Abstract
Surgical excision is the traditional treatment for osteoid osteoma. However, the complexity of the foot anatomy makes a satisfactory outcome challenging. Difficulty in localizing the lesion intraoperatively may result in either incomplete tumor resection or excessive bone loss. To date, no published report has described the use of three-dimensional printing in the surgical treatment of osteoid osteoma of the calcaneus. In this case, we printed a three-dimensional model of the calcaneus of a 17-year-old female patient with a 2-year history of night pain in the lateral aspect of the hindfoot and ankle, evaluated the lesion as an osteoid osteoma, and designed a surgical guiding plate. Intraoperatively, we had no difficulty achieving complete resection of the lesion from the lateral calcaneus bone window, autogenous bone grafting, and subtalar arthrodesis. At the 2-year follow-up examination, the patient remained asymptomatic with no recurrence of the osteoid osteoma.
Keywords: Calcaneus, osteoid osteoma, three-dimensional printing, surgical treatment
Introduction
The first osteoid osteoma was reported by Jaffe in 1935. This lesion accounts for approximately 11% of all benign bone tumors. The most commonly affected bones are the tibia and femur1,2; only about 2% to 10% of cases occur in the foot.3,4 Osteoid osteomas rarely exceed 1.5 cm, and it is thus difficult to localize the tumor during surgery. Furthermore, inadequate resection often leads to recurrence.
Three-dimensional (3D) printing has been widely used in trauma and joint surgery.5–8 However, no published reports have described the use of this technology in the surgical treatment of osteoid osteoma of the calcaneus.
Case report
A 17-year-old female patient with no significant medical history presented with a 2-year history of night pain in the lateral aspect of the hindfoot and ankle. She denied any history of trauma. Her symptoms could be partially relieved with aspirin. A plain radiograph showed a sclerotic area in the left calcaneus just inferior to the subtalar joint (Figure 1). She underwent a needle biopsy of the calcaneus in a local hospital. The pathological report described a small amount of bone tissue with a poor blood supply and no signs of tumors or tuberculosis. She was diagnosed with chronic osteomyelitis and received conservative treatments including analgesic drugs and physiotherapy. One month later, the patient presented to our medical center because the pain had become severe. On physical examination, we found severe swelling of the left hindfoot (Figure 2) with mild tenderness, and the motion of the subtalar joint was limited. A computed tomography (CT) scan revealed a lesion with a sclerotic rim in the anterolateral aspect of the left calcaneus adjacent to the posterior talocalcaneal joint (Figure 3). Magnetic resonance images showed a well-circumscribed area of low-signal intensity in the anterolateral aspect of the left calcaneus with surrounding edema (Figure 4). The erythrocyte sedimentation rate and C-reactive protein concentration were within their reference ranges. The tuberculosis antibody titer was negative. A clinical diagnosis of osteoid osteoma was made.
Figure 1.
Lateral radiograph showing a sclerotic area in the left calcaneus just inferior to the subtalar joint.
Figure 2.
Swelling of the left hindfoot.
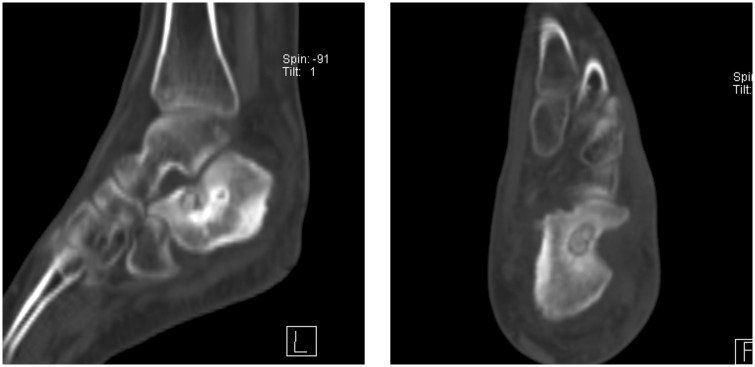
Figure 3.
Computed tomography images demonstrating the lesion with a sclerotic rim in the anterolateral aspect of the left calcaneus adjacent to the posterior talocalcaneal joint.
Figure 4.
Magnetic resonance images showing a well-circumscribed area of low-signal intensity in the anterolateral aspect of the left calcaneus with surrounding edema.
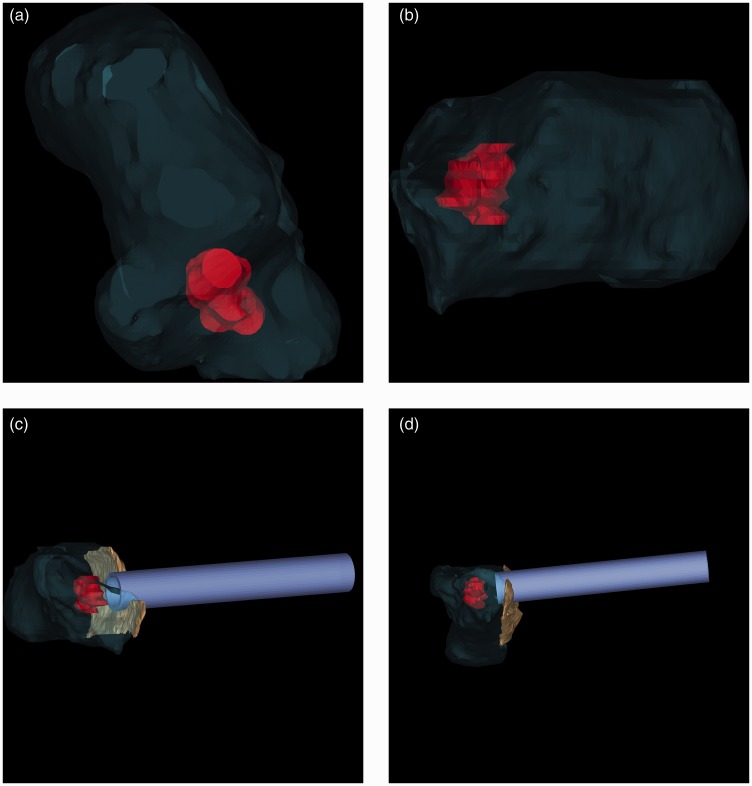
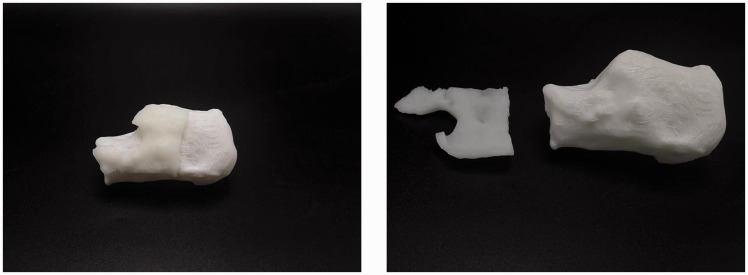
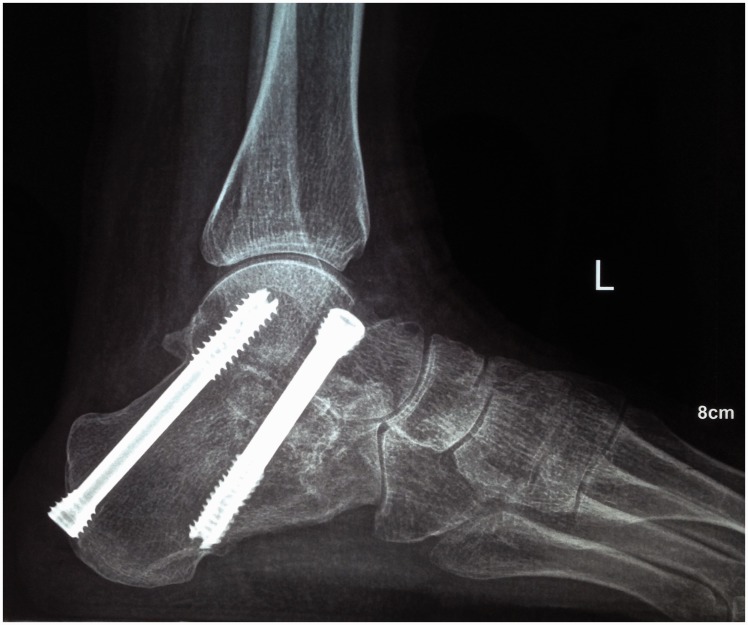
The CT images were processed with MIMICS software (Materialise, Ann Arbor, MI). A 3D model of the left calcaneus was created, and the volume (cm3) and position of the osteoid osteoma was determined (Figure 5a, b). A surgical guiding plate was designed to guide a trephine to make a bone window on the lateral aspect of the calcaneus (Figure 5c, d). Both the 3D model of the calcaneus and surgical guiding plate were fabricated by a 3D printer (ZPrinter 450; Z Corporation, Burlington, MA) in our medical center (Figure 6). After administration of epidural anesthesia, the patient was placed in the supine position, and a suitably sized sandbag was placed under the ipsilateral buttock to maintain the position of the limb. A tourniquet was positioned around the left thigh. A lateral approach was used to expose the subtalar joint. We found effusion in the peroneus tendon sheath, and the cartilage of the calcaneus had been eroded by the tumor. With the aid of the surgical guiding plate, we made a bone window on the lateral aspect of the calcaneus using a trephine. The tumor lesion was easily reached, and complete resection was achieved. The bone defect in the calcaneus was repaired with an autogenous bone graft. The subtalar arthrodesis was completed as planned. The postoperative pathological diagnosis was an osteoid osteoma (Figure 7). At the 2-year follow-up examination, the patient remained asymptomatic with no recurrence of the osteoid osteoma (Figures 8, 9).
Figure 5.
(a, b) The three-dimensional models of the left calcaneus and the osteoid osteoma. (c, d) Preoperative surgical plan to achieve complete resection of the osteoid osteoma. The fuchsia object represents the calcaneus. The red object represents the osteoid osteoma. The green object represents the surgical guiding plate. The blue object represents the trephine.
Figure 6.
The three-dimensional models of the calcaneus and surgical guiding plate.
Figure 7.
Image of hematoxylin and eosin staining of the nidus of the mature osteoid osteoma (scale bar, 200 µm).
Figure 8.
Lateral radiograph at 2 years postoperatively.
Figure 9.
Left subtalar joint at 2 years postoperatively.
Discussion
In the medical field, 3D printing is more than a sole manufacturing method.9 It promotes the development of precision medicine and meets the ever-growing needs of individualized medical treatment.10 3D models are created and printed based on two-dimensional CT or magnetic resonance images, which can be used for preoperative plans and surgical training. These models facilitate reduced surgical times, decrease intraoperative blood loss, and promote better reduction of complex fractures.5,11–13 Moreover, 3D printing makes it possible to fabricate custom implants for patients with anatomic deformities or large bone defects.14
An osteoid osteoma is a benign bone tumor. The characteristic clinical presentation includes severe night pain, soft tissue swelling, and joint effusion.1 When the lesion is located in the juxta-articular region of the foot, establishment of a correct diagnosis and effective treatment plan is difficult due to the complexity of the anatomy in this area.4,15–17 Surgical excision is the traditional treatment for osteoid osteoma.18 However, difficulty in localizing the lesion intraoperatively may result in either incomplete tumor resection or excessive bone loss.15 These complications may lead to treatment failure and tumor recurrence or unnecessary bone grafting.
In the present case, the rarity of osteoid osteoma in the calcaneus and the uncharacteristic signs on plain radiography were the main causes of misdiagnosis of the lesion as chronic osteomyelitis at the local hospital. For preoperative evaluation of the lesion, the patient underwent a CT scan at our medical center. The 3D model of the calcaneus created with Mimics software demonstrated that the osteoid osteoma was located in the anterolateral one-third of the calcaneus and that the volume of the lesion was about 1000 mm3. A surgical plan was made to achieve complete resection of the lesion from the lateral calcaneus bone window, perform autogenous bone grafting, and carry out subtalar arthrodesis. With the aid of the surgical guiding plate intraoperatively, we had no difficulty making a bone window in the lateral wall of the calcaneus with a trephine and reached the lesion directly. We found that the preoperative evaluation and the intraoperative findings were consistent. No X-ray exposure occurred during surgery. The operation was finished as planned within 40 min. Compared with conventional surgical methods, this new method saved about one-third of the surgical time. The cost of 3D printing was no more than $200 USD.
In conclusion, management of osteoid osteoma in the calcaneus is difficult. 3D printing is helpful in evaluating the osteoid osteoma preoperatively and localizing the lesion intraoperatively. We recommend the use of this novel technology in foot and ankle surgery.
Disclaimers
The views expressed in the submitted article are our own and not an official position of the institution or funder.
Declaration of conflicting interests
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Lee EH, Shafi M, Hui JH. Osteoid osteoma - a current review. J Pediatr Orthop 2006; 26: 695–700. [DOI] [PubMed] [Google Scholar]
- 2.Buchner M, Bernd L, Zahlten-Hinguranage A, et al. Bone and soft-tissue tumors of the foot and ankle. Chirurg 2005; 76: 391–397. [in German, English Abstract]. [DOI] [PubMed] [Google Scholar]
- 3.Jordan RW, Koc T, Chapman AW, et al. Osteoid osteoma of the foot and ankle–a systematic review. Foot Ankle Surg 2015; 21: 228–234. [DOI] [PubMed] [Google Scholar]
- 4.Houdek MT, Wenger DE, Sherman CE, et al. Osteoid osteomas of the foot and ankle: a study of patients over a 20-year period. Am J Orthop (Belle Mead, NJ) 2014; 43: 552–556. [PubMed] [Google Scholar]
- 5.Green JM, 3rd, Lawson ST, Liacouras PC, et al. Custom anatomical 3D spacer for temporomandibular joint resection and reconstruction. Craniomaxillofac Trauma Reconstr 2016; 9: 82–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang J, Tian XB, Sun L, et al. Establishing a customized guide plate for osteotomy in total knee arthroplasty using lower-extremity X-ray and knee computed tomography images. Chin Med J (Engl) 2016; 129: 386–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin HB, Huang W, Chen X, et al. Digital design of internal fixation for distal femoral fractures via 3D printing and standard parts database. Zhonghua Yi Xue Za Zhi 2016; 96: 344–348. [in Chinese, English Abstract]. [DOI] [PubMed] [Google Scholar]
- 8.Zeng C, Xiao J, Wu Z, et al. Evaluation of three-dimensional printing for internal fixation of unstable pelvic fracture from minimal invasive para-rectus abdominis approach: a preliminary report. Int J Clin Exp Med 2015; 8: 13039–13044. [PMC free article] [PubMed] [Google Scholar]
- 9.Murphy SV, Atala A. 3D bioprinting of tissues and organs. Nat Biotechnol 2014; 32: 773–785. [DOI] [PubMed] [Google Scholar]
- 10.Rengier F, Mehndiratta A, von Tengg-Kobligk H, et al. 3D printing based on imaging data: review of medical applications. Int J Comput Assist Radiol Surg 2010; 5: 335–341. [DOI] [PubMed] [Google Scholar]
- 11.Chen H, Guo K, Yang H, et al. Thoracic pedicle screw placement guide plate produced by three-dimensional (3-D) laser printing. Med Sci Monit 2016; 22: 1682–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yang M, Li C, Li Y, et al. Application of 3D rapid prototyping technology in posterior corrective surgery for lenke 1 adolescent idiopathic scoliosis patients. Medicine (Baltimore) 2015; 94: e582–e582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Li Z, Li Z, Xu R, et al. Three-dimensional printing models improve understanding of spinal fracture-a randomized controlled study in China. Sci Rep 2015; 5: 11570–11570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Xu N, Wei F, Liu X, et al. Reconstruction of the upper cervical spine using a personalized 3D-printed vertebral body in an adolescent with Ewing sarcoma. Spine (Phila pa 1976) 2016; 41: E50–E54. [DOI] [PubMed] [Google Scholar]
- 15.Dimnjakovic D, Bojanić I, Smoljanović T, et al. Periarticular osteoid osteoma of the ankle: a report of nine arthroscopically treated patients. J Foot Ankle Surg 2015; 54: 89–93. [DOI] [PubMed] [Google Scholar]
- 16.Dubuc JE, Docquier PL, Schubert T, et al. Diagnosis failure led to the recurrence of an intra-articular osteoid osteoma at the talus neck after arthroscopic excision. Foot Ankle Surg 2014; 20: E40–E42. [DOI] [PubMed] [Google Scholar]
- 17.Sanhudo JA. Osteoid osteoma of the calcaneus mimicking os trigonum syndrome: a case report. Foot Ankle Int 2006; 27: 548–551. [DOI] [PubMed] [Google Scholar]
- 18.Ghanem I. The management of osteoid osteoma: updates and controversies. Curr Opin Pediatr 2006; 18: 36–41. [DOI] [PubMed] [Google Scholar]