Abstract
Objective
To explore the potential presence of a social/behavioural gradient in dental health among Italian adults using a cross-sectional study.
Methods
Caries indices were recorded among 480 subjects (52.9% men, 47.1% women) who also completed a structured self-administered social and behavioural questionnaire. A social/behavioural gradient was generated as the sum of the worst circumstances recorded on the questionnaire (cariogenic diet, smoking, lowest occupational profile, brushing teeth < twice daily, lowest educational level, uneven dental examination attendance).
Results
Caries figures (DMFT) and the number of filled sound teeth (FS-T) were statistically significantly linked to the social/behavioural gradient (DMFT: χ2(9) = 20.17 p = 0.02, Z = 0.02 p = 0.99; FS-T: χ2(9) = 25.68 p < 0.01, Z = −4.31 p < 0.01). DMFT was statistically significantly associated with gender and with social and behavioural variables. FS-T was higher in women (p = 0.03) and was linked to smoking (p < 0.01).
Conclusions
The proposed social/behavioural gradient demonstrated how subjects reporting the worst circumstances on the questionnaire exhibited the worst dental health. The use of the gradient demonstrates that health promotion and prevention cannot be compartmentalized.
Keywords: Caries, risk assessment, social economical, adults, behaviour
Introduction
Health is directly linked to individual lifestyle factors related to living and working conditions, as well as socioeconomic, cultural, and environmental factors. The causes of social inequality in health are considered to be multiple and inter-related. Several hypotheses have been formulated to describe social inequalities based on behavioural, environmental, psychological, and material patterns. Regardless of the level of income, in every country, health and illness are strongly related to a social gradient. The lower an individual’s socioeconomic position, the worse his/her health. This gradient in health runs from the top to the bottom of the socioeconomic range. In addition to the social gradient, health behaviours are also involved in the development of diseases, suggesting the existence of a social/behavioural gradient.1,2
Dental caries remains one of the most common chronic and multifactorial diseases worldwide, and this epidemiological evidence reflects a failure to understand the social determinants of the disease.3 Caries is the result of a series of events occurring in a chain that generally begins years before the detection of the lesion, and social status—determined by social class, educational level, occupational status, and income—is closely associated with the clinical features of the disease.4,5 Several health behaviours also enter into this casual chain, such as dietary, lifestyle, and oral hygiene habits.6,7
Socioeconomic inequalities across a broad spectrum of oral indicators reflecting unmet needs were described in a national sample of adults in the United States, and this topic was also addressed in later studies, where socioeconomic inequalities were found in different markers of oral health.4,8,9 Moreover, an inverse association has been reported between social inequalities and edentulousness in English adults.1
Despite these existing findings, the relationship between position on the social gradient and caries is not as strong among adults as it is among children, and few studies on this topic in adults are available.10,11 However, analyses of a population’s oral health habits are fundamental to providing “good behaviours” messages.12 In Italy, the few surveys on the oral health status of adults that exist have reported a high level of caries experience and correlations between oral health status and social status, lifestyle, and oral health behaviours.6,13,14
Expanding on the existing research, the objectives of this study, conducted with a sample of Italian adults, were to describe the developmental process for generating a social/behavioural gradient and to explore the potential presence of this gradient in dental health. To achieve these objectives, a cross-sectional study was designed and performed.
Materials and methods
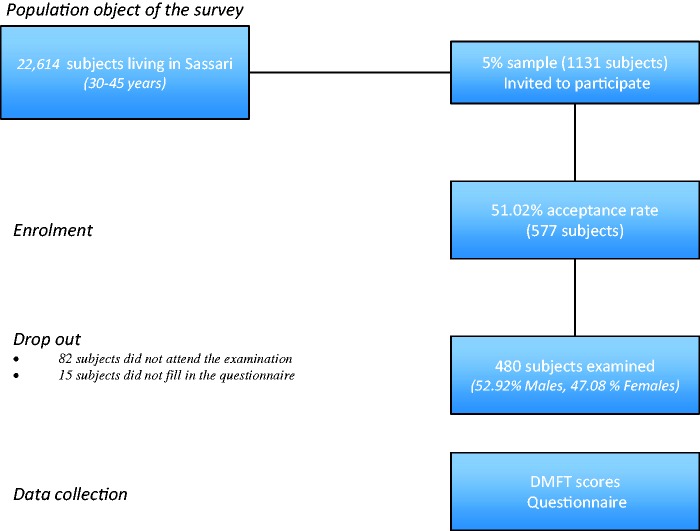
The present study was carried out in Sassari (Sardinia, Italy) under the supervision of the World Health Organization (WHO) Collaborating Centre for Epidemiology and Community Dentistry of Milan (Italy). From a population of 22,614 Sassari residents aged 30–45 years, a power analysis [G*Power 3.1.3 for Apple] (logistic regression with an odds ratio of 1.5 and an error probability of 0.04) estimated a final sample size of 432 people. With the collaboration of the municipal electoral register office, the electoral list was computed, and 1131 subjects (5% of the population) were randomly selected using Microsoft Excel® 2015 for Apple. A letter explaining the purpose of the study and requesting informed consent to participate was then distributed to the selected sample. A total of 577 subjects (51.0%) agreed to participate; 82 (14.2%) did not attend the examination appointment, and 15 (0.2%) did not complete the questionnaire. Overall, 480 subjects (52.9% men and 47.1% women, mean age = 40.7 ± 0.3) were included in the final analytical sample (Figure 1). The study design was registered (2013_01_21_a) at the Sassari local office of the National Bioethics Committee, and the results were reported following the STROBE guidelines for cross-sectional studies.15
Figure 1.
Flowchart of the study design.
Records registration
One examiner (G. Carta) was calibrated, examining and re-examining 55 adults before the survey. Inter-examiner reliability was evaluated using a fixed-effects analysis of variance in comparison with benchmark values (G. Campus). Intra-examiner reproducibility was assessed using Cohen’s kappa statistic.16 Good inter-examiner reliability was found for DMFT > 0 (caries experience), with no significant difference from benchmark values (p = 0.15) and a low mean squared error (0.47). Intra-examiner reliability was also high (Cohen’s kappa statistic = 0.88). The same examiner performed all of the dental examinations.
Subjects were examined at the Dental Institute of the University of Sassari after a professional oral hygiene session. During the examinations, subjects sat in a dental chair, and the examiner used a mouth mirror and a WHO Community Periodontal Index probe under optimal lighting. Subjects’ teeth were dried before evaluation.
Following WHO indications, the DMFT and FS-T indices were recorded.17 Dental caries was recorded starting from the D3 dentinal lesion level.18 The DMFT index was categorized into three classes using as reference the categorization of the DMFS created by Lesaffre and colleagues,19 and this was used as an ordinal score.
The FS-T index allows for the assessment of the number of filled and sound teeth and is a measure of functional status. Furthermore, it has an increased model performance and might be more effective than the DMFT index in describing social, demographic, and behavioural factors associated with caries experience in adults.20
Questionnaire
A structured self-administered questionnaire was completed by participants before the clinical examination. To guarantee anonymity, the questionnaire was printed on one side of a sheet of paper, and the clinical chart was on the other side. The questionnaire was pre-tested for reliability and validity.6 It was highly structured and divided into three domains: (1) personal data (age, gender, educational level, category of employment), (2) lifestyle behaviour (smoking and dietary habits), and (3) oral health behaviour (tooth brushing and frequency of dental check-ups). Educational level was classified as primary school, secondary school, or university. Employment was categorized using the Italian Institute for Statistics.21 Smoking status was coded following the WHO definition for tobacco users modified by the authors6, with participants defined as smokers only if they had started smoking more than 3 years earlier.
Statistical analyses
Data from the dental examination and questionnaire were entered in a FileMaker Pro 9.0 Runtime database and then exported to a Microsoft Excel® spreadsheet. All data were analysed using Stata® (Mac version 13). For all analyses, the statistical significance level was set at α = 0.05.
Descriptive statistics and cross-tabulations were calculated for questionnaire items and both caries experience—DMFT and the components of decayed teeth, missing teeth resulting from caries, and filled teeth because of caries—and functioning teeth (FS-T).
The variables derived from the questionnaire were dichotomized as follows: Educational level—primary/secondary school vs. university degree; occupational status— unemployed/housewife vs. technician/clerk/professional; dental attendance: pain/problem/every 2 years vs. once a year/every 6 months.
A social/behavioural gradient was generated as the sum of the worst circumstances recorded on the questionnaire regarding social conditions and oral health behaviours. Subjects were stratified into four social gradient levels based on their number of worst options: “best,” with up to two; “good,” with three; “bad,” with four; and “worst,” with five or more. The association between the different caries risk categories and DMFT/FS-T was calculated. The nonparametric test for trend across ordered groups as an extension of the Wilcoxon rank-sum test was also calculated.
Separate multinomial logistic regression models were estimated using the DMFT categorization scores and the FS-T categorization scores as dependent variables. The Akaike Information Criterion was used to measure the goodness of fit of the statistical model. The possible modifying effects of covariates on the outcomes were tested through an interaction model (likelihood-ratio test statistic). Multicollinearity can sometimes cause problems with regression results. This problem was solved using the DFBETA command in Stata, which excludes information that has too much influence on the regression line. After the data elaboration, no statistically significant multicollinearity was observed, so it was decided to report the findings without outliers.
Results
Consistent differences were found in DMFT and its components by position on the social gradient (gender, occupational status, educational level) and oral health behaviours (smoking status and frequency of dental examination attendance) (Table 1). The DMFT index was statistically significantly lower for men than for women (9.11 ± 5.12 and 11.09 ± 5.06, respectively, p < 0.01). There was a statistically significant difference in caries figures by occupational status, regardless of gender; the lowest occupational status categories showed the highest caries experience (p < 0.01). The mean number of missing teeth due to caries was statistically significantly associated with gender (p = 0.04), smoking (p < 0.01), and educational level (p < 0.01).
Table 1.
DMFT and its components by position on the social gradient (occupational status, educational level), oral health behaviours (smoking status, frequency of brushing teeth, frequency of dental examination attendance), and gender.
| DT (mean ± SD) | MT (mean ± SD) | FT (mean ± SD) | DMFT (mean ± SD) | |
|---|---|---|---|---|
| Total sample | 0.22 ± 0.61 | 1.61 ± 2.76 | 8.21 ± 4.60 | 10.04 ± 5.18 |
| Men | 0.22 ± 0.46 | 1.45 ± 2.57 | 7.44 ± 4.51 | 9.11 ± 5.12 |
| Women | 0.23 ± 0.75 | 1.79 ± 2.95 | 9.06 ± 4.57 | 11.09 ± 5.06 |
| One-way ANOVA | F = 0.03 p = 0.93 | F = 1.81 p = 0.18 | F = 15.53 p < 0.01 | F = 18.05 p < 0.01 |
| Occupational status | ||||
| Unemployed/housewife | 0.28 ± 0.78 | 2.46 ± 3.41 | 9.74 ± 3.98 | 12.47 ± 4.65 |
| Technician/clerk | 0.19 ± 0.45 | 1.40 ± 2.57 | 7.51 ± 4.59 | 9.10 ± 5.02 |
| Professional | 0.26 ± 0.66 | 0.92 ± 1.88 | 8.14 ± 4.67 | 9.32 ± 5.00 |
| One-way ANOVA | F = 0.97 p = 0.44 | F = 2.98 p < 0.01 | F = 1.47 p = 0.08 | F = 2.52 p < 0.01 |
| Unemployed/housewife | 0.28 ± 0.78 | 2.46 ± 3.41 | 9.73 ± 3.99 | 12.47 ± 4.65 |
| Men | 0.29 ± 0.94 | 1.86 ± 2.48 | 8.70 ± 3.41 | 12.67 ± 4.64 |
| Women | 0.24 ± 1.02 | 3.05 ± 3.44 | 10.51 ± 4.23 | 13.44 ± 4.93 |
| One-way ANOVA | F = 0.02 p = 0.89 | F = 3.21 p = 0.08 | F = 15.53 p < 0.01 | F = 1.13 p = 0.35 |
| Professional | 0.26 ± 0.66 | 0.91 ± 1.89 | 8.14 ± 4.67 | 9.32 ± 5.00 |
| Men | 0.22 ± 0.46 | 0.38 ± 1.09 | 7.34 ± 4.46 | 7.94 ± 4.78 |
| Women | 0.31 ± 0.82 | 1.51 ± 2.37 | 9.02 ± 4.79 | 10.84 ± 4.85 |
| One-way ANOVA | F = 0.45 p = 0.50 | F = 9.24 p < 0.01 | F = 3.14 p = 0.08 | F = 1.77 p = 0.04 |
| Educational level | ||||
| Primary school | 0.26 ± 0.74 | 2.70 ± 4.00 | 7.60 ± 4.98 | 10.55 ± 6.13 |
| Secondary school | 0.20 ± 0.48 | 1.65 ± 2.65 | 8.22 ± 4.61 | 10.07 ± 5.03 |
| University degree | 0.24 ± 0.70 | 0.98 ± 1.78 | 8.51 ± 4.39 | 9.74 ± 4.85 |
| One-way ANOVA | F = 0.84 p = 0.54 | F = 2.38 p < 0.01 | F = 1.68 p = 0.03 | F = 1.30 p = 0.15 |
| Primary school | ||||
| Men | 0.25 ± 0.52 | 1.89 ± 2.65 | 6.75 ± 4.99 | 8.89 ± 5.86 |
| Women | 0.26 ± 1.00 | 3.94 ± 5.27 | 8.88 ± 4.764 | 13.09 ± 5.72 |
| One-way ANOVA | F = 2.19 p = 0.08 | F = 1.01 p = 0.45 | F = 2.61 p < 0.01 | F = 1.59 p = 0.08 |
| Secondary school | ||||
| Men | 0.25 ± 0.47 | 1.77 ± 3.03 | 7.27 ± 4.51 | 9.29 ± 5.12 |
| Women | 0.15 ± 0.49 | 1.53 ± 2.20 | 9.18 ± 4.52 | 10.86 ± 4.83 |
| One-way ANOVA | F = 2.33 p = 0.07 | F = 1.39 p = 0.17 | F = 1.54 p = 0.07 | F = 1.61 p = 0.04 |
| Smoking status | ||||
| Nonsmoker | 0.18 ± 0.48 | 1.20 ± 1.98 | 8.18 ± 4.66 | 9.56 ± 4.97 |
| Smoker | 0.33 ± 0.88 | 2.72 ± 4.00 | 8.30 ± 4.46 | 11.36 ± 5.53 |
| One-way ANOVA | F = 2.87 p < 0.01 | F = 3.88 p < 0.01 | F = 1.25 p = 0.20 | F = 2.33 p < 0.01 |
| Nonsmoker | ||||
| Men | 0.19 ± 0.42 | 1.02 ± 1.80 | 7.34 ± 4.56 | 8.56 ± 4.76 |
| Women | 0.30 ± 0.55 | 2.59 ± 3.73 | 7.69 ± 4.38 | 10.59 ± 5.75 |
| One-way ANOVA | F = 1.75 p = 0.16 | F = 1.11 p = 0.35 | F = 2.12 p < 0.01 | F = 1.86 p = 0.01 |
| Smoker | ||||
| Men | 0.30 ± 0.55 | 2.59 ± 3.73 | 7.69 ± 4.38 | 10.59 ± 5.75 |
| Women | 0.17 ± 0.54 | 1.40 ± 2.16 | 9.10 ± 4.61 | 10.68 ± 4.98 |
| One-way ANOVA | F = 2.59 p = 0.01 | F = 1.05 p = 0.41 | F = 0.83 p = 0.65 | F = 1.35 p = 0.15 |
| Dental attendance | ||||
| Every 6 months | 0.09 ± 0.29 | 0.95 ± 2.90 | 8.98 ± 4.68 | 10.02 ± 5.01 |
| Once a year | 0.11 ± 0.37 | 1.31 ± 1.85 | 8.21 ± 4.16 | 9.63 ± 4.56 |
| Every 2 years | 0.33 ± 0.67 | 1.56 ± 2.79 | 8.83 ± 4.85 | 10.73 ± 5.47 |
| Pain/problem | 0.31 ± 0.83 | 2.27 ± 3.38 | 7.34 ± 4.75 | 9.92 ± 5.64 |
| One-way ANOVA | F = 2.37 p = 0.03 | F = 1.95 p = 0.02 | F = 2.80 p = 0.01 | F = 1.41 p = 0.09 |
| Once a year | ||||
| Men | 0.12 ± 0.33 | 1.08 ± 1.78 | 7.49 ± 4.18 | 8.67 ± 4.52 |
| Women | 0.09 ± 0.41 | 1.59 ± 1.91 | 9.11 ± 3.97 | 10.79 ± 4.37 |
| One-way ANOVA | F = 1.68 p = 0.19 | F = 1.49 p = 0.17 | F = 1.08 p = 0.37 | F = 1.65 p = 0.04 |
| Every 2 years | ||||
| Men | 0.37 ± 0.54 | 1.61 ± 2.71 | 7.80 ± 4.69 | 9.76 ± 5.40 |
| Women | 0.28 ± 0.81 | 1.50 ± 2.92 | 10.17 ± 4.78 | 11.94 ± 5.38 |
| One-way ANOVA | F = 3.46 p = 0.02 | F = 1.09 p = 0.38 | F = 2.01 p = 0.01 | F = 1.69 p = 0.04 |
| Brushing frequency | ||||
| More than once a day | 0.21 ± 0.64 | 1.25 ± 2.27 | 7.89 ± 4.30 | 9.35 ± 4.80 |
| Once a day | 0.24 ± 0.57 | 2.17 ± 3.29 | 8.69 ± 5.01 | 11.11 ± 5.66 |
| One-way ANOVA | F = 1.48 p = 0.18 | F = 1.80 p = 0.04 | F = 1.42 p = 0.10 | F = 2.49 p < 0.01 |
Note: Only variables with at least one statistically significant difference in DMFT and/or its components are reported.
A significant association between dental health (FS-T index) and educational level was found (Table 2). Subjects with the highest educational levels presented the best oral health status. Smoking was a threat to oral health: Smokers showed the lowest percentages of sound and filled teeth (5.62% with 3–23 FS-T, 5.21% with 24–25 FS-T, 7.92% with 26–27 FS-T, and 7.92% with 28 FS-T).
Table 2.
Sample distribution of filled and sound teeth (FS-T) by social gradient and oral health behaviours.
| 3–23 FS-T n (%) | 24–25 FS-T n (%) | 26–27 FS-T n (%) | 28 FS-T n (%) | |
|---|---|---|---|---|
| Educational level | ||||
| Primary school | 18 (3.75) | 21 (4.37) | 20 (4.17) | 27 (5.62) |
| Secondary school | 29 (6.04) | 32 (6.67) | 77 (16.04) | 89 (18.54) |
| University degree | 16 (3.34) | 19 (3.95) | 40 (8.34) | 92 (19.17) |
| χ2(6) = 25.70, p < 0.01 | ||||
| Smoking status | ||||
| Nonsmoker | 36 (7.50) | 47 (9.80) | 99 (20.62) | 170 (35.41) |
| Smoker | 27 (5.62) | 25 (5.21) | 38 (7.92) | 38 (7.92) |
| Χ2(3) = 18.41, p < 0.01 | ||||
| Frequency of tooth brushing | ||||
| Less than 2 times/day | 37 (7.70) | 31 (6.45) | 53 (11.04) | 68 (14.17) |
| More than 2 times/day | 26 (5.41) | 41 (8.54) | 84 (17.50) | 140 (29.17) |
| χ2(3) = 14.21, p < 0.01 | ||||
Note: Only statistically significant associations are reported.
Table 3 displays the new approach, which is clearly able to demonstrate how the worst social and behavioural factors expose adults to a greater risk for caries. Subjects reporting more than five of the worst options on the questionnaire (e.g., a cariogenic diet, smoking, lowest occupational profile, brushing teeth less than twice a day, lowest educational level, and uneven dental examination attendance) had the worst dental health. A statistically significant trend was observed for FS-T score and the worst social/behavioural conditions (Z = −4.31, p < 0.01).
Table 3.
Association between social/behavioural gradient levels and dental health (DMFT and FS-T categories)
| Gradient | “Best” level n (%) | “Good” level n (%) | “Bad” level n (%) | “Worst” level n (%) |
|---|---|---|---|---|
| 0–5 DMFT | 22 (24.18) | 24 (26.37) | 30 (32.97) | 15 (16.47) |
| 6–10 DMFT | 52 (29.38) | 67 (37.85) | 34 (19.21) | 24 (13.56) |
| 10–15 DMFT | 54 (37.24) | 42 (28.97) | 30 (20.69) | 19 (13.10) |
| 15–28 DMFT | 13 (19.41) | 20 (29.85) | 17 (25.37) | 17 (25.37) |
| χ2(9) = 20.17 p = 0.02, Z = 0.02 p = 0.99 | ||||
| 3–23 FS-T | 13 (20.63) | 15 (23.81) | 15 (23.81) | 20 (31.75) |
| 24–25 FS-T | 16 (22.22) | 22 (30.56) | 20 (27.78) | 14 (19.44) |
| 26–27 FS-T | 41 (29.93) | 40 (29.20) | 37 (27.01) | 19 (13.86) |
| 28 FS-T | 71 (34.13) | 76 (36.54) | 39 (18.75) | 22 (10.58) |
| χ2(9) = 25.68 p < 0.01, Z = − 4.31 p < 0.01 | ||||
Multinomial logistic regression models were carried out to assess the association between the categorized DMFT/FS-T scores and the social gradient and oral health behaviours (Table 4). In the first model, caries experience (DMFT categorization) was used as the dependent variable. Here, gender (female) played a protective role in caries, and the association between the two variables became stronger as caries experience increased (p < 0.01, except for 0–5 DMFT, where p = 0.05). A clear association was also found between occupational status and caries, indicating that low-status occupational categories corresponded to more experience with caries. Additionally, a strong association was noted between the highest scores of DMFT and the frequency of tooth brushing; brushing teeth more than twice per day had a protective effect on mild and severe caries experience.
Table 4.
Multinomial logistic regression showing significant associations of categorized DMFT and FS-T scores with position on the social gradient and oral health behaviours
| RRR | SE | P > |z| | [95% CI] | |
|---|---|---|---|---|
| 0–5 DMFT (base outcome) | ||||
| 6–10 DMFT | ||||
| Gender (female) | 1.74 | 0.50 | 0.05 | 0.99–3.05 |
| Work category (Unemployed/housewife) | 1.67 | 0.22 | <0.01 | 1.28–2.17 |
| 10–15 DMFT | ||||
| Gender (female) | 3.44 | 1.03 | <0.01 | 1.91–6.20 |
| Work category (Unemployed/housewife) | 2.26 | 0.34 | <0.01 | 1.67–3.04 |
| Tooth brushing (Less than 2 times/day) | 0.56 | 0.18 | 0.06 | 0.30–1.03 |
| 15–28 DMFT | ||||
| Gender (female) | 3.94 | 1.45 | <0.01 | 1.91–8.11 |
| Work category (Unemployed/housewife) | 3.19 | 0.68 | <0.01 | 2.10–4.84 |
| Tooth brushing (Less than 2 times/day) | 0.16 | 0.62 | <0.01 | 0.07–0.34 |
| Number of observations = 480, Log-likelihood = −583.97 p < 0.01 | ||||
| RRR | SE | P > |z| | [95% CI] | |
| 3–23 FS-T | ||||
| Gender (female) | 1.97 | 0.61 | 0.03 | 1.08–3.62 |
| Smoking status (smoker) | 2.54 | 0.83 | <0.01 | 1.33–4.84 |
| Educational level (primary school) | 0.51 | 0.11 | <0.01 | 0.33–0.79 |
| Tooth brushing (<2 times/day) | 0.39 | 0.12 | <0.01 | 0.21–0.72 |
| 24–25 FS-T | ||||
| Gender (female) | 1.75 | 0.50 | 0.05 | 0.99–3.08 |
| Smoking status (smoker) | 2.01 | 0.64 | 0.02 | 1.07–3.78 |
| Educational level (primary school) | 0.48 | 0.10 | <0.01 | 0.32–0.73 |
| 26–27 FS-T | ||||
| Educational level (primary school) | 0.69 | 0.11 | 0.02 | 0.50–0.95 |
| 28 FS-T (base outcome) | ||||
Number of observations = 480, Log-likelihood = −583.27 p < 0.01
Categories 1 and 2 of FS-T (3–23 and 24–25) were mildly associated with gender (p = 0.03 and p = 0.05, respectively); women had better oral health status. The same categories also showed a statistically significant association with smoking (p < 0.01 and p = 0.02, respectively). As expected, the model demonstrated a strong association between educational level and oral health status, showing that the best oral health status was related to the highest educational level (p < 0.01).
Discussion
The purpose of this study, which was conducted using a sample of Italian (Sardinian) adults, was to describe the developmental process for generating a social/behavioural gradient and to explore this gradient’s potential presence in dental health using a cross-sectional survey.
To the authors’ knowledge, a combined model of a social/behavioural gradient has not been proposed previously. The results confirm the hypothesis: In the study population, a social/behavioural gradient was found to be associated with dental health. Caries experience was almost ubiquitous, and the worst social and behavioural conditions appear to expose adults to greater risk for caries.
In the studied population, all stages of the caries process were recorded, and the snapshot of the disease demonstrates that the highest number of caries lesions was detected in subjects with the worst social/behavioural conditions (e.g., cariogenic diet, smoking, lowest occupational profile, brushing teeth less than twice a day, lowest educational level, and uneven dental examination attendance). Conversely, as the social/behavioural conditions improve, the number of sound or restored teeth increases. These findings are partially consistent with those of previous studies.22,23
The social gradient occurs because of the social stratification present in society. In all societies—rich and developed or poor and underdeveloped—life experiences, behaviours, advantages, and disadvantages of its members are structured and tend to be clustered by social group.24 Several conceptualizations of the social determinants of oral health and how these operate and interact at multiple levels have been well described in the international literature.25 However, to this point, there has been little translation of these conceptual frameworks into a tangible mechanism to drive decision-making in public health and dental services. A complete reorientation of health politics is required to reduce oral health inequalities and achieve sustainable oral health improvements.
The common risk factor approach might be used by public dental practitioners in cooperation with other health professionals, considering oral health in the wider context of general health. Designing health promotion programs with common risk factors for multiple diseases, such as non-communicable diseases and oral diseases like caries, is the focus of applying the common risk factor approach. Health promotion cannot and should not be compartmentalized to address problems and diseases related only to specific parts of the body.26 Despite the lack of uniformity in current preventive policies, new strategies should be focused primarily on reducing all risk factors common to several diseases. The social/behavioural gradient proposed here might be useful in the common risk factor approach, because it can significantly increase the ability to detect high-priority groups.
Higher educational levels have been found to be associated with good general health, and it has been suggested previously that education affects health mainly by increasing an individual’s sense of control.27 Access to public dental care may weaken the social/behavioural gradient in oral health through preventive and reparative mechanisms.28 The oral health care system could be re-oriented to reduce inequalities in oral health through an evidence-based public health approach.
The main limitation of this report is related to the study design: The cross-sectional nature of the investigation did not allow for the clarification of the directionality of the association between disease and the social/behavioural gradient or of the timeframe of exposure. Nevertheless, because the social/behavioural gradient comprises factors that are almost immutable, the association might be appropriately investigated using a cross-sectional study, and causal factors might act in defined periods of the subject’s life. Additionally, the study findings refer to adults living in a country (Italy) where access to public dental services is quite limited, and the findings may not be generalizable to other countries with different oral health policies. However, the sample was quite large and representative of the national population in the targeted age range.
Conclusion
In the present study, a social/behavioural gradient was generated, and its role on dental health was evaluated among Italian adults. This newly proposed social/behavioural gradient was clearly able to demonstrate how subjects reporting the worst social and behavioural conditions (e.g., cariogenic diet, smoking, lowest occupational profile, brushing teeth less than twice a day, lowest educational level, and uneven dental examination attendance) had the worst dental health conditions. This gradient might be useful in identifying groups among the population who are at a greater risk for caries and require prevention strategies based on a common risk factor approach.
Declaration of conflicting interests
The authors declare that there is no conflict of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not for-profit sectors.
References
- 1.Tsakos G, Demakakos P, Breeze E, et al. Social gradients in oral health in older adults: findings from the English longitudinal survey of aging. Am J Public Health 2011; 101: 1892–1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Golkari A, Sabokseir A, Sheiham A, et al. Socioeconomic gradients in general and oral health of primary school children in Shiraz, Iran. F1000Res 2016; 5: 767–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanders A. Social determinants of oral health: conditions linked to socioeconomic inequalities in oral health in the Australian population. Population health series no. 7. Cat. no. POH 7. Canberra: AIHW. http://www.aihw.gov.au/publication-detail/?id=6442468051 (2007, accessed 15 September 2016).
- 4.Sanders AE, Slade GD, Turrel G, et al. The shape of the socioeconomic-oral health gradient: implications for theoretical explanations. Community Dent Oral Epidemiol 2006; 34: 310–319. [DOI] [PubMed] [Google Scholar]
- 5.Sanders AE, Spencer AJ, Slade GD. Evaluating the role of dental behavior in oral health inequalities. Community Dent Oral Epidemiol 2006; 34: 71–79. [DOI] [PubMed] [Google Scholar]
- 6.Campus G, Cagetti MG, Senna A, et al. Does smoking increase risk for caries? a cross-sectional study in an Italian military academy. Caries Res 2011; 45: 40–46. [DOI] [PubMed] [Google Scholar]
- 7.Lingström P, Holm AK, Mejàre I, et al. Dietary factors in the prevention of dental caries: a systematic review. Acta Odontol Scand 2003; 61: 331–340. [DOI] [PubMed] [Google Scholar]
- 8.Drury TF, Garcia I, Adesanya M. Socioeconomic disparities in adult oral health in the United States. Ann N Y Acad Sci 1999; 896: 322–324. [DOI] [PubMed] [Google Scholar]
- 9.Locker D. Deprivation and oral health: a review. Community Dent Oral Epidemiol 2000; 28: 161–169. [DOI] [PubMed] [Google Scholar]
- 10.Sabbah W, Tsakos G, Chandola T, et al. Social gradients in oral and general health. J Dent Res 2007; 86: 992–996. [DOI] [PubMed] [Google Scholar]
- 11.Costa SM, Martins CC, Bonfim Mde L, et al. A systematic review of socioeconomic indicators and dental caries in adults. Int J Environ Res Public Health 2012; 9: 3540–3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reisine ST, Psoter W. Socioeconomic status and selected behavioral determinants as risk factors for dental caries. J Dent Educ 2001; 65: 1009–1016. [PubMed] [Google Scholar]
- 13.Vano M, Gennai S, Karapetsa D, et al. The influence of educational level and oral hygiene behaviors on DMFT index and CPITN index in an adult Italian population: an epidemiological study. Int J Dent Hyg 2015; 13: 151–157. [DOI] [PubMed] [Google Scholar]
- 14.Carta G, Cagetti MG, Cocco F, et al. Caries-risk profiles in Italian adults using computer caries assessment system and ICDAS. Braz Oral Res 2015; 29: S1806-83242015000100306–S1806-83242015000100306. [DOI] [PubMed] [Google Scholar]
- 15.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med 2007; 4: e297–e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Castiglia P, Campus G, Solinas G, et al. Children’s oral health in Italy: training and clinical calibration of examiners for the national pathfinder about caries disease. Oral Health Prev Dent 2007; 5: 255–261. [PubMed] [Google Scholar]
- 17.Schuller AA, Holst D. Oral status indicators DMFT and FS-T: reflections on index selection. Eur J Oral Sci 2001; 109: 155–159. [DOI] [PubMed] [Google Scholar]
- 18.Pitts NB, Longbottom C. Preventive care advised (PCA)/Operative care advised (OCA)—categorising caries by the management option. Community Dent Oral Epidemiol 1995; 23: 55–59. [DOI] [PubMed] [Google Scholar]
- 19.Lesaffre E, Mwalili SM, Declerck D. Analysis of caries experience taking inter-observer bias and variability into account. J Dent res 2004; 83: 951–955. [DOI] [PubMed] [Google Scholar]
- 20.Holtfreter B, Berg MH, Kocher T, et al. Change in FS-T index in adults in the German national oral health surveys between 1989 and 2005. Community Dent Oral Epidemiol 2013; 41: 251–260. [DOI] [PubMed] [Google Scholar]
- 21.ISTAT Italian National Institute of Statistics. http://www.istat.it/en/ (2016, accessed 10 July 2016).
- 22.Susin C, Oppermann RV, Haugejorden O, et al. Tooth loss and associated risk indicators in an adult urban population from south Brazil. Acta Odontol Scand 2005; 63: 85–93. [DOI] [PubMed] [Google Scholar]
- 23.Eustaquio MV, Montiel JM, Almerich JM. Oral health survey of the adult population of the Valencia region (Spain). Med Oral Patol Oral Cir Bucal 2010; 15: e538–e544. [DOI] [PubMed] [Google Scholar]
- 24.Kosteniuk JG, Dickinson HD. Tracing the social gradient in the health of Canadians: primary and secondary determinants. Soc Sci Med 2003; 57: 263–276. [DOI] [PubMed] [Google Scholar]
- 25.Petersen PE. The World Oral Health Report 2003. Continuous improvement of oral health in the 21st century - the approach of the WHO Global Oral Health Programme. http://www.who.int/oral_health/media/en/orh_report03_en.pdf (2003, accessed 10 July 2016).
- 26.Sheiham A, Alexander D, Cohen L, et al. Global oral health inequalities: task group–implementation and delivery of oral health strategies. Adv Dent Res 2011; 23: 259–267. [DOI] [PubMed] [Google Scholar]
- 27.Grembowski D, Spiekerman C, Milgrom P. Social gradients in dental health among low-income mothers and their young children. J Helth Care Poor Underserved 2012; 23: 570–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Donaldson AN, Everitt B, Newton T, et al. Effects of social class and dental attendance on oral health. J Dent Res 2008; 87: 60–64. [DOI] [PubMed] [Google Scholar]