Abstract
Objective
To investigate the incidence of postoperative sore throat (POST) in Korean patients undergoing general anaesthesia with endotracheal intubation and to assess potential risk factors.
Methods
This prospective study enrolled patients who underwent all types of elective surgical procedures with endotracheal intubation and general anaesthesia. The patients were categorized into group S (those with a POST) or group N (those without a POST). The demographic, clinical and anaesthetic characteristics of each group were compared.
Results
This study enrolled 207 patients and the overall incidence of POST was 57.5% (n = 119). Univariate analysis revealed that significantly more patients in group S had a cough at emergence and hoarseness in the postanaesthetic care unit compared with group N. Receiver operating characteristic curve analysis showed that an intracuff pressure ≥17 cmH2O was associated with POST. Multivariate analysis identified an intracuff pressure ≥17 cmH2O and cough at emergence as risk factors for POST. At emergence, as the intracuff pressure over ≥17 cmH2O increased, the incidence of hoarseness increased.
Conclusions
An intracuff pressure ≥17 cmH2O and a cough at emergence were risk factors for POST in Korean patients. Intracuff monitoring during anaesthesia and a smooth emergence are needed to prevent POST.
Keywords: Cough, intubation, intracuff pressure, sore throat
Introduction
Despite rapid advancement in anaesthetic techniques, sore throat following endotracheal intubation still is a long-standing concern for anaesthesiologists. In a recent report, postoperative sore throat (POST) was ranked as the second most common minor adverse event during anaesthesia recovery.1 The overall incidence of POST after general anaesthesia varies from 20% to 74%.1,2 The aetiology is multifactorial, including patient-related factors such as age,3 sex,4–6 smoking;7 and intubation factors including technique,8 duration,3 tube size,4 intracuff pressure,9,10 cuff design,3 intraoperative tube movement,4 and suctioning.8 Postoperative pain, including sore throat, increases analgesic use.11 The aims of this study were to assess the incidence and possible risk factors of POST in Korean patients undergoing elective surgery with endotracheal intubation.
Patients and methods
Patient population
This prospective study enrolled consecutive patients who underwent elective surgery requiring endotracheal intubation under general anaesthesia in the Department of Anaesthesiology and Pain Medicine, Seoul St Mary’s Hospital, The Catholic University of Korea, Seoul, Korea between April 2011 and December 2011. Inclusion criteria included: (i) patients aged 18–80 years; (ii) American Society of Anesthesiologists (ASA) physical status I or II.12 Exclusion criteria included: (i) emergency surgery, airway-related surgery, laparoscopic surgery; (ii) any history of difficult intubation; (iii) loose teeth; (iv) current upper respiratory tract infections, pre-existing sore throat and/or hoarseness, difficult intubation requiring more than two attempts; (v) nasogastric tube insertion; (vi) operation time longer than 2 h.
The following baseline demographic and clinical characteristics were recorded for all patients: age, sex, body mass index, ASA physical status, Charlson comorbidity index, presence of diabetes mellitus, and smoking status.
The study was approved by the Institutional Review Board of Seoul St Mary’s Hospital, The Catholic University of Korea, Seoul, Korea (Ref: KC11OISI0303) and registered with the Clinical Research Information Service (http://cris.cdc.go.kr; Ref: KCT0000405). All patients provided written informed consent prior to study enrolment.
Anaesthesia
Anaesthetic management was standardized. No patients were premedicated. Standard monitoring (IntelliVue MP70 patient monitor; Philips Healthcare, Best, the Netherlands), including electrocardiogram, end-tidal carbon dioxide, pulse oximeter, and non-invasive arterial blood pressure, was performed. Anaesthesia was induced with 2 mg/kg propofol intravenous (i.v.) and 1 µg/kg per min remifentanil i.v.; and muscle paralysis was obtained with 0.6 mg/kg rocuronium i.v. Endotracheal intubation was performed with a Macintosh laryngoscope by an experienced anaesthesiologist (J.Y.L. and H.J.P.) after approximately 5 min of mask ventilation and loss of all four twitches by train-of-four stimulation of the ulnar nerve. The laryngoscopic view was assessed according to the Cormack-Lehane grade.13 Endotracheal tubes of 7.0 mm internal diameter for women and 8.0 mm internal diameter for men were used (Lo-Contour® Murphy; Mallinckrodt Medical, Athlone, Ireland). The cuff was inflated manually with air to a clinical endpoint of loss of an audible leak. Next, the intracuff pressure was measured using a hand-held manometer (Posey Cufflator™ Endotracheal Tube Inflator and Manometer; Posey Company, Arcadia, CA, USA). None of the patients received topical lidocaine or lidocaine jelly during the intubation procedure. The lungs were ventilated with 50% oxygen with air. This was adjusted to maintain an end-tidal carbon dioxide of 32–42 mmHg. Anaesthesia was maintained with 1.5–3.0 vol% sevoflurane and with a continuous infusion of 0.05–0.1 µg/kg per min remifentanil. At the end of surgery, patients were administered 0.03 mg/kg pyridostigmine i.v. and 0.002 mg/kg glycopyrrolate i.v. The intracuff pressure was measured, then the cuff was completely deflated, and the endotracheal tube was suctioned and extubation was performed. Two anaesthesiologists (J.Y.L. and H.J.P.) conducted all anaesthesia procedures to ensure consistency.
Study outcomes
The primary outcomes of this study were to evaluate the incidence and possible risk factors of POST. The secondary outcome was to identify other laryngeal complaints, such as cough and hoarseness. These symptoms were scored by an independent nurse and/or patient. It was recorded either ‘yes’ or ‘no’ during the 10 min after arrival to the postanaesthetic care unit (PACU). Sore throat was defined as pain at the larynx or pharynx. It was asked with a direct questionnaire survey, ‘Do you have a sore throat after operation?’. Cough was defined as a sudden, strong abdominal contraction. It was checked twice, at emergence and at the PACU. Even a single cough was recorded as ‘yes’. Hoarseness was defined as a harsh or stained voice assessed by patients. If a nurse observed the patient’s voice change, it was also scored as ‘yes’. After the survey, patients with a postoperative pain score over 6 on a visual analogue scale (VAS; 0 = no pain, 10 = the worst pain imaginable) received 0.5 µg/kg fentanyl i.v. and/or a patient-controlled analgesia (PCA) as a rescue analgesic. The PCA regimen comprised of 15 µg/ml fentanyl i.v. in normal saline 100 ml.
The following surgery-related characteristics were recorded for all patients: surgery type, patient’s position during surgery, duration of anaesthesia, intubation trial number, Cormack-Lehane grade, total rocuronium dose, total remifentanil dose, cuff pressures at intubation and emergence, cough at emergence, and hoarseness at PACU.13
Statistical analyses
All statistical analyses were performed using the SAS® statistical package, version 9.4 (SAS Institute, Cary, NC, USA). Data are expressed as the mean ± SD or as frequencies and proportions, as appropriate. The intergroup differences were assessed using Fisher’s exact test and the Mann–Whitney U-test. Possible risk factors for POST were examined by univariate and multivariate analyses. A receiver operating characteristic (ROC) curve was constructed to investigate the cut-off intracuff pressure to correctly predict POST at the maximum area under the curve (AUC), which ranges from 0.5 to 1.0. Spearman’s correlation coefficient was calculated for intracuff pressure ≥ 17 cmH20 at intubation and emergence with cough and hoarseness. A P-value < 0.05 was considered statistically significant.
Results
A total of 221 patients were enrolled in this study, of whom 14 were excluded due to exclusion criteria or other data loss, but there were no cases of incomplete data collection due to drowsiness from anaesthesia. Thus, 207 patients were included in the final analysis. The patients ranged in age from 18 to 80 years old and they were all ASA physical status I or II. There were no cases of failed intubation, intraoperative tube migration, gastric fluid aspiration and/or pneumonia. The baseline demographic and clinical characteristics and anaesthetic data are summarized in Table 1.
Table 1.
Baseline demographic and clinical characteristics and potential predictive factors for postoperative sore throat in patients undergoing elective surgery requiring endotracheal intubation under general anaesthesia (n = 207).
| Characteristic | All patients n = 207 | Group S n = 119 | Group N n = 88 | Univariate statistical significance | Multivariate analysis |
||
|---|---|---|---|---|---|---|---|
| 95% CI | P-value | OR | |||||
| Age, years | 46.2 ± 14.5 | 44.2 ± 14.4 | 48.9 ± 14.2 | NS | – | – | – |
| Sex, male/female | 67/140 | 43/76 | 24/64 | NS | – | – | – |
| Body mass index, kg/m2 | 23.6 ± 3.0 | 23.5 ± 3.0 | 23.8 ± 3.0 | NS | – | – | – |
| ASA physical status, I/II | 133/74 | 77/42 | 56/32 | NS | – | – | – |
| Charlson comorbidity index | 0.4 ± 0.6 | 0.4 ± 0.6 | 0.4 ± 0.7 | NS | – | – | – |
| Presence of diabetes mellitus | 16 (7.7%) | 10 (8.4%) | 6 (6.8%) | NS | – | – | – |
| Smoking | 23 (11.1%) | 12 (10.1%) | 11 (12.5%) | NS | – | – | – |
| Surgery type | |||||||
| Ophthalmic | 51 | 33 | 18 | NS | – | – | – |
| Gynaecological | 49 | 22 | 27 | ||||
| Orthopaedic | 38 | 18 | 20 | ||||
| Visceral | 49 | 34 | 15 | ||||
| Urological | 15 | 9 | 6 | ||||
| Plastic | 5 | 3 | 2 | ||||
| Patient’s surgical position | |||||||
| Supine | 123 | 78 | 45 | NS | – | – | – |
| Lithotomy | 58 | 29 | 29 | NS | |||
| Lateral | 26 | 12 | 14 | NS | |||
| Anaesthesia time, min | 104.8 ± 58.4 | 106.9 ± 61.2 | 102.0 ± 54.7 | NS | – | – | – |
| Intubation trial number, 1/2 | 201/6 | 114/5 | 87/1 | NS | – | – | – |
| Cormack-Lehane grade, 1/2/3/4 | 128/77/2/0 | 75/43/1/0 | 53/34/1/0 | NS | – | – | – |
| Total rocuronium dose, mg | 43.1 ± 9.0 | 48.4 ± 8.7 | 50.7 ± 10.3 | NS | – | – | – |
| Total remifentanil dose, µg/kg per min | 0.06 ± 0.01 | 0.07 ± 0.02 | 0.05 ± 0.03 | NS | – | – | – |
| Cuff pressure, cmH2O | |||||||
| At intubation | 19.9 ± 6.8 | 20.6 ± 4.7 | 19.9 ± 5.3 | NS | – | – | – |
| At emergence | 20.3 ± 5.0 | 20.7 ± 6.4 | 18.9 ± 7.3 | NS | |||
| Cuff pressure ≥ 17 cmH2O | |||||||
| At intubation | 163 (78.7%) | 100 (84.0%)* | 63 (71.6%) | P = 0.032 | – | – | – |
| At emergence | 138 (66.7%) | 88 (73.9%)* | 50 (56.8%) | P = 0.010 | 1.06, 3.80 | P = 0.031 | 2.01 |
| Cough at emergence | 113 (54.6%) | 79 (66.4%)* | 34 (38.6%) | P < 0.001 | 1.33, 4.53 | P = 0.004 | 2.45 |
| Hoarseness at PACU | 80 (38.6%) | 60 (50.4%)* | 20 (22.7%) | P < 0.001 | 1.44, 5.32 | P = 0.002 | 2.76 |
All data are presented as the mean ± SD or n (%) of patients.
P < 0.05 compared with group N.
Group S, patients with a postoperative sore throat; Group N, patients without a postoperative sore throat; CI, confidential interval; OR, odds ratio; ASA, American Society of Anesthesiologists; PACU, postanaesthetic care unit; NS, not statistically significant (P ≥ 0.05).
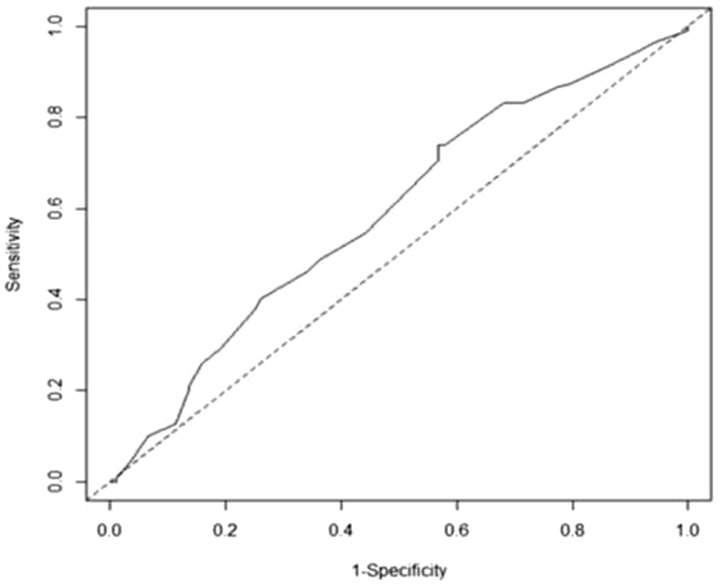
Of the 207 patients, 119 (57.5%) developed a POST. Group S was defined as those who had a POST (n = 119) and group N as those without a POST (n = 88) (Table 1). In the univariate analysis, age, sex, body mass index, ASA physical status, Charlson comorbidity index, presence of diabetes mellitus, smoking, surgery type, patient’s surgical position, anaesthesia time, intubation trial number, Cormack-Lehane grade, total rocuronium dose, total remifentanil dose, and mean intracuff pressure did not differ significantly between the two groups. An intracuff pressure ≥17 cmH2O during intubation (P = 0.032) and at emergence (P = 0.010) was significantly more frequent in group S compared with group N. The ROC curves of intracuff pressure during intubation and emergence are shown in Figure 1. An intracuff pressure ≥17 cmH2O at emergence was associated with POST (AUC, 0.586). Factors with a P-value < 0.1 according to the univariate analysis were entered into the multivariate model. Having an intracuff pressure ≥17 cmH2O at emergence (odds ratio [OR], 2.01; 95% confidence interval [CI], 1.06, 3.80; P = 0.031) was significantly associated with POST (Table 1).
Figure 1.
Receiver operating characteristic curve of intracuff pressure for predicting postoperative sore throat in patients in group S (n = 199). The optimal cut-off point was ≥17 cmH2O at emergence with an area under the curve of 0.586.
In the univariate analysis, a cough at emergence was also more frequently observed in group S compared with group N (P < 0.001). More patients in group S had hoarseness at PACU compared with group N (P < 0.001) (Table 1). In the multivariate analysis, cough at emergence (OR, 2.45; 95% CI, 1.33, 4.53; P = 0.004) was significantly associated with POST; and hoarseness at PACU was significantly associated with POST (OR, 2.76; 95% CI, 1.44, 5.32; P = 0.002). At emergence, a high intracuff pressure from ≥17 cmH2O increased the incidence of hoarseness (r = 0.174; P = 0.021) (Table 2).
Table 2.
Spearman’s correlation coefficient analysis of the associations between cough and hoarseness with having an intubation or emergence intracuff pressure ≥ 17 cmH2O.
| Intracuff pressure ≥17 cmH2O | Cough | Hoarseness |
|---|---|---|
| At intubation | r = −0.020 | r = −0.012 |
| At emergence | r = 0.075 | r = 0.174* |
P = 0.021, which was considered statistically significant.
Discussion
Sore throat, cough, and hoarseness are common complaints after tracheal intubation.1–11,14–16 In this present study, the incidence of POST was 57.5%. An intracuff pressure ≥17 cmH2O at emergence was a risk factor for POST in the present study. Intracuff pressure depends on both tracheal and cuff compliance.17 Although evidence from in vivo studies is not insufficient, human capillary perfusion pressure ranges from 30 to 44 cmH2O and mucosal blood flow impairment at the tracheal cartilage occurs at ≥30 cmH2O.10 In an animal study, tracheal lateral wall damage occurred within 15 minutes at 27 cmH2O pressure.16 Mechanical compression from a high intracuff pressure leads to tracheal mucosal hypoperfusion, ischaemia, ulceration, and pain.17,18 This present study showed a lower intracuff pressure threshold than previously reported (20–30 cmH2O).17–19 This is probably due to different compliances and receptor sensitivity of airways in Korean patients. Additionally, preoperative psychological status and anxiety level may contribute to pain perception in patients.20
The incidence of cough at emergence ranges from 40% to 96%.21 In the present study, the incidence of cough was 66.4% in group S and 38.6% in group N. Cough is essentially a reflex for airway protection. It can be evoked by mechanical and/or chemical stimuli, which activate sensory receptors distributed along the respiratory tract.22 At light anaesthesia or during emergence, endotracheal tube movement may irritate the trachea and laryngeal mucosa, leading to cough. An appropriate cough can remove respiratory secretions and decrease the risk of aspiration, but it also activates the sympathetic nervous system, leading to tachycardia, hypertension, intraocular hypertension, intracranial hypertension, and surgical site bleeding.23 Cough at emergence was a risk factor for POST in the present study. These findings suggest that at the time of extubation, patients who are almost awake may have more head and neck movement, leading to an irritated airway and intracuff pressure change associated with increased postoperative laryngotracheal morbidity. In addition, hoarseness is known to relate to increased cuff pressure.9,24 Hoarseness results from oedema of the vocal cords following endotracheal intubation, mechanical contact, and abrasion by the tube in the glottis area.24 This present study showed that the incidence of hoarseness in group S was higher compared with group N, and it significantly increased with an intracuff pressure ≥17 cmH2O at emergence.
Numerous modalities for preventing or minimizing POST have been performed with uncertain efficacy.11,19,25–27 During anaesthesia, intracuff pressure can be influenced by anaesthetic depth, degree of muscle relaxation, patient temperature and position, ventilation mode, and additional drug administration.28,29 Although there is no standard for the frequency of monitoring cuff pressure during anaesthesia, routine cuff pressure measurements are important in reducing POST.30
This study had several limitations. First, intracuff pressure was not monitored continuously during anaesthesia, but only twice, after intubation and at emergence. Intermittent monitoring may give a false interpretation that the pressure is within a therapeutic range. Secondly, POST and other laryngeal symptoms were evaluated using binary scale (yes or no),27,31 because incomplete data collection was experienced during our pilot study, when a four-point scale was used.15,32 Thirdly, various types of surgical procedures were included, which may have influenced airway reactivity. Fourthly, the present study only followed patients through the PACU recovery period without a longer follow-up because enrolled patients were composed of both inpatients and outpatients. There is no established guideline for POST evaluation time, but several publications have described that POST is measured from 15 minutes to 24 hours postextubation, because POST is worse in the early postoperative period up to 6 hours, then decreases over time.5,24,27 Despite these limitations, this present study attempted to quantify the proper airway pressure limit in Korean patients. The current findings also warrant future well-controlled, prospective randomized trials for reducing POST. Also, these current findings suggest that intracuff pressure should be adjusted based on each patient’s characteristics.
In conclusion, POST in Korean patients was significantly associated with a lower intracuff pressure threshold compared with previous reports. These current findings suggest that intracuff monitoring during anaesthesia and a smooth emergence are necessary to prevent POST.
Contribution of authors
Jin Young Lee: study design, data collection and analysis, writing and revising the manuscript; Woo Seog Sim, Eun Sung Kim, Sangmin M Lee: providing criticism of the manuscript; Hue Jung Park: study design, data collection and analysis, writing and revising the manuscript; Duk Kyung Kim, Yu Ri Na and Dahye Park: providing criticism of the manuscript.
Declaration of conflicting interests
The authors declare that there are no conflicts of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
References
- 1.Lehmann M, Monte K, Barach P, et al. Postoperative patient complaints: a prospective interview study of 12,276 patients. J Clin Anesth 2010; 22: 13–21. [DOI] [PubMed] [Google Scholar]
- 2.Arts MP, Rettig TC, de Vries J, et al. Maintaining endotracheal tube cuff pressure at 20 mm Hg to prevent dysphagia after anterior cervical spine surgery; protocol of a double-blind randomised controlled trial. BMC Musculoskelet Disord 2013; 14: 280–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El-Boghdadly K, Bailey CR, Wiles MD. Postoperative sore throat: a systematic review. Anaesthesia 2016; 71: 706–717. [DOI] [PubMed] [Google Scholar]
- 4.Hu B, Bao R, Wang X, et al. The size of endotracheal tube and sore throat after surgery: a systematic review and meta-analysis. PLoS One 2013; 8: e74467–e74467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Orandi A, Orandi A, Najafi A, et al. Post-intubation sore throat and menstruation cycles. Anesth Pain Med 2013; 3: 243–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christensen AM, Willemoes-Larsen H, Lundby L, et al. Postoperative throat complaints after tracheal intubation. Br J Anaesth 1994; 73: 786–787. [DOI] [PubMed] [Google Scholar]
- 7.Biro P, Seifert B, Pasch T. Complaints of sore throat after tracheal intubation: a prospective evaluation. Eur J Anaesthesiol 2005; 22: 307–311. [DOI] [PubMed] [Google Scholar]
- 8.McHardy FE, Chung F. Postoperative sore throat: cause, prevention and treatment. Anaesthesia 1999; 54: 444–453. [DOI] [PubMed] [Google Scholar]
- 9.Combes X, Schauvliege F, Peyrouset O, et al. Intracuff pressure and tracheal morbidity: influence of filling with saline during nitrous oxide anesthesia. Anesthesiology 2001; 95: 1120–1124. [DOI] [PubMed] [Google Scholar]
- 10.Seegobin RD, van Hasselt GL. Endotracheal cuff pressure and tracheal mucosal blood flow: endoscopic study of effects of four large volume cuffs. Br Med J (Clin Res Ed) 1984; 288: 965–968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maruyama K, Yamada T, Hara K. Effect of clonidine premedication on postoperative sore throat and hoarseness after total intravenous anesthesia. J Anesth 2006; 20: 327–330. [DOI] [PubMed] [Google Scholar]
- 12.American Society of Anesthesiologists. ASA Physical Status Classification System, https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system (2014, accessed 12 September 2016).
- 13.Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia 1984; 39: 1105–1111. [PubMed] [Google Scholar]
- 14.Higgins PP, Chung F, Mezei G. Postoperative sore throat after ambulatory surgery. Br J Anaesth 2002; 88: 582–584. [DOI] [PubMed] [Google Scholar]
- 15.Mencke T, Echternach M, Kleinschmidt S, et al. Laryngeal morbidity and quality of tracheal intubation: a randomized controlled trial. Anesthesiology 2003; 98: 1049–1056. [DOI] [PubMed] [Google Scholar]
- 16.Nordin U. The trachea and cuff-induced tracheal injury. An experimental study on causative factors and prevention. Acta Otolaryngol Suppl 1977; 345: 1–71. [PubMed] [Google Scholar]
- 17.Sultan P, Carvalho B, Rose BO, et al. Endotracheal tube cuff pressure monitoring: a review of the evidence. J Perioper Pract 2011; 21: 379–386. [DOI] [PubMed] [Google Scholar]
- 18.Sole ML, Penoyer DA, Su X, et al. Assessment of endotracheal cuff pressure by continuous monitoring: a pilot study. Am J Crit Care 2009; 18: 133–143. [DOI] [PubMed] [Google Scholar]
- 19.Lee JH, Lee HK, Chun NH, et al. The prophylactic effects of gabapentin on postoperative sore throat after thyroid surgery. Korean J Anesthesiol 2013; 64: 138–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lanitis S, Mimigianni C, Raptis D, et al. The impact of educational status on the postoperative perception of pain. Korean J Pain 2015; 28: 265–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Minogue SC, Ralph J, Lampa MJ. Laryngotracheal topicalization with lidocaine before intubation decreases the incidence of coughing on emergence from general anesthesia. Anesth Analg 2004; 99: 1253–1257. [DOI] [PubMed] [Google Scholar]
- 22.Mazzone SB. An overview of the sensory receptors regulating cough. Cough 2005; 1: 2–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Irwin RS. Complications of cough: ACCP evidence-based clinical practice guidelines. Chest 2006; 129(Suppl 1): 54S–58S. [DOI] [PubMed] [Google Scholar]
- 24.Liu J, Zhang X, Gong W, et al. Correlations between controlled endotracheal tube cuff pressure and postprocedural complications: a multicenter study. Anesth Analg 2010; 111: 1133–1137. [DOI] [PubMed] [Google Scholar]
- 25.Akbay BK, Yildizbas S, Guclu E, et al. Analgesic efficacy of topical tramadol in the control of postoperative pain in children after tonsillectomy. J Anesth 2010; 24: 705–708. [DOI] [PubMed] [Google Scholar]
- 26.Lam F, Lin YC, Tsai HC, et al. Effect of intracuff lidocaine on postoperative sore throat and the emergence phenomenon: a systematic review and meta-analysis of randomized controlled trials. PLoS One 2015; 10: e0136184–e0136184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Estebe JP, Dollo G, Le Corre P, et al. Alkalinization of intracuff lidocaine improves endotracheal tube-induced emergence phenomena. Anesth Analg 2002; 94: 227–230. [DOI] [PubMed] [Google Scholar]
- 28.Felten ML, Schmautz E, Delaporte-Cerceau S, et al. Endotracheal tube cuff pressure is unpredictable in children. Anesth Analg 2003; 97: 1612–1616. [DOI] [PubMed] [Google Scholar]
- 29.Stevanovic A, Rossaint R, Fritz HG, et al. Airway reactions and emergence times in general laryngeal mask airway anaesthesia: a meta-analysis. Eur J Anaesthesiol 2015; 32: 106–116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kim D, Jeon B, Son JS, et al. The changes of endotracheal tube cuff pressure by the position changes from supine to prone and the flexion and extension of head. Korean J Anesthesiol 2015; 68: 27–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cirilla DJ, 2nd, Ngo J, Vaisman V, et al. Does the incidence of sore throat postoperatively increase with the use of a traditional intubation blade or the GlideScope? J Clin Anesth 2015; 27: 646–651. [DOI] [PubMed] [Google Scholar]
- 32.Stout DM, Bishop MJ, Dwersteg JF, et al. Correlation of endotracheal tube size with sore throat and hoarseness following general anesthesia. Anesthesiology 1987; 67: 419–421. [DOI] [PubMed] [Google Scholar]