Highlights
-
•
Stroke subjects had lower EE during the 6MWT and SCT compared to the healthy subjects.
-
•
Stroke subjects had higher EC during the 6MWT and SCT compared to the healthy subjects.
-
•
Walking speed differentiated healthy from stroke subjects gait.
-
•
The stroke subjects who walked faster showed better energy efficiency.
-
•
Evidence-based interventions to improve walking speed should be implemented.
Keywords: Stroke, Walking, Energy metabolism, Oxygen consumption, Rehabilitation
Abstract
Background
Subjects with stroke show higher energy cost (EC) during walking, when compared to healthy individuals, but the mechanisms are not fully understood. Additionally, the behavior of physiological variables during other activities has not been investigated.
Objectives
To investigate energy expenditure (EE) and EC during the six-minute walking test (6MWT) and stair climb test (SCT) in chronic stroke subjects compared to healthy controls.
Methods
Cross-sectional study in which stroke subjects (n = 18) (community-walking speed ≥0.8 m/s) or limited-community <0.8 m/s walkers and matched healthy controls (n = 18) had their EE and EC assessed during the 6MWT and SCT with a portable monitoring system.
Results
Significant differences in EE were observed for both the 6MWT (MD 7.29; 95%CI 4.08–10.50) and SCT (MD 8.53; 95%CI 5.07–12.00) between the stroke and control groups, but not between the stroke subgroups. Significant between-group differences in EC were found for both the 6MWT and SCT. For the 6MWT, differences were significant between the limited-community and the community walkers (MD 0.19; 95%CI 0.05–0.33) and controls (MD 0.17; 95%CI 0.04–0.29). No significant differences were found between the community walkers and controls (MD 0.02; 95%CI −0.09 to 0.13). For the SCT, the limited-community walkers showed highest EC, followed by the community walkers, and controls.
Conclusions
Both stroke subgroups demonstrated lower EE compared to healthy controls. During the 6MWT, the limited-community walkers demonstrated higher EC compared to the community walkers and controls. During the SCT, the limited-community walkers demonstrated higher EC, followed by the community walkers, and controls.
Introduction
Physiological energy measurements are reliable methods to assess quantitatively the changes imposed by gait disabilities.1 After a stroke, individuals are left with several impairments and disabilities, which interfere with their movement efficiency. Although the mechanisms are not fully understood, the higher energy cost (EC) of walking after stroke has been linked to reduced walking performance and restrictions in community participation.2
The Compendium of Physical Activities3 provides normative data for the estimation of metabolic cost of hundreds of specific daily activities for healthy individuals. Meanwhile, it was observed that, even for the elderly, the real metabolic costs of daily activities are substantially different from the normative values proposed by the Compendium. In addition, mobility impairments may increase the metabolic cost4 of everyday activities. In this sense, it is important to know if, after stroke, the severity of impairments and levels of disabilities could affect the efficiency of the movement.
Previous studies5, 6, 7 used treadmills to examine the differences in oxygen consumption between stroke and healthy individuals. The advantage of using treadmills is that walking speeds can be more easily controlled.8 However, the automaticity provided by the treadmills is not comparable to that of daily activities, which can impose different demands on individuals with stroke. A recent study9 reported that, compared to healthy controls, stroke individuals demonstrated lower energy expenditure (EE) and EC during the performance of typical motor activities, such as sit-to-walk-to-sit, walking over an obstacle, walking at comfortable speeds, and reaching for an object, while in a standing position.9
A recent systematic review10 that included four studies compared the EE and EC of stroke and healthy individuals during walking. These studies investigated these variables during overground walking, with a mean sample of 30 individuals, including both stroke and healthy controls. In this sense, even for the most basic daily activity, i.e., overground walking, there is still limited information regarding the differences in EE and EC between stroke and healthy individuals. For example, no studies were found that compared the energy variables of stroke individuals with different functional levels (i.e., various walking speeds) to healthy controls. Similarly, no study was found that investigated the behavior and characteristics of energy variables in individuals with stroke during stair management. For instance, stairs are common in many places11 and the ability to manage stairs has been shown to be the best predictor of free-living physical activity with community-dwelling stroke individuals.12 However, there is no available data regarding the metabolic demands during stair negotiation in individuals with stroke.
Therefore, the aim of this study was to investigate EE and EC during the performance of the six-minute walking test (6MWT) and stair climb test (SCT) in individuals with chronic stroke, who were classified as community and limited-community walkers, compared to age- and sex-matched healthy controls.
Methods
Design
For this cross-sectional study, the participants were recruited from the general community and outpatient physical therapy clinics of the city of Belo Horizonte, Brazil. This study was conducted from September to December 2014. The outcome measures were collected in random order, during the afternoons, over one day in a university laboratory setting. Prior to the data collection, at least 500 mL of water were provided to the participants to ensure normal hydration. The participants were asked to avoid strenuous activity in the previous 24 h and to keep taking their usual medications. In addition, they were asked to avoid taking any stimulants, such as coffee, black tea, or chocolate, on the day of the test. This study was approved by the Research Ethics Review Board of Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil (#ETIC 0254.0.203.000.11), and prior to data collection, all participants provided written consent.
Participants
Individuals with chronic stroke were eligible if they were ≥20 years of age, had a mean duration of unilateral stroke between one and five years, and were able to walk at least 14 m independently, without walking aids. They were excluded if they had cognitive deficits as determined by the following Brazilian education-adjusted cut-off scores on the Mini-mental state examination: 18/19 for the individuals with illiteracy and 24/25 for those with basic education13 or any other neurological or orthopedic disorder.
The outcome measures were collected by two well-trained physical therapists, who had clinical and research experience in stroke rehabilitation. Characteristics, such as age, sex, paretic side, time since the onset of the stroke, tonus of the plantar-flexor muscles (modified Ashworth scale), functional independence (Barthel Index), motor recovery (Fugl-Meyer – lower extremity section scores), minute ventilation-carbon dioxide production (VE/VCO2), and respiratory exchange ratio (RER), were collected. During the 6MWT and SCT, the mean perceived exertion was collected. Based on their walking speed values, the individuals with stroke were stratified into two clinically functional subgroups: community walkers (walking speed ≥0.8 m/s) and limited-community walkers (walking speed <0.8 m/s).14
Outcomes
Measures of EE, determined by oxygen consumption (VO2) in mL kg−1 min−1 during the 6MWT and SCT, were randomly collected with a portable monitoring system (Metamax 3B – Cortex, Leipzig, Germany), which provides reliable measures in individuals with chronic stroke during walking.15
The 6MWT, which has shown acceptable test–retest reliability for individuals with stroke,16 was performed according to the procedures and recommendations of the American Thoracic Society.17 For the SCT, the individuals were asked to ascend and descend an 11-step flight of stairs (18 cm high and 30 cm deep) for five minutes, holding the handrail with their non-paretic hands, at their comfortable pace.11 To ensure safety, the examiner stood closely behind the participants during all tests.
The VO2 measures over the last two minutes (steady-state condition) of both the 6MWT and SCT were considered for analyses.18 EC was calculated by dividing the EE values by the distance, in meters, covered in the 6MWT and reported as mL kg−1 m−1. For the SCT, the distance covered was calculated as the hypotenuse of the step height and depth (35 cm) multiplied by the number of steps.
Data analyses
The characteristics of the participants are given as means (SD) or numbers (%). One-way analyses of variance (ANOVAs), followed by Bonferroni post hoc tests, were employed to investigate the differences between the groups (community walkers, limited-community walkers, and healthy controls) regarding the EE and EC during the performance of the 6MWT and SCT. All analyses were carried out with the SPSS software (version 17.0) with a significance level of 5%.
Results
Participants’ characteristics
Thirty-six individuals (18 stroke and 18 age- and sex-matched healthy controls) were assessed. The individuals with stroke had a mean time since the onset of the stroke of 25 (SD = 14) months. Eight individuals were classified as limited-community walkers and 10 as community walkers. For the stroke subjects, their means of perceived exertion during the 6MWT and SCT were 7/10 and 8/10, respectively, whereas for the healthy controls, they were 5/10 and 7/10, respectively. The characteristics of the participants are summarized in Table 1.
Table 1.
Characteristics of the participants.
| Characteristic | Limited-community walkers (n = 8) | Community walkers (n = 10) | Healthy (n = 18) |
|---|---|---|---|
| Age (years), mean (SD) | 61.4 (7.8) | 63.1 (9.3) | 62.1 (8.3) |
| Sex, n men (%) | 5 (67) | 6 (60) | 12 (67) |
| Body mass index (kg/m2), mean (SD) | 26.1 (3.2) | 25.8 (3.5) | 25.6 (3.1) |
| Paretic side, n right (%) | 4 (50) | 5 (50) | NA |
| Type of stroke, n ischemic (%) | 6 (88) | 8 (80) | NA |
| Time since stroke (months), mean (SD) | 26 (13) | 24 (15) | NA |
| Associated diseases (number), mean (SD) | 2 (1) | 2 (1) | NA |
| Tonus of the plantar flexor muscles (modified Ashworth Scale), n (%) | |||
| 0 | 0 (0) | 0 (0) | NA |
| 1 | 2 (25) | 3 (30) | |
| 1+ | 3 (37.5) | 4 (40) | |
| 2 | 2 (25) | 1 (10) | |
| 3 | 1 (12.5) | 2 (20) | |
| 4 | 0 (0) | 0 (0) | |
| Cognition (MMSE score 0–30), mean (SD) | 25 (3) | 24 (2) | 27 (2) |
| Independence (Barthel 0–20), mean (SD) | 15 (2) | 18 (1) | NA |
| Functional Mobility (Fugl-Meyer – lower extremity 0–34), mean (SD) | 16 (4) | 25 (3) | NA |
| Distance covered during the 6MWT, mean (SD) | 194 (77) | 412 (97) | 565 (92) |
| VO2(mL kg−1 min−1), mean (SD) | |||
| 6MWT | 8.99 (2.19) | 10.99 (2.45) | 17.51 (6.08) |
| SCT | 11.24 (3.06) | 16.07 (3.50) | 22.73 (5.96) |
| RER, mean (SD) | |||
| 6MWT | 0.92 (0.05) | 0.90 (0.06) | 0.90 (0.08) |
| SCT | 0.97 (0.15) | 0.95 (0.08) | 1.05 (0.09) |
| VE/VCO2, mean (SD) | |||
| 6MWT | 38.16 (3.19) | 34.63 (2.99) | 34.71 (3.39) |
| SCT | 36.47 (3.45) | 32.28 (3.46) | 33.36 (4.16) |
SD, standard deviation; MMSE, Mini Mental State Examination; VO2, oxygen expenditure; 6MWT, six-minute walking test; SCT, stair climb test; NA, not applicable; RER, respiratory exchange ratio; VE/VCO2, ventilation/carbon dioxide production.
Differences between the groups
The descriptive data regarding the energy variables during the performance of the 6MWT and SCT, as well as the ANOVA results, are given in Table 2.
Table 2.
Descriptive data (means ± standard deviations) and ANOVA results (F and p values) regarding the between-group comparisons during the performance of the six-minute walking and stair climb tests.
| Variable | Limited-community walkers (n = 8) | Community walkers (n = 10) | Healthy controls (n = 18) | F (p) values |
|---|---|---|---|---|
| Energy expenditure (mL kg−1 min−1) | ||||
| 6MWT | 8.99 ± 2.19a | 10.99 ± 2.45a | 17.51 ± 6.08b | 11.39 (<0.0001) |
| SCT | 11.24 ± 3.10a | 16.10 ± 3.50a | 22.73 ± 5.96b | 15.94 (<0.0001) |
| Energy cost (mL kg−1 m−1) | ||||
| 6MWT | 0.35 ± 0.25a | 0.16 ± 0.03b | 0.18 ± 0.04b | 6.92 (<0.0001) |
| SCT | 0.64 ± 0.15a | 0.51 ± 0.09b | 0.17 ± 0.08c | 61.92 (<0.0001) |
6MWT, six-minute walking test; SCT, stair climb test; ANOVA, analyses of variance. For each row, different letters indicate significant differences between the groups (p < 0.05).
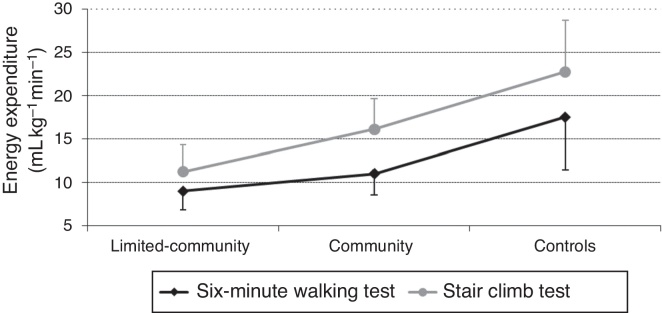
EE
For the 6MWT, significant between-group differences were found (mean difference – MD 7.29; 95%CI 4.08–10.50). Post hoc analysis revealed that the differences were significant between the stroke and control groups (community walkers and controls – MD 6.52; 95%CI 2.01–11.02, and limited-community walkers and controls – MD 8.51; 95%CI 3.27–13.76), but not between the stroke subgroups (MD −1.99; 95%CI −7.69 to 3.69) (Table 3). When compared to the control group, lower EE, i.e., lower VO2 values, were found for both stroke subgroups.
Table 3.
Mean differences and 95% confidence intervals regarding the comparisons between the groups during the performance of the six-minute walking and stair climb tests.
| Variables | Comparisons | Mean difference | 95% confidence interval |
||
|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||
| Energy expenditure (mL kg−1 min−1) during 6MWT | Limited-community walkers | Community walkers | −1.99 | −7.68 | 3.69 |
| Healthy controls | 8.51 | 3.27 | 13.76 | ||
| Community walkers | Limited-community walkers | 1.99 | −3.69 | 7.69 | |
| Healthy controls | 6.52 | 2.01 | 11.02 | ||
| Energy expenditure (mL kg−1 min−1) during the SCT | Limited-community walkers | Community walkers | 4.83 | 1.10 | 10.77 |
| Healthy controls | 11.49 | 6.02 | 16.96 | ||
| Community walkers | Limited-community walkers | 4.83 | −1.10 | 10.77 | |
| Healthy controls | 6.66 | 1.96 | 11.35 | ||
| Energy cost (mL kg−1 m−1) during the 6MWT | Limited-community walkers | Community walkers | 0.19 | 0.05 | 0.33 |
| Healthy controls | 0.17 | 0.04 | 0.29 | ||
| Community walkers | Limited-community walkers | −0.19 | −0.33 | −0.05 | |
| Healthy controls | 0.02 | 0.09 | 0.13 | ||
| Energy cost (mL kg−1 m−1) during the SCT | Limited-community walkers | Community walkers | 0.14 | 0.01 | 0.27 |
| Healthy controls | 0.47 | 0.34 | 0.59 | ||
| Community walkers | Limited-community walkers | 0.14 | −0.27 | −0.01 | |
| Healthy controls | 0.33 | 0.23 | 0.43 | ||
6MWT, six-minute walking test; SCT, stair climb test.
For the SCT, similar results were found and significant between-group differences were also observed (MD 8.53; 95%CI 5.07–12.0). The differences were significant between the stroke and control groups (community walkers and controls – MD 6.66; 95%CI 1.96–11.35 and limited-community walkers and controls – MD 11.49; 95%CI 6.02–16.96), but not between the stroke subgroups (MD 4.83; 95%CI −1.10 to 10.77), indicating that both stroke subgroups showed lower VO2 values, when compared to the control group (Table 3). Fig. 1 illustrates the EE during the 6MWT and SCT of both stroke subgroups and controls.
Figure 1.
Energy expenditure (VO2) values, in mL kg−1 min−1, during the performance of the six-minute walking and stair climb tests by the limited-community walkers, community walkers, and healthy controls.
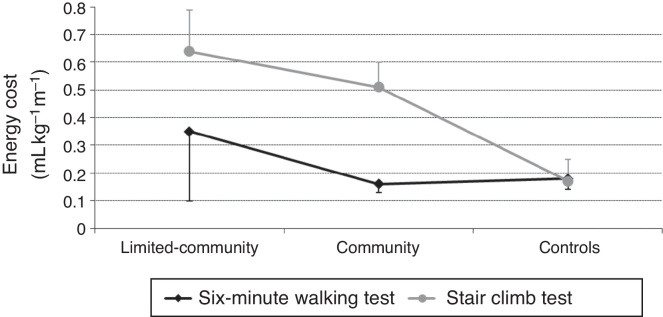
EC
For the 6MWT, significant differences were observed when the limited-community subgroup was compared to the community walkers (MD 0.19; 95%CI 0.05–0.33) and to controls (MD 0.17; 95%CI 0.04–0.29). However, no significant differences were found between the community walkers and controls (MD 0.02; 95%CI −0.09 to 0.13) (Table 3). These results indicated that the EC during the 6MWT was significantly higher for the limited-community walkers.
For the SCT, significant differences were observed between the groups. Post hoc analyses revealed that the limited-community subgroup showed higher values (MD 0.14; 95%CI 0.01–0.27) compared to the community walkers. In addition, the community walkers showed higher values (MD 0.33; 95%CI 0.23–0.43) when compared to controls (Table 3 and Fig. 2).
Figure 2.
Energy cost values, in mL kg−1 m−1, during the performance of the six-minute walking and stair climb tests by the limited-community walkers, community walkers, and healthy controls.
Discussion
The present study aimed to investigate the differences in EE and EC during the performance of the 6MWT and SCT in subgroups of individuals with chronic stroke, who were community and limited-community walkers, compared to healthy controls. This is the first study to investigate differences in energy variables in individuals with stroke who had different functional status, as determined by their walking speeds. In general, the results showed that both stroke subgroups demonstrated lower EE and higher EC during the performance of both the 6MWT and SCT, when compared to sex- and age-matched healthy controls. However, during the 6MWT, the limited-community walkers demonstrated higher EC, when compared to the community walkers and controls. During the SCT, the limited-community walkers demonstrated the highest EC, followed by the community walkers and controls.
Similar findings were reported by a recent systematic review10 including four studies, which compared the EE and EC of stroke individuals and healthy controls during overground walking. One of the studies imposed the speed to the stroke individuals, who walked with a mean speed of 0.72 m/s,19, 20 and two studies8, 21 evaluated the energy variables at self-selected speeds and the stroke individuals walked with a mean speed of 0.37 m/s. In this sense, the EE and cost at these speeds may not be applicable to stroke individuals who are community walkers, for instance. The results of the present study, which compared the energy variables of stroke subgroups (community and limited-community walkers) and healthy individuals, may provide more relevant information to clinical practice.
For the 6MWT, the community walkers showed similar VO2 values to those of the limited-community walkers. However, the metabolic efficiency, i.e., the EC of the community walkers, was similar to that of healthy controls. These results emphasize that walking speed, rather than stroke as traditionally thought,1 differentiated healthy individuals from individuals with stroke during the performance of sustained gait. Since the performance during the 6MWT could reflect physical capacity to carry out daily tasks,22, 23 it is reasonable to assume that the energy utilization of the community walkers, i.e., those with walking speeds >0.8 m/s, is more efficient and comparable to that of healthy individuals. In other words, despite some physical limitations as a result of stroke, the system could adequately cope with the demands imposed by the 6MWT.
For the SCT, similar findings regarding the VO2 measures were found. Nevertheless, although the community walkers demonstrated better metabolic efficiency than the limited-community walkers did, the healthy controls showed lower EC compared to both stroke subgroups. These findings could be explained by three main reasons. Firstly, the demands of stair negotiation are greater than those of overground walking, since this task requires important motor components that can deteriorate after stroke, such as balance, coordination,11 and the ability to maintain the weight of the body on one leg while the other advances to the next step. In addition to the greater mechanical demands, the use of the handrail can impose greater metabolic demands compared to overground walking.24 Finally, it is well known that stroke individuals have poor postural control of the vertical and horizontal components of the movement,25 which can negatively interfere with SCT performance.
The results from a recent study found that habitual walking speed alone explained 47% of the variance in EC during the SCT in individuals with chronic stroke.26 These findings highlight the importance of implementing evidence-based rehabilitation interventions, such as treadmill training27 and cardiovascular conditioning,28 in clinical practice to increase walking speed in individuals with stroke. In addition, previous studies reported that higher walking speeds were related to higher functional status, better perception of quality of life,29 and improvement in long-distance walking function2 in individuals with stroke. It is important to point out that all individuals performed the tests at high intensities, i.e., their relative efforts during both the 6MWT and SCT were similar, as no significant between-group differences were observed regarding the RER and VE/VCO2 values.
The findings of the present study have important clinical implications. The stroke subgroup of community walkers (walking speeds >0.8 m/s) demonstrated similar metabolic efficiency to that of healthy controls. These findings highlight the importance of implementing interventions aimed at increasing walking speeds. Increase in walking speed equals efficiency in terms of oxygen consumption, when comparing individuals with stroke to healthy controls. During the SCT, which imposes greater demands, it was observed that the individuals with stroke demonstrated an EC at least three times higher than that of healthy controls. This finding stresses the importance of training the components related to SCT tasks, such as balance, coordination, and muscle strength.
This study has both strengths and weaknesses. Its main strength is that the sample size (n = 36) was greater than that of previous studies with similar objectives, thereby, increasing the power of the findings. Additionally, this was the first study to carry out a subgroup analysis to evaluate the energy variables during sustained overground walking and stair negotiation. However, the sample was composed of individuals with relatively high functional levels (Barthel Index 17/20). In this sense, the results of the present study cannot be extrapolated to individuals with different characteristics. It is important to stress that, although the subjects were paired by sex and age, their body mass indices were similar. Thus, differences in body composition (e.g., fat mass) did not interfere with the results.
Conclusions
The findings of the present study demonstrated that both stroke subgroups demonstrated lower EE during the performance of the 6MWT and SCT, when compared to healthy controls. However, during the 6MWT, the limited-community walkers demonstrated higher EC compared to the community walkers and controls. During the SCT, the limited-community walkers demonstrated the highest EC, followed by the community walkers and controls.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgements
Brazilian national funding agencies: Conselho Nacional de Pesquisa (CNPq) and Fundação de Amparo à Pesquisa de Minas Gerais (FAPEMIG). The funding sources had no involvement in the study design, data collection, analysis, and interpretation of data, in the writing of the report, and in the decision to where to submit the study for publication.
References
- 1.Waters R.L., Mulroy S. The energy expenditure of normal and pathologic gait. Gait Posture. 1999;9:207–231. doi: 10.1016/s0966-6362(99)00009-0. [DOI] [PubMed] [Google Scholar]
- 2.Awad L.N., Reisman D.S., Wright T.R., Roos M.A., Binder-Macleod S.A. Maximum walking speed is a key determinant of long distance walking function after stroke. Top Stroke Rehabil. 2014;21:502–509. doi: 10.1310/tsr2106-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ainsworth B.E., Haskell W.L., Herrmann S.D. Compendium of Physical Activities: a second update of codes and MET values. Med Sci Sports Exerc. 2011;43:1575–1581. doi: 10.1249/MSS.0b013e31821ece12. [DOI] [PubMed] [Google Scholar]
- 4.Knaggs J.D., Larkin K.A., Manini T.M. Metabolic cost of daily activities and effect of mobility impairment in older adults. J Am Geriatr Soc. 2011;59:2118–2123. doi: 10.1111/j.1532-5415.2011.03655.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen G., Patten C., Kothari D.H., Zajac F.E. Gait differences between individuals with post-stroke hemiparesis and non-disabled controls at matched speeds. Gait Posture. 2005;22:51–56. doi: 10.1016/j.gaitpost.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 6.Danielsson A., Sunnerhagen K.S. Oxygen consumption during treadmill walking with and without body weight support in patients with hemiparesis after stroke and in healthy subjects. Arch Phys Med Rehabil. 2000;81:953–957. doi: 10.1053/apmr.2000.6283. [DOI] [PubMed] [Google Scholar]
- 7.Fredrickson E., Ruff R.L., Daly J.J. Physiological Cost Index as a proxy measure for the oxygen cost of gait in stroke patients. Neurorehabil Neural Repair. 2007;21:429–434. doi: 10.1177/1545968307300400. [DOI] [PubMed] [Google Scholar]
- 8.Platts M.M., Rafferty D., Paul L. Metabolic cost of over ground gait in younger stroke patients and healthy controls. Med Sci Sports Exerc. 2006;38:1041–1046. doi: 10.1249/01.mss.0000222829.34111.9c. [DOI] [PubMed] [Google Scholar]
- 9.Kafri M., Myslinski M.J., Gade V.K., Deutsch J.E. High metabolic cost and low energy expenditure for typical motor activities among individuals in the chronic phase after stroke. J Neurol Phys Ther. 2014;38:226–232. doi: 10.1097/NPT.0000000000000053. [DOI] [PubMed] [Google Scholar]
- 10.Kramer S., Johnson L., Bernhardt J., Cumming T. Energy expenditure and cost during walking after stroke: a systematic review. Arch Phys Med Rehabil. 2016;97:619–632. doi: 10.1016/j.apmr.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Pinheiro M.B., Polese J.C., Machado G.C., Faria C.D.C.M., Hirochi T.L., Teixeira-Salmela L.F. The ability to manage stairs for chronic stroke survivors improves with increases in physical activity levels. J Nov Physiother. 2013;3:159. [Google Scholar]
- 12.Alzahrani M.A., Dean C.M., Ada L. Ability to negotiate stairs predicts free-living physical activity in community-dwelling people with stroke: an observational study. Aust J Physiother. 2009;55:277–281. doi: 10.1016/s0004-9514(09)70008-x. [DOI] [PubMed] [Google Scholar]
- 13.Bertolucci P.H., Brucki S.M.D., Campacci S.R., Juliano Y. Suggestions for utilization of the mini-mental state examination in Brazil. Arq Neuropsiquiatr. 1994;52:1–7. [PubMed] [Google Scholar]
- 14.Perry J., Garrett M., Gronley J.K., Mulroy S.J. Classification of walking handicap in the stroke population. Stroke. 1995;26:982–989. doi: 10.1161/01.str.26.6.982. [DOI] [PubMed] [Google Scholar]
- 15.Polese J., Ada L., Parreira V., Faria G., Avelino P., Teixeira-Salmela L. Test–retest reliability of cardiorespiratory variables measured with the Metamax 3B during the six-minute walking test after stroke. Phys Med Rehabil Int. 2015;2:1028. [Google Scholar]
- 16.Fulk G.D., Echternach J.L., Nof L., O'Sullivan S. Clinimetric properties of the six-minute walk test in individuals undergoing rehabilitation poststroke. Physiother Theory Pract. 2008;24:195–204. doi: 10.1080/09593980701588284. [DOI] [PubMed] [Google Scholar]
- 17.ATS statement: guideline for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 18.Wasserman K., Hansen J.E., Sue D.Y., Stringer W., Whipp B. Clinical exercise testing. In: Weinberg A., editor. Principles of Exercise Testing and Interpretation. 4th ed. Lippincott, Williams and Wilkins; Philadelphia: 2005. [Google Scholar]
- 19.Bard G. Energy expenditure of hemiplegic subjects during walking. Arch Phys Med Rehabil. 1963;44:368–370. [PubMed] [Google Scholar]
- 20.Teixeira da Cunha-Filho I., Henson H., Qureshy H., Williams A.L., Holmes S.A., Protas E.J. Differential responses to measures of gait performance among healthy and neurologically impaired individuals. Arch Phys Med Rehabil. 2003;84:1774–1779. doi: 10.1016/s0003-9993(03)00373-3. [DOI] [PubMed] [Google Scholar]
- 21.Delussu A.S., Morone G., Iosa M., Bragoni M., Traballesi M., Paolucci S. Physiological responses and energy cost of walking on the Gait Trainer with and without body weight support in subacute stroke patients. J Neuroeng Rehabil. 2014;11:54. doi: 10.1186/1743-0003-11-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Polese J.C., Pinheiro M.B., Faria C.D., Britto R.R., Parreira V.F., Teixeira-Salmela L.F. Strength of the respiratory and lower limb muscles and functional capacity in chronic stroke survivors with different physical activity levels. Braz J Phys Ther. 2013;17:487–493. doi: 10.1590/S1413-35552012005000114. [DOI] [PubMed] [Google Scholar]
- 23.Britto R.R., Probst V.S., de Andrade A.F. Reference equations for the six-minute walk distance based on a Brazilian multicenter study. Braz J Phys Ther. 2013;17:556–563. doi: 10.1590/S1413-35552012005000122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Åstrand P.O., Rodahl K., Dahl H.A., Stromme S.B. 4th ed. Human Kinetics; 2003. Physical Performance. Textbook of Work Physiology: Physiological Bases of Exercise; pp. 237–272. [Google Scholar]
- 25.Snowdon N., Scott O. Perception of vertical and postural control following stroke: a clinical study. Physiotherapy. 2005;91:165–170. [Google Scholar]
- 26.Polese J., Scianni A.A., Teixeira-Salmela L. Predictors of energy cost during stair ascent and descent in individuals with chronic stroke. J Phys Ther Sci. 2015;27(12):3739–3743. doi: 10.1589/jpts.27.3739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Polese J.C., Ada L., Dean C.M., Nascimento L.R., Teixeira-Salmela L.F. Treadmill training is effective for ambulatory adults with stroke: a systematic review. J Physiother. 2013;59:73–80. doi: 10.1016/S1836-9553(13)70159-0. [DOI] [PubMed] [Google Scholar]
- 28.Mehta S., Pereira S., Janzen S. Cardiovascular conditioning for comfortable gait speed and total distance walked during the chronic stage of stroke: a meta-analysis. Top Stroke Rehabil. 2012;19:463–470. doi: 10.1310/tsr1906-463. [DOI] [PubMed] [Google Scholar]
- 29.Schmid A., Duncan P.W., Studenski S. Improvements in speed-based gait classifications are meaningful. Stroke. 2007;38:2096–2100. doi: 10.1161/STROKEAHA.106.475921. [DOI] [PubMed] [Google Scholar]