Abstract
Objective
To evaluate effects attributable to age, time period and birth cohort, on stroke mortality data from urban and rural regions in China between 1988 and 2013.
Methods
Mortality data were obtained from the Chinese Health Statistics Annual Report (1987–2001) and Chinese Health Statistics Yearbooks (2003–2014). Population data were obtained from population censuses (i.e. 1982, 1990, 2000 and 2010). Data were analysed using an age-period-cohort (APC) model and intrinsic estimation (IE) method.
Results
The age effect suggested that all older residents had higher stroke mortality risk than younger residents. Period effect showed that compared with figures for 1988, stroke mortality in 2013 was 1.8 times higher for urban regions and 2.4 times higher for rural regions. After controlling for age and period effects, cohorts born before the Chinese economic reform had a steady decline in stroke mortality. However, mortality rates increased and fluctuated in post-reform cohorts.
Conclusions
This APC-IE analysis identified a modest period effect with large age and cohort contributions to both the overall mortality and the disparity between urban and rural stroke mortality. Identifying early life and cumulative risk factors for stroke, improving equality in stroke prevention and care are needed to reduce the stroke mortality in China.
Keywords: China, mortality, stroke, age-period-cohort analysis, intrinsic estimator, rural, urban
Introduction
Stroke or a cerebrovascular accident, is a common cause of death and a leading cause of long-term, severe disability in both developed and developing countries.1 In China, stroke is becoming the leading cause of death and adult disability.2 Stroke mortality accounts for 19% of the total mortality rate and exceeds ischaemic heart disease mortality, which accounts for 8% of all deaths.3 It has been estimated that China has 2.5 million new stroke cases each year and 7.5 million stroke survivors.4
Historically, China had a higher stroke mortality rate in urban areas compared with rural areas.4 By contrast, in developed countries, the risk of stroke has always tended to be higher among economically disadvantaged populations than better-off ones.5,6 However, the burden of stroke in China is shifting; two studies have reported that stroke mortality rates in rural areas now exceed rates in urban regions.7,8 One study found that there was a significant decrease in stroke mortality in urban areas compared with rural areas where stroke mortality barely changed.7 In addition, the fall in the mortality rate in urban regions was mainly among elderly subjects aged 55–74 years.7
To understand factors that contribute to the urban–rural shift in stroke mortality in China and to determine if age is an important factor, it is important to examine macro-level trends from multiple dimensions. Biological, historical and/or social factors may explain the dependent effects of age, period and cohort that bridge the gap between a micro-level theory and a macro-level phenomenon.9–11 The challenge in evaluating temporal patterns in stroke mortality is finding the best way to deconstruct the effects of cohort, age and time-period.9 The age-period-cohort (APC) analysis has been suggested as being one of the best ways to tease out the effects of each factor.9 The model has been widely used in sociological, demographical and epidemiologic studies.12 Accordingly, empirical studies from several countries have examined stroke incidence and trends in mortality using the APC analysis.13,14 However, a recent methodological development in APC analysis, namely the Intrinsic Estimator (IE), which has been shown to resolve identification of various sources of variation and improve the validity of the APC model, has not previously been used.9,12,15,16
To the best of our knowledge, few studies have examined the effect of age, period and cohort on trends in stroke mortality in China. Therefore, the objective of this present study was to evaluate stroke mortality in urban and rural regions in China between 1988 and 2013 using an IE-based APC analysis that would hopefully provide useful information for policy makers.
Materials and methods
Stroke mortality data collection
For data preceding 2002, stroke was defined using codes ICD-9 430 to 438 and for data from 2002 onwards the codes used were ICD-10 I60 to I69. These codes have been used by researchers investigating trends in stroke mortality in other countries.15 Data were obtained on annual stroke mortalities from the Chinese Health Statistics Annual Report (1987–2001) and Chinese Health Statistics Yearbooks (2003–2014). Data were collected from 117 urban area districts and 315 rural area counties from all 31 provinces.17 Information about the Chinese population was obtained from the population censuses (i.e. 1982, 1990, 2000 and 2010). These data are separated into 18, 5-year age groupings by sex and location (i.e. urban/ rural). Using the two pieces of information, age- and regional-specific stroke deaths were computed for six time periods (P) over the years 1988 and 2013 and 13 age groups (A) for the population aged between 20–84 years. In addition, 18 birth cohorts (C) were selected beginning with those born 1904–08 and aged 80–84 in 1988 and ending with those born in 1989–93 and aged 20–24 in 2013. Subjects over 85 years were not included.
Statistical analyses
This study used advanced APC modelling to examine temporal changes in Chinese adult stroke mortality from 1987 to 2013 and the analysis was performed by one of the authors (Y.S.). The basic APC model is based on a log-linear model for the expected rates with additive effects for age, period, and cohort.12 The model can be written as follows:
where rAPC represents the expected stroke mortality rate in an age-period-cohort group (A, P, C); sAPC denotes the expected number of stroke deaths; nAPC is the population at risk; α is the intercept or adjusted mean stroke mortality rate; βA is the effect for age groups A = 1,…, a; γP is the effect for time periods P = 1,…, p; and δC is the effect for cohorts C = 1,…, c.
The APC model cannot be estimated using conventional regression techniques because of an identification problem.9,16 Any two factors (e.g. age and birth) enable the prediction of the third factor (i.e. time period).16 The latest IE algorithm for the APC model has been shown to be estimable, non-biased, valid, and asymptotic and can solve the identification problem of the classical APC model.15 In this present study, data were analysed using the APC_IE model and it was evaluated using Akaike’s Information Criteria and Bayesian Information Criteria.12 The APC_IE model produces coefficients of the effects of age, period, and cohort and these coefficients provide estimates of the mean change in stroke associated with a particular APC group relative to the mean for all APC groups combined. The standard error (SE) for every model coefficient was calculated. The log-likelihood test was used to test the significance of the coefficient estimates. Additionally, rate ratios were calculated from estimated model parameters which represented the mortality level. Mortality change was expressed by the difference in rate ratio before and after the birth cohort.
All data analyses were performed using Stata Statistical Software (Release 14; StataCorp LP, College Station, TX, USA). A P-value < 0.05 was considered to indicate statistical significance.
Results
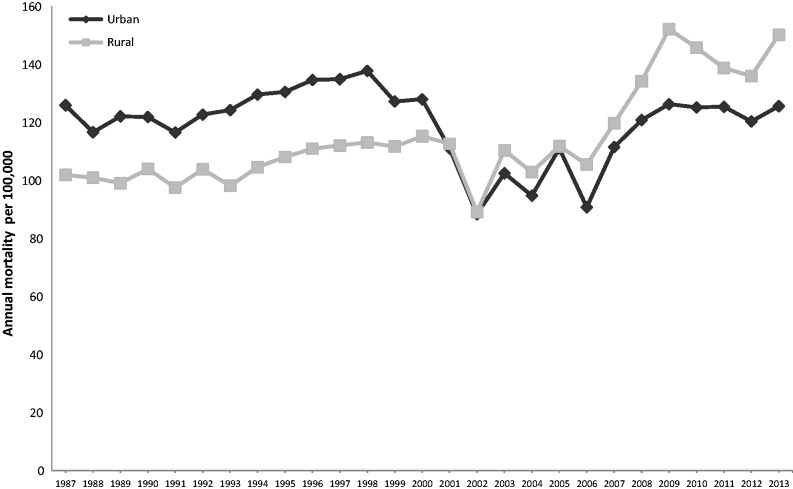
Crude stroke mortality rates for both urban and rural Chinese residents from 1987 to 2013 are shown in Figure 1. The data show that until 2001, rates were higher in the urban population compared with the rural population. Stroke mortality rates in both populations then declined to their lowest values in 2003, but over the past 10 years have increased to previous levels and are now greater in the rural residents compared with urban residents.
Figure 1.
Overall stroke mortality in China, 1987–2013.
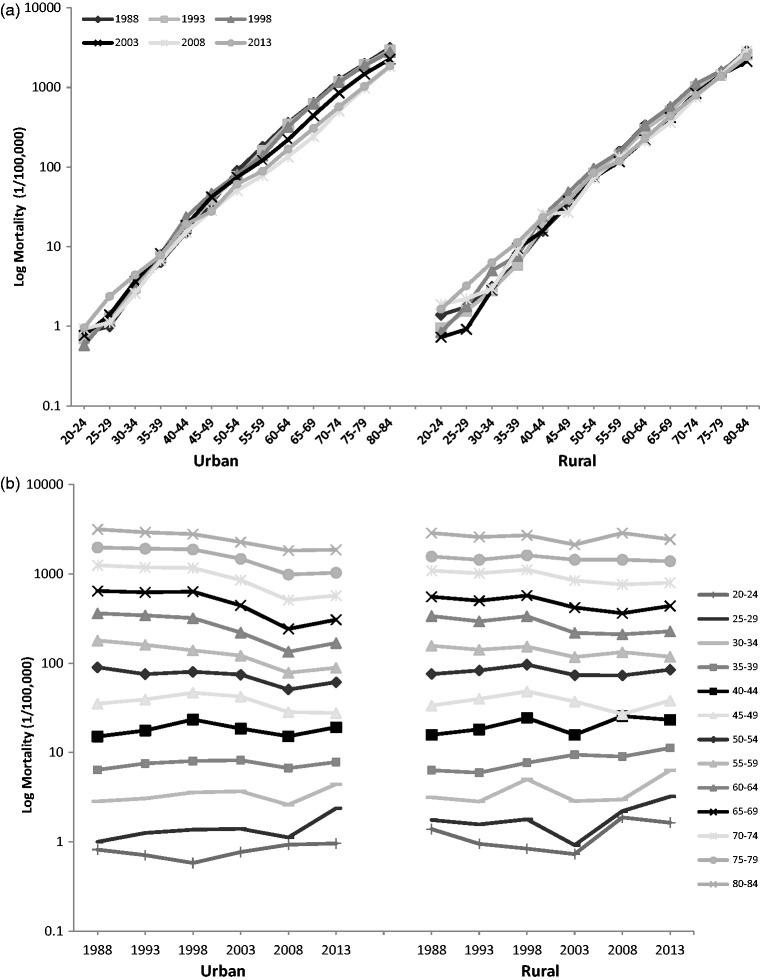
Age-specific variations in stroke mortality in China across the six periods for 1988, 1993, 1998, 2003, 2008 and 2013 are shown in Figure 2a and variations in stroke mortality by age group over the years 1988 to 2013 (i.e. period-based variation) are shown in Figure 2b. Both urban and rural regions exhibited a log linear correlation and shared the same pattern for stroke mortality with mortality increasing by age group (Figure 2a). The pattern of period-based variation was different across age-groups in urban populations compared with rural populations (Figure 2b). In rural regions, younger age-groups appeared to have large variations, whereas in urban population older age groups had large variations (Figure 2b).
Figure 2.
Advanced age-period-cohort modelling analysis to examine temporal changes in adult stroke mortality from 1988 to 2013. Age-specific log stroke deaths per 100 000 of the population across the 13 age groups (a). Period-based effect on log stroke deaths per 100 000 of the population across the 13 different age groups over 1988–2013 (b). Cohort-based variation of age-specific log stroke deaths per 100 000 of the population for the 13 age groups (c).
A cohort-based variation of age-specific mortality was constructed to evaluate the birth cohort effect (Figure 2c). With the exception of Group 80–84 in the urban region whose mortality rate decreased continuously, stroke mortality for all age groups fluctuated between the different cohort years. Generally, younger groups had less stroke mortality.
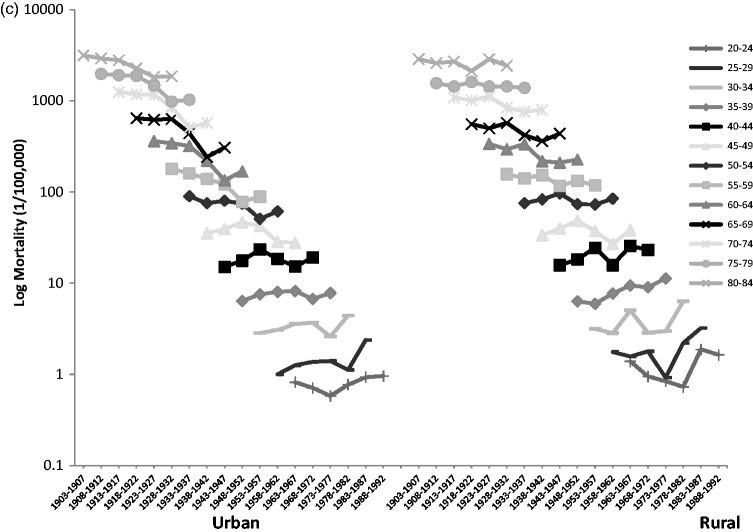
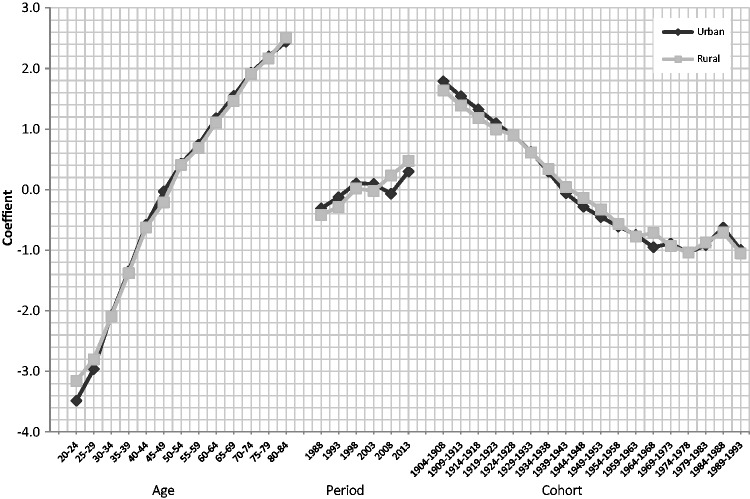
Graphs of the APC coefficients were generated to show the net effects of age, period and cohort on overall mortality trends (Figure 3). For urban residents, the adjusted mean stroke mortality rate over the entire period was approximately 62.7 per 100 000 (i.e. the exponential of the intercept, –7.37) and for rural residents it was approximately 68.7 per 100 000 (i.e. the exponential of the intercept, –7.28) (Table 1). The same age pattern of stroke death risk was observed for both urban and rural residents, with the 20–24 years age group having the lowest stroke mortality and the 80–84 years age group having the highest (Table 1 and Figure 3). Compared with the overall adjusted mean mortality rate, the mortality risk of the 80–84 year old residents was 11.5 times higher for urban residents and 12.3 times higher for rural residents (Table 1). Rural residents had a stronger age effect on mortality among younger adults (i.e. 20–24 and 25–29 age groups) compared with urban residents but a weaker age effect on mortality was observed in the 45–49 age-group (Figure 3).
Figure 3.
Age-period-cohort effects on stroke mortality in China from 1988–2013.
Table 1.
Age-period-cohort (APC) model analysis of stroke mortality in urban and rural China showing the results of APC analysis using the intrinsic estimator approach.15
| Urban |
Rural |
|||||||
|---|---|---|---|---|---|---|---|---|
| APC | SE | 95% CI | Rate ratio* | APC | SE | 95% CI | Rate ratio* | |
| Intercept | −7.37 | 0.03 | −7.44, −7.31 | 0.00 | −7.28 | 0.05 | −7.38, −7.19 | 0.00 |
| Age (year) | ||||||||
| 20–24 | −3.49 | 0.23 | −3.94, −3.03 | 0.03 | −3.16 | 0.29 | −3.73, −2.59 | 0.04 |
| 25–29 | −2.96 | 0.17 | −3.29, −2.63 | 0.05 | −2.80 | 0.23 | −3.25, −2.35 | 0.06 |
| 30–34 | −2.07 | 0.12 | −2.32, −1.83 | 0.13 | −2.09 | 0.17 | −2.43, −1.75 | 0.12 |
| 35–39 | −1.34 | 0.09 | −1.53, −1.16 | 0.26 | −1.38 | 0.13 | −1.63, −1.13 | 0.25 |
| 40–44 | −0.58 | 0.08 | −0.72, −0.43 | 0.56 | −0.62 | 0.10 | −0.82, −0.43 | 0.54 |
| 45–49 | −0.03 | 0.06 | −0.15, 0.09 | 0.97 | −0.21 | 0.08 | −0.37, −0.05 | 0.81 |
| 50–54 | 0.43 | 0.05 | 0.33, 0.53 | 1.54 | 0.41 | 0.07 | 0.28, 0.54 | 1.51 |
| 55–59 | 0.74 | 0.04 | 0.66, 0.83 | 2.10 | 0.69 | 0.06 | 0.58, 0.80 | 1.99 |
| 60–64 | 1.18 | 0.03 | 1.11, 1.25 | 3.25 | 1.11 | 0.04 | 1.02, 1.20 | 3.03 |
| 65–69 | 1.55 | 0.03 | 1.49, 1.60 | 4.69 | 1.46 | 0.04 | 1.39, 1.54 | 4.32 |
| 70–74 | 1.93 | 0.03 | 1.88, 1.98 | 6.90 | 1.91 | 0.04 | 1.84, 1.99 | 6.77 |
| 75–79 | 2.20 | 0.03 | 2.14, 2.26 | 9.01 | 2.17 | 0.04 | 2.09, 2.25 | 8.75 |
| 80–84 | 2.44 | 0.04 | 2.37, 2.52 | 11.49 | 2.51 | 0.05 | 2.41, 2.61 | 12.31 |
| Period (year) | ||||||||
| 1988 | −0.31 | 0.03 | −0.37, −0.25 | 0.73 | −0.42 | 0.05 | −0.51, −0.33 | 0.66 |
| 1993 | −0.12 | 0.02 | −0.17, −0.08 | 0.89 | −0.29 | 0.03 | −0.35, −0.22 | 0.75 |
| 1998 | 0.10 | 0.02 | 0.07, 0.14 | 1.11 | 0.02 | 0.02 | −0.02, 0.07 | 1.02 |
| 2003 | 0.09 | 0.02 | 0.06, 0.13 | 1.10 | −0.02 | 0.02 | −0.07, 0.02 | 0.98 |
| 2008 | −0.07 | 0.02 | −0.11, −0.02 | 0.94 | 0.23 | 0.03 | 0.17, 0.29 | 1.26 |
| 2013 | 0.30 | 0.03 | 0.24, 0.36 | 1.35 | 0.47 | 0.04 | 0.40, 0.55 | 1.61 |
| Cohort (years) | ||||||||
| 1904–1908 | 1.79 | 0.07 | 1.65, 1.92 | 5.97 | 1.64 | 0.10 | 1.45, 1.83 | 5.15 |
| 1909–1913 | 1.54 | 0.05 | 1.44, 1.65 | 4.68 | 1.39 | 0.07 | 1.25, 1.54 | 4.02 |
| 1914–1918 | 1.32 | 0.04 | 1.24, 1.41 | 3.76 | 1.19 | 0.06 | 1.07, 1.30 | 3.27 |
| 1919–1923 | 1.09 | 0.04 | 1.03, 1.16 | 2.99 | 1.00 | 0.05 | 0.90, 1.09 | 2.71 |
| 1924–1928 | 0.90 | 0.03 | 0.84, 0.96 | 2.46 | 0.90 | 0.04 | 0.82, 0.98 | 2.46 |
| 1929–1933 | 0.63 | 0.03 | 0.57, 0.69 | 1.87 | 0.61 | 0.04 | 0.53, 0.70 | 1.85 |
| 1934–1938 | 0.29 | 0.04 | 0.22, 0.36 | 1.34 | 0.34 | 0.05 | 0.24, 0.43 | 1.40 |
| 1939–1943 | −0.06 | 0.05 | −0.15, 0.03 | 0.94 | 0.04 | 0.06 | −0.08, 0.16 | 1.04 |
| 1944–1948 | −0.28 | 0.05 | −0.39, −0.18 | 0.76 | −0.13 | 0.07 | −0.28, 0.01 | 0.87 |
| 1949–1953 | −0.45 | 0.06 | −0.58, −0.33 | 0.64 | −0.32 | 0.09 | −0.49, −0.16 | 0.72 |
| 1954–1958 | −0.61 | 0.07 | −0.75, −0.47 | 0.55 | −0.56 | 0.10 | −0.76, −0.37 | 0.57 |
| 1959–1963 | −0.75 | 0.08 | −0.91, −0.58 | 0.48 | −0.77 | 0.12 | −1.01, −0.54 | 0.46 |
| 1964–1968 | −0.95 | 0.10 | −1.14, −0.76 | 0.39 | −0.71 | 0.13 | −0.97, −0.46 | 0.49 |
| 1969–1973 | −0.89 | 0.11 | −1.11, −0.67 | 0.41 | −0.93 | 0.15 | −1.23, −0.63 | 0.40 |
| 1974–1978 | −1.04 | 0.15 | −1.33, −0.75 | 0.35 | −1.04 | 0.21 | −1.45, −0.63 | 0.35 |
| 1979–1983 | −0.92 | 0.19 | −1.30, −0.54 | 0.40 | −0.87 | 0.28 | −1.42, −0.32 | 0.42 |
| 1984–1988 | −0.63 | 0.25 | −1.12, −0.14 | 0.54 | −0.71 | 0.35 | −1.40, −0.01 | 0.49 |
| 1989–1993 | −0.99 | 0.46 | −1.89, −0.10 | 0.37 | −1.05 | 0.62 | −2.26, 0.16 | 0.35 |
Rate ratios were calculated from estimated model parameters that represented the mortality level. Mortality change was expressed by the difference in rate ratio before and after the birth cohort.
Emboldened values are statistically significant at P < 0.05.
SE, standard error; CI, confidence interval.
After controlling for both age and cohort effects, analysis showed that the period effect on stroke mortality was modest (Table 1 and Figure 3). The variation in stroke mortality by period followed a similar pattern to that observed for overall mortality rates. However, the period effect had a bigger impact on rural residents compared with urban residents after 2003. Figure 3 also shows the net cohort effect on stroke mortality rates for urban and rural residents. For the birth cohorts born before 1924, the cohort effect on stroke mortality was greater for urban residents compared with rural residents. For cohorts born between 1934 and 1973, the cohort effect on stroke mortality was greater for rural residents compared with urban residents. For the cohort born after 1974, both urban and rural residents shared the same trend in cohort effect; the mortality rate increased year on year from 1974 to1988 and then declined.
Discussion
In this present study, Chinese stroke mortality data were analysed by the APC_IE model that identified a modest but critical period effect, accompanied by substantial age and cohort effects over the years 1987 to 2013. According to the principle of the APC model, cohort effects should account for any historical influences on individuals and the period effect should assess any contemporaneous factors across the cohorts.18 The findings of this study indicate that the Chinese government faces serious challenges with regard to stroke mortality. For example, Chinese society is aging rapidly; in 2015, the proportion of people aged 65 or above was approximately 10%, but it is estimated that this proportion will rise rapidly and reach 25% in 2040–2050 and the population aged 65 and above is estimated to reach 300 million by 2040.19 The largely expanding elderly population will enhance the age effect on stroke mortality observed in this study and so will increase the burden of stroke for the Chinese health authorities.
The cohort effect on stroke mortality in the present study has probably been influenced by socioeconomic developments in China. This current analysis showed a large continuous decline in the cohort effect on stroke mortality for both urban and rural residents from those born in the earliest cohort dates (i.e. 1903–1907) to those born in the period after the reform and opening-up policy (i.e. 1988–1992). Therefore, perhaps stable domestic environments, reduced exposure to infectious diseases, improved nutrition, improved health services and increased access to health services, may have all contributed to the improved cohort survival rate.20 Interestingly, the rural population had a slower decline in stroke mortality than the urban population, which suggests that rural regions are lagging behind urban regions in socioeconomic improvement. For cohorts from 1974 to 1988, the increase in stroke mortality may be explained by changes in other major stroke risk factors such as unbalanced nutrition and unhealthy lifestyles (e.g. high calorie diets, less exercise, increased smoking and alcohol use).21 Without preventative interventions targeting unhealthy lifestyles and poor diet, these current findings suggest that stroke mortality rates will presumably rise again, especially in young adults.
Although the period effect was relatively modest compared with the age and cohort effects, the period effect may have been the main determinant of final stroke mortality for a specific year and might explain the urban/rural disparity of stroke mortality among different years. We suggest that several risk factors such as environmental change, access to health care services and economic difference may have caused the increase in stroke mortality attributed to the period effect for 1988 to 2013. For example, with regard to environmental influences, China is currently facing the worst and continuous air pollution problems in the world22 and empirical studies have suggested ambient air pollution may be responsible for stroke mortality.23–25 In addition, critical differences in access to health care services may also explain the urban/rural differences in the period effect.26 China switched to a market-oriented health care system in the late 1970s,27,28 but the profit-seeking policy resulted in the collapse of basic and essentially free health care under the Cooperative Medical Scheme and caused a rapid escalation of health care costs in the 1980s, which hit the rural residents particularly hard. By contrast, over the same period, urban residents were protected by an employment-based health insurance scheme.29 With regard to economic differences, despite the introduction of the New Cooperative Medical Scheme in 2003 that aimed to subsidize Chinese rural residents and reduce the risk of disastrous medical costs,30 research suggests that socioeconomic status remains a fundamental cause of mortality.31 The income gap between urban and rural residents in China has continued to widen over recent years from an income ratio of 1.82 to 1 in 1983, to 3.33 to 1 in 2009.32 It has been suggested that rural residents are more likely to give up seeking medication for diseases such as stroke because paying for necessary services could plunge families into bankruptcy.33
This present study had several limitations. First, it did not differentiate the different subtypes of stroke because it was thought that the involvement of more strata in the analyses may have decreased the statistical power to detect small or modest effects in the three distinctive temporal effects since APC analysis is a data-thirst analytical tool.15 Also, differentiating stroke subtypes may have introduced measurement error because disadvantaged rural areas have less precision in their diagnoses compared with urban areas.34,35 Distinguishing stroke subtypes will be a goal for any future research that is undertaken. Secondly, the disease coding procedures changed in 2001 and the ICD-10 coding that was introduced broadened some of the disease groups to reflect more recent concepts about the pathology and aetiology of stroke; specifically, deaths previously coded as arteriosclerotic dementia were now coded as ischaemic stroke. Without additional evidence on the incidence of the arteriosclerotic dementia case deaths before and after 2002, it is difficult to speculate on the impact of this coding change on stroke mortality data. However, the ICD coding change is an historical event and therefore would only have a period effect on stroke mortality rates, and it could not affect age or cohort effects. Finally, there may have been differences between rural and urban areas in the coding of the disease in terms of completeness and accuracy. This discrepancy may have led to biases of the data but in the absence of additional information it is difficult to speculate on how these differences may have affected the overall results. Further research is required to substantiate these current findings.
In summary, the APC model was used to analyse stroke mortality trends in China between 1988 and 2013 and found a difference between urban and rural residents. These results will contribute to the limited information on stroke mortality prediction and analysis, which is important for assessing emerging risk factors for stroke and re-strategizing stroke intervention programmes, health services and health insurance policies in China.
Declaration of conflicting interests
The authors declare that there are no conflicts of interest.
Funding
The study was supported by the National Natural Science Fund of China (grant no. 71303012).
References
- 1.Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol 2009; 8: 345–354. [DOI] [PubMed] [Google Scholar]
- 2.Wang Z, Li J, Wang C, et al. Gender differences in 1-year clinical characteristics and outcomes after stroke: results from the China national stroke registry. PLoS One 2013; 8: e56459–e56459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim AS, Johnston SC. Global variation in the relative burden of stroke and ischemic heart disease. Circulation 2011; 124: 314–323. [DOI] [PubMed] [Google Scholar]
- 4.Zhao S, Mao J, Hu J. Mortality and the major causes of deaths in selected urban and rural populations in China. Chinese Journal of Health Statistics 1999, pp. 21–26. [Google Scholar]
- 5.Avendaño M, Kunst AE, van Lenthe F, et al. Trends in socioeconomic disparities in stroke mortality in six European countries between 1981–1985 and 1991–1995. Am J Epidemiol 2005; 161: 52–61. [DOI] [PubMed] [Google Scholar]
- 6.Maheswaran R, Elliott P, Strachan DP. Socioeconomic deprivation, ethnicity, and stroke mortality in greater London and south East England. J Epidemiol Community Health 1997; 51: 127–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang XH, Guan T, Mao J, et al. Disparity and its time trends in stroke mortality between urban and rural populations in China 1987 to 2001: changing patterns and their implications for public health policy. Stroke 2007; 38: 3139–3144. [DOI] [PubMed] [Google Scholar]
- 8.Cui C, Gu X, Wang H, et al. Epidemiology of cerebrovascular disease mortality in China, 2006–2010. Disease Surveillance 2013; 28: 1007–1011 [Article in Chinese].
- 9.Yang Y. Age/period/cohort distinctions. In: Markides KS. (ed). Encyclopedia of health and aging, Los Angeles, CA: Sage Publications, 2007, pp. 20–22. [Google Scholar]
- 10.Wray M, Colen C, Pescosolido B. The sociology of suicide. Annu Rev Sociol 2011; 37: 505–528. available at: http://www.annualreviews.org/doi/abs/10.1146/annurev-soc-081309-150058). [Google Scholar]
- 11.Phillips JA. A changing epidemiology of suicide? The influence of birth cohorts on suicide rates in the United States. Soc Sci Med 2014; 114: 151–160. [DOI] [PubMed] [Google Scholar]
- 12.Yang Y, Schulhofer-Wohl S, Fu WJ, et al. The intrinsic estimator for age-period-cohort analysis: what it is and how to use it. Am J Sociol 2008; 113: 1697–1736. [Google Scholar]
- 13.Khellaf M, Quantin C, d’Athis P, et al. Age-period-cohort analysis of stroke incidence in Dijon from 1985 to 2005. Stroke 2010; 41: 2762–2767. [DOI] [PubMed] [Google Scholar]
- 14.Sutton CJ, Marsden J, Watkins CL, et al. Changing stroke mortality trends in middle-aged people: an age-period-cohort analysis of routine mortality data in persons aged 40 to 69 in England. J Epidemiol Community Health 2010; 64: 523–529. [DOI] [PubMed] [Google Scholar]
- 15.Yang Y, Land KC. Age-period-cohort analysis: New models, methods, and empirical applications, Interdisciplinary Statisitics Series. Boca Raton: CRC Press Inc, 2013. [Google Scholar]
- 16.Mason KO, Winsboro HH. Some methodological issues in cohort analysis of archival data. Am Sociol Rev 1973; 38: 242–258. [Google Scholar]
- 17.NHFPC. Chinese health statistics year-books 2014. 2014.
- 18.Willekens R and Scherbov S. Age-period-cohort (APC) analysis of mortality with applications to soviet data; 1991 (available at: http://pure.iiasa.ac.at/3523/1/WP-91-042.pdf).
- 19.Peng X. China’s demographic history and future challenges. Science 2011; 333: 581–587. [DOI] [PubMed] [Google Scholar]
- 20.The People’s Republic of China. State Council. Medical and Health Services in China. December 2012, Beijing. (available at: http://english.gov.cn/archive/white_paper/2014/08/23/content_281474982986476.htm; accessed 19 October 2016).
- 21.Patra J, Taylor B, Irving H, et al. Alcohol consumption and the risk of morbidity and mortality for different stroke types–a systematic review and meta-analysis. BMC Public Health 2010; 10: 258–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kan H, Chen R, Tong S. Ambient air pollution, climate change, and population health in China. Environ Int 2012; 42: 10–19. [DOI] [PubMed] [Google Scholar]
- 23.Chen R, Zhang Y, Yang C, et al. Acute effect of ambient air pollution on stroke mortality in the China air pollution and health effects study. Stroke 2013; 44: 954–960. [DOI] [PubMed] [Google Scholar]
- 24.Hong YC, Lee JT, Kim H, et al. Air pollution: a new risk factor in ischemic stroke mortality. Stroke 2002; 33: 2165–2169. [DOI] [PubMed] [Google Scholar]
- 25.Villeneuve PJ, Chen L, Stieb D, et al. Associations between outdoor air pollution and emergency department visits for stroke in Edmonton, Canada. Eur J Epidemiol 2006; 21: 689–700. [DOI] [PubMed] [Google Scholar]
- 26.Meng Q, Zhang J, Yan F, et al. One country, two worlds - the health disparity in China. Glob Public Health 2012; 7: 124–136. [DOI] [PubMed] [Google Scholar]
- 27.Hu S, Liu X, Peng Y. Assessment of antibiotic prescription in hospitalised patients at a Chinese university hospital. J Infect 2003; 46: 161–163. [DOI] [PubMed] [Google Scholar]
- 28.Li JS, Zhang XG, Wang HQ, et al. The meaningful use of EMR in Chinese hospitals: a case study on curbing antibiotic abuse. J Med Syst 2013; 37: 9937–9937. [DOI] [PubMed] [Google Scholar]
- 29.You X, Kobayashi Y. The new cooperative medical scheme in China. Health Policy 2009; 91: 1–9. [DOI] [PubMed] [Google Scholar]
- 30.Phelan JC, Link BG, Diez-Roux A, et al. Fundamental causes of social inequalities in mortality: a test of the theory. J Health Soc Behav 2004; 45: 265–285. [DOI] [PubMed] [Google Scholar]
- 31.Tang S, Meng Q, Chen L, et al. Tackling the challenges to health equity in China. Lancet 2008; 372: 1493–1501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang LY. China’s urban, rural income gap widens despite economic recovery. Xinhua online news. 2010; Economy edition. (available at: http://news.xinhuanet.com/english2010/china/2010-01/21/c_13145748.htm; accessed 19 October 2016).
- 33.Meng Q, Xu K. Progress and challenges of the rural cooperative medical scheme in China. Bull World Health Organ 2014; 92: 447–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sun S, Chen J, Johannesson M, et al. Regional differences in health status in China: Population health-related quality of life results from the National Health Services Survey 2008. Health Place 2011; 17: 671–680. [DOI] [PubMed] [Google Scholar]
- 35.Shi L. Health care in China: a rural-urban comparison after the socioeconomic reforms. Bull World Health Organ 1993; 71: 723–736. [PMC free article] [PubMed] [Google Scholar]