Abstract
Objective
To evaluate the anatomical safety margins in relation to thoracic epidural block by analysing magnetic resonance (MR) images.
Methods
This retrospective study identified consecutive patients who underwent MR imaging of the thoracic vertebral spine. The distance from the dura mater to the spinal cord (DTC) was measured at different thoracic intervertebral levels using three different pathways as references: the ‘U’, ‘L’ and ‘M’ lines.
Results
A total of 346 patients provided MR images for analysis. The vertical DTC was the longest at the T5/6 intervertebral level (mean ± SD: 4.22 ± 1.43 mm) and the shortest at the T11/12 intervertebral level (mean ± SD: 2.51 ± 0.87 mm). The DTC was the longest on the ‘L’ line at the T1/2 and T5/6 intervertebral levels and on the ‘U’ line at the T10/11 intervertebral level. The difference in DTC between the ‘U’ and ‘L’ lines was the greatest at the T5/6 intervertebral level.
Conclusion
Differences in the DTC were observed among the thoracic intervertebral levels. The variability of the safety margin according to the angle of needle insertion was the largest at the T5/6 intervertebral level.
Keywords: Thoracic epidural analgesia, distance from dura mater to spinal cord, magnetic resonance image
Introduction
Thoracic epidural analgesia (TEA) has been used to treat acute pain after thoracic and abdominal surgery,1,2 but rare neurological complications related to epidural analgesia can be devastating.3 Thus, it is important to understand the anatomy of the spinal canal to prevent needle-related neurological injury to the spinal cord.
The most common method used to identify the epidural space is the ‘loss of resistance’ (LOR) to either air or fluid technique4 or fluoroscopic guidance. When a dura puncture occurs, the distance from the dura mater to the spinal cord (DTC) is a critical factor in neurological injury caused by needle trauma.5,6 The longer the DTC is, the larger the safety margin will be.5,6
The anatomical dimensions related to TEA, including the DTC, are not uniform at different vertebral levels;7,8 thus, it is necessary to investigate the difference in distance according to the vertebral level to determine the target level and choose a safe method of approach. Several studies have investigated the DTC in the thoracic region and have reported that the vertical distance was significantly greater in the middle thoracic region than at the upper and lower thoracic levels.7,8 However, these studies examined a relatively small number of patients and did not consider the angle at which the needle approached.7,8 Safety margins can change at the same vertical DTC using different approach angles. Previous studies have investigated the DTC at just three regions, rather than at all thoracic intervertebral levels.7,8
The present study retrospectively investigated the DTC at all thoracic segments by analysing the magnetic resonance (MR) images of patients. The length from the skin to the dura mater (STD) and the DTC at various approach lines from three different thoracic vertebral levels were also examined to understand the shape of the interspinous space and develop safe approach strategies.
Patients and methods
Study population
This retrospective study identified consecutive patients at the Seoul National University Boramae Hospital, Seoul, Republic of Korea who underwent MR imaging of the thoracic vertebral segments between January and December 2010. The MR images were evaluated by radiologists. Exclusion criteria were as follows: (i) patients who were diagnosed with thoracic spinal or medullary disease that could affect the contour of the spinal cord and epidural space (e.g. severe compression fracture, spinal cord tumour or cerebrospinal fluid seeding); (ii) patients whose anatomical dimensions were unclear due to poor-quality MR images; (iii) patients < 15 years of age.
Ethical approval was provided by the Institutional Review Board of Seoul National University Boramae Hospital, Seoul, Republic of Korea (reference number: 20120507/06-2012-102/119), which also granted a waiver of informed consent for this retrospective study. This study was registered with the Clinical Research Information Service (http://cris.nih.go.kr/cris/en/use_guide/cris_introduce.jsp; reference number: KCT0001881).
Magnetic resonance image analyses
Magnetic resonance imaging was undertaken on a MAGNETOM® Verio 3.0 T scanner (Siemens, Erlangen, Germany). T2-weighted spine MR images were acquired in the sagittal plane closest to the midline of the vertebral column using a Picture Archiving and Communication System (INFINITT Healthcare, Seoul, Republic of Korea). Three independent medical observers trained in identifying spinal canal anatomy reviewed the images. The most appropriate plane was evaluated at each level and all dimensions are measured using a Preview program (Maroview 5.4; INFINITT Healthcare).
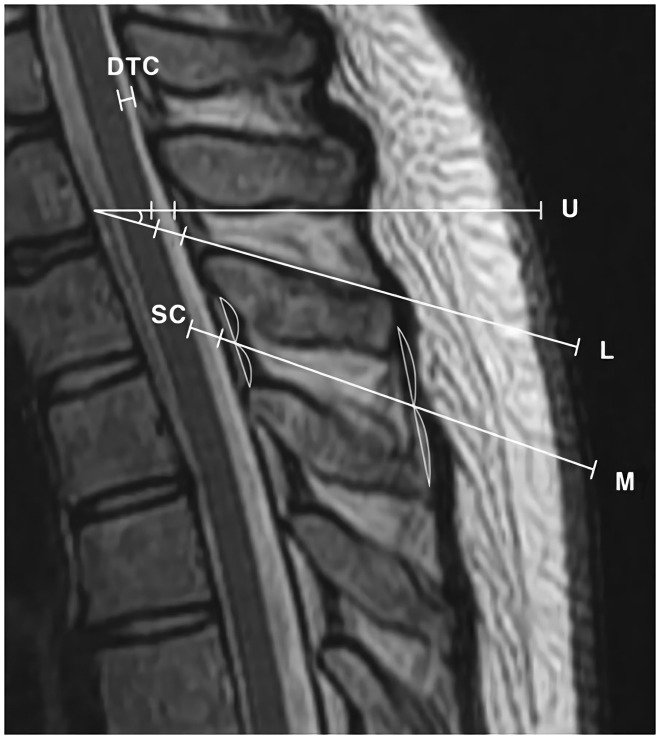
The vertical DTC was measured at each thoracic intervertebral level. The line on the vertical DTC was estimated to be perpendicular to the spinal cord and dura mater at each level and started from the midpoint between two adjacent vertebral bodies (Figure 1). The STD and DTC were measured on three different approach pathways at the upper (T1/2), middle (T5/6), and lower (T10/11) thoracic intervertebral levels. The first approach pathway was the ‘U’ line. The ‘U’ line was defined as the line contacting the lower border of the spinous process of the adjacent upper vertebra at the thoracic intervertebral level. The second was the ‘L’ line, which contacted the upper border of the spinous process of the lower vertebra at the thoracic intervertebral space. Therefore, the ‘U’ and ‘L’ lines were the upper and lower borders of the interspinous space, respectively, and were selected to evaluate the distinct outlines of the interspinous space at different thoracic regions and to demonstrate differences in the safety margin according to various approach angles. The third was the ‘M’ line, which passed the midpoint of two spinous process tips and the point that bisected the ligament flavum between the two spinous processes. The ‘M’ line was supposed to represent a blind approach using the LOR technique. When performing TEA, a physician touches two tips of adjacent spinous processes over the skin and searches for the interspinous space. The midpoint of two adjacent tips was selected as a point on the ‘M’ line. Using the blind technique, a needle can pass several courses in the interspinous space. It was assumed that the point bisecting the ligamentum flavum between the two processes suggested the average of many possible courses and chose that point as another mark on the ‘M’ line.
Figure 1.
Representative T2-weighted spine magnetic resonance image showing the dimensions of the three approaching lines and the angle between the ‘U’ and the ‘L’ lines. The line on the vertical distance from the dura mater to the spinal cord (DTC) was estimated to be perpendicular to the spinal cord (SC) and dura mater at each level and started from the midpoint between the two adjacent vertebral bodies. The ‘U’ line is the line contacting the upper border of the interspinous space and the ‘L’ line contacts the lower border of the interspinous space. The ‘M’ line passes the midpoint of two spinous process tips and the point that bisects the ligamentum flavum between the two spinous processes.
The angles between the ‘U’ and ‘L’ lines at the T1/2, T5/6, and T10/11 intervertebral levels were examined to analyse the trend in the borders of the interspinous spaces and to evaluate variability in the approach angle at each intervertebral level (Figure 1).
Statistical analyses
For each variable (DTC and STD), an intraclass correlation coefficient (ICC) was calculated to quantify agreement between measurements: slight (0.00–0.19), fair (0.20–0.39), moderate (0.40–0.59), substantial (0.60–0.79), and almost perfect (0.80–1.0) agreement.
All statistical analyses were performed using the SPSS® statistical package, version 19.0 (SPSS Inc., Chicago, IL, USA) for Windows®. Continuous variables are expressed as the mean ± SD and were compared using paired t-tests. Multiple pairwise comparisons were made using the Bonferroni correction. A P-value < 0.05 was considered statistically significant.
Results
This retrospective study identified 870 consecutive patients who had undergone MR imaging of the thoracic vertebral segments. Of these, 421 patients who were diagnosed with thoracic spinal or medullary disease that could affect the contour of the spinal cord and epidural space, 67 patients whose anatomical dimensions were unclear due to poor-quality MR images and 36 patients who were<15 years of age were excluded. A total of 346 MRI images from 177 males and 169 females were evaluated and their demographic characteristics are presented in Table 1.
Table 1.
Demographic characteristics of patients (n = 346) who had undergone magnetic resonance imaging of the thoracic vertebral segments and who were included in this analysis of the anatomical safety margins in relation to thoracic epidural block.
| Characteristic | Value |
|---|---|
| Age, years | 51.0 ± 17.2 |
| Sex, male/female | 177/169 |
| Height, cm | 163.4 ± 8.9 |
| Weight, kg | 59.9 ± 11.9 |
| Body mass index, kg/m2 | 22.4 ± 3.7 |
Data presented as mean ± SD or n of patients.
The vertical DTC was the longest at the T5/6 level and the shortest at the T11/12 level (4.22 ± 1.43 and 2.51 ± 0.87 mm, respectively) (Table 2). A significant difference was observed for the DTC at all intervertebral levels compared with the adjacent levels, indicating a significant difference in the safety margin between adjacent thoracic levels (P < 0.01; Bonferroni correction).
Table 2.
The distance from the dura mater to the spinal cord (DTC) at thoracic intervertebral levels in patients (n = 346) who had undergone magnetic resonance imaging of the thoracic vertebral segments and who were included in this analysis of the anatomical safety margins in relation to thoracic epidural block.
| Intervertebral level | DTC, mma | ICC (95% CI) |
|---|---|---|
| T1/2 | 2.91 ± 0.90 | 0.79 (0.34, 0.95) |
| T2/3 | 3.52 ± 1.12 | 0.82 (0.45, 0.96) |
| T3/4 | 3.84 ± 1.23 | 0.88 (0.64, 0.97) |
| T4/5 | 4.15 ± 1.42 | 0.88 (0.60, 0.98) |
| T5/6 | 4.22 ± 1.43 | 0.95 (0.83, 0.99) |
| T6/7 | 4.10 ± 1.46 | 0.91 (0.73, 0.96) |
| T7/8 | 3.87 ± 1.26 | 0.73 (0.20, 0.93) |
| T8/9 | 3.35 ± 1.17 | 0.63 (0.49, 0.72) |
| T9/10 | 2.96 ± 1.05 | 0.66 (0.02, 0.91) |
| T10/11 | 2.83 ± 0.92 | 0.67 (0.48, 0.88) |
| T11/12 | 2.51 ± 0.87 | 0.74 (0.20, 0.94) |
Data presented as mean ± SD.
A significant difference was observed for DTC compared with the adjacent levels (Bonferroni correction; P < 0.01).
ICC, intraclass correlation coefficient; CI, confidence interval.
The STD and DTC were the longest on the ‘L’ line at the T1/2 and T5/6 levels; and longest on the ‘U’ line at the T10/11 level (Table 3). The angle between the ‘U’ and ‘L’ lines was the largest at the T1/2 level, narrowed from the upper to the lower region, and the difference in DTC between the ‘U’ and ‘L’ lines was the greatest at the T5/6 intervertebral level, where the vertical DTC was the longest (Table 4). In 32 of 346 patients (9%), the ‘M’ lines at the T10/11 intervertebral level did not pass through the interspinous space on the MR images.
Table 3.
Differences among the ‘U’, ‘M’ and ‘L’ lines at the T1/2, T5/6 and T10/11 intervertebral levels in patients (n = 346) who had undergone magnetic resonance imaging of the thoracic vertebral segments and who were included in this analysis of the anatomical safety margins in relation to thoracic epidural block.
| Intervertebral level | Line | STD, mm | DTC, mm |
|---|---|---|---|
| T1/2 | U | 55.12 ± 9.60 (0.60) | 3.13 ± 0.96 (0.48) |
| M | 56.73 ± 9.45 (0.55) | 3.30 ± 1.15 (0.51) | |
| L | 60.27 ± 9.88a (0.52) | 3.77 ± 1.23a (0.44) | |
| T5/6 | U | 68.23 ± 15.15 (0.66) | 8.64 ± 5.37 (0.79) |
| M | 69.56 ± 15.17 (0.71) | 8.85 ± 5.23 (0.88) | |
| L | 80.05 ± 16.41a (0.69) | 11.68 ± 7.21a (0.82) | |
| T10/11 | U | 51.66 ± 10.72b (0.64) | 3.56 ± 1.61b (0.62) |
| M | 49.50 ± 9.30 (0.71) | 3.21 ± 1.12 (0.52) | |
| L | 49.62 ± 9.46 (0.63) | 3.23 ± 1.10 (0.46) |
Data presented as mean ± SD (ICC).
A significant difference compared with corresponding values on ‘U’ and ‘M’ lines at the same intervertebral level (Bonferroni correction; P < 0.01).
A significant difference compared with corresponding values on ‘M’ and ‘L’ lines at the T10/11 intervertebral level (Bonferroni correction; P < 0.05).
ICC, intraclass correlation coefficient.
Table 4.
Angles and differences between the ‘U’ and ‘L’ lines at T1/2, T5/6 and T10/11 intervertebral levels in patients (n = 346) who had undergone magnetic resonance imaging of the thoracic vertebral segments and who were included in this analysis of the anatomical safety margins in relation to thoracic epidural block.
| Intervertebral level | Angle between U and L, ° | DTC (L) – DTC (U), mm |
|---|---|---|
| T1/2 | 14.6 ± 8.1* | 0.6 ± 0.3* |
| T5/6 | 9.1 ± 6.1* | 3.0 ± 3.8* |
| T10/11 | 2.2 ± 11.1* | 1.9 ± 1.1* |
Data presented as mean ± SD.
A significant difference was observed compared with another level (Bonferroni correction; P < 0.01).
DTC, distance from the dura mater to the spinal cord.
Discussion
The course of needle insertion when performing TEA using the midline approach is from the skin to the ligamentum flavum, and the needle should stop before piercing the dura mater for correct epidural needle placement. However, accidental dura puncture during epidural analgesia occurs in 0.4–6.0% of patients.9
This present study identified the anatomical dimensions of the thoracic spinal canal in relation to TEA by MR imaging. Reproducibility of measurements was verified by calculation of the ICCs between measurements. These current results revealed that the vertical DTC was longer in the middle thoracic region than at the upper or lower thoracic levels and the shortest at the T11/12 levels. These current results were in good agreement with prior studies of the thoracic spinal canal.8,10 The spinal cord in the middle thoracic area is situated more ventrally, but the spinal cord occupies more space at the upper and lower thoracic levels because of cervical and lumbar enlargement. Several previous studies indicated that ligamentum flavum midline gaps at the thoracic vertebral levels were more frequent than at the lumbar levels but less frequent at the cervical levels.11–13 The peak incidence among the thoracic vertebral levels was found in the region between T10 and T12.12 Midline gaps were also frequent at the upper thoracic level.13 In contrast to the hanging-drop technique, the LOR technique is considered to be dependent on the penetration of the ligamentum flavum.4 Therefore, the midline approach using the LOR technique at the lower or upper thoracic level could be especially dangerous, not only due to a short DTC but also due to the midline fusion defect.
This present study investigated the vertical DTC at all thoracic levels and the current results will be helpful to determine the level at which epidural catheterization should be performed. Because a comparable effect of TEA can be expected from different thoracic levels by adjusting the drug dose or extent of catheter insertion, there are several possible target levels for needle insertion for an intended level of segmental block. Therefore, a significant difference in the vertical DTC between adjacent thoracic intervertebral levels is valuable to select an insertion point with a larger safety margin. Ensuring a larger distance is one strategy to increase the safety margin during TEA and, of course, during spinal anaesthesia. A recent report presented a case of segmental spinal anaesthesia for cholecystectomy in a patient with severe lung disease.14
The present study demonstrated that the angle between the ‘U’ and ‘L’ lines was the largest at the T1/2 level. The larger the angle is between the ‘U’ and ‘L’ lines, the higher the flexibility will be regarding the angle of needle insertion at the interspinous space. However, the objective difference in DTC between the ‘U’ and ‘L’ lines was greatest at the T5/6 level, where the vertical DTC was longest, indicating that variability in the safety margin according to the needle insertion angle was the largest at T5/6 and that the increase in the safety margin was most significant at the mid-thoracic region. Thus, the STD and DTC on the ‘L’ line were longer than those on the ‘U’ line or ‘M’ line at the T1/2 and T5/6 levels. By contrast, the STD and DTC were the longest on the ‘U’ line at the lower thoracic region of T10/11. Therefore, we speculate that TEA can be managed more safely by inserting a needle through a pathway near the lower border of the interspinous space at the upper or middle thoracic region and near the upper border at lower levels than by approaching from a random direction, as represented by the ‘M’ line.
The ‘U’ line at the upper or middle thoracic region and the ‘L’ line at lower levels might not be the longest pathway possible in the intervertebral space. For example, a line that starts from the posterior part of the lower border to the upper end of the ligamentum flavum suggests a greater safety margin than the ‘L’ line. Therefore, the ‘U’ and ‘L’ lines are not absolute clinical guides for safety but references that can be used to understand the anatomy of the thoracic vertebral spine.
This present study had a number of limitations. First, approximately 9% of all patients (32 of 346) had ‘M’ lines at the T10/11 intervertebral level that did not pass through the interspinous space on the MR images. This was because the lower thoracic spinous processes have more variable shapes, and the midpoint of two adjacent tips can be far apart from the centre of the posterior interspinous space. In those patients, the ‘M’ line does not represent a blind approach and is just an imaginary line. Secondly, all of the data in this study were measured using supine MR images. However, most neuraxial blockades are performed with patients in the lateral decubitus position with or without leg flexion. Previous studies have demonstrated that the spinal cord and cauda equina move with gravity and also ventrally with leg flexion.7,15,16 Consequently, it is expected that the safety margin would be greater in a lateral than a supine position. However, whether the correlation between spinal structure and vertebral level would be maintained using a lateral posture is uncertain. Supplementary studies are needed to elucidate the effect of various postures on the thoracic vertebral canal.
In conclusion, there were differences in the DTC among thoracic intervertebral levels, the longest being at the T5/6 level and the shortest at the T11/12 level. By comparing different approach angles, the safety margin was found to be the longest on the ‘L’ line at the T1/2 and T5/6 levels and the longest on the ‘U’ line at lower thoracic regions. The variability of the safety margin according to the angle of needle insertion was the largest at T5/6. These differences merit consideration to prevent serious cord damage in association with TEA.
Declaration of conflicting interests
The authors declare that there are no conflicts of interest.
Funding
This work was supported by a Kangwon National University research grant.
References
- 1.Kehlet H, Dahl JB. The value of “multimodal” or “balanced analgesia” in postoperative pain treatment. Anesth Analg 1993; 77: 1048–1056. [DOI] [PubMed] [Google Scholar]
- 2.Rosenberg PH, Heino A, Scheinin B. Comparison of intramuscular analgesia, intercostal block, epidural morphine and on-demand-i.v.-fentanyl in the control of pain after upper abdominal surgery. Acta Anaesthesiol Scand 1984; 28: 603–607. [DOI] [PubMed] [Google Scholar]
- 3.Kasai T, Yaegashi K, Hirose M, et al. Spinal cord injury in a child caused by an accidental dural puncture with a single-shot thoracic epidural needle. Anesth Analg 2003; 96: 65–67. [DOI] [PubMed] [Google Scholar]
- 4.Schier R, Guerra D, Aguilar J, et al. Epidural space identification: a meta-analysis of complications after air versus liquid as the medium for loss of resistance. Anesth Analg 2009; 109: 2012–2021. [DOI] [PubMed] [Google Scholar]
- 5.van Zundert AA, Stultiens G, Jakimowicz JJ, et al. Laparoscopic cholecystectomy under segmental thoracic spinal anaesthesia: a feasibility study. Br J Anaesth 2007; 98: 682–686. [DOI] [PubMed] [Google Scholar]
- 6.Imbelloni LE, Fornasari M, Fialho JC. Combined spinal epidural anesthesia during colon surgery in a high-risk patient: case report. Rev Bras Anestesiol 2009; 59: 741–745. [in Portuguese, English Abstract]. [DOI] [PubMed] [Google Scholar]
- 7.Lee RA, van Zundert AA, Botha CP, et al. The anatomy of the thoracic spinal canal in different postures: a magnetic resonance imaging investigation. Region Anesth Pain Med 2010; 35: 364–369. [DOI] [PubMed] [Google Scholar]
- 8.Lee RA, van Zundert AA, Breedveld P, et al. The anatomy of the thoracic spinal canal investigated with magnetic resonance imaging (MRI). Acta Anaesthesiol Belg 2007; 58: 163–167. [PubMed] [Google Scholar]
- 9.Berger CW, Crosby ET, Grodecki W. North American survey of the management of dural puncture occurring during labour epidural analgesia. Can J Anaesth 1998; 45: 110–114. [DOI] [PubMed] [Google Scholar]
- 10.Imbelloni LE, Quirici MB, Ferraz Filho JR, et al. The anatomy of the thoracic spinal canal investigated with magnetic resonance imaging. Anesth Analg 2010; 110: 1494–1495. [DOI] [PubMed] [Google Scholar]
- 11.Lirk P, Moriggl B, Colvin J, et al. The incidence of lumbar ligamentum flavum midline gaps. Anesth Analg 2004; 98: 1178–1180. [DOI] [PubMed] [Google Scholar]
- 12.Lirk P, Colvin J, Steger B, et al. Incidence of lower thoracic ligamentum flavum midline gaps. Br J Anaesth 2005; 94: 852–855. [DOI] [PubMed] [Google Scholar]
- 13.Lirk P, Kolbitsch C, Putz G, et al. Cervical and high thoracic ligamentum flavum frequently fails to fuse in the midline. Anesthesiology 2003; 99: 1387–1390. [DOI] [PubMed] [Google Scholar]
- 14.van Zundert AA, Stultiens G, Jakimowicz JJ, et al. Segmental spinal anaesthesia for cholecystectomy in a patient with severe lung disease. Br J Anaesth 2006; 96: 464–466. [DOI] [PubMed] [Google Scholar]
- 15.Takiguchi T, Yamaguchi S, Okuda Y, et al. Deviation of the cauda equina by changing position. Anesthesiology 2004; 100: 754–755. [DOI] [PubMed] [Google Scholar]
- 16.Takiguchi T, Yamaguchi S, Hashizume Y, et al. Movement of the cauda equina during the lateral decubitus position with fully flexed leg. Anesthesiology 2004; 101: 1250–1250. [DOI] [PubMed] [Google Scholar]