Abstract
Background
Among individuals without hypertension based on clinic blood pressure (BP), it is unclear who should be screened for masked hypertension, defined as having hypertension based on out-of-clinic BP. We hypothesized that individuals with a higher 10-year predicted atherosclerotic cardiovascular disease (ASCVD) risk, calculated using the Pooled Cohort risk equations, have a higher prevalence of masked hypertension.
Methods and Results
We analyzed data from the Jackson Heart Study, a population-based cohort of African Americans, to determine the association of predicted ASCVD risk with masked hypertension. The sample included 644 participants, 40–79 years of age, with clinic systolic/diastolic BP <140/90 mmHg, who completed ambulatory BP monitoring (ABPM), were free of cardiovascular disease, and had data on factors needed to calculate ASCVD risk. Ten-year predicted ASCVD risk was calculated using the Pooled Cohort risk equations. Any masked hypertension was defined as masked daytime hypertension (mean daytime systolic/diastolic BP≥135/85 mmHg), masked nighttime hypertension (mean nighttime systolic/diastolic BP≥120/70 mmHg), or masked 24-hour hypertension (mean 24-hour systolic/diastolic BP≥130/80 mmHg). The prevalence of any masked hypertension was 54.0%. Compared to participants in the lowest (<5%) predicted ASCVD risk category, multivariable adjusted prevalence ratios (95% confidence interval [CI]) for any masked hypertension were 1.36 (1.03–1.79), 1.62 (1.22–2.16), and 1.91 (1.47–2.48) for those with ASCVD risk of 5% to <7.5%, 7.5% to <10%, and ≥10%, respectively. The c-statistic for discriminating between participants with versus without any masked hypertension was 0.681 (95% CI 0.640–0.723) for ASCVD risk and 0.703 (95% CI 0.662–0.744) for clinic SBP and DBP.
Conclusions
Higher ASCVD risk was associated with an increased prevalence of masked hypertension. Although the discrimination of ASCVD risk for masked hypertension was not superior to clinic BP, risk prediction equations may be useful for identifying the subgroup of individuals with both masked hypertension and high predicted ASCVD risk.
Keywords: Cardiovascular disease risk factors, risk score, black, blood pressure measurement/monitoring, masked hypertension
Subject Terms: Hypertension, Risk Factors, Race and Ethnicity
Blood pressure (BP) is traditionally measured in the clinic setting. However, studies have demonstrated that BP measured in the clinic differs substantially when measured outside of the clinic using ambulatory blood pressure monitoring (ABPM).1, 2 Masked hypertension, defined as not having hypertension on clinic BP measurements but having hypertension based on daytime BP measurements from outside of the clinic setting, is a common phenotype with prevalence estimates ranging from 15% to 30% in population-based studies.1 When the definition of masked hypertension includes having hypertension based on nighttime BP, the prevalence has been reported to be substantially higher.3 Masked hypertension has been associated with an increased risk for atherosclerotic cardiovascular disease (ASCVD) events in several prior studies.1–6
It is unclear who should undergo ABPM to identify masked hypertension among adults without hypertension based on BP measured in the clinic. In prior studies, the prevalence of masked hypertension has increased with higher clinic systolic BP (SBP) and diastolic BP (DBP).1, 2 In addition to higher clinic BP, older age, male sex, smoking, diabetes, and antihypertensive medication use have each been associated with an increased prevalence of masked hypertension.1, 2 Therefore, a composite score based on multiple ASCVD risk factors may be a useful tool for choosing who to screen with ABPM for identifying masked hypertension.
In the current study, we evaluated whether higher 10-year predicted ASCVD risk, assessed using the Pooled Cohort risk equations,7 is associated with a higher prevalence of masked hypertension. Additionally, we compared 10-year predicted ASCVD risk to clinic BP for discriminating participants with and without masked hypertension. These analyses were conducted in the Jackson Heart Study (JHS), a large population-based cohort of African Americans. The results of this study may help identify individuals who should undergo ABPM for detecting masked hypertension.
Methods
Study population
The JHS, a population-based prospective cohort study, was designed to evaluate cardiovascular disease risk among African Americans.8 Briefly, the JHS enrolled 5,306 non-institutionalized African Americans, aged ≥20 years, between 2000 and 2004 from the Atherosclerosis Risk in the Community site in Jackson, Mississippi, a representative sample of urban and rural Jackson, Mississippi metropolitan tri-county (Hinds, Madison and Rankin counties) residents, volunteers, randomly contacted individuals and secondary family members of participants.9, 10
The current analysis was restricted to JHS participants who underwent ABPM following the baseline exam (n=1,148). Participants who did not meet the International Database on ABPM in relation to Cardiovascular Outcomes11 (IDACO) criteria for a complete ABPM recording (n=102; described below) or were missing clinic BP and/or information on antihypertensive medication use (n=30) were excluded from the current analysis. As masked hypertension can only be present among individuals without hypertension based on clinic-measured BP (i.e., clinic SBP <140 mmHg and clinic DBP <90 mmHg), participants who had clinic SBP ≥140 mmHg or clinic DBP ≥90 mmHg (n=196) were also excluded. Also, since the Pooled Cohort risk equations were developed and validated among adults 40 to 79 years of age, participants less than 40 years of age or greater than 79 years of age (n=51) were excluded.7 Participants were excluded if they had missing data on ASCVD risk factors (n=64) including age, sex, total cholesterol, high density lipoprotein cholesterol, smoking status, and diabetes. Finally, as the Pooled Cohort risk equations were designed to evaluate predicted ASCVD risk among adults without cardiovascular disease,7 participants with a history of myocardial infarction or stroke (n=61) were excluded from the current study, leaving a final sample size of 644 participants. The Institutional Review Board governing human subjects’ research at the participating institutions approved the JHS protocol and all data collection procedures. All participants provided written informed consent. The current analysis was approved by the Institutional Review Board at Columbia University and University of Alabama at Birmingham.
Data collection
Detailed descriptions of data collection, methodology, specimen collection and processing have been previously described.10, 12 Data for this analysis were collected during the baseline in-home interview and study visit and through ABPM.
Baseline characteristics
Age, sex, and education were obtained by self-report using standardized interviewer-administered questionnaires. Current smoking was defined by affirmative responses to the questions “Have you smoked more than 400 cigarettes in your lifetime?” and “Do you now smoke cigarettes?” Antihypertensive medication use in the two weeks prior to the study visit was self-reported. Height, weight, and clinic BP were measured and blood samples were collected by trained staff during the study visit. Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared. Total and high-density lipoprotein (HDL) cholesterol were quantified by an oxidase method.12 Serum glucose was measured using a glucose oxidase method on a Vitros 250 or 950, Ortho-Clinical Diagnostics analyzer.12 Hemoglobin A1c was measured using a TOSOH high performance liquid chromatography system. Diabetes was defined as a fasting (≥8 hours) serum glucose ≥126 mg/dL or hemoglobin A1c ≥6.5% or self-reported use of insulin or oral hypoglycemic medications within 2 weeks prior to the study visit. Serum creatinine was measured using a multi-point enzymatic spectrophotometric assay on a Vitros 950 Ortho-Clinical Diagnostic analyzer. Estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation.13 Reduced eGFR was defined as <60 ml/min/1.73 m2.
Clinic BP measurement
A standardized protocol was followed to measure clinic BP. Participants were asked to avoid caffeine, eating, heavy physical activity, smoking and alcohol intake for 12 hours prior to their study visit. An appropriately sized cuff, determined from an arm circumference measurement, and a random-zero sphygmomanometer (Hawksley and Sons Ltd) were used for the BP measurement.10, 14 Participants sat for at least five minutes in an upright position with their back and arms supported, feet flat on the floor and legs uncrossed before trained staff conducted two BP measurements, separated by one minute, in the right arm. The JHS Coordinating Center conducted quality control through training and semi-annual retraining of staff,15 monitoring digit preference for each staff member, and by comparing mean BP measurements within and between trained technicians. As previously described,16 a BP comparability substudy for which BP was assessed simultaneously, using a Y connector, by random-zero sphygmomanometer and an Omron HEM-907XL oscillometric device was conducted among 2,115 JHS participants in 2005–2008. The random-zero BP measurements were calibrated to the oscillometric device using robust regression. The average of the two clinic BP measurements was used for analysis.
Ambulatory blood pressure monitoring
Following the baseline study visit, participants were fitted with an ABPM device (Spacelabs 90207) on their non-dominant arm. Ambulatory BP was recorded every 20 minutes for 24 hours. Data were evaluated for quality and processed with Medifacts International’s Medicom software (Rockville, MD). IDACO criteria were used to define whether the ABPM measurement was complete.11 Participants were considered to have a complete ABPM if they had ≥10 daytime (10:00 AM to 8:00 PM) and ≥5 nighttime (midnight to 6:00 AM) SBP and DBP measurements.11
Hypertension categories
Daytime hypertension was defined as a mean ambulatory SBP ≥135 mmHg or a mean ambulatory DBP ≥85 mmHg using BP measurements obtained between 10:00 AM and 8:00 PM.17 Nighttime hypertension was defined by a mean ambulatory SBP ≥120 mmHg or a mean ambulatory DBP ≥70 mmHg using BP measurements obtained between midnight and 6:00 AM, and 24-hour hypertension was defined as a mean ambulatory SBP ≥130 mmHg or a mean ambulatory DBP ≥80 mmHg using all BP measurements obtained on ABPM.17 As the current analysis was restricted to participants with clinic SBP <140 mmHg and clinic DBP <90 mmHg, those with daytime, nighttime and 24-hour hypertension were considered to have masked daytime hypertension, masked nighttime hypertension, and masked 24-hour hypertension, respectively. Participants with masked daytime hypertension, masked nighttime hypertension, or masked 24-hour hypertension were categorized as having any masked hypertension. Participants were categorized as either having prehypertension, defined by a mean clinic SBP 120–139 mmHg or a mean clinic DBP 80–89 mmHg, or normal clinic BP, defined by a mean clinic SBP <120 mmHg and a mean clinic DBP <80 mmHg. For participants taking antihypertensive medication, “on-treatment clinic SBP/DBP of 120 to 139/80 to 89 mmHg” and “masked uncontrolled hypertension” are corresponding terms for prehypertension and masked hypertension, respectively.18 For simplicity in the presentation of the results, we use the terms “prehypertension” and “masked hypertension” for all participants, regardless of antihypertensive medication use.
Ten-year predicted ASCVD risk
In 2013, the American College of Cardiology and American Heart Association recommended the use of the Pooled Cohort risk equations for estimating10-year ASCVD risk.7 There are four race-sex specific Pooled Cohort risk equations, each of which uses age, total cholesterol, HDL cholesterol, clinic SBP and status of antihypertensive medication use, current smoking, and diabetes to calculate 10-year predicted ASCVD risk.19 For the primary analyses, participants were categorized into four 10-year predicted ASCVD risk categories: <5%, 5% to <7.5%, 7.5% to <10%, and ≥10%.7
Statistical analyses
Participant characteristics were calculated by 10-year predicted ASCVD risk category for the overall analytic sample and for those taking and not taking antihypertensive medication, separately. Herein, we describe the analysis for any masked hypertension. Identical analyses were performed for masked daytime hypertension, masked nighttime hypertension, and masked 24-hour hypertension. The prevalence of any masked hypertension was calculated by category of 10-year predicted ASCVD risk. Using the lowest 10-year predicted ASCVD risk category (<5%) as the referent group, prevalence ratios (95% confidence interval [CI]) for any masked hypertension were calculated for participants with 10-year predicted ASCVD risk of 5% to <7.5%, 7.5% to <10%, and ≥10%. Associations were examined in an unadjusted model and after adjustment for age, sex, BMI, less than high school education, and reduced eGFR. The p-trend across the categories was calculated by modeling category of 10-year predicted ASCVD risk as a continuous variable using a Cochran-Armitage test for trend. Analyses were repeated for participants taking and not taking antihypertensive medication, separately. Due to a limited sample size being available in some sub-groups, participants were grouped into three categories of 10-year predicted ASCVD risk (<5%, 5% to <7.5%, ≥7.5%) for these stratified analyses. The distribution of 10-year predicted ASCVD risk categories was then calculated for participants with and without any masked hypertension, separately.
As previous studies have demonstrated a substantial diagnostic overlap between prehypertension and masked hypertension,6, 20, 21 the prevalence and prevalence ratios (95% CI) for any masked hypertension associated with 10-year predicted ASCVD risk were calculated for participants with prehypertension and normal clinic BP, separately. Also, adjusted prevalence ratios (95% CI) for any masked hypertension were calculated for each standard deviation higher 10-year predicted ASCVD risk, clinic SBP, and clinic DBP.
The ability of the 10-year predicted ASCVD risk score and clinic SBP and DBP, clinic SBP alone, clinic DBP alone, to discriminate between participants with versus without any masked hypertension was determined by calculating c-statistics. Differences in the c-statistic were calculated comparing clinic SBP and clinic DBP together, clinic SBP alone, and clinic DBP alone versus 10-year predicted ASCVD risk. Also, differences in c-statistics were calculated comparing clinic SBP and DBP versus clinic SBP alone and separately, clinic DBP alone. Differences in the c-statistic were calculated overall, and after stratifying participants into those not taking and taking antihypertensive medication. The 95% confidence intervals for the c-statistics and the difference in c-statistics, were calculated using 1,000 iteration bootstraps with each iteration including the same sample size as in the main analyses.
P-values <0.05 were considered statistically significant. All data analyses were conducted using SAS version 9.4 (SAS Institute, Cary, NC) or Stata/IC version 12.1 (Stata Inc., College Station, TX).
Results
Participant characteristics
Participants with higher 10-year predicted ASCVD risk were older, more likely to be men, have less than high school education, be current smokers, have diabetes and reduced eGFR, and to be taking antihypertensive medication (Table 1). Mean total and LDL-cholesterol were higher and HDL-cholesterol was lower among participants with higher 10-year predicted ASCVD risk. Also, those with higher ASCVD risk had higher clinic, daytime, nighttime, and 24-hour SBP, higher clinic and nighttime DBP, and a higher prevalence of prehypertension (Supplemental Table 1). Participant characteristics and the clinic and ambulatory BP levels among participants not taking and taking antihypertensive medication, separately, are reported in Supplemental Table 2.
Table 1.
Characteristics of Jackson Heart Study participants by category of 10-year predicted atherosclerotic cardiovascular risk.
| 10-year predicted ASCVD risk | |||||
|---|---|---|---|---|---|
| Characteristics | <5% | ≥5% to <7.5% | ≥7.5% to <10% | ≥10% | p-trend |
| (n=212) | (n=93) | (n=74) | (n=265) | ||
| Age, years | 49.6 ± 6.1 | 57.8 ± 6.7 | 61.8 ± 6.4 | 66.2 ± 6.8 | <0.001 |
| Male, % | 14.2 | 33.3 | 33.8 | 40.4 | <0.001 |
| Less than high school education, % | 6.2 | 19.4 | 16.2 | 21.7 | <0.001 |
| Current smoking, % | 5.7 | 7.5 | 5.4 | 10.9 | 0.045 |
| Diabetes, % | 1.9 | 6.5 | 13.5 | 40.4 | <0.001 |
| eGFR <60 ml/min/m2, % | 0.0 | 5.4 | 10.8 | 14.7 | <0.001 |
| Body mass index, kg/m2 | 31.1 ± 7.6 | 31.7 ± 6.1 | 31.3 ± 6.6 | 30.6 ± 5.2 | 0.261 |
| Total cholesterol, mg/dL | 196.9 ± 35.5 | 199.9 ± 36.3 | 202.3 ± 36.6 | 208.7 ± 42.9 | <0.001 |
| LDL cholesterol, mg/dL | 121.9 ± 35.0 | 125.5 ± 36.4 | 126.8 ± 35.4 | 131.1 ± 36.4 | 0.005 |
| HDL cholesterol, mg/dL | 56.7 ± 15.1 | 52.9 ± 14.4 | 54.2 ± 12.4 | 54.4 ± 15.0 | 0.135 |
| Antihypertensive medication use, % | 25.0 | 51.6 | 59.5 | 73.2 | <0.001 |
The numbers in the table are mean ± standard deviation or percentages.
ASCVD: Atherosclerotic cardiovascular disease
eGFR: estimated glomerular filtration rate
HDL: high-density lipoprotein
LDL: low-density lipoprotein
ASCVD risk category and masked hypertension
The prevalence of any masked hypertension, masked daytime hypertension, masked nighttime hypertension, and masked 24-hour hypertension was 54.0%, 31.5%, 49.2%, and 34.8%, respectively. Participants with higher ASCVD risk had a higher prevalence of each type of masked hypertension (Figure 1). As compared to 10-year predicted ASCVD risk <5%, the adjusted prevalence ratio (95% CI) for having any masked hypertension was 1.36 (1.03 – 1.79), 1.62 (1.22 – 2.16), and 1.91 (1.47 – 2.48) for 10-year predicted ASCVD risk ≥5% to <7.5%, ≥7.5% to <10%, and ≥10% respectively (p-trend <0.001) (Table 2). Similar findings were observed for masked daytime hypertension, masked nighttime hypertension, and masked 24-hour hypertension, and among participants not taking and taking antihypertensive medication, separately (Supplemental Table 3)
Figure 1.
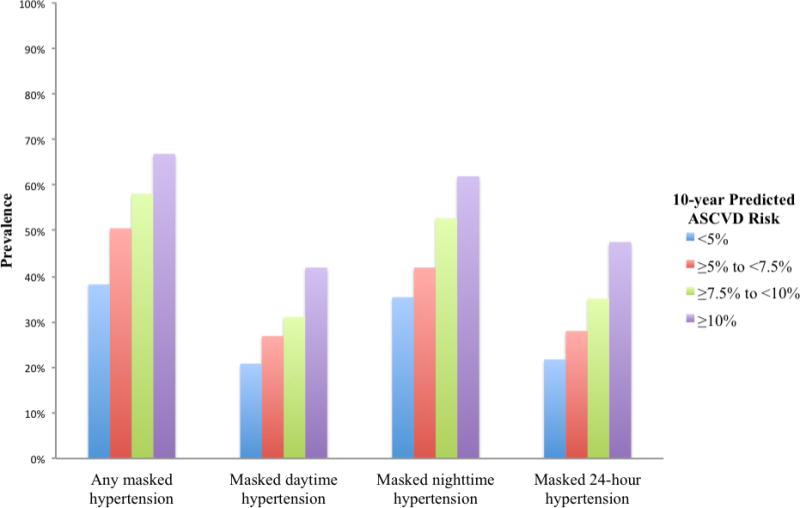
Prevalence of masked hypertension by category of 10-year predicted atherosclerotic cardiovascular disease risk.
Table 2.
Prevalence and prevalence ratios for masked hypertension by category of 10-year predicted atherosclerotic cardiovascular disease risk.
| 10-year predicted ASCVD risk | |||||
|---|---|---|---|---|---|
| <5% | ≥5% to <7.5% | ≥7.5% to <10% | ≥10% | p-trend | |
| Type of masked hypertension | (n=212) | (n=93) | (n=74) | (n=265) | |
| Prevalence | |||||
| Any masked hypertension | 38.2% | 50.5% | 58.1% | 66.8% | <0.001 |
| Masked daytime hypertension | 20.8% | 26.9% | 31.1% | 41.9% | <0.001 |
| Masked nighttime hypertension | 35.4% | 41.9% | 52.7% | 61.9% | <0.001 |
| Masked 24-hour hypertension | 21.7% | 28.0% | 35.1% | 47.5% | <0.001 |
| Unadjusted prevalence ratio (95% CI) | |||||
| Any masked hypertension | 1 (ref) | 1.32 (1.02 – 1.72) | 1.52 (1.17 – 1.97) | 1.75 (1.44 – 2.12) | <0.001 |
| Masked daytime hypertension | 1 (ref) | 1.30 (0.85 – 1.98) | 1.50 (0.97 – 2.30) | 2.02 (1.50 – 2.72) | <0.001 |
| Masked nighttime hypertension | 1 (ref) | 1.19 (0.88 – 1.60) | 1.49 (1.12 – 1.98) | 1.75 (1.43 – 2.15) | <0.001 |
| Masked 24-hour hypertension | 1 (ref) | 1.29 (0.85 – 1.95) | 1.62 (1.08 – 2.42) | 2.19 (1.65 – 2.91) | <0.001 |
| Adjusted prevalence ratio (95% CI)* | |||||
| Any masked hypertension | 1 (ref) | 1.36 (1.03 – 1.79) | 1.62 (1.22 – 2.16) | 1.91 (1.47 – 2.48) | <0.001 |
| Masked daytime hypertension | 1 (ref) | 1.52 (0.97 – 2.37) | 1.82 (1.13 – 2.91) | 2.64 (1.74 – 4.01) | <0.001 |
| Masked nighttime hypertension | 1 (ref) | 1.13 (0.83 – 1.55) | 1.43 (1.04 – 1.96) | 1.66 (1.24 – 2.23) | <0.001 |
| Masked 24-hour hypertension | 1 (ref) | 1.34 (0.87 – 2.06) | 1.69 (1.10 – 2.60) | 2.36 (1.60 – 3.48) | <0.001 |
ASCVD: Atherosclerotic cardiovascular disease
CI: Confidence interval
Adjusted for age, sex, body mass index, less than high school education, and estimated glomerular filtration rate <60 ml/min/m
Prevalence of ASCVD risk category by masked hypertension status
The percentage of participants with 10-year predicted ASCVD risk ≥10% was higher among those with versus without any masked hypertension (50.9% versus 29.7%), masked daytime hypertension (54.7% versus 34.9%), masked nighttime hypertension (51.7% versus 30.9%), and masked 24-hour hypertension (56.3% versus 33.1%) (Figure 2 and Supplemental Table 4). Among participants not taking and taking antihypertensive medication, separately, the percentage in the ≥7.5% ASCVD risk category was higher among those with versus without each type of masked hypertension (Supplemental Table 5 and Supplemental Figure 1).
Figure 2.
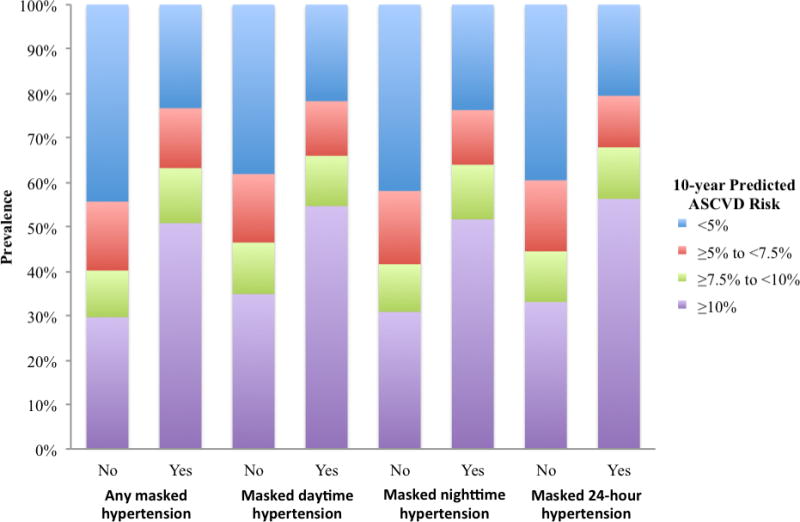
Distribution of 10-year predicted atherosclerotic cardiovascular disease risk categories among Jackson Heart Study participants with and without masked hypertension. The prevalence data, depicted here, are presented in Supplemental Table 4.
ASCVD risk category and masked hypertension, stratified by prehypertension status
The prevalence of 10-year predicted ASCVD risk ≥10% was 25.6% and 50.0% for participants with normal clinic blood pressure and prehypertension, respectively. Among participants with normal clinic BP, as compared to 10-year predicted ASCVD risk <5%, the adjusted prevalence ratio (95% CI) for having any masked hypertension was 1.73 (1.01 – 2.97), 1.88 (1.00 – 3.54), and 2.22 (1.24 – 3.99) for 10-year predicted ASCVD risk ≥5% to <7.5%, ≥7.5% to <10%, and ≥ 10% respectively (p-trend = 0.015) (Supplemental Table 6). Similar findings were observed for masked nighttime hypertension, but not masked daytime hypertension or masked 24-hour hypertension. Among participants with prehypertension, the adjusted prevalence ratio (95% CI) for having any masked hypertension was 1.06 (0.77 – 1.44), 1.29 (0.94 – 1.75), and 1.42 (1.07 – 1.89) for 10-year predicted ASCVD risk ≥5% to <7.5%, ≥7.5% to <10%, and ≥10% respectively (p-trend = 0.007). Similar findings were observed for masked daytime hypertension and masked 24-hour hypertension, but not masked nighttime hypertension.
ASCVD risk category and clinic BP for detecting masked hypertension
The prevalence ratios for any masked hypertension was larger for each standard deviation higher clinic SBP (1.31, 95% CI 1.21 – 1.41) compared with each standard deviation higher ASCVD risk score (1.23, 95% CI 1.14 – 1.33) or clinic DBP (1.13, 95% CI 1.05 – 1.22) (Table 3). Similar findings were observed for masked daytime hypertension, masked nighttime hypertension, and masked 24-hour hypertension. The multivariable-adjusted c-statistic for masked 24-hour hypertension was higher for clinic SBP and DBP versus ASCVD risk score (difference 0.036, 95% CI 0.002 to 0.073) and lower for clinic DBP alone versus ASCVD risk score (difference −0.033, 95% CI −0.070 to −0.001) (Table 4). There was no statistically significant difference in the c-statistics for masked 24-hour hypertension associated with clinic SBP alone versus ASCVD risk score. Also, there were no statistically significant differences in the c-statistic for any masked hypertension, masked daytime hypertension, and masked nighttime hypertension for clinic SBP and DBP, clinic SBP alone, and clinic DBP alone versus ASCVD risk score. There was no statistically significant difference in the c-statistic for clinic SBP alone versus clinic SBP and DBP in detecting any masked hypertension, masked daytime hypertension, masked nighttime hypertension, or masked 24-hour hypertension. The c-statistics for any masked hypertension, masked daytime hypertension, masked nighttime hypertension, and masked 24-hour hypertension were each lower for clinic DBP alone versus clinic SBP and DBP (difference −0.050, 95% CI −0.088 to −0.024); −0.070, 95% CI −0.111 to −0.036; −0.043, 95% CI −0.077 to −0.017; and −0.069, 95% CI −0.111 to −0.039, respectively).
Table 3.
Adjusted prevalence ratios for masked hypertension associated with one standard deviation higher atherosclerotic cardiovascular disease risk, clinic systolic blood pressure, and clinic diastolic blood pressure.
| Adjusted prevalence ratio (95% CI)* | ||||
|---|---|---|---|---|
| Any masked hypertension | Masked daytime hypertension | Masked nighttime hypertension | Masked 24-hour hypertension | |
| 10-year ASCVD risk (SD = 8.3%) |
1.23 (1.14 – 1.33) | 1.48 (1.32 – 1.67) | 1.22 (1.12 – 1.33) | 1.42 (1.27 – 1.58) |
| Clinic SBP (SD = 10.4 mmHg) |
1.31 (1.21 – 1.41) | 1.64 (1.44 – 1.87) | 1.30 (1.19 – 1.42) | 1.57 (1.39 – 1.77) |
| Clinic DBP (SD = 7.4 mmHg) |
1.13 (1.05 – 1.22) | 1.22 (1.08 – 1.39) | 1.13 (1.04 – 1.23) | 1.18 (1.05 – 1.33) |
ASCVD: Atherosclerotic cardiovascular disease
CI: Confidence interval
SBP: Systolic Blood Pressure
DBP: Diastolic Blood Pressure
SD: standard deviation
Adjusted for age, sex, body mass index, less than high school education, and estimated glomerular filtration rate <60 ml/min/m2
Table 4.
Adjusted c-statistics* for masked hypertension associated with 10-year predicted atherosclerotic cardiovascular disease risk, clinic systolic blood pressure and diastolic blood pressure, clinic systolic blood pressure alone, and clinic diastolic blood pressure alone. Statistically significant differences versus ASCVD risk score are shown in bold.
| Adjusted c-statistic (95% CI)* | Difference in c-statistic (95% CI) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Outcome | ASCVD risk score | Clinic SBP and DBP | Clinic SBP | Clinic DBP | Clinic SBP and DBP versus ASCVD risk score | Clinic SBP versus ASCVD risk score | Clinic DBP versus ASCVD risk score | Clinic SBP versus Clinic SBP and DBP | Clinic DBP versus Clinic SBP and DBP |
| Any masked hypertension | 0.681 (0.640 to 0.723) | 0.703 (0.663 to 0.744) | 0.703 (0.662 to 0.744) | 0.653 (0.611 to 0.696) | 0.022 (−0.014 to 0.056) |
0.022 (−0.012 to 0.057) |
−0.028 (−0.67 to 0.002) |
0.000 (−0.003 to 0.002) |
−0.050 (−0.088 to −0.024) |
| Masked daytime hypertension | 0.682 (0.636 to 0.728) | 0.721 (0.680 to 0.763) | 0.721 (0.679 to 0.762) | 0.651 (0.606 to 0.697) | 0.039 (−0.002 to 0.081) |
0.039 (−0.001 to 0.080) |
−0.031 (−0.074 to 0.004) |
0.000 (−0.007 to 0.002) |
−0.070 (−0.111 to −0.036) |
| Masked nighttime hypertension | 0.664 (0.621 to 0.706) | 0.689 (0.648 to 0.730) | 0.689 (0.648 to 0.730) | 0.646 (0.603 to 0.689) | 0.025 (−0.007 to 0.060) |
0.025 (−0.005 to 0.060) |
−0.018 (−0.051 to 0.017) |
0.000 (−0.001 to 0.002) |
−0.043 (−0.077 to −0.017) |
| Masked 24-hour hypertension | 0.696 (0.652 to 0.739) | 0.732 (0.691 to 0.772) | 0.730 (0.690 to 0.771) | 0.662 (0.618 to 0.707) |
0.036 (0.002 to 0.073) |
0.035 (0.000 to 0.072) |
−0.033 (−0.070 to −0.001) |
−0.001 (−0.011 to 0.002) |
−0.069 (−0.111 to −0.039) |
ASCVD: Atherosclerotic cardiovascular disease
CI: Confidence interval
SBP: Systolic Blood Pressure
DBP: Diastolic Blood Pressure
Adjusted for age, sex, body mass index, less than high school education, and estimated glomerular filtration rate <60 ml/min/m2
The c-statistics for masked hypertension among participants not taking and, separately, taking antihypertensive medication are shown in Supplemental Table 7. Among participants not taking antihypertensive medication, the c-statistics for any masked hypertension and masked daytime hypertension were higher for clinic SBP and DBP versus ASCVD risk score (difference 0.085, 95% CI 0.037 to 0.150; 0.039, 95% CI 0.000 to 0.030, respectively). The c-statistic for any masked hypertension was also higher for clinic SBP alone versus ASCVD risk score (difference 0.085, 95% CI 0.038 to 0.154). Among participants taking antihypertensive medication, the c-statistics for masked daytime hypertension, masked nighttime hypertension, and masked 24-hour hypertension were higher for both clinic SBP and DBP (difference 0.039, 95% CI 0.041 to 0.095; 0.025, 95% CI 0.013 to 0.064; 0.036, 95% CI 0.031 to 0.076, respectively) and clinic SBP alone (difference 0.039, 95% CI 0.043 to 0.094; 0.025, 95% CI 0.016 to 0.053; 0.035, 95% CI 0.034 to 0.071, respectively) versus the ASCVD risk score.
Discussion
In this population-based sample of African Americans, higher 10-year predicted ASCVD risk was associated with a higher prevalence of any masked hypertension, masked daytime hypertension, masked nighttime hypertension, and masked 24-hour hypertension. These associations were consistent for participants taking and not taking antihypertensive medication, and among those with prehypertension and normal clinic BP. Also, a majority of participants with each type of masked hypertension had a 10-year predicted ASCVD risk ≥ 10%. The c-statistic for discriminating between participants with versus without masked hypertension was similar or lower for predicted ASCVD risk when compared with clinic SBP and clinic DBP.
Previous studies of European and Japanese cohorts have demonstrated a high prevalence of masked hypertension and a strong association between masked hypertension and ASCVD events.1, 2, 4–6 Similar observations have been made in the JHS.3 In the current study, among participants with clinic SBP/DBP <140/90 mmHg, there was a high prevalence of masked hypertension, ranging from 31.5% to 54.0% depending on the type of masked hypertension being evaluated. There may be a role for masked hypertension screening using ABPM among African Americans given its high prevalence and strong association with ASCVD events in this population.
The optimal approach for identifying whom to screen for masked hypertension using ABPM is unknown. Several recent position papers, scientific statements and guidelines recommend that ABPM should be used to assess out-of-clinic BP.17, 22–25 However, recommendations on who to screen with ABPM to identify masked hypertension were not provided. One approach may be to perform ABPM among all individuals with clinic SBP/DBP <140/90 mmHg. We previously estimated that 153 million US adults would have to be screened using this approach,26 making it impractical. Another strategy is to perform ABPM in individuals who have risk factors for masked hypertension. Previous studies have shown that, among individuals with clinic SBP/DBP <140/90 mmHg, higher clinic BP, particularly in the prehypertension range, is a strong predictor of masked hypertension.1, 6, 20, 27 In the current analysis, higher 10-year predicted ASCVD risk, estimated with the Pooled Cohort risk equations, was associated with a higher prevalence of masked hypertension. However, the c-statistic for discriminating between participants with versus without masked hypertension was similar or lower using predicted ASCVD risk when compared with clinic SBP and clinic DBP. Despite the prior evidence that several ASCVD risk factors are associated with masked hypertension,1, 2, 21, 28, 29 clinic BP, particularly in the prehypertension range,1, 6, 20, 26 may be sufficient for identifying individuals with masked hypertension.
In the 2013 guidelines for the management of arterial hypertension, the European Society of Hypertension and European Society of Cardiology recommended that “lifestyle measures and antihypertensive drug treatment should be considered” for individuals with masked hypertension (Class IIa recommendation, Level C evidence).30 However, there have been no randomized trials evaluating whether these interventions reduce the risk of ASCVD events among individuals with masked hypertension. There is increasing evidence that predicted ASCVD risk should be considered when deciding when to initiate or intensify hypertension treatment.31, 32 In the current study, the majority (50.9%) of participants with any masked hypertension were in the highest (≥10%) ASCVD risk category. Individuals with masked hypertension and elevated ASCVD risk might derive a greater absolute cardiovascular benefit from treatment compared to individuals with masked hypertension and low ASCVD risk.31 Therefore, using elevated ASCVD risk as a screening criterion for conducting ABPM may identify the majority of individuals with masked hypertension as well as the majority of those likely to have ASCVD events.19 We acknowledge that a large percentage (38.2%) of participants with the lowest ASCVD risk (<5%) had any masked hypertension. It remains unknown whether masked hypertension is associated with an increased risk of ASCVD events among individuals with low predicted ASCVD risk. It is likely that antihypertensive medication treatment will have limited benefit in this group given their low predicted ASCVD risk. This issue has important implications for whether ABPM should be performed for individuals with low ASCVD risk to identify masked hypertension, and underscores the need for further research in this area.
There are several strengths of the current study. We used data from JHS, a population-based cohort, comprised of African Americans with a broad range of ASCVD risk. The JHS includes one of the largest samples of ABPM conducted among African Americans, and ABPM and clinic BP were conducted following standardized protocols. The large sample size allowed us to evaluate the association between ASCVD risk categories and masked hypertension among participants with normal clinic BP and prehypertension, separately, and by antihypertensive medication use. There are also several potential limitations to the current study. Participants in the JHS underwent only one ABPM session and therefore we cannot exclude the possibility that the results would have differed with the inclusion of additional 24-hour periods of ABPM. Without additional ABPM recordings prior to visit 1, it is also not possible to determine how long participants had masked hypertension. Further, clinic BP was measured using a manual device. However, for the current analysis, clinic BP values were calibrated with an oscillometric device. Finally, there was a relatively small sample size in some of the ASCVD risk categories in the sub-group analyses.
In conclusion, among African Americans without BP in the hypertensive range based on clinic measurements, higher ASCVD risk was associated with a higher prevalence of any masked hypertension, masked daytime hypertension, masked nighttime hypertension, and masked 24-hour hypertension. Over 50% of participants with each type of masked hypertension had a 10-year predicted ASCVD risk ≥10%. The c-statistic discriminating between individuals with and without masked hypertension associated with ASCVD risk was equivalent to or lower than clinic-measured BP. However, risk prediction equations may be useful for identifying individuals with both masked hypertension and increased ASCVD risk who may derive the greatest absolute risk reduction from antihypertensive treatment.
Supplementary Material
What is Known
Blood pressure measured in the clinic can differ substantially from blood pressure measured outside of the clinic assessed using ambulatory blood pressure monitoring.
Masked hypertension, defined as not having hypertension on clinic blood pressure measurements but having hypertension on ambulatory blood pressure monitoring, is a common phenotype and is associated with an increased risk of cardiovascular disease events.
Current guidelines do not specify whom with non-elevated clinic blood pressure should be screened for masked hypertension with ambulatory blood pressure monitoring.
What the Study Adds
Higher predicted atherosclerotic cardiovascular disease risk using the Pooled Cohort risk equations is associated with an increased prevalence of masked hypertension among African Americans.
Cardiovascular disease risk prediction equations may be useful in determining whom should be screened for masked hypertension using ambulatory blood pressure monitoring.
Acknowledgments
The authors wish to thank the staffs and participants of the JHS.
Funding Sources: The Jackson Heart Study is supported and conducted in collaboration with Jackson State University (HHSN268201300049C and HHSN268201300050C); University of Mississippi Medical Center (HHSN268201300046C and HHSN268201300047C); and Touglaoo College (HHSN268201300048C) contracts from the National Heart, Lung, and Blood Institute (NHLBI) and the National Center on Minority Health and Health Disparities (NCMHD) at the National Institute of Health (NIH). The current study is also supported by R01 HL117323 from the NHLBI. DEA receives support through 2T32HL007854-21. JNB III receives support through F31 HL129701 from the NHLBI. MA receives support through HL117323-02S2. DS receives support through K24-HL125704 and P01-HL047540 from the NHLBI. PM and DS receive support through 15SFRN2390002 from the American Heart Association. The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute; the National Institutes of Health; or the U.S. Department of Health and Human Services.
PM received an institutional grant from Amgen Inc. unrelated to the topic of the current manuscript.
Footnotes
Disclosures: DS is a consultant for Abbott Vascular and Novartis Pharmaceuticals Corporation. There are no other potential conflicts of interest.
References
- 1.Peacock J, Diaz KM, Viera AJ, Schwartz J, Shimbo D. Unmasking Masked Hypertension: Prevalence, Clinical Implications, Diagnosis, Correlates, and Future Directions. J Hum Hypertens. 2014;28:521–528. doi: 10.1038/jhh.2014.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Angeli F, Reboldi G, Verdecchia P. Masked hypertension: evaluation, prognosis, and treatment. Am J Hypertens. 2010;23:941–948. doi: 10.1038/ajh.2010.112. [DOI] [PubMed] [Google Scholar]
- 3.Booth JN, 3rd, Diaz KM, Seals SR, Sims M, Ravenell J, Muntner P, Shimbo D. Masked Hypertension and Cardiovascular Disease Events in a Prospective Cohort of Blacks: The Jackson Heart Study. Hypertension. 2016;68:501–510. doi: 10.1161/HYPERTENSIONAHA.116.07553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fagard RH, Cornelissen VA. Incidence of cardiovascular events in white-coat, masked and sustained hypertension versus true normotension: a meta-analysis. J Hypertens. 2007;25:2193–2198. doi: 10.1097/HJH.0b013e3282ef6185. [DOI] [PubMed] [Google Scholar]
- 5.Hansen TW, Kikuya M, Thijs L, Bjorklund-Bodegard K, Kuznetsova T, Ohkubo T, Richart T, Torp-Pedersen C, Lind L, Jeppesen J, Ibsen H, Imai Y, Staessen JA, Investigators I Prognostic superiority of daytime ambulatory over conventional blood pressure in four populations: a meta-analysis of 7,030 individuals. J Hypertens. 2007;25:1554–1564. doi: 10.1097/HJH.0b013e3281c49da5. [DOI] [PubMed] [Google Scholar]
- 6.Redmond N, Booth JN, 3rd, Tanner RM, Diaz KM, Abdalla M, Sims M, Muntner P, Shimbo D. Prevalence of Masked Hypertension and Its Association With Subclinical Cardiovascular Disease in African Americans: Results From the Jackson Heart Study. J Am Heart Assoc. 2016;5:e002284. doi: 10.1161/JAHA.115.002284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goff DC, Jr, Lloyd-Jones DM, Bennett G, Coady S, D’Agostino RB, Sr, Gibbons R, Greenland P, Lackland DT, Levy D, O’Donnell CJ, Robinson JG, Schwartz JS, Shero ST, Smith SC, Jr, Sorlie P, Stone NJ, Wilson PW, American College of Cardiology/American Heart Association Task Force on Practice G 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63:2935–2959. doi: 10.1016/j.jacc.2013.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Taylor HA., Jr The Jackson Heart Study: an overview. Ethn Dis. 2005;15:S6-1–3. [PubMed] [Google Scholar]
- 9.Wilson JG, Rotimi CN, Ekunwe L, Royal CD, Crump ME, Wyatt SB, Steffes MW, Adeyemo A, Zhou J, Taylor HA, Jr, Jaquish C. Study design for genetic analysis in the Jackson Heart Study. Ethn Dis. 2005;15:S6-30–37. [PubMed] [Google Scholar]
- 10.Taylor HA, Jr, Wilson JG, Jones DW, Sarpong DF, Srinivasan A, Garrison RJ, Nelson C, Wyatt SB. Toward resolution of cardiovascular health disparities in African Americans: design and methods of the Jackson Heart Study. Ethn Dis. 2005;15:S6-4–17. [PubMed] [Google Scholar]
- 11.Thijs L, Hansen TW, Kikuya M, Bjorklund-Bodegard K, Li Y, Dolan E, Tikhonoff V, Seidlerova J, Kuznetsova T, Stolarz K, Bianchi M, Richart T, Casiglia E, Malyutina S, Filipovsky J, Kawecka-Jaszcz K, Nikitin Y, Ohkubo T, Sandoya E, Wang J, Torp-Pedersen C, Lind L, Ibsen H, Imai Y, Staessen JA, O’Brien E, Investigators I The International Database of Ambulatory Blood Pressure in relation to Cardiovascular Outcome (IDACO): protocol and research perspectives. Blood Press Monit. 2007;12:255–262. doi: 10.1097/mbp.0b013e3280f813bc. [DOI] [PubMed] [Google Scholar]
- 12.Carpenter MA, Crow R, Steffes M, Rock W, Heilbraun J, Evans G, Skelton T, Jensen R, Sarpong D. Laboratory, reading center, and coordinating center data management methods in the Jackson Heart Study. Am J Med Sci. 2004;328:131–144. doi: 10.1097/00000441-200409000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF, 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, Ckd EPI. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barker MH, Erlanger J, Meakins J, Schneider R, Scholz SB, Ungerleider H, White PD, Wiggers C, Wright I, Bramwell C, Cotton TF, Evans W, Gilchrist AR, Hay J, Campbell M, Pressure CSB, Pressure CSB. Standard method for taking and recording blood pressure readings. J Amer Med Assoc. 1939;113:294–297. [Google Scholar]
- 15.Jackson Heart Study. Jackson Heart Study Protocol, Manual 4, Blood Pressure, Visit 1. 2001 [Google Scholar]
- 16.Abdalla M, Booth JN, 3rd, Seals SR, Spruill TM, Viera AJ, Diaz KM, Sims M, Muntner P, Shimbo D. Masked Hypertension and Incident Clinic Hypertension Among Blacks in the Jackson Heart Study. Hypertension. 2016;68:220–226. doi: 10.1161/HYPERTENSIONAHA.115.06904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O’Brien E, Parati G, Stergiou G, Asmar R, Beilin L, Bilo G, Clement D, de la Sierra A, de Leeuw P, Dolan E, Fagard R, Graves J, Head GA, Imai Y, Kario K, Lurbe E, Mallion JM, Mancia G, Mengden T, Myers M, Ogedegbe G, Ohkubo T, Omboni S, Palatini P, Redon J, Ruilope LM, Shennan A, Staessen JA, vanMontfrans G, Verdecchia P, Waeber B, Wang J, Zanchetti A, Zhang Y, European Society of Hypertension Working Group on Blood Pressure M European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens. 2013;31:1731–1768. doi: 10.1097/HJH.0b013e328363e964. [DOI] [PubMed] [Google Scholar]
- 18.Shimbo D, Abdalla M, Falzon L, Townsend RR, Muntner P. Role of Ambulatory and Home Blood Pressure Monitoring in Clinical Practice: A Narrative Review. Ann Intern Med. 2015;163:691–700. doi: 10.7326/M15-1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Muntner P, Colantonio LD, Cushman M, Goff DC, Jr, Howard G, Howard VJ, Kissela B, Levitan EB, Lloyd-Jones DM, Safford MM. Validation of the atherosclerotic cardiovascular disease Pooled Cohort risk equations. JAMA. 2014;311:1406–1415. doi: 10.1001/jama.2014.2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shimbo D, Newman JD, Schwartz JE. Masked hypertension and prehypertension: diagnostic overlap and interrelationships with left ventricular mass: the Masked Hypertension Study. Am J Hypertens. 2012;25:664–671. doi: 10.1038/ajh.2012.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diaz KM, Veerabhadrappa P, Brown MD, Whited MC, Dubbert PM, Hickson DA. Prevalence, Determinants, and Clinical Significance of Masked Hypertension in a Population-Based Sample of African Americans: The Jackson Heart Study. Am J Hypertens. 2015;28:900–908. doi: 10.1093/ajh/hpu241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hackam DG, Quinn RR, Ravani P, Rabi DM, Dasgupta K, Daskalopoulou SS, Khan NA, Herman RJ, Bacon SL, Cloutier L, Dawes M, Rabkin SW, Gilbert RE, Ruzicka M, McKay DW, Campbell TS, Grover S, Honos G, Schiffrin EL, Bolli P, Wilson TW, Feldman RD, Lindsay P, Hill MD, Gelfer M, Burns KD, Vallee M, Prasad GV, Lebel M, McLean D, Arnold JM, Moe GW, Howlett JG, Boulanger JM, Larochelle P, Leiter LA, Jones C, Ogilvie RI, Woo V, Kaczorowski J, Trudeau L, Petrella RJ, Milot A, Stone JA, Drouin D, Lavoie KL, Lamarre-Cliche M, Godwin M, Tremblay G, Hamet P, Fodor G, Carruthers SG, Pylypchuk GB, Burgess E, Lewanczuk R, Dresser GK, Penner SB, Hegele RA, McFarlane PA, Sharma M, Reid DJ, Tobe SW, Poirier L, Padwal RS, Canadian Hypertension Education P The 2013 Canadian Hypertension Education Program recommendations for blood pressure measurement, diagnosis, assessment of risk, prevention, and treatment of hypertension. Can J Cardiol. 2013;29:528–542. doi: 10.1016/j.cjca.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 23.Hypertension: The Clinical Management of Primary Hypertension in Adults: Update of Clinical Guidelines 18 and 34. London, UK: Royal College of Physicians; 2011. [PubMed] [Google Scholar]
- 24.Redon J, Lurbe E. Ambulatory blood pressure monitoring is ready to replace clinic blood pressure in the diagnosis of hypertension: con side of the argument. Hypertension. 2014;64:1169–1174. doi: 10.1161/HYPERTENSIONAHA.114.03883. [DOI] [PubMed] [Google Scholar]
- 25.Siu AL, Force USPST Screening for high blood pressure in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2015;163:778–786. doi: 10.7326/M15-2223. [DOI] [PubMed] [Google Scholar]
- 26.Booth JN, 3rd, Muntner P, Diaz KM, Viera AJ, Bello NA, Schwartz JE, Shimbo D. Evaluation of Criteria to Detect Masked Hypertension. J Clin Hypertens (Greenwich) 2016;18:1086–1094. doi: 10.1111/jch.12830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alwan H, Pruijm M, Ponte B, Ackermann D, Guessous I, Ehret G, Staessen JA, Asayama K, Vuistiner P, Younes SE, Paccaud F, Wuerzner G, Pechere-Bertschi A, Mohaupt M, Vogt B, Martin PY, Burnier M, Bochud M. Epidemiology of masked and white-coat hypertension: the family-based SKIPOGH study. PLoS One. 2014;9:e92522. doi: 10.1371/journal.pone.0092522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Verberk WJ, Kessels AG, de Leeuw PW. Prevalence, causes, and consequences of masked hypertension: a meta-analysis. Am J Hypertens. 2008;21:969–975. doi: 10.1038/ajh.2008.221. [DOI] [PubMed] [Google Scholar]
- 29.Sobrino J, Domenech M, Camafort M, Vinyoles E, Coca A, investigators Eg Prevalence of masked hypertension and associated factors in normotensive healthcare workers. Blood Press Monit. 2013;18:326–331. doi: 10.1097/MBP.0000000000000002. [DOI] [PubMed] [Google Scholar]
- 30.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Ryden L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) Eur Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 31.Jackson R, Lawes CM, Bennett DA, Milne RJ, Rodgers A. Treatment with drugs to lower blood pressure and blood cholesterol based on an individual’s absolute cardiovascular risk. Lancet. 2005;365:434–441. doi: 10.1016/S0140-6736(05)17833-7. [DOI] [PubMed] [Google Scholar]
- 32.Blood Pressure Lowering Treatment Trialists C. Sundstrom J, Arima H, Woodward M, Jackson R, Karmali K, Lloyd-Jones D, Baigent C, Emberson J, Rahimi K, MacMahon S, Patel A, Perkovic V, Turnbull F, Neal B. Blood pressure-lowering treatment based on cardiovascular risk: a meta-analysis of individual patient data. Lancet. 2014;384:591–598. doi: 10.1016/S0140-6736(14)61212-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


