Abstract
Background
Rehabilitation before anterior cruciate ligament (ACL) reconstruction (ACLR) is effective at improving postoperative outcomes at least in the short term. Less is known about the effects of preoperative rehabilitation on functional outcomes and return-to-sport (RTS) rates 2 years after reconstruction.
Purpose/Hypothesis
The purpose of this study was to compare functional outcomes 2 years after ACLR in a cohort that underwent additional preoperative rehabilitation, including progressive strengthening and neuromuscular training after impairments were resolved, compared with a nonexperimental cohort. We hypothesized that the cohort treated with extended preoperative rehabilitation would have superior functional outcomes 2 years after ACLR.
Study Design
Cohort study; Level of evidence, 3.
Methods
This study compared outcomes after an ACL rupture in an international cohort (Delaware-Oslo ACL Cohort [DOC]) treated with extended preoperative rehabilitation, including neuromuscular training, to data from the Multicenter Orthopaedic Outcomes Network (MOON) cohort, which did not undergo extended preoperative rehabilitation. Inclusion and exclusion criteria from the DOC were applied to the MOON database to extract a homogeneous sample for comparison. Patients achieved knee impairment resolution before ACLR, and postoperative rehabilitation followed each cohort's respective criterion-based protocol. Patients completed the International Knee Documentation Committee (IKDC) subjective knee form and Knee injury and Osteoarthritis Outcome Score (KOOS) at enrollment and again 2 years after ACLR. RTS rates were calculated for each cohort at 2 years.
Results
After adjusting for baseline IKDC and KOOS scores, the DOC patients showed significant and clinically meaningful differences in IKDC and KOOS scores 2 years after ACLR. There was a significantly higher (P < .001) percentage of DOC patients returning to preinjury sports (72%) compared with those in the MOON cohort (63%).
Conclusion
The cohort treated with additional preoperative rehabilitation consisting of progressive strengthening and neuromuscular training, followed by a criterion-based postoperative rehabilitation program, had greater functional outcomes and RTS rates 2 years after ACLR. Preoperative rehabilitation should be considered as an addition to the standard of care to maximize functional outcomes after ACLR.
Keywords: knee, return to sport, rehabilitation, prehabilitation, ACL reconstruction, outcomes
Early anterior cruciate ligament (ACL) reconstruction (ACLR) remains the gold standard of treatment for active patients with ACL ruptures in the United States,20,22 with up to 175,000 reconstructions being performed annually.28 The goals for ACLR include restoring primary passive restraint, returning to preinjury activities and previous levels of function, and preserving long-term knee joint health.20,22 Reconstruction, however, does not guarantee a return to previous activities or functional levels or the prevention of posttraumatic knee osteoarthritis.10,11,20
Large, multicenter orthopaedic registries have been developed and implemented to track outcomes after ACLR in the United States and abroad. The Multicenter Orthopaedic Outcomes Network (MOON) registry pools data together from 7 orthopaedic centers across the United States.27 These centers are all highly active in orthopaedic and sports clinical treatment and research, with unified pre-operative milestones to undergo ACLR and a single criterion-based postoperative protocol with objective return-to-sport (RTS) criteria.27,30 The MOON cohort can serve as the benchmark or usual care for comparative effectiveness studies to compare ACLR outcomes.27
Rehabilitation before surgery, termed “preoperative rehabilitation” or “prehabilitation,” is physical preparation for a period of immobility and reduced activity due to surgery. Few studies have explored the effects of preoperative rehabilitation on outcomes after ACLR.13 Shaarani and colleagues,25 in a randomized controlled trial, found that a 6-week preoperative rehabilitation program led to improved functional performance and self-reported function up to 12 weeks after reconstruction. The addition of neuromuscular training to preoperative rehabilitation is another attempt to improve outcomes after an ACL injury.6,7,14,15 Specifically, perturbation training has been studied in conjunction with a preoperative rehabilitation program9 and is currently under investigation for its use after surgery.29 Grindem and colleagues12 compared functional outcome measures 2 years after ACLR in the Norwegian half of our cohort to usual care as benchmarked by the Norwegian Knee Ligament Registry (NKLR). There were statistically significant and clinically meaningfully better outcomes in the Delaware-Oslo ACL Cohort (DOC) as evidenced by higher Knee injury and Osteoarthritis Outcome Score (KOOS) results. The limitation of this study, however, is that rehabilitation in the NKLR was not standardized. The question remains how progressive preoperative rehabilitation that includes neuromuscular training affects outcomes after ACLR when both cohorts receive otherwise similar care.
The purpose of this study was to assess functional outcomes 2 years after ACLR in a cohort that underwent additional preoperative rehabilitation, including progressive strengthening and neuromuscular training after impairments were resolved, compared with a nonexperimental reference group (MOON cohort). We hypothesized that the cohort treated with extended preoperative rehabilitation would have superior functional outcomes 2 years after ACLR. The implications of this research could lead to changes in the standard of care before undergoing reconstruction after an ACL injury.
Methods
This was a cohort study comparing outcomes in an international cohort (DOC) treated with extended preoperative rehabilitation, including neuromuscular training, with data from a nonexperimental cohort (MOON consortium). The outcomes of interest included preoperative and postoperative International Knee Documentation Committee (IKDC) subjective knee form2 scores as well as KOOS24 results and RTS rates. Eighty-four patients from the Norwegian arm of the DOC were previously included in the comparison to the NKLR by Grindem and colleagues12 described above.
Patients
The DOC is an ongoing, international prospective collaboration evaluating the effects of neuromuscular training after an ACL injury and reconstruction. This collaboration includes 150 patients from the University of Delaware in the United States and 150 patients from the Norwegian Research Center for Active Rehabilitation, Norwegian School of Sport Sciences in Oslo, Norway. Patients were enrolled at both centers between 2007 and 2012. Patients were included if they had a unilateral primary ACL rupture within 7 months of enrollment and participated in level 1 or 2 sports (IKDC activity classification) for more than 50 hours per year before the injury.4 Patients were excluded if they had a concomitant grade 3 ligamentous injury, a full-thickness articular cartilage lesion larger than 1 cm2, a symptomatic meniscal tear, a potentially repairable meniscal tear, or a previous injury or surgery of the uninvolved knee. All patients underwent initial impairment resolution (little to no swelling or pain, full range of motion [ROM], 70% quadriceps strength index), followed by progressive strengthening and neuromuscular training called perturbation training, as previously described by Eitzen and Moksnes.9 After completion of these additional training sessions, patients selected to undergo ACLR or remain nonoperatively managed. While all patients were followed, only those who underwent ACLR were included in this analysis. Those from the DOC who did not immediately undergo reconstruction after training continued on a home exercise program, if needed, for maintenance until reconstruction was performed (see Appendix 1, available online at http://ajsm.sagepub.com/supplemental). All patients after ACLR underwent a criterion-based postoperative rehabilitation protocol with strict RTS criteria.1 The University of Delaware Institutional Review Board and the Region Ethics Committee for South East Norway approved all aspects of this study, and written informed consent was obtained for all patients before enrollment.
The MOON cohort consists of patients enrolled between 2002 and 2008 from 7 orthopaedic/sports medicine centers around the United States. Patients were included if they were scheduled to undergo unilateral ACLR and were between the ages of 10 and 85 years. Patients were enrolled at the time of presentation to the orthopaedic surgeon and were observed prospectively after surgery. This cohort was intended to be community based, with all ages, activity levels, injury history, and concomitant injuries included.27 All patients after ACLR underwent a criterion-based postoperative rehabilitation protocol with strict RTS criteria (see Appendix 2, available online).30 Institutional review board approval was obtained from all participating centers, and written informed consent was obtained for all patients before enrollment.
For this study, inclusion and exclusion criteria from the DOC were applied to the MOON cohort, and only those who met the criteria for the DOC described above were included. MOON data were extracted based on these criteria, and deidentified data were provided for analysis. Patients whose imaging revealed a potentially repairable meniscal injury were excluded from enrollment in the DOC. During reconstruction, however, 11% of the DOC patients underwent concomitant meniscal repair, despite initial presentation on imaging, and we therefore included those who underwent concomitant meniscal repair from the MOON dataset. Surgical variables recorded included graft type, concomitant meniscal procedures, and articular cartilage condition (Figure 1).
Figure 1.
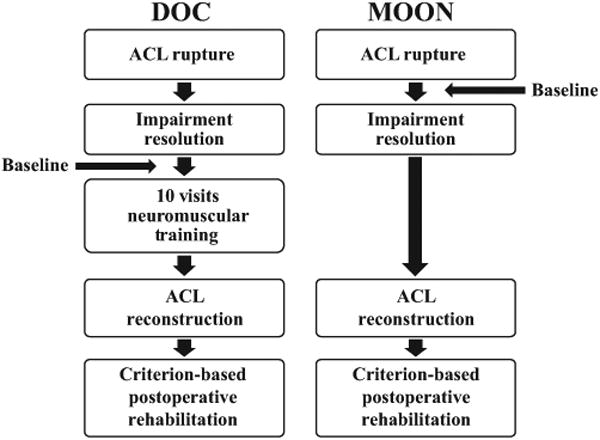
Testing timeline differences between cohorts. ACL, anterior cruciate ligament; DOC, Delaware-Oslo ACL Cohort; MOON, Multicenter Orthopaedic Outcomes Network.
Criteria for Reconstruction
Both cohorts used guidelines to determine when athletes were ready to undergo ACLR. The recommendations for the DOC patients to undergo ACLR were little to no knee joint effusion, symmetrical knee ROM, no obvious gait impairments, and a minimum of 70% quadriceps strength index (“quiet knee”). The MOON preoperative guidelines included no obvious gait impairments, knee ROM from 0° to 120°, minimal knee joint effusion, and the ability to complete 20 straight-leg raises without a lag.
Rehabilitation
Postoperative rehabilitation for the DOC patients followed a rigorous criterion-based protocol. Objective clinical criteria, such as pain, ROM, quadriceps strength and activation, and changes in knee joint effusion, were used to monitor and determine progression through the different phases of postoperative rehabilitation. These criteria, in addition to functional performance testing and patient-reported outcomes, were utilized to determine RTS readiness for athletes. Patients were observed for repeated testing at 6, 12, and 24 months after reconstruction. If patients were not maintaining strength or functional levels required to return to sport, counseling was provided. The respective rehabilitation protocols can be found in Appendices 1 and 2.
The MOON cohort patients followed a unified postoperative protocol regardless of the location at which their surgery or rehabilitation was performed. This protocol was criterion based, utilizing measures of pain, ROM, functional strength, and movement quality to progress patients through the phases of rehabilitation. RTS readiness was determined by a combination of objective measures (functional performance testing, patient-reported outcomes) and subjective measures (movement quality and confidence). Beyond those RTS criteria, the MOON protocol also recommended isokinetic strength testing, vertical jumps, and deceleration testing.
Outcome Measures
Patients completed the IKDC and KOOS preoperatively and again 2 years after ACLR. The IKDC is a valid and reliable measure commonly used in the ACL population.2,16 The minimal clinically important difference (MCID) for the IKDC is 11.5 points.16 The KOOS is a valid and reliable outcome measure commonly used in the ACL-injured population to assess outcomes in knee pain, knee symptoms, knee function in daily activity, knee function in sporting activity, and knee-related quality of life.23,24 The proposed MCID for each subscale is 10 points.23
At enrollment, each patient was asked to report his or her primary sporting activity before the injury. At 2-year follow-up, patients were asked to name their primary sport currently (MOON) or if they had returned to their preinjury sport (DOC). Patients were considered to have returned to sport if they were participating in their preinjury sport 2 years after ACLR.
Statistical Analysis
Group differences were analyzed using chi-square tests for nominal variables and t tests for continuous variables. To account for differences in baseline IKDC scores, a 1-way analysis of covariance (ANCOVA) was used to compare 2-year IKDC scores between groups with baseline IKDC scores as a covariate. To account for differences in baseline KOOS values, a 1-way ANCOVA was used to compare 2-year KOOS values between groups with baseline KOOS values as a covariate for each subscale. Because differences were found between groups in the proportion of concomitant meniscal surgery, an analysis of variance (ANOVA) was used to assess the interaction of group and meniscal surgery on 2-year IKDC scores. Because differences were found between groups in the proportion of graft types used for ACLR, an ANOVA was used to assess the interaction of group and graft type on 2-year IKDC scores. All statistical analyses were performed using PASW version 23 (SPSS Inc).
Results
Patients who underwent ACLR from the DOC (n = 192) as well as 1995 MOON patients who met the DOC inclusion criteria were included in this study. There were no differences between groups in age, sex, or body mass index (Table 1). Baseline Marx scores were available in the MOON cohort (12.78 ± 4) but not the DOC. Surgical demographics revealed a higher proportion of patellar tendon autografts (P = .001) in the MOON cohort patients and a higher proportion of hamstring autografts (P = .006) in the DOC patients. There was also a significantly higher proportion of concomitant meniscal surgery performed (P = .029) in the MOON cohort (Table 2). There were no significant group × meniscal procedure (P = .345) or group 3 graft type (P = .073) interactions on 2-year IKDC scores.
Table 1. Comparison of Baseline Characteristics Between Cohortsa.
| DOC (n = 192) | MOON (n = 1995) | P Value | |
|---|---|---|---|
| Age, y | 24.7 ± 9 | 24.3 ± 10 | .612 |
| Sex, % male | 55 | 54 | .144 |
| Body mass index, kg/m2 | 24.5 ± 4 | 25.0 ± 4 | .231 |
| Time from injury to enrollment, mo | 1.9 ± 1 | <6.0 |
Data are reported as mean ± SD unless otherwise indicated. DOC, Delaware-Oslo ACL Cohort; MOON, Multicenter Orthopaedic Outcomes Network.
Table 2. Comparison of Surgical Procedures Between Cohortsa.
| DOC (n = 192) | MOON (n = 1995) | P Value | |
|---|---|---|---|
| Patellar tendon autograft | 21 | 48 | .001 |
| Hamstring autograft | 51 | 36 | .006 |
| Soft tissue allograft | 28 | 16 | .005 |
| No meniscal procedure | 60 | 46 | .029 |
| Meniscal excision | 18 | 28 | .017 |
| Meniscal repair | 11 | 14 | .301 |
| Meniscal trephination | 2 | 2 | >.999 |
| Combination of meniscal procedures | 9 | 11 | .433 |
| Time from ACLR to 2-y follow-up, y | 2.1 ± 0.2 | 2.4 ± 0.4 | .532 |
Data are reported as % unless otherwise indicated. ACLR, anterior cruciate ligament reconstruction; DOC, Delaware-Oslo ACL Cohort; MOON, Multicenter Orthopaedic Outcomes Network.
DOC patients had significantly higher baseline IKDC scores compared with the MOON cohort patients (70 ± 13 vs 50 ± 17, respectively; P < .001), which also exceeded the MCID (Figure 2). The IKDC score in DOC patients significantly improved from baseline to posttraining (after preoperative rehabilitation) (from 70 ± 13 to 77 ± 13; P < .001). Two years after reconstruction, 148 patients from the DOC and 1994 patients from the MOON cohort completed the IKDC. After controlling for baseline IKDC scores, DOC patients continued to have significantly higher IKDC scores than MOON cohort patients at 2 years after ACLR (84 ± 25 vs 71 ± 32, respectively; P < .001), again exceeding the MCID (Figure 3). Post hoc power analysis revealed the ability to detect a difference of 2 points on the IKDC between groups.
Figure 2.
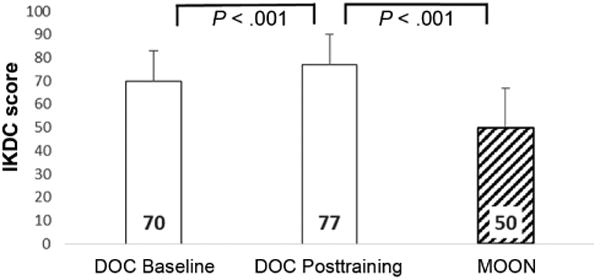
Baseline International Knee Documentation Committee (IKDC) scores between cohorts. DOC, Delaware-Oslo ACL Cohort; MOON, Multicenter Orthopaedic Outcomes Network.
Figure 3.
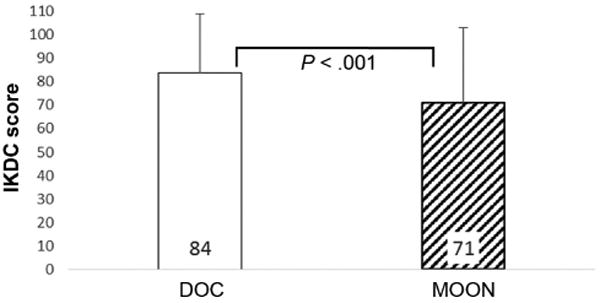
International Knee Documentation Committee (IKDC) scores 2 years after anterior cruciate ligament reconstruction. DOC, Delaware-Oslo ACL Cohort; MOON, Multicenter Orthopaedic Outcomes Network.
Baseline KOOS values were available for 1991 patients in the MOON cohort and 58 patients in the DOC. DOC patients had significantly higher baseline KOOS values than MOON cohort patients across all subscales: pain (84 ± 11 vs 73 ± 17, respectively), symptoms (75 ± 14 vs 67 ± 18, respectively), activities of daily living (93 ± 7 vs 82 ± 17, respectively), sports/recreation (66 ± 19 vs 48 ± 29, respectively), and quality of life (51 ± 19 vs 37 ± 20, respectively) (all P < .001). After controlling for baseline KOOS values, DOC patients continued to have higher and clinically meaningful differences in KOOS subscale scores at 2 years compared with MOON cohort patients: pain (94 ± 10 vs 78 ± 33, respectively; P = .004), symptoms (89 ± 12 vs 72 ± 32, respectively; P < .001), activities of daily living (98 ± 5 vs 82 ± 34, respectively; P = .006), sports/recreation (85 6 18 vs 70 6 33, respectively; P < .001), and quality of life (76 ± 20 vs 64 ± 32, respectively; P = .072) (Figure 4). RTS rates were significantly higher in the DOC (72%) compared with the MOON cohort (63%) (P < .001).
Figure 4.
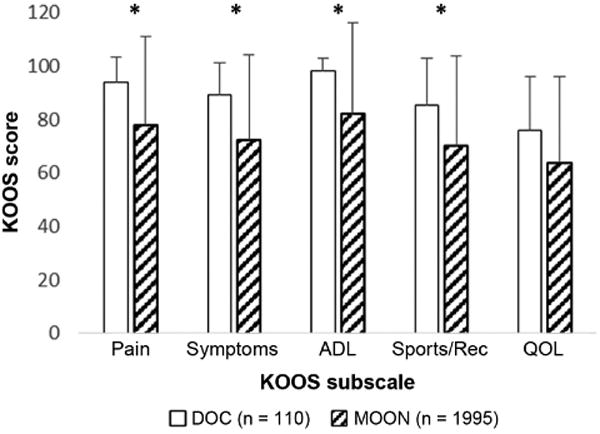
Knee injury and Osteoarthritis Outcome Score [KOOS] results by subscale at 2 years after anterior cruciate ligament reconstruction. *Statistically significant between-group difference (P < .05). ADL, activities of daily living; DOC, Delaware-Oslo ACL Cohort; MOON, Multicenter Orthopaedic Outcomes Network; QOL, quality of life; Sports/Rec, sports/recreation.
Discussion
The purpose of this study was to compare functional outcomes 2 years after ACLR in DOC patients who underwent additional progressive preoperative rehabilitation, including neuromuscular training, compared with the MOON cohort. The primary findings of this study are that the DOC patients had significantly higher and clinically meaningful patient-reported function and higher RTS rates 2 years after ACLR. Grindem and colleagues12 found that preoperative rehabilitation led to higher KOOS values 2 years after reconstruction compared with the patients in the NKLR; however, the NKLR's postoperative rehabilitation was not standardized. Conversely, the patients in the MOON cohort received specified postoperative care at facilities that were part of large orthopaedic and sports medicine research centers, which allowed for a more homogeneous comparison between cohorts. This study did not determine what the optimal preoperative rehabilitation program is, and it did not differentiate which aspect of a program is most important (ie, progressive strengthening, neuromuscular training), but it does suggest that giving patients additional rehabilitation beyond a quiet knee (full ROM and quadriceps activation, little to no pain, or joint effusion) before surgery may lead to meaningful improved outcomes 2 years after ACLR.
Preoperative IKDC scores were higher in the DOC and may have been related to differences in the timing of baseline testing between cohorts. Baseline testing may have occurred before impairment resolution in the MOON cohort; however, the MOON protocol called for impairments to be resolved before undergoing reconstruction.30 Both cohorts had to achieve minimum criteria before surgery, ensuring that neither cohort had substantial impairments going into reconstruction. Several studies have shown preoperative muscle performance maximization and ROM deficit minimization related to optimized postoperative outcomes.5,8,18,21 This is also consistent with previously published findings that preoperative outcome scores significantly predict postoperative outcome scores.26 Eitzen and Moksnes9 found that a 5-week preoperative program can lead to improved functional outcomes after ACLR. Our overall findings are consistent with both Eitzen et al8 and Grindem et al12 in that progressive preoperative rehabilitation is an important factor to maximize postoperative outcomes.
While each cohort used a different rehabilitation protocol for preoperative and postoperative rehabilitation, both protocols utilized a criterion-based approach. Criterion-based rehabilitation protocols utilizing tissue-healing time frames, factors associated with outcomes, and expert opinion are considered the most evidence-based protocols to our current knowledge. Both of the protocols used have been published and are considered standard of care after an ACL injury.1,30 The primary difference between the postoperative protocols is that the DOC protocol used primarily objective criteria and the MOON cohort used a mixture of objective and subjective criteria for program advancement. Patients in the DOC also underwent structured follow-up testing at 6 months and 1 year after ACLR, which may have benefited them in terms of progressing home exercise programs or providing counseling and/or consultation on current functional status. While differences between graft type and meniscal procedure proportions between cohorts also have the potential to influence outcome scores at 2 years, our analysis of graft type and meniscal procedure on IKDC scores suggests that differences in proportions of surgical variables between cohorts did not have an effect on the outcome scores.
The DOC patients had a significantly higher RTS rate 2 years after ACLR compared with the MOON cohort patients. The MOON cohort's RTS rate of 63% is consistent with the Ardern et al3 meta-analysis that reported that 65% returned to preinjury sports. The DOC's RTS rate of 72% exceeded both that of the MOON cohort and that reported by Ardern et al.3 Objective RTS criteria were used in both cohorts to determine individual readiness to return to sport among patients. There is currently no consensus on specific RTS criteria; however, the use of clinical, functional performance, and patient-reported outcome measures has been suggested as the current standards after ACLR.17 The DOC criteria used higher cutoff scores than the MOON criteria, which ensured higher symmetry between limbs before clearance for RTS. Functional performance symmetry restoration is needed to maximize patient-reported functional recovery19 and may also explain some of the variation in 2-year outcome scores between cohorts.
A limitation of our study is that comparing 2 separate cohorts does not allow for a true cause and effect evaluation of extended preoperative rehabilitation to postoperative outcomes. There were also some differences in the postoperative rehabilitation programs, graft types, and RTS criteria that may have affected the outcomes. The strengths of this study are the large sizes of the cohorts, the application of similar inclusion and exclusion criteria to both cohorts for a homogeneous comparison, and the use of criterion-based postoperative protocols. Future studies should use the randomized controlled trial study design to better assess the value of preoperative rehabilitation after an ACL rupture.
Conclusion
The cohort treated with preoperative rehabilitation consisting of progressive strengthening and neuromuscular training had higher functional outcomes and RTS rates compared with the benchmark cohort that also used a criterion-based postoperative rehabilitation program 2 years after ACLR. The standard of care in the United States is to achieve a quiet knee before undergoing reconstruction. While achieving a quiet knee before surgery may thwart surgical complications such as arthrofibrosis, it may not be enough to maximize functional outcomes even with rigorous postoperative rehabilitation. Progressive preoperative rehabilitation before ACLR should be considered as an addition to the standard of care to maximize functional outcomes after ACLR.
Supplementary Material
Acknowledgments
The authors thank the Norwegian Sports Medicine Clinic (http://www.nimi.no), the University of Delaware Physical Therapy Clinic (http://www.udptclinic.com), and the rehabilitation clinics affiliated with the MOON group (https://medschool.vanderbilt.edu/orthopaedics/moon-knee-project) for assistance in providing treatment and data collection of patients. The authors thank Ingrid Eitzen, Annika Storevold, Ida Svege, Håvard Moksnes, Espen Selboskar, Karin Rydevik, and Marte Lund for their role in data collection of the Norwegian arm. They also thank Andrew Lynch, Kathleen White, Airelle Giordano, Tara Manal, Angela Smith, and Martha Callahan for assistance with data collection, patient scheduling, and database management of the Delaware arm. The authors thank the following MOON group physicians, without whom the data utilized in this study would not exist. These members include Richard D. Parker, MD, Jack T. Andrish, MD, Morgan H. Jones, MD, MPH (Cleveland Clinic); Emily K. Reinke, PhD, Charles L. Cox, MD, MPH (Vanderbilt University School of Medicine); Christopher C. Kaeding, MD, David C. Flanigan, MD (The Ohio State University); Rick W. Wright, MD, Matthew J. Matava, MD, Robert H. Brophy, MD, Matthew V. Smith, MD (Washington University School of Medicine at Barnes-Jewish Hospital); Robert G. Marx, MD, MSc (Hospital for Special Surgery); Annunziato Amendola, MD (Duke University); Brian R. Wolf, MD, MS (University of Iowa); Eric C. McCarty, MD, Armando Vidal, MD, Michelle Wolcott, MD (University of Colorado School of Medicine); Warren R. Dunn, MD, MPH (University of Wisconsin). Finally, the authors thank all the physician and medical assistants, research coordinators, analysts, and support staff from the MOON sites, whose tireless efforts make the MOON consortium possible.
Footnotes
Presented at the 41st annual meeting of the AOSSM, Orlando, Florida, July 2015.
One or more of the authors has declared the following potential conflict of interest or source of funding: The Delaware-Oslo ACL Cohort was funded by grant number 5R37 HD 037985, and the MOON ACL cohort was partially funded by grant number 5R01 AR053684 (to K.P.S.) from the National Institutes of Health (NIH)/National Institute of Arthritis and Musculoskeletal and Skin Diseases. The project was also supported by the Vanderbilt Sports Medicine Research Fund. Vanderbilt Sports Medicine received unrestricted educational gifts from Smith & Nephew Endoscopy and DonJoy Orthopaedics. M.J.A. is a paid consultant for Smith & Nephew. L.E. is a paid consultant and receives royalties and research support from Arthrex Inc, receives research support from Biomet and Smith & Nephew, and has stock or stock options in iBalance. K.P.S. has received NIH funding as well as unrestricted educational gifts from Smith & Nephew Endoscopy and DonJoy Orthopaedics and is a paid consultant for Mitek and the Cytori-Scientific Advisory Board. L.S.-M. has received NIH funding.
References
- 1.Adams D. Current concepts for anterior cruciate ligament reconstruction: a criterion-based rehabilitation progression. J Orthop Sports Phys Ther. 2012;42(7):601–614. doi: 10.2519/jospt.2012.3871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anderson AF, Irrgang JJ, Kocher MS, Mann BJ, Harrast JJ. The International Knee Documentation Committee subjective knee evaluation form: normative data. Am J Sports Med. 2006;34(1):128–135. doi: 10.1177/0363546505280214. [DOI] [PubMed] [Google Scholar]
- 3.Ardern CL, Taylor NF, Feller JA, Webster KE. Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med. 2014;48(21):1543–1552. doi: 10.1136/bjsports-2013-093398. [DOI] [PubMed] [Google Scholar]
- 4.Daniel D, Stone M. Fate of the ACL-injured patient. Am J Sports Med. 1994;22(5):632–644. doi: 10.1177/036354659402200511. [DOI] [PubMed] [Google Scholar]
- 5.de Jong SN, van Caspel DR, van Haeff MJ, Saris DBF. Functional assessment and muscle strength before and after reconstruction of chronic anterior cruciate ligament lesions. Arthroscopy. 2007;23(1):21–28. 28.e1–28.e3. doi: 10.1016/j.arthro.2006.08.024. [DOI] [PubMed] [Google Scholar]
- 6.DiStasi S, Myer GD, Hewett TE. Neuromuscular training to target deficits associated with second anterior cruciate ligament injury. J Orthop Sports Phys Ther. 2013;43(11):777–792. A1–A11. doi: 10.2519/jospt.2013.4693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DiStasi SL, Snyder-Mackler L. The effects of neuromuscular training on the gait patterns of ACL-deficient men and women. Clin Biomech (Bristol Avon) 2012;27(4):360–365. doi: 10.1016/j.clinbiomech.2011.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eitzen I, Holm I, Risberg MA. Preoperative quadriceps strength is a significant predictor of knee function two years after anterior cruciate ligament reconstruction. Br J Sports Med. 2009;43(5):371–376. doi: 10.1136/bjsm.2008.057059. [DOI] [PubMed] [Google Scholar]
- 9.Eitzen I, Moksnes PH. A progressive 5-week exercise therapy program leads to significant improvement in knee function early after anterior cruciate ligament injury. J Orthop Sport Phys Ther. 2010;40(2):705–721. doi: 10.2519/jospt.2010.3345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. Br Med J. 2013;346:f232. doi: 10.1136/bmj.f232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gobbi A, Francisco R. Factors affecting return to sports after anterior cruciate ligament reconstruction with patellar tendon and hamstring graft: a prospective clinical investigation. Knee Surg Sports Traumatol Arthrosc. 2006;14(10):1021–1028. doi: 10.1007/s00167-006-0050-9. [DOI] [PubMed] [Google Scholar]
- 12.Grindem H, Granan LP, Risberg MA, Engebretsen L, Eitzen I. How does a combined preoperative and postoperative rehabilitation programme influence the outcome of ACL reconstruction 2 years after surgery? A comparison between patients in the Delaware-Oslo ACL Cohort and the Norwegian National Knee Ligament Registry. Br J Sports Med. 2014;49(6):385–389. doi: 10.1136/bjsports-2014-093891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hägglund M, Waldén M, Thomeé R. Should patients reach certain knee function benchmarks before anterior cruciate ligament reconstruction? Does intense “prehabilitation” before anterior cruciate ligament reconstruction influence outcome and return to sports? Br J Sports Med. 2015;49(22):1423–1424. doi: 10.1136/bjsports-2015-094791. [DOI] [PubMed] [Google Scholar]
- 14.Hartigan E, Axe MJ, Snyder-Mackler L. Perturbation training prior to ACL reconstruction improves gait asymmetries in non-copers. J Orthop Res. 2009;27(6):724–729. doi: 10.1002/jor.20754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hartigan EH, Zeni J, Di Stasi S, Axe MJ, Snyder-Mackler L. Preoperative predictors for noncopers to pass return to sports criteria after ACL reconstruction. J Appl Biomech. 2012;28(4):366–373. doi: 10.1123/jab.28.4.366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Irrgang JJ. Responsiveness of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2006;34(10):1567–1573. doi: 10.1177/0363546506288855. [DOI] [PubMed] [Google Scholar]
- 17.Logerstedt D, Arundale A, Lynch A. A conceptual framework for a sports knee injury performance profile (SKIPP) and return to activity criteria (RTAC) Braz J Phys Ther. 2015;19(5):340–359. doi: 10.1590/bjpt-rbf.2014.0116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Logerstedt D, Lynch A, Axe MJ, Snyder-Mackler L. Pre-operative quadriceps strength predicts IKDC 2000 scores 6 months after anterior cruciate ligament reconstruction. Knee. 2013;20(3):208–212. doi: 10.1016/j.knee.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Logerstedt D, Lynch A, Axe MJ, Snyder-Mackler L. Symmetry restoration and functional recovery before and after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(4):859–868. doi: 10.1007/s00167-012-1929-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Marx RG, Jones EC, Angel M, Wickiewicz TL, Warren RF. Beliefs and attitudes of members of the American Academy of Orthopaedic Surgeons regarding the treatment of anterior cruciate ligament injury. Arthroscopy. 2003;19(7):762–770. doi: 10.1016/s0749-8063(03)00398-0. [DOI] [PubMed] [Google Scholar]
- 21.Myer GD, Ford KR, Divine JG, Wall EJ, Kahanov L, Hewett TE. Longitudinal assessment of noncontact anterior cruciate ligament injury risk factors during maturation in a female athlete: a case report. J Athl Train. 2009;44(1):101–109. doi: 10.4085/1062-6050-44.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Myklebust G, Bahr R. Return to play guidelines after anterior cruciate ligament surgery. Br J Sports Med. 2005;39(3):127–131. doi: 10.1136/bjsm.2004.010900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roos EM, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis pilot study. Health Qual Life Outcomes. 2003;1:64. doi: 10.1186/1477-7525-1-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS): development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28(2):88–96. doi: 10.2519/jospt.1998.28.2.88. [DOI] [PubMed] [Google Scholar]
- 25.Shaarani SR, Hare CO, Quinn A, et al. Effect of prehabilitation on the outcome of anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41:2117–2127. doi: 10.1177/0363546513493594. [DOI] [PubMed] [Google Scholar]
- 26.Spindler KP, Huston LJ, Wright RW, et al. The prognosis and predictors of sports function and activity at minimum 6 years after anterior cruciate ligament reconstruction: a population cohort study. Am J Sports Med. 2011;39(2):348–359. doi: 10.1177/0363546510383481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spindler KP, Parker RD, Andrish JT, et al. Prognosis and predictors of ACLR using the MOON cohort: a model for comparative effectiveness studies. J Orthop Res. 2014;31(1):2–9. doi: 10.1002/jor.22201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spindler KP, Wright RW. Anterior cruciate ligament tear. N Engl J Med. 2008;359:2135–2142. doi: 10.1056/NEJMcp0804745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.White K, Di Stasi SL, Smith AH, Snyder-Mackler L. Anterior cruciate ligament- specialized post-operative return-to-sports (ACL-SPORTS) training: a randomized control trial. BMC Musculoskelet Disord. 2013;14(1):108. doi: 10.1186/1471-2474-14-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wright RW, Haas AK, Anderson J, et al. Anterior cruciate ligament reconstruction rehabilitation: MOON guidelines. Sports Health. 2015;7(3):239–243. doi: 10.1177/1941738113517855. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


