Abstract
Introduction
The objective of the present study is to assess the safety and feasibility of the use of telemedicine-based services for surgical wound care and to measure patient satisfaction with telemedicine-based follow-up.
Material and methods
24 patients were included, they were provided with a corporate mail address. On day 7 after surgery patients sent, via email, an image of their surgical wound together with a completed questionnaire in order to obtain an early diagnosis. Two independent physicians studied this information and the histologic analysis of the specimen. On day 8, all patients underwent face-to-face office examination by a third physician and all of them completed a satisfaction questionnaire at the end of the study.
Results
The use of telemedicine-based services showed a sensitivity of 100%, a specificity of 91.6%, a positive predictive value of 75% and a negative predictive value of 100%.
Degree of concordance between the two physicians, as regards the necessity of face-to-face follow-up yielded a kappa coefficient of 0.42 (standard error 0.25 and confidence interval 95% (0.92–0.08), which means a moderate agreement between the two evaluations.
94% of patients were satisfied with telemedicine-based follow-up and 93% showed their preference for this procedure over conventional methods.
Conclusions
The telemedicine-based follow-up, has proven to be feasible and safe for the evaluation of early postoperative complications. Patients reported high levels of satisfaction with the procedure. Telemedicine-based follow-up could become standard practice with the development of a specific mobile application.
Keywords: Appendectomy, Telemedicine, Follow-up, Mobile phone, E-mail, Surgical wound
Highlights
-
•
A system to provide follow-up after surgery without the need of physical examination.
-
•
Using a cell phone and a mail address follow-up is achieved.
-
•
Feasibility and security of this system was assessed.
-
•
E-mail follow-up achieved high sensibility and specificity rates compared to face-to-face follow-up.
-
•
Patients were satisfied with telemedicine follow-up and preferred it to face-to-face regular examinations.
1. Introduction
According to the WHO, telemedicine can be defined as the practice of medical care over a distance using information and communication technologies (ICTs) for diagnosis, follow-up and treatment of diseases and injuries and for the continuing education and exchange of medical information in a situation where the actors are not at the same spatial or temporal location [1], [2]. Telemedicine has applications in a variety of medical areas, including teledermatology and wound care [3], [4], [5] the most popular fields, where images and videos are exchanged using telecommunication technologies.
At present, patients undergoing appendectomy are seen as outpatients one month after the operation for evaluation of surgical wound and confirmation of pathologic findings. Yet, the percentage of surgical wound infections diagnosed in face-to-face consultation among patients undergoing appendectomy after at least a one-month follow-up period reaches 3.7% [6], being inferior in laparoscopic than in open surgery (1.9% vs. 22.2%). The incidence of unusual histopathologic findings (tumors, parasites, mucocele, inflammatory bowel disease) revealed by the analysis of the resected specimen is of 1% [7].
Face-to-face consultations have an economic cost and affect patients' quality of life as it require unnecessary transfers to the health facility and absences from work [8]. Remote assessment via e-mail simplifies the follow-up of patients whose conditions or diseases make it unnecessary or impossible to undergo face-to-face examination by a surgeon.
The objective of the present study is to assess the safety and feasibility of telemedicine-based follow up in patients undergoing appendectomy in comparison with conventional face-to-face follow-up, as well as to measure patient satisfaction with telemedicine-based follow-up.
2. Material and methods
Prospective pilot study to evaluate the validity of a new diagnostic method. Images of the surgical wounds of cases obtained via their own mobile devices, questionnaires completed by patients and pathologic analysis of the surgical specimens were used to establish a diagnosis of complications vs. discharge (no complications). Control evaluation was carried out a day later via face-to-face consultation in our institution. Telemedicine-based evaluation and face-to-face consultation were carried out by independent surgeons. Two independent surgeons were in charge of telemedicine-based evaluation.
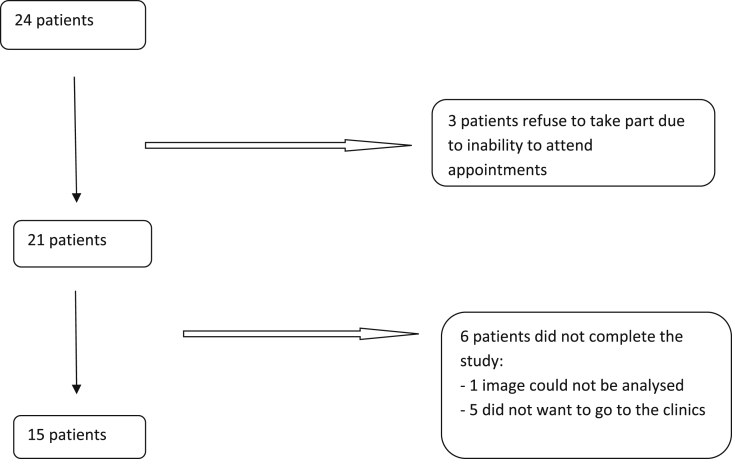
24 patients (14 males and 10 females) were treated in University Hospital Virgen del Rocío, from September 1 through December 15, 2014. Average age of patients was 25.4 ± 10.6 and all of them had undergone appendectomy in our institution. Of the 24 patients, 15 agreed to participate in the study and completed it successfully, 6 patients did not complete it correctly and 3 other patients refused to participate and give informed consent (Table 1 and Fig. 1). All patients presented with at least a surgical wound. The study was approved by the ethics committee of the University Hospital Virgen del Rocío.
Table 1.
Inclusion and exclusion criteria of patients under study.
| Inclusion criteria |
|
| Exclusion criteria |
|
Fig. 1.
Flow chart.
2.1. Procedure
Patients were discharged as soon as they met the criteria established by the physician in charge of the postoperative period. Prior to discharge, patients taking part in the study were applied exactly the same hospitalization protocol as the rest of patients treated in our institution but not participating in the study.
Seven days after surgery, each patient sent an image of the surgical wound via the corporate encrypted e-mail they had been provided with at discharge, together with a questionnaire to evaluate symptoms of systemic complications. After the reception, the information was evaluated by two independent physicians, A and B, who assigned patients to 2 different groups: complications requiring new consultation or satisfactory evolution and discharge. 24 hrs after the images and questionnaires were sent, patients underwent face-to-face examination of their surgical wound by a third physician, C, who confirmed the presence or absence of complications.
At the end of the study, patients satisfaction was measured using the Telemedicine Satisfaction Questionnaire developed and validated by Yip MP et al. [9].
Names of patients did not appear in the questionnaires sent via e-mail. The e-mail address provided to patients was encrypted and was only used under the security and privacy measures of the hospital environment. Data concerning the patients included in the study were treated and processed in compliance with the Data Protection Act (Law 15/1999 on the protection of personal data).
2.2. Variables
The variables under study include: sex, age, condition, date of surgery, surgical procedure (open/laparoscopy), surgical wound (McBurney incision/trocar/median laparotomy/others) and date of discharge.
Each questionnaire measured: presence of pain (Yes/No), fever (Yes/No), general feeling of discomfort (Yes/No) or return to normal activity (Yes/No).
In the images physicians evaluated the presence of tumor (Yes/No), rubor (Yes/No), suppuration (Yes/No) and dehiscence (Yes/No).
Histopathologic analysis of the surgical specimen was carried out in all patients.
At the end of the study, patients completed the satisfaction questionnaire.
2.3. Statistical analysis
Qualitative variables were expressed in terms of absolute frequencies and percentages. Mean values and standard deviation were used to express quantitative variables. Degree of concordance between physicians was obtained by means of Kappa coefficient.
All the analysis were performed using the statistical software IBM SPSS 19.0 (SPSS. Inc., Chicago, IL).
3. Results
The 15 patients who completed the study underwent appendectomy as they presented with symptoms of acute appendicitis. Laparoscopy was used in 10 patients (66.6%), none of them requiring conversion (0%). The remaining 5 patients were operated by laparotomy, 4 via McBurney's incision (26.6%) and another patient via infraumbilical midline approach (6.6%). All patients were discharged without complications after a hospital stay of 1.2 ± 0.48 days.
The telemedicine-based analysis of the surgical wound carried out on day 7 by surgeons A and B revealed no sign of rubor, secretion or solution of continuity in any patient (0%). In the questionnaire, one patient (66%) mentioned tumefaction and serous discharge and two patients (13.3%) reported increased temperature at wound site. None of them indicated fever or deterioration of general condition and all of them reported partial recovery of daily activities but no return to work or school.
Pain was measured using the Visual Analog Scale (VAS), which was self-completed by the patients. Only one patient reported a score of 8 out of 10 in the scale, which was considered as complication (Table 2).
Table 2.
| Pain (VAS) | Patients | % |
|---|---|---|
| NO PAIN | 5 | 33.3 |
| MILD | 4 | 26.6 |
| MODERATE | 4 | 26.6 |
| ACUTE | 2 | 13.3 |
0: No pain; 1–3: Mild pain; 4–6: Moderate pain; 7–10: Acute pain.
In the face-to-face examination carried out a day after the mailing of the questionnaires, surgeon C did not observe increase of temperature at wound site, tumefaction or rubor in any of the patients (0%) but he reported two wounds with serous secretion (13.3%) and another wound presenting with dehiscence (6.6%).
Pathologic analysis of resected specimens revealed 13 instances of phlegmonous appendicitis (86.6%), one purulent appendicitis (6.6%) and one carcinoid tumor with mesoappendix infiltration (6.6%).
The telemedicine-based analysis concluded that 4 patients (26.6%) required face-to-face consultation: 3 patients showed alterations either in the image or in the questionnaire and the fourth patient presented with a carcinoid tumor in the surgical specimen.
The face-to-face examination concluded that only 3 of the 15 patients required face-to-face examination by a surgeon: the patient with the carcinoid tumor of the appendix and two patients with surgical wound complications (Table 3).
Table 3.
Results
| Id. num. | Ev. | Pain | Rubor | Temp. | Tumefaction | Dehis. | Suppur. | Fever | P | Incision | Face-to-face consult. |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | TE | 0 | No | No | No | No | No | No | Ph | MB | No |
| FE | No | No | No | No | No | No | No | ||||
| 2 | TE | 7 | No | No | No | No | No | No | Ph | Trocar | No |
| FE | No | No | No | No | No | No | No | ||||
| 3 | TE | 0 | No | No | No | No | No | No | Ph | Trocar | No |
| FE | No | No | No | No | No | No | No | ||||
| 4 | TE | 0 | No | No | No | No | No | No | C | Trocar | Yes |
| FE | No | No | No | No | No | No | Yes | ||||
| 5 | TE | 0 | No | No | No | No | No | No | Ph | Trocar | No |
| FE | No | No | No | No | No | No | No | ||||
| 6 | TE | 2 | No | No | No | No | No | No | Ph | IU | Yes |
| FE | No | No | No | Yes | Yes serous | No | Yes | ||||
| 7 | TE | 4 | No | No | No | No | No | No | P | Trocar | No |
| FE | No | No | No | No | No | No | No | ||||
| 8 | TE | 2 | No | No | No | No | No | No | Ph | Trocar | No |
| FE | No | No | No | No | No | No | No | ||||
| 9 | TE | 3 | No | Yes | No | No | No | No | Ph | Trocar | No |
| FE | No | No | No | No | No | No | No | ||||
| 10 | TE | 8 | No | No | No | No | No | No | Ph | Trocar | Yes |
| FE | No | No | No | No | Yes serous | No | Yes | ||||
| 11 | TE | 0 | No | Yes | Yes | No | Yes serous | No | Ph | Trocar | Yes |
| FE | No | No | No | No | No | No | No | ||||
| 12 | TE | 4 | No | No | No | No | No | No | Ph | MB | No |
| FE | No | No | No | No | No | No | No | ||||
| 13 | TE | 3 | No | No | No | No | No | No | Ph | MB | No |
| FE | No | No | No | No | No | No | No | ||||
| 14 | TE | 6 | No | No | No | No | No | No | Ph | Trocar | No |
| FE | No | No | No | No | No | No | No | ||||
| 15 | TE | 4 | No | No | No | No | No | No | Ph | MB | No |
| FE | No | No | No | No | No | No | No |
Id. Numb: Identification number of each patient; Ev: Evaluation; TE: Telemedicine-based evaluation; FE: face-to-face evaluation.
Ph: Phlegmonous; C: Carcinoid; P: Purulent; MB: McBurney; IU: Infraumbilical Midline.
Degree of concordance between the two physicians, A and B, as regards the necessity of face-to-face consultation yielded a kappa coefficient of 0.42 (standard error 0.25 and confidence interval 95% (0.08–0.92).
Telemedicine-based services showed a sensitivity of 100%, detecting all instances of surgical wound complication and a specificity of 91.67%, as one of the positive cases in the telemedicine-based evaluation was not confirmed by the face-to-face consultation. Positive predictive value was 75% as only 3 of the 4 patients considered for face-to-face examination presented with actual complications. As regards the negative predictive value, it reached 100% as the face-to-face examination confirmed the results of the telemedicine-based analysis in relation to patients showing no complications.
Once the telemedicine-based and the face-to-face examinations were completed, the satisfaction questionnaire showed that 94% of the patients were satisfied with the telemedicine-based follow-up. 99% scored the quality of the procedure positively; 92% considered that both telemedicine-based and conventional face-to-face follow-up were similar and 91% showed a positive attitude towards the new procedure. 93% of the patients expressed their preference for this procedure over conventional methods (Table 4).
Table 4.
Outcomes of satisfaction questionnaire.
| Factor | Num. item | % | Item |
|---|---|---|---|
| I | 1 | 100 | The information I get prior to the study is sufficient |
| 2 | 97 | It is easy to complete the questionnaire | |
| 3 | 100 | It is easy to obtain and send the images | |
| II | 4 | 100 | Telemedicine saves me time travelling to hospital or a specialist clinic |
| 5 | 93 | Telemedicine is cost-saving in comparison to face-to-face appointment | |
| 6 | 71 | Telemedicine avoids absences from work/university/school | |
| 7 | 97 | I find telemedicine more comfortable | |
| 9 | 97 | Telemedicine facilitates early detection of complications | |
| III | 8 | 90 | I find telemedicine a reliable way to receive health care services |
| 10 | 90 | I do receive adequate attention | |
| 11 | 92 | I find telemedicine an acceptable way to receive health care services | |
| 12 | 93 | I'd rather use telemedicine than face-to-face consultation |
4. Discussion
The outcomes of the present study show the feasibility of telemedicine for the follow-up of emergency surgery wounds, under routine conditions, using new generation mobile phones and exchange of information via e-mail. Telemedicine also appears to be a valid option to follow up other surgical wounds, particularly wounds resulting from ambulatory surgery.
Successful wound management following emergency surgery poses a challenge to surgeons because of the high incidence of infections and complications associated to this type of wounds [6], [7]. Face-to-face consultations have an economic cost and affect patients quality of life as they require unnecessary transfers to the health facility and absences from work. In general, initial management of surgical wounds is carried out by the nurses in outpatients clinics who, in case of doubt or complications refer patients to the emergency department of a hospital. This means that some patients must pay a number of unnecessary visits to the emergency department and a double transfer, first to the clinic and then to the hospital [8].
The new generation of mobile telephones is the ideal tool to carry out telemedicine-based follow-up as they are small portable devices easy to use [10]. Images of acceptable quality can be obtained and sent immediately via e-mail from the patient's home. These technological advances are the basis of our protocol: patients send via e-mail an image of their surgical wounds together with a clinical evaluation questionnaire and a surgeon gets immediate access to all the information. This remote surgeon has the image on a computer screen and can evaluate it with the answers of the questionnaire and based on this information, he can contact patients for a face-to-face consultation if necessary.
To evaluate whether this scenario is viable, we performed a feasibility study at our institution. Our aim was to carry out the evaluation in a setting as close as possible to reality. For that reason, we decided to obtain the images under routine conditions. Patients took the images and transferred them via e-mail using their own device and from their home. Two remote physicians analyzed the images and a third surgeon carried out the face-to-face consultation.
The evaluation of the remote physicians was excellent compared with the face-to-face consultation. Degree of concordance between independent physicians reached 86.6%. Remote physicians could not detect only one local complication, being able to identify the rest of complications.
The kappa coefficients for the telemedicine-based evaluations carried out by physicians A and B showed a moderate agreement.
Telemedicine-based evaluation showed a sensitivity of 100% and a negative predictive value of 100%. This suggests that the remote evaluation successfully detected all instances of surgical wound complications as well as patients who did not require face-to-face consultation in the absence of complications.
The specificity of 91.7% and the positive predictive value of 100% of the remote evaluation are explained by one complication detected in this evaluation, which was not subsequently confirmed by the face-to-face consultation.
The high sensitivity and specificity together with the negative predictive value of 100% confirm the feasibility and safety of the use of telemedicine-based services for the follow up of patients. The aim of telemedicine-based follow-up is to avoid that some complications may be unnoticed in the face-to-face evaluation. The high sensitivity and negative predictive value of our study guarantee such an objective without affecting specificity and positive predictive values, which remain high.
We should also pay special attention to how patients and physicians perceive the interaction resulting from this new follow-up procedure. Our patients reported a high level of satisfaction, over 90%. They were satisfied with the use of telemedicine-based services and defined remote follow-up as a high quality procedure. Most of them considered telemedicine-based follow-up as similar or even superior to conventional procedures and 93% of the patients expressed their preference for remote follow-up over conventional methods. Although these preliminary results seem promising, we must state that the demographic characteristics of our study population-young patients, close to the new technologies, users of smart phones-could constitute a bias. Therefore, further studies in larger cohorts should be carried out as this high level of satisfaction may decrease in a different type of patients.
As regards health care costs, in 2002, the INSALUD (National Health Institute) estimated the direct costs of diabetic patients in Spain, considering both direct costs (labor costs and running costs) and indirect costs (building maintenance, subordinate staff, catering, management of appointments and admissions and others). According to the results of such estimation, the cost of each first visit was € 79.4 and the cost of each subsequent visit €47.6 [8].
These figures suggest that the potential saving derived from the use of telemedicine-based services to follow up 10 patients would amount to €794, corresponding to direct costs. We would have to add to this figure the specific indirect costs per patient.
The collaborative follow-up model we present here, in which both patients and surgeons become responsible for the development and outcome of the consultation, means a step forward to increase patients motivation and compliance with protocols. New generation mobile devices allow patients to play an active part in their own recovery and get involved in the process as they have to send the image of their wounds to surgeons for further analysis. The possibility of immediate access to the images, the questionnaires and pathologic findings has the potential to improve patients care drastically [11].
In conclusion, the high sensitivity and specificity of the use of telemedicine-based services to follow up patients make it a feasible and safe method. The degree of acceptance and satisfaction reported by patients was very high. Moreover, this collaborative follow-up model might reduce costs to our health system and gets patients fully involved in their recovery.
We are aware that the results of our study must be analyzed critically, especially due to the reduced number of selected patients included in our study and the low incidence of complications. Our study, however, offers preliminary evidence that this novel use of telemedicine-based services to follow up surgical wounds through the combination of clinical and imaging techniques may be suitable for remote management of patients. It would be advisable to test this follow-up method on larger populations and to incorporate it in the routine practice to confirm its value to promote cooperation between patients and surgeons, facilitate self-management, boost confidence and improve surgical management and reduce readmission rates in patients with surgery-derived complications. No doubt telemedicine will play an important role in future health care.
Fundings
No sources or funding for research or publication.
Contributions
a. Juan José Segura Sampedro, Inés Rivero Belenchón and Rosa M Jimenez-Rodriguez were responsible for conceptualizing and designing the study; collecting, analyzing and interpreting the data and drafting the manuscript.
b. Verónica Pino Díaz, MC, Rodríguez, Felipe Pareja Ciuró and Javier Padillo contributed to the study concept and design.
c. Juan José Segura Sampedro and Rosa M Jimenez-Rodriguez were responsible for the critical revision of the intellectual content of the manuscript.
d. All authors gave their approval on the final version for publication.
Conflicts of interest
No conflicts of interest.
Guarantor
Juan José Segura Sampedro.
Authors disclosures
Drs. Juan José Segura Sampedro, Inés Rivero Belenchón, Verónica Pino Díaz, MC Rodríguez, Felipe Pareja Ciuró, Javier Padillo and Rosa María Jiménez Rodríguez have no conflicts of interest or financial ties to disclose.
References
- 1.Bashshur R.L., Shannon G., Krupinski E.A., Grigsby J. Sustaining and realizing the promise of telemedicine. Telemed. J. E Health. 2013;19:339–345. doi: 10.1089/tmj.2012.0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Komesaroff P. Telehealth series. Intern Med. J. 2013;43:581. doi: 10.1111/imj.12145. Editor’s note. [DOI] [PubMed] [Google Scholar]
- 3.Nordheim L.V., Haavind M.T., Iversen M.M. Effect of telemedicine follow-up care of leg and foot ulcers: a systematic review. BMC Health Serv. Res. 2014;14:565. doi: 10.1186/s12913-014-0565-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hasselberg M., Beer N., Blom L., Wallis L.A., Laflamme L. Image-based medical expert teleconsultation in acute care of injuries. A systematic review of effects on information accuracy, diagnostic validity, clinical outcome, and user satisfaction. PLoS One. 2014;9:e98539. doi: 10.1371/journal.pone.0098539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gagnon M.-P., Breton E., Courcy F., Quirion S., Côté J., Paré G. The influence of a wound care teleassistance service on nursing practice: a case study in Quebec. Telemed. J. E Health. 2014;20:1–8. doi: 10.1089/tmj.2013.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mehrabi Bahar M., Jangjoo A., Amouzeshi A., Kavianifar K. Wound infection incidence in patients with simple and gangrenous or perforated appendicitis. Arch. Iran. Med. 2010;13:13–16. [PubMed] [Google Scholar]
- 7.Akbulut S., Tas M., Sogutcu N., Arikanoglu Z., Basbug M., Ulku A. Unusual histopathological findings in appendectomy specimens: a retrospective analysis and literature review. World J. Gastroenterol. 2011;17:1961–1970. doi: 10.3748/wjg.v17.i15.1961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oliva J., Lobo F., Molina B., Monereo S. Direct health care costs of diabetic patients in Spain. Diabetes Care. 2004;27:2616–2621. doi: 10.2337/diacare.27.11.2616. [DOI] [PubMed] [Google Scholar]
- 9.Yip M.P., Chang A.M., Chan J., MacKenzie A.E. Development of the Telemedicine Satisfaction Questionnaire to evaluate patient satisfaction with telemedicine: a preliminary study. J. Telemed. Telecare. 2003;9:46–50. doi: 10.1258/135763303321159693. [DOI] [PubMed] [Google Scholar]
- 10.Martínez-Ramos C., Cerdán M.T., López R.S. Mobile phone-based telemedicine system for the home follow-up of patients undergoing ambulatory surgery. Telemed. J. E Health. 2009;15:531–537. doi: 10.1089/tmj.2009.0003. [DOI] [PubMed] [Google Scholar]
- 11.Sikka N., Carlin K.N., Pines J., Pirri M., Strauss R., Rahimi F. The use of mobile phones for acute wound care: attitudes and opinions of emergency department patients. J. Health Commun. 2012;17:37–43. doi: 10.1080/10810730.2011.649161. [DOI] [PubMed] [Google Scholar]