor tenotomy, closed reduction, and dynamic long leg casting method was adopted to treat paediatric patients with DDH. The hips were divided into four groups according to the Tonnis radiographic dislocation classification. Groups were also classified according to the baseline acetabular index (AI): 30°–35°, 36°–40°, and > 40°. The outcomes of the reductions were evaluated according to McKay’s hip function criteria and Severin’s radiological criteria.
Results
A total of 246 patients (339 hips) had complete follow-up data. After 3 months of orthosis fixation, the results were satisfactory in 264 hips (77.88%). Hip function was rated as ‘excellent’ or ‘good’ in 43 of 51 (84.31%) Tonnis type 1 hips, 125 of 155 (80.65%) type 2 hips, 70 of 90 (77.78%) type 3 hips, and 34 of 43 (79.07%) type 4 hips. The higher the baseline AI, the lower the rates of ‘excellent’ and ‘good’ hip function. Favourable radiological results (Severin types I and II) were found in 266 of 339 (78.47) hips.
Conclusions
Dynamic long leg casting is an effective method for treating patients with DDH aged 12–18 months at diagnosis.
Keywords: Hip dislocation treatment, long-term outcome, closed reduction treatment, infants
Introduction
The treatment method used for 12- to 18-month-old paediatric patients with developmental dysplasia of the hip (DDH) has become controversial. For example, increasingly more surgeons advocate an early operation,1 but reports on the long-term effects of the conservative treatment for patients older than 12 months are very rare.2 As a noninvasive treatment method, conservative treatment results in less trauma, so it is easier for patients and their families to accept, but the applicable age has been a controversial issue.3 To date, a number of different types of conservative treatment have been used, such as frog fixation and human position fixation.4 The traditional method was often utilized to fix hips in an abduction and buckling position.4 Furthermore, some surgeons have developed modified methods based on the traditional treatment.3 The aim of this present study was to determine the outcome of the adductor tenotomy, closed reduction, and dynamic long leg casting method in infants with DDH diagnosed between the ages of 12 and 18 months.
Patients and methods
Study population
This retrospective study reports the outcomes for the period between January 1993 and July 2004, in which the adductor tenotomy, closed reduction, and dynamic long leg casting method was adopted to treat consecutive paediatric patients with DDH aged 12- to 18-months old in the Department of Paediatric Orthopaedics, Shengjing Hospital of China Medical University, Shenyang, Liaoning Province, China. Completed follow-up data were available for a proportion of these patients. All patients met the following inclusion criteria: (i) they suffered from simple hip dislocation that was not associated with other congenital malformations; (ii) they were aged from 12 to 18 months old when treatment was started; (iii) they did not receive treatment before hospitalization. Infants with dislocation of the hip caused by inflammation, spasticity, spinal bifida, arthroereisis and Down’s syndrome, and a dislocation of the hip associated with other malformations, were excluded.
Ethic approval was provided by the Ethics Committee of Shengjing Hospital of China Medical University (no. 201409871) and written informed consent was provided by the legally authorized representatives of the paediatric patients. Patients were divided into three groups according to the acetabular index (AI) before treatment: a 30°–35°group; a 36°–40°group; and a > 40° group. The acetabular index is the angle formed by a horizontal line connecting both triradiate cartilages (Hilgenreiner’s line) and a second line connecting the acetabular roof and the acetabular centre. According to the Tonnis classification of the radiological grades of dislocation (Table 1),5 the patients were divided into Tonnis types 1 to 4.
Table 1.
Definition of different clinical classifications that were used in this study to determine the outcome of the adductor tenotomy, closed reduction, and dynamic long leg casting method in infants with developmental dysplasia of the hip diagnosed between the ages of 12 and 18 months.
| Classification | Definition | Grade and criteria |
|---|---|---|
| Tonnis classification | Radiological grades of dislocation | Type 1: Femoral capital epiphysis medial to Perkin’s line and below Hilgenreiner’s line |
| Type 2: Epiphysis below Hilgenreiner’s line but lateral to Perkin’s line | ||
| Type 3: Epiphysis lateral to Perkin’s line at the level of the acetabular margin | ||
| Type 4: Epiphysis lateral to Perkin’s line and above the acetabular rim | ||
| McKay’s criteria | Function of hip | Excellent: Painless, stable hip; no limp; more than 15° of internal rotation |
| Good: Painless, stable hip; slight limp or decreased motion; negative Trendelenburg’s sign | ||
| Fair: Minimum pain; moderate stiffness; positive Trendelenburg’s sign | ||
| Poor: Significant pain | ||
| Severin’s classification | Evaluation of radiographic results | Type I: Normal hips |
| Type II: Concentric reduction of the joint with deformity of the femoral neck, head or acetabulum | ||
| Type III: Dysplastic hips without subluxation | ||
| Type IV: Subluxation | ||
| Type V: The head articulating with a secondary acetabulum in the upper part of the original acetabulum | ||
| Type VI: Redislocation | ||
| Salter’s criteria | Presentation of avascular necrosis | Yes or No |
Study treatment
In all patients, traction was implemented before reduction. For patients suffering from Tonnis types 1 and 2 dislocations, this included double lower limb suspension skin traction. For patients classified as Tonnis types 3 and 4, femoral condyle pinning horizontal bone traction was implemented with lower leg level skin traction with a weight of 0.5 kg/6 months of age. The traction duration was 2 weeks. For Tonnis types 3 and 4, an X-ray examination was performed post-traction to ensure that the femoral head centre was pulled below the upper margin of the acetabulum.
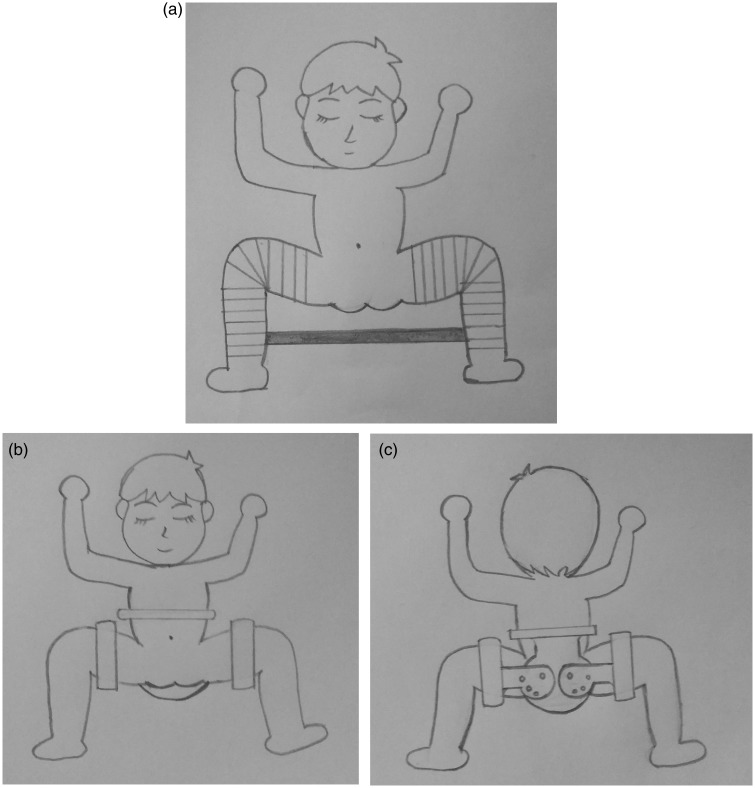
All patients in this study had a general anaesthetic, adductor tenotomy and closed reduction. General anaesthesia was administered to achieve full muscle relaxation, and the supine position was adopted to abduct the hip joint on the affected side to see that the adductor was tensioned. A scalpel was used, approaching the regio pubica, to percutaneously cut off a large part of the adductor tendon to relieve the tension, and a gauze compression haemostasis and pressure dressing without suture was applied. An assistant held the pelvis of the infant patient in place. The surgeon flexed the hip and knee joints to 90° and slowly and gently implemented traction to make the femoral head slide towards the front inner side from the upper back of the acetabulum. The hip abduction and external rotation was then gradually completed. The greater trochanter of the femur was pressed by the thumb of the other hand, so that the femoral head could pass through the glenoid labrum to produce a snap to enter the acetabulum, and in this way, the reduction was accomplished. An intraoperative X-ray machine was used to confirm the success of the reduction. With both hips at 90° abduction and external rotation and 110° of flexion, through which the femoral head can return to the centre of acetabulum, dynamic long leg casting fixation was used to fix the limbs above the ankle joint and below the hip joint (with the ankle joint and hip joint exposed) and between the two lower legs, using stick casting for the connection. Please note that the casting at the thighs should be slightly loose to ensure that the hip joint can make an 80° to 110° flexion and extension movement during the fixing period. This only limited the straightening and adduction motion, which could easily cause hip joint dislocation. Other motions of the hip joint were not limited (Figure 1a).
Figure 1.
(a) Dynamic frog casting fixation. Abduction-adduction motion of hips is limited. Hip joint can make 80°–110° flexion-extension motion and some rotation. The ankle can move freely. (b) Front of the adjustable abductions orthosis. (c) Back of the adjustable abductions orthosis.
After discharge, patients were allowed to make sitting, lying, standing, flexing, and extension motions. After 3 months of fixation, they returned to the hospital for cast removal. An adjustable abductions orthosis was fitted that only fixes the thighs and allows the knee and ankle joints to move freely and allows the hip joints to have a certain amount of movement (Figures 1b and 1c). The orthosis was removed after a further 3 months, and then the infants were able to walk freely. At 6-month intervals, a pelvic X-ray examination was taken to observe the development of the acetabulum and femoral head, and to set up the follow-up database.
Statistical analyses
All statistical analyses were performed using the SPSS® statistical package, version 15.0 (SPSS Inc., Chicago, IL, USA) for Windows®. The clinical criteria for the assessment of the results at the final follow-up visit were based on (i) McKay’s function of the hip criteria;6 and (ii) an X-ray imaging evaluation that was carried out according to Severin’s classification (Table 1).7 An evaluation of the presence of avascular necrosis (AVN) of the femoral head was performed according to Salter’s criteria (Table 1).8 The patients were divided into groups based on their AI and the Tonnis type of radiological dislocation to form paired data. Data are presented as mean ± SD or n of patients. Two independent samples t-test was used for continuous variables and χ2-test was used for categorical variables. A P-value < 0.05 was considered statistically significant.
Results
A total of 280 (381 hips) paediatric patients with DDH who were aged 12–18-months were enrolled in the study. Of these, 246 patients (339 hips) had complete follow-up data available. The follow-up data were collected over a period of 6.5–15.5 years (mean: 9.5 years). In the 246 patients (339 hips) with complete follow-up data who were selected for inclusion in these analyses, the adductor tenotomy, closed reduction, and dynamic long leg casting method was used when they were 12–18 months old. There were 48 males and 198 females (153 unilateral patients; 93 bilateral patients); and the mean age was 15 months when treatment was started. Patients were divided into three groups according to their AI before treatment: 106 hips in the 30°–35° group; 121 hips in the 36°–40° group; and 112 hips in the > 40° group. According to the Tonnis classification, the patients were divided into four groups: 51 hips with type 1, 155 hips with type 2, 90 hips with type 3, and 43 hips with type 4.
For 264 hips (77.88%), after 3 months of orthosis fixation, the result was satisfactory and no further treatment was received. Subluxation occurred or the joint space was increased in 75 hips after the orthosis removal. Ideal reduction was achieved for 42 of 75 hips by prolonging the orthosis fixation time (mean 9 months), but 33 hips required an operation, which included a Salter pelvic osteotomy (20 hips) or a Pemberton acetabular arthroplasty (13 hips). Prior to the final follow-up examination, the clinical results according to McKay’s hip function criteria were as follows: ‘excellent’ in 169 hips, ‘good’ in 103 hips, ‘fair’ in 37 hips and ‘poor’ in 30 hips. The ‘excellent’ and ‘good’ rate was 80.24% (272 of 339). Among the 67 hips rated as ‘fair’ and ‘poor’, 9.73% (33 of 339 hips) underwent an operation.
The final radiological examination was performed at the final follow-up visit. The X-rays were assessed according to the Severin’s classification and the findings were as follows: 130 hips at type I, 136 hips at type II, 43 hips at type III, and 30 hips at type IV. Favourable radiological results (types I and II) were observed in 266 of 339 hips (78.47%). According to the Salter’s criteria, 16 of 339 hips (4.72%), all with Tonnis type 4 before reduction, were complicated by AVN.
When the function of the hip (using McKay’s criteria) was analysed in patients who were stratified according to their baseline Tonnis type before the reduction was undertaken, the ‘excellent’ and ‘good’ rate for Tonnis types 1, 2, 3 and 4 were 84.31%, 80.65%, 77.78% and 79.07%, respectively; and the four groups were not significantly different (Table 2). All 16 hips complicated by AVN had a Tonnis type 4 dislocation before reduction and the dislocation height was > 2 cm higher than the acetabular rim. According to McKay’s hip function criteria, seven of 16 hips with AVN were rated as ‘good’, four hips were rated as ‘fair’ and five hips were rated as ‘poor’. For the nine hips rated as ‘fair’ or ‘poor’, a Salter pelvic osteotomy was later performed.
Table 2.
Relationship between baseline Tonnis types before reduction was undertaken and the McKay’s criteria achieved after treatment was complete (n = 339).
| Tonnis type | Total hips | McKay’s hip function criteria |
||||
|---|---|---|---|---|---|---|
| Excellent | Good | Fair | Poor | Total ‘excellent’ and ‘good’ ratea | ||
| 1 | 51 | 27 | 16 | 6 | 2 | 43 (84.31) |
| 2 | 155 | 92 | 33 | 16 | 14 | 125 (80.65) |
| 3 | 90 | 35 | 35 | 11 | 9 | 70 (77.78) |
| 4 | 43 | 15 | 19 | 4 | 5 | 34 (79.07) |
| Total | 339 | 169 | 103 | 37 | 30 | 272 (80.24) |
Data presented as n of hips (%).
No significant difference in the rates of McKay’s criteria of ‘excellent’ and ‘good’ between the four Tonnis type groups; χ2-test (P ≥ 0.05).
Before treatment, the AI values in all hips were > 30°. There was no significant difference between the rates of ‘excellent’ and ‘good’ between the 30°–35° and 36°–40° groups, but when compared with the > 40° group, both groups demonstrated a significant difference (P < 0.05 for both comparisons) (Table 3).
Table 3.
Relationship between baseline acetabular index (AI) value before reduction was undertaken and the McKay’s criteria achieved after treatment was complete (n = 339).
| AI value | Total hips | McKay’s hip function criteria |
||||
|---|---|---|---|---|---|---|
| Excellent | Good | Fair | Poor | Total ‘excellent’ and ‘good’ rate | ||
| 30°–35° | 106 | 73 | 18 | 10 | 5 | 91 (85.85)a |
| 36°–40° | 121 | 56 | 44 | 12 | 9 | 100 (82.64)a |
| > 40° | 112 | 40 | 41 | 15 | 16 | 81 (72.32) |
Data presented as n of hips (%).
Significant difference in the rate of McKay’s criteria of ‘excellent’ and ‘good’ compared with the > 40° group; χ2-test (P ≥ 0.05).
Discussion
After many years of clinical research, it is now recognized that the starting treatment age is one of the most important factors that affects the long-term outcome of conservative treatment of DDH.9,10 As age and dislocation time increases, a series of pathological changes occur to the anatomical structure of the hip joint in patients with DDH, especially after the patients start to walk.11 The grade of dislocation and the hip joint surrounding the soft tissue contracture often become more obvious.12,13 It has been reported that it is difficult to achieve satisfactory development of the acetabulum in reductions undertaken after 18 months of age.14 The developmental potential of an acetabular shape can last until the patient is 10 years old.15 In China, as screening for DDH is not widely undertaken, some infants with DDH are not diagnosed prior to them starting to walk.16 Their parents usually seek medical advice at around 12 months of age following abnormal movements, which leads to more infants with DDH being diagnosed from 12 to 18 months of age in China.16 Hip development ability in infants under 18 months of age is rather strong,12,15 so it is advisable to adopt a minimally-invasive conservative treatment. In this present study, dynamic casting for the hip joint was applied for patients with DDH aged 12–18 months at diagnosis with satisfactory outcomes.
Our previous study of the acetabular development of 400 normal infants (males 50%) at different ages found that their mean AI at birth was 34.2°; and prior to 6 months of age, their mean AI was always > 30°.17 When they were between 3 and 5 years old, there was a developmental peak during which the AI decreased rapidly; and by the time they were between 7 and 8 years old, the AI was close to the adult level.17 In all cases in this present study, reduction was performed to restore the anatomical position before the development peak so that the femoral head and acetabulum may interact to promote the full use of the development peak. The results of this present study showed that for most 12- to 18-month-old patients, after the orthosis had been fixed for 3 months, the femoral head and acetabulum had achieved good development and were in a satisfactory position. The mean follow-up time was 9.5 years and 80.24% (272 of 339) of hips achieved McKay’s hip functional criteria of ‘excellent’ and ‘good’. These current findings suggest that the dynamic long leg casting method is a good technique for treating patients with DDH who are older than 12 months. The position fixation used by us was the ‘frog’ position with 90° abduction and 110° of flexion, through which the femoral head can return to the centre of the acetabulum. Meanwhile, due to the existence of the femoral anteversion angle, the femoral head contacts the upper wall of the acetabulum, and after we implemented external rotations for hip joints, the femoral head contacts the upper and posterior walls of the acetabulum. Therefore, mechanical stimulation is conducive to the development and growth of the upper and posterior walls of the acetabulum.
It is generally recognized that the grade of dislocation has an impact on the pathological changes of the hip.18 However, there are different opinions about the relationship between the dislocation grade and the result of conservative treatment. For example, a study that analysed 100 patients with DDH aged from 6 to 36 months who were treated with a closed reduction method, reported that the dislocation grade before reduction impacted on the effect of treatment.19 This is in direct contrast to the current findings, which found no significant differences between the rates of ‘excellent’ and ‘good’ hip function based on McKay’s criteria between the four groups stratified according to their baseline Tonnis type before the reduction was undertaken (Table 2). These current findings suggest that the radiographic dislocation grade does not have a direct relationship with the long-term therapeutic outcomes.
The AI is a common imaging index used to evaluate the condition of a hip joint. DDH is mainly manifested as AI increases.20 To date, there have been various inconsistent reports regarding the influence of AI before treatment on acetabulum development post-reduction.21,22 During the follow-up period in the present study, the AI before the reduction was demonstrated to have an impact on the outcomes. The higher the baseline AI, the lower the rates of ‘excellent’ and ‘good’ hip function based on McKay’s criteria. Therefore, patients with an AI > 40° should be treated by closed reduction with caution. In this current group of 339 hips, subluxation or joint space increases occurred in 75 hips post-orthosis removal. Even after prolonging the orthosis fixation time, there were still 33 hips (9.73%) that required an operation. Therefore, the closed reduction method cannot be adopted for all patients with DDH younger than 18 months because it does not appear to be applicable for those with an AI > 40°.
In this present study, the dynamic long leg casting method achieved good results. According to Salter’s criteria, the incidence rate of AVN was 4.72%. In our opinion, this relates to the following factors: (i) the use of preoperative traction and adductor tenotomy in the current study was based on previous research that found that compared with patients receiving preoperative traction, the patients with Tonnis type 1 and 2 dislocations who did not receive traction treatment had a more tensioned joint during reduction and had a higher pressure between the femoral head and acetabulum after reduction.23 We speculate this is related to contracture of the peripheral tissue and capsular ligament of the hip joint. Therefore, the present study implemented a 2-week traction treatment for all patients before reduction. We routinely cut the adductor and implemented skin traction or bone traction of the lower limbs for 2 weeks. With this method, the deformed muscle groups can be effectively relaxed to improve the blood circulation in blood vessels on the inside of the circumflex femoral between the iliopsoas muscle and the adductor muscle and to reduce the pressure in the joint after reduction; (ii) the implementation of closed reduction under general anaesthesia to place the contracted muscles into a relaxed state, which was conducive to the repair and to temporarily eliminate the mechanical pressure between the femoral head and the acetabulum; (iii) and based on the premise that the hip joint can make an 80°–110° flexion and extension movement, we changed the static point contact between the femoral head and the acetabulum into a dynamic surface contact, to make the stress between the acetabulum and the femoral head closer to the physiological state. At the same time, we made the forces of the muscle groups around the hip joint point to different directions along the axial direction of the femoral shaft to relieve the pressure between the acetabulum and the femoral head to some extent.
In conclusion, the adductor tenotomy, closed reduction, dynamic long leg casting method is an effective method for treating 12- to 18-month-old patients with DDH. The AI prior to reduction had an impact on treatment outcome and could be used to select patients most likely to benefit from the closed reduction method because patients with an AI < 40° had higher rates of treatment success compared with patients with an AI > 40°. The extent of radiographic dislocation before reduction had little effect on the success rate of this closed reduction treatment method.
Declaration of conflicting interests
The authors declare that there are no conflicts of interest.
Funding
This research was supported by the National Nature Science Foundation of China (no. 81371918) and the Science and Technique Programme of Liaoning Province (no. 2013225303, no. LZ2014036).
References
- 1.Feeley IH, Green CJ, Rowan FE, et al. International variance in the treatment of developmental dysplasia of the hip. J Child Orthop 2014; 8: 381–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahmed E, Mohamed AH, and Wael H. Surgical treatment of the late - presenting developmental dysplasia of the hip after walking age. Acta Ortop Bras 2013; 21: 276–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaneko H, Kitoh H, Mishima K, et al. Long-term outcome of gradual reduction using overhead traction for developmental dysplasia of the hip over 6 months of age. J Pediatr Orthop 2013; 33: 628–634. [DOI] [PubMed] [Google Scholar]
- 4.Madhu TS, Akula M, Scott BW, et al. Treatment of developmental dislocation of hip: does changing the hip abduction angle in the hip spica affect the rate of avascular necrosis of the femoral head? J Pediatr Orthop B 2013; 22: 184–188. [DOI] [PubMed] [Google Scholar]
- 5.Tonnis D. Congenital dysplasia and dislocation of the hip in children and adults, Heidelberg: Springer-Verlag, 1987. [Google Scholar]
- 6.McKay DW. A comparison of the innominate and the pericapsular osteotomy in the treatment of congenital dislocation of the hip. Clin Orthop Relat Res 1974; 98: 124–132. [DOI] [PubMed] [Google Scholar]
- 7.Severin E. Contribution to the knowledge of congenital dislocation of the hip joint. Late results of closed reduction and arthrographic studies of recent cases. Acta Chirurgica Scandinavica 1941; 84: 1–142. [Google Scholar]
- 8.Salter RB, Kostuik J, Dallas S. Avascular necrosis of the femoral head as a complication of treatment for congenital dislocation of the hip in young children: a clinical and experimental investigation. Can J Surg 1969; 12: 44–61. [PubMed] [Google Scholar]
- 9.Sllamniku S, Bytyqi C, Murtezani A, et al. Correlation between avascular necrosis and the presence of the ossific nucleus when treating developmental dysplasia of the hip. J Child Orthop 2013; 7: 501–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ruszkowski K, Pucher A, Strzyzewski W. The effect of absent ossific nucleus of the femoral head on results of surgical treatment for developmental dislocation of the hip. Chir Narzadow Ruchu Ortop Pol 2005; 70: 391–396. [in Polish, English Abstract]. [PubMed] [Google Scholar]
- 11.Kitano T, Imai Y, Morita M, et al. New treatment method for developmental dysplasia of the hips after walking age: arthroscopic redaction with limboplasty based on the findings of preoperative imaging. J Orthop Sci 2010; 15: 443–451. [DOI] [PubMed] [Google Scholar]
- 12.Huang S, Zhao D, Yang L. New approach to the treatment of adolescent hip dysplasia. Med Hypotheses 2013; 81: 122–124. [DOI] [PubMed] [Google Scholar]
- 13.Duppe H, Danielsson LG. Screening of neonatal instability and of developmental dysplasia of the hip. A survey of 132,601 living newborn infants between 1956 and 1999. J Bone Joint Surg Br 2002; 84: 878–885. [DOI] [PubMed] [Google Scholar]
- 14.Salter RB. The classic. Innominate osteotomy in the treatment of congenital dislocation and subluxation of the hip by Robert B. Salter, J. Bone Joint Surg. (Brit) 43B:3:518, 1961. Clin Orthop Relat Res 1978; 137: 2–14. [PubMed] [Google Scholar]
- 15.Birkenmaier C, Jorysz G, Jansson V, et al. Normal development of the hip: a geometrical analysis based on planimetric radiography. J Pediatri Orthop B 2010; 19: 1–8. [DOI] [PubMed] [Google Scholar]
- 16.Di YZ, Yang JP, Wang WW, et al. Early screening of developmental dysplasia of the hip in Tianjin. Chinese Journal of Orthopaedics 2011; 31: 463–468. [Google Scholar]
- 17.Zhao Q, Ji SJ, Zhou YD. The research of closed reduction of congenital hip dislocation after acetabulum development change. J Chinese Journal of Orthopaedics 1990; 6: 415–417. [Google Scholar]
- 18.Ardila OJ, Divo EA, Moslehy FA, et al. Mechanics of hip dysplasia reductions in infants using the Pavlik harness: a physics-based computational model. J Biomech 2013; 46: 1501–1507. [DOI] [PubMed] [Google Scholar]
- 19.Li G, Lin Q, Huang C, et al. A study of acetabular development after closed reduction in developmental dysplasia of the hip. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2008; 22: 657–661. [in Chinese, English Abstract]. [PubMed] [Google Scholar]
- 20.El-Sayed M, Ahmed T, Fathy S, et al. The effect of Dega acetabuloplasty and Salter innominate osteotomy on acetabular remodeling monitored by the acetabular index in walking DDH patients between 2 and 6 years of age: short- to middle-term follow-up. J Child Orthop 2012; 6: 471–477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Albinana J, Dolan LA, Spratt KF, et al. Acetabular dysplasia after treatment for developmental dysplasia of the hip. Implications for secondary procedures. J Bone Joint Surg Br 2004; 86: 876–886. [DOI] [PubMed] [Google Scholar]
- 22.Werner CM, Copeland CE, Ruckstuhl T, et al. Relationship between Wiberg’s lateral center edge angle, Lequesne’s acetabular index, and medial acetabular bone stock. Skeletal Radiol 2011; 40: 1435–1439. [DOI] [PubMed] [Google Scholar]
- 23.Yamada N, Maeda S, Fujii G, et al. Closed reduction of developmental dislocation of the hip by prolonged traction. J Bone Joint Surg Br 2003; 85: 1173–1177. [DOI] [PubMed] [Google Scholar]