Abstract
Previous studies have indicated that schizophrenia is linked to abnormal lipid metabolism. Free fatty acids (FFAs) in peripheral blood can reflect the status of lipid metabolism in human body. The purpose of this study was to scan the FFA pattern and elucidate the characteristics of lipid metabolic abnormality in schizophrenia patients. One hundred and ten patients with schizophrenia (SCZs) and 109 healthy controls (HCs) were included in the study and divided into a discovery set and a validation set. Forty-seven serum FFAs were detected by UPLC-QTOF-MS and 39 of them were absolutely quantified by establishing standard curves. Monounsaturated fatty acids (MUFAs) and ω-6 polyunsaturated fatty acids (ω-6 PUFAs) were significantly increased in SCZs compared with HCs. Desaturation from saturated fatty acids to MUFAs and β-oxidation were enhanced, as estimated by the ratios of products to precursors. These results suggest that lipolysis and β-oxidation are upregulated in SCZ, presumably resulting from insufficient brain energy supply.
Introduction
Schizophrenia is a psychiatric disease associated with delusions, hallucinations, thought disorders and cognitive deficits.1 Schizophrenia affects approximately 0.5 to 1.0% of the population worldwide and is disastrous for affected individuals and their families. Schizophrenia is also a serious burden on the social healthcare system.1, 2 Unfortunately, our current understanding of schizophrenia remains limited.
Accumulating evidence indicates that schizophrenia is linked to abnormal lipid metabolism and related pathways in both the central and peripheral nervous systems. Prabakaran demonstrated that the lipid biosynthetic pathway was down-regulated in the brains of schizophrenia patients, whereas several fatty acid beta-oxidation enzymes were significantly increased.3 Free fatty acids (FFAs) and phosphatidylcholines were significantly changed in the prefrontal cortex (both gray matter and white matter) of schizophrenia patients.4 In 2013, another study showed a number of statistically significant changes in prefrontal cortex lipid concentrations, including changes in total lipids, phospholipids, triglycerides and cholesteryl esters, in schizophrenia patients compared with these concentrations in controls.5 This metabolic dysfunction is also reflected in the peripheral blood. Higher levels of serum triglycerides and lower levels of serum HDL have been detected in schizophrenia patients,6 and associations between serum triglycerides and positive psychotic symptoms and between polyunsaturated membrane fatty acids (PUFAs) in RBCs and negative symptoms have been demonstrated.7 We previously noted that fatty acids and ketone bodies were elevated in the serum or urine of schizophrenia patients, suggesting upregulated fatty acid catabolism.8
Compared with brain tissue, peripheral blood samples are more accessible and can be controlled to collect a medication-free group of samples that better reflects the disease state without the interference of antipsychotic drugs. Fasting plasma FFAs have been reported to be closely related to adipose tissue fatty acids,9 which might reflect the energy supply. A comprehensive scan of FFAs might facilitate the elucidation of the characteristic lipid metabonomics abnormality of schizophrenia and may contribute to a better understanding of this disease.
In many previous studies, the reported fatty acid profile was incomplete or lacked absolute quantification data. To better investigate the lipid metabolism dysfunction in schizophrenia patients, we enrolled 110 schizophrenia patients and 109 normal healthy subjects as controls, utilizing a UPLC-QTOF-MS platform to achieve targeted FFA quantitative analysis.
Materials and methods
Subjects
Our sample set was consistent with our previous research.8 We recruited 110 patients from the Anhui Province, China, diagnosed as schizophrenic (SCZ) according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Of the 110 patients, 63 were experiencing first-onset psychosis, and 47 were hospitalized for relapse after at least 1 month without any antipsychotic drugs. A total of 109 healthy controls (HC) were recruited in the same district and were matched for age, body mass index (BMI) and gender. In both the patient and control groups, we excluded participants with metabolic disorders (such as type I or type II diabetes) and/or with heavy consumption of alcohol. The enrolled subjects were separated into a discovery set (60 SCZ & 61 HC) and a validation set (50 SCZ & 48 HC; Supplementary Table 1).
Written informed consent was obtained from all participants. All samples were collected following the guidelines of the local ethics committee. The overall sampling was finished within 1 year.
Serum sample collection
Venous blood was collected in polypropylene tubes in the early morning after overnight fasting. The fresh blood samples were stored at room temperature and clotted naturally after approximately 2 h. Serum was then obtained after centrifugation at 10 000 r.p.m. for 10 min and immediately stored at −80 °C.
Reagents and instrumentation
Reference standards of FFAs (purity>90%) and deuterated internal standards (IS) were acquired from Sigma-Aldrich and NU-CHEK. HPLC-grade methanol, n-hexane, acetonitrile, and water were obtained from Merck.
A Waters ACQUITY ultraperformance LC system equipped with a binary solvent delivery manager and a sample manager (Waters, Milford, MA, USA) was used throughout the study. The mass spectrometer was a Waters XEVO TQ-S instrument with an ESI source (Waters, Milford, MA, USA). The entire LC−MS system was controlled by MassLynx 4.1 software. All chromatographic separations were performed with an ACQUITY BEH C18 column (1.7 μm, 100 mm × 2.1 mm internal dimensions; Waters, Milford, MA, USA).
Serum specimen preparation
A 30-μl aliquot of serum sample was extracted for UPLC-QTOF-MS analysis. Each sample was spiked with the internal standard (10 μl of C19:0-d37) and added to 500 μl of a mixture of isopropanol/n-hexane/2 M phosphoric acid (40:10:1, v/v/v). The resulting samples were vortexed for 2 min and incubated at room temperature for 20 min. After the incubation, 400 μl of n-hexane and 300 μl of water were added, and the mixtures were vortexed for 2 min and centrifuged at 12 000 r.p.m., 4 °C for 5 min. An aliquot of 400 μl of supernatant was collected and transferred into a clean tube. The remaining mixture was further extracted with additional 400 μl of n-hexane by vortexing and centrifuging at 12 000 r.p.m., 4 °C for 5 min, after which the second 400 μl of supernatant was collected. The two supernatants were pooled together and vacuum-dried at room temperature. The residue was re-dissolved in 80 μl of methanol.10, 11 After centrifugation, the supernatant was used for UPLC−QTOF-MS analysis (Waters, Manchester, UK).
UPLC-QTOF-MS spectral acquisition
A 5- μl aliquot of the sample was injected into an ACQUITY BEH C18 column with the column temperature set at 40 °C. The elution solvents were water (A) and acetonitrile/isopropyl (v/v=80/20, B) with a flow rate of 400 μl/min. The elution gradient was as follows: 0−2 min (70% B), 2−5 min (75% B), 5−10 min (80% B), 13−16 min (90% B), and 16−24 min (99% B). Samples from healthy controls and schizophrenic individuals were alternately injected. In addition to the internal standard, a blank vial and a mixture of all the samples were prepared and run after every 10 serum samples for quality control.
The mass spectrometer was operated in negative ion mode with the following optimal conditions: capillary voltage 2.5 kV, cone voltage 55 V, and extractor voltage 4 V. The desolvation and cone gas flow rates were 650 and 50 l h−1, respectively. The source temperature was 120 °C, and the temperature for the desolvation gas was set at 450 °C. MassLynx software (Waters, Manchester, UK) was used to collect the data with a mass range of 50 to 1000 Da. The scan time was set to 0.35 s, and the interscan delay was set to 0.02 s. Leucine (encephalin) was used as the lock mass (m/z=554.2615).
Data processing
The UPLC-QTOF-MS raw data were analyzed by the MarkerLynx applications (manager version 4.1). A list of the ion intensities of each detected peak was generated using the RT and m/z data pairs as the identifier for each ion. The resulting three-dimensional matrix contained arbitrarily assigned peak indices (retention time–m/z pairs), sample names (observations), and ion intensity information (variables). The missing values were imputed with 50. The internal standard and QC were used for data quality control (reproducibility), and the QC was used for data normalization. The ion peaks generated by the internal standard were removed.
To obtain more information, we conducted the statistical analysis based on the relative quantitative data and also presented the absolute quantitative values for reference.
Statistical analysis
All data analyses were performed using SIMCA-P 11.5 (Umetrics, Umea, Sweden) and R 3.2.1 software (Stanford University, Stanford, CA, USA). The well-matched discovery set and the validation set both followed the procedure for basic analysis. The Shapiro-Wilk normality test was performed first to evaluate the normality of our data. Then, the Mann−Whitney U-test was chosen to investigate differences between the SCZ and HC in FFA measurements. The resultant P-values for all FFAs were subsequently adjusted to account for multiple testing by the Benjamin–Hochberg method. We regarded P-values of <0.05 as significant. For multivariable analysis, PLS-DA was conducted, and we obtained the VIP (variable importance for the projection) values.
According to the fatty acid metabolism pathways, we analyzed 18 pairs of interconverted FFAs. A Mann−Whitney U-test was used to evaluate the differences in the product/substrate ratios between SCZ and HC. P-values were also adjusted by the Benjamin–Hochberg method. Geometric averages were used in the progress.
Pearson correlation analysis was performed to evaluate the interactions between the FFAs and age, gender and BMI, as well as the correlations between mutual transformed FFAs.
Results
Demographic characteristics
The study included 110 patients with schizophrenia and 109 healthy controls, consistent with our previous work.8 We selected 60 patients and 61 healthy controls matched by age, gender and BMI before statistical analysis as the discovery set, and the remaining subjects composed the validation set (Supplementary Table 1).
Univariate analysis of 47 free fatty acids
Forty-seven FFAs were detected by UPLC-QTOF-MS, as shown in Table 1, and were classified into 8 types: saturated fatty acids (SFAs), monounsaturated fatty acids (MUFAs), ω-6 polyunsaturated fatty acids (ω-6 PUFAs), ω-3 polyunsaturated fatty acids (ω-3 PUFAs), trans-fatty acids (TFAs), branched-chain fatty acids (BCFAs), odd-carbon fatty acids (OCFAs) and others. The first four types participate in the metabolism of fatty acids in the human body. We refer to these FFAs as the FFAs of most concern, and a total of 26 FFAs belonging to the first four types were detected.
Table 1. Forty-seven FFAs detected by UPLC-QTOF-MS and analyzed by PLS-DA and the Mann−Whitney U-test.
| FFA | Retention time (RT) | VIPa | P-valueb | FCc |
|---|---|---|---|---|
| SFAs | ||||
| C8.0 | 0.98 | 0.54 | 0.9406 | 1.03 |
| C12.0 | 2.52 | 1.05 | 0.1853 | −1.18 |
| C14.0 | 4.52 | 0.83 | 0.0795 | 1.14 |
| C16.0 | 7.31 | 0.92 | 0.008 | 1.49 |
| C18.0 | 10.92 | 0.98 | 0.173 | 1.15 |
| C20.0 | 13.7 | 1.24 | 0.4199 | 1.1 |
| C22.0 | 15.36 | 0.83 | 0.6836 | −1.14 |
| C24.0 | 16.52 | 1.02 | 0.0181 | −1.22 |
| MUFAs | ||||
| C12.1.cis.11 | 1.73 | 0.8 | 0.5958 | 1.25 |
| C14.1.cis.9 | 2.84 | 1.14 | 0.0034 | 2.25 |
| C16.1.cis.9 | 4.88 | 1.32 | 9.23E−06 | 2.67 |
| C18.1.cis.9 | 7.68 | 0.97 | 0.001 | 1.67 |
| C20.1.cis.11 | 11.12 | 1.33 | 7.97E−08 | 3.18 |
| C22.1.cis.13 | 13.7 | 1.5 | 7.97E−08 | 3.7 |
| C24.1.cis.15 | 15.27 | 1.77 | 2.05E−08 | 1.88 |
| ω-6 PUFAs | ||||
| C18.2.cis.9.12 | 5.49 | 0.59 | 0.2364 | 1.34 |
| C20.2.cis.11.14 | 8.27 | 0.95 | 0.007 | 1.61 |
| C20.3.cis.8.11.14 | 6.25 | 0.92 | 0.0131 | 1.34 |
| C20.4.cis.5.8.11.14 | 5.07 | 1.53 | 0.0038 | 1.4 |
| C22.2.cis.13.16 | 11.67 | 1.1 | 0.0046 | 2.11 |
| C22.4.cis.7.10.13.16 | 7.15 | 0.92 | 0.0351 | 1.47 |
| C22.5.cis.4.7.10.13.16 | 6.13 | 1.12 | 0.6627 | 1.14 |
| ω-3 PUFAs | ||||
| C20.5.cis.5.8.11.14.17 | 3.67 | 0.84 | 0.6709 | 1.15 |
| C22.3.cis.13.16.19 | 9.29 | 0.9 | 1 | −1.01 |
| C22.5.cis.7.10.13.16.19 | 5.41 | 1.02 | 0.0204 | 1.5 |
| C22.6.cis.4.7.10.13.16.19 | 4.57 | 1.09 | 0.9856 | 1.06 |
| TFAs | ||||
| C14.1.trans.9 | 3.13 | 1.18 | 0.4026 | 1.34 |
| C16.1.trans.9 | 5.22 | 0.4 | 0.9511 | 1.21 |
| C18.2.trans.9.12 | 6.19 | 0.87 | 0.4199 | 1.09 |
| BCFAs | ||||
| C14.0.iso | 4.23 | 1.19 | 0.4026 | −1.1 |
| C16.0.iso | 6.9 | 0.88 | 0.9511 | −1.05 |
| C18.0.iso | 10.42 | 0.77 | 0.571 | 1.09 |
| OCFAs | ||||
| C15.0.iso | 5.38 | 0.62 | 0.975 | −1.54 |
| C15.0 | 5.82 | 0.67 | 0.9018 | −1.89 |
| C17.1.cis.10 | 6.19 | 0.96 | 0.0012 | 1.86 |
| C17.0.iso | 9.04 | 0.78 | 0.8718 | 1.02 |
| C17.0 | 8.41 | 1.08 | 0.1955 | 1.11 |
| C19.2.cis.10.13 | 6.83 | 0.79 | 0.1062 | 1.22 |
| C19.1.cis.10 | 9.36 | 0.8 | 0.0087 | 2.65 |
| C19.0 | 12.52 | 0.98 | 0.4199 | 1.07 |
| C21.1.cis.12 | 12.6 | 1 | 0.3891 | 1.12 |
| C21.0 | 14.62 | 0.54 | 0.975 | −1.14 |
| C23.1.cis.14 | 14.24 | 0.29 | 0.8586 | 1.02 |
| C23.0 | 15.96 | 1.19 | 0.2436 | −1.18 |
| Others | ||||
| C18.2.CLA | 5.8 | 1.08 | 0.9406 | 1.54 |
| C16.1.unknown | 5.02 | 0.7 | 0.2106 | 1.6 |
| C18.3.unknown | 4.15 | 1.12 | 0.9406 | 1.14 |
Abbreviations: FFA, free fatty acid; MUFA, monounsaturated fatty acid; PUFA, polyunsaturated fatty acids; SFA, saturated fatty acid.
Variable importance in the projection (VIP) was obtained from PLS-DA. The black bold values indicate VIP>1.
P-values are calculated from the nonparametric Mann−Whitney U-test. The black bold values indicate P<0.05
Fold changes (FCs) were calculated from the intra-group means of FFAs, with a positive value indicating a relatively higher concentration in SCZ and a negative value indicating a relatively lower concentration compared to concentration in the healthy controls. The black bold numbers indicate that the absolute value of the FC is >1.5.
All detected FFAs deviated from normality according to the Shapiro-Wilk test, and we therefore applied the Mann-Whitney U-test to compare the 47 FFAs between SCZ and HC. Sixteen FFAs differed significantly (adjusted P-values <0.05; Table 1) between SCZ and HC in the discovery set. Fifteen FFAs were significantly increased in SCZ, with changes ranging from 1.34- to 3.7-fold, and only one (C24:0) was decreased, with a change of 1.22-fold. All differential FFAs were verified in the validation set (Supplementary table 2).
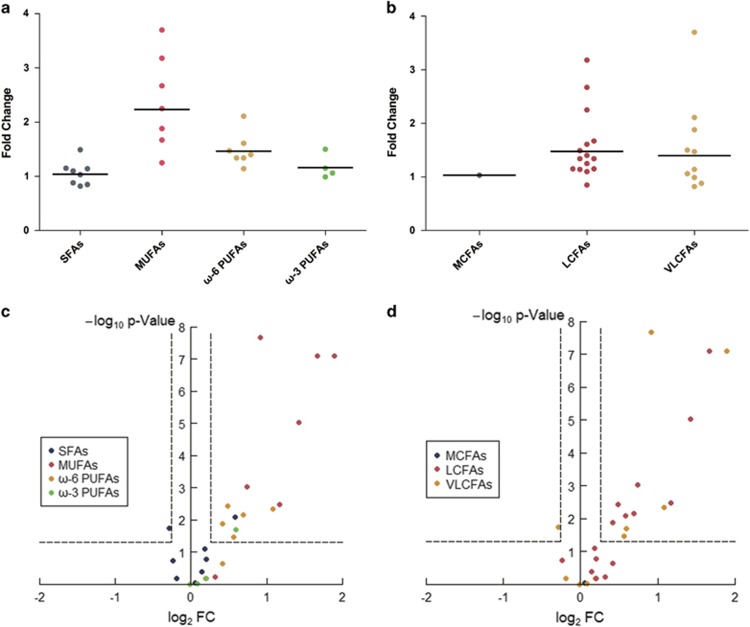
As noted previously, the 26 FFAs of most concern included the following four groups according to saturation: 8 SFAs, 7 MUFAs, 7 ω-6 PUFAs and 4 ω-3 PUFAs. Among the 8 SFAs, one was significantly increased (C16:0, FC=1.49), and one was significantly decreased (C24:0, FC=-1.22). All 7 MUFAs were elevated in SCZ (FC>1.2), 6 significantly. C22:1(cis.13), C20:1(cis.11), C16:1(cis.9) and C14:1(cis.9) had the top four fold changes (FCs) of 3.7, 3.18, 2.67 and 2.25, respectively. The geometric mean of the FCs of the 7 MUFAs of most concern was 2.234 (Figure 1a). Five of the 7 ω-6 PUFAs were significantly increased in SCZ compared with their levels in HC, with a geometric mean of the FCs of 1.46. By contrast, only one of the four ω-3 PUFAs (C22:5) showed a significant increase, with a geometric mean of the FC of 1.16.
Figure 1.
(a) Fold changes (FCs) of the 26 free fatty acids (FFAs) of most concern grouped by saturation. The horizontal lines present the geometric mean of each group. (b) FCs of the 26 FFAs of most concern grouped by carbon number. The horizontal lines present the geometric mean of each group. (c) Volcano plot of the 26 FFAs of most concern colored by saturation. (d) Volcano plot of the 26 FFAs of most concern colored by carbon number.
With respect to carbon (C) chain-length, the 26 FFAs of most concern were classified into the following three groups: medium-chain fatty acids (MCFAs), long-chain fatty acids (LCFAs) and very long-chain FAs (VLCFAs). The only MCFA of most concern, octanoic acid, did not differ between SCZ and HC. Fifteen LCFAs of most concern were detected, and 8 were significantly increased in SCZ, with FCs ranging from 1.34 to 3.18. C20:1(cis.11), C16:1(cis.9), and C14:1(cis.9) had FC values of 3.18, 2.67 and 2.25, respectively. The geometric mean of the FCs of the 15 LCFAs of most concern was 1.475 (Figure 1b). Of the 10 VLCFAs of most concern detected in our study, 5 were significantly increased in SCZ, with FCs ranging from 1.47 to 3.7. C22:1(cis.13) and C22:2(cis.13, 16) had FC values of 3.7 and 2.11, respectively. C24:0 was the only one that decreased significantly in SCZ (Table 1). The geometric mean of the FCs of the 10 VLCFAs of most concern was 1.395 (Figure 1b).
In addition to the 26 FFAs of most concern, twelve odd-carbon FAs were detected in the study. C17:1(cis.10) and C19:1(cis.10) were increased significantly in SCZ. The elevation of the contents of these FAs was verified in the validation set (Supplementary Table 2).
Multivariate analysis of 47 free fatty acids
The PLS-DA score plot showed a good separation between SCZ and HC corresponding to the first 3 PLS-DA components (Supplementary Figure 1). The explained variation in X (R2X) was 60.1%, while the explained variation in Y (R2Y) was 61.5%. A permutation test with a permutation number of 200 was also performed to test the overfitting status of the model (Supplementary Figure 2), which indicated the success of the model for differentiating SCZ from HC.
The VIP scores of the 47 FFAs are listed in Table 1. The top five VIP scores were C24:1(cis.15), C20:4(cis.5.8.11.14), C22:1(cis.13), C20:1(cis.11), and C16:1(cis.9), which all belong to the unsaturated FFA group.
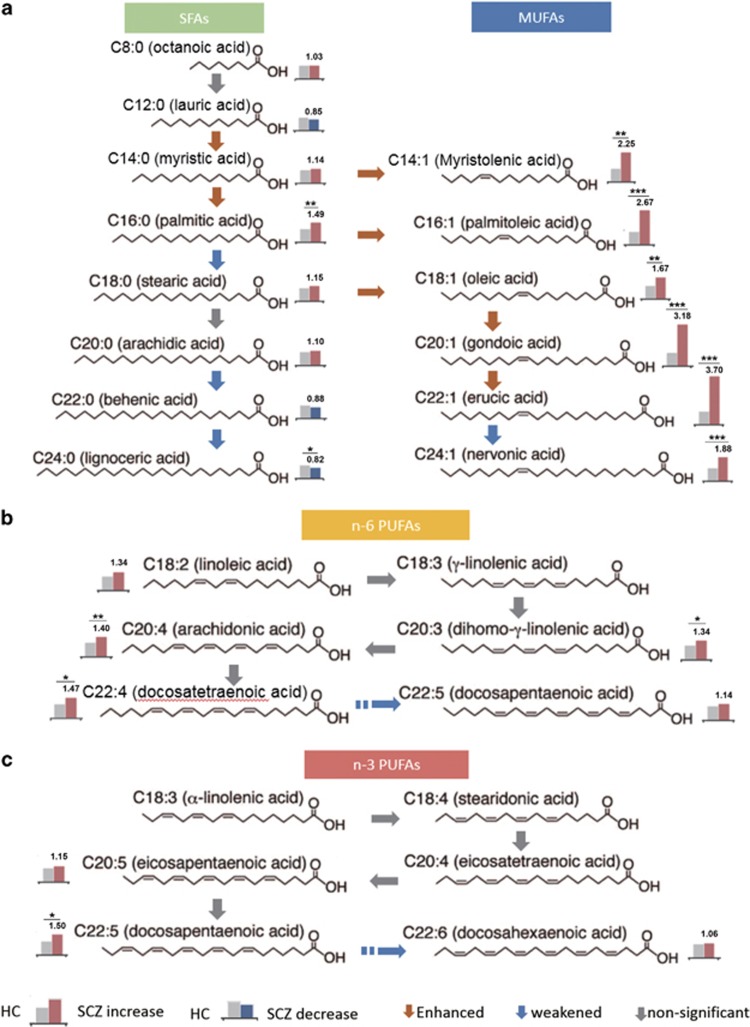
Fatty acid metabolic pathway analysis based on the product/precursor ratio
To further explore the changes in FFAs in SCZ patients, we investigated the ratios of product to precursor that were transformed unidirectionally or bidirectionally. There were 18 pairs of transformations among the 47 FFAs we detected (Figure 2). The ratios of product to precursor in HC and SCZ were calculated. Analysis using the Mann-Whitney test followed by Benjamin–Hochberg adjustment indicated that the ratios of 14 pairs of FFAs differed significantly between the two groups (Figure 2 and Supplementary Table 3). These results demonstrate that the regulation of FFA equilibrium differs between SCZ and HC.
Figure 2.
Fatty acid (FA) elongation pathways differ between schizophrenia patients (SCZ) and healthy controls (HC). The FA elongation pathways of SFAs, MUFAs, n-3 PUFAs and n-6 PUFAs are illustrated. The histograms present the relative concentration of each free fatty acid (FFA) in HC (left) and SCZ (right, normalized by HC). Red histograms indicate increases in SCZ, whereas blue indicates decreases. The figure above the histogram is the fold change (FC), and asterisks indicate significance. The red arrows indicate a significant increase in the ratio of product: substrate, which was deduced to be enhanced in this direction. The blue arrows are the opposite and indicate ratios that were deduced to be weakened. The gray arrows indicate no statistical significance. a) The FA elongation pathways of SFAs and MUFAs. b) The FA elongation pathways of ω-6 PUFAs. c) The FA elongation pathways of ω-3 PUFAs.
Δ9-Desaturase catalyzes the one-way reaction from SFAs to MUFAs, including C14:0 to C14:1, C16:0 to C16:1 and C18:0 to C18:1, and these reactions were enhanced in SCZ according to our data (Supplementary Table 3). As an example, the correlation coefficient for C18:0 and C18:1 was 0.32 in HC and 0.69 in SCZ. The geometric average of the ratio of C18:1/C18:0 was 0.72 in HC and increased significantly to 0.99 in SCZ. Similar phenomena were observed for C14:0/C14:1 and C16:0/C16:1. These results are consistent with the general increase in the MUFAs we mentioned previously. Therefore, our data support an enhanced tendency of desaturation from SFAs to MUFAs as one of the characteristics of serum FFAs in schizophrenia patients.
With respect to carbon number, C16:0 and C22:1 (cis.13) accumulated among SFAs and MUFAs, respectively. Elongation from C12:0 to C14:0 and from C14:0 to C16:0 was enhanced. In addition, β-oxidation from C24:0 to C22:0, from C22:0 to C20:0 and from C18:0 to C16:0 was increased in SCZ. Both of these phenomena were reflected in the trend to produce more C16:0. Among MUFAs, the ratios of product to precursor indicated a tendency to accumulate C22:1 (cis.13) (Figure 2 and Supplementary Table 3).
Absolute quantitation of 39 FFAs in serum from schizophrenia patients and healthy controls
We performed absolute quantitation of 39 FFAs using standard curves according to a method described previously.11, 12
The concentrations of the 39 FFAs are presented in μg/ml (Supplementary Table 4). The most abundant classes of FFAs in SCZ were MUFAs, SFAs and ω-6 PUFAs, accounting for 98.6% of all quantitated FFAs (Supplementary figure 3). In HC, these three classes were also the most abundant, accounting for 97.7% of the total FFAs, whereas SFAs were greater than MUFAs and came first. With respect to individual fatty acids, the most highly concentrated FFAs were C18:1, C18:2(ω-6) and C16:0. The pattern of FFAs in human bodies presented in our research is consistent with the work of other groups but depends on the technology platform.13
We computed the coefficients of variation (CVs) of the concentration data. Ninety-seven percent of FFAs (38/39) in SCZ and 95% (37/39) in HC in the discovery set had CV values of <15%, while in the validation set, there were 87% FFAs with CV<15% both in SCZ and HC group, indicating that the content of FFAs was relatively stable for all individuals with the same health status.
Discussion
Schizophrenia, a mental disease that affects approximately 30 million people globally, has devastating consequences for patients and their families.1 Accumulating evidence indicates that abnormal lipid metabolism is the main characteristic of schizophrenia and may contribute to its pathology.
Previous studies generally focused on ω-3 and ω-6 PUFAs in samples of patients with schizophrenia. In the present study, we were able to compare the concentrations of not only the ω-3 and ω-6 PUFA series but also MUFAs, SFAs, TFAs, BCFAs, and OCFAs in the serum of patients experiencing their first episodes or drug-free schizophrenia with those of matched control subjects. Moreover, we estimated the endogenous metabolic enzyme activities, as well as changes in metabolic progress.
Factors influencing alterations of the free fatty acid pattern in schizophrenia patients
Changes in the lipid metabolic process
FFAs can be used for fat synthesis or as fuel through β-oxidation. Previous studies have provided converging evidence for an insufficient energy supply in schizophrenia patients and elevated lipolysis and β-oxidation as compensatory mechanisms.3, 8
We observed significant accumulation of 13 even-carbon FFAs, whereas only one even-carbon FFA decreased significantly (Table 1, Figure 1). The activities of lipid metabolic enzymes can be estimated using indices based on product to precursor fatty acid ratios.13, 14 Fasting plasma FFAs are closely correlated with adipose tissue.9 The ratios of FFAs may reflect the desaturase activity in adipose tissue. By comparing the ratios of products to precursors between patients and controls, we determined that β-oxidation prevailed from C24:0 to C16:0 and from C24:1 to C22:1 (Figure 2, blue arrows indicate statistical significance). This result provides evidence in the level of free fatty acid of the hypothesis that lipid mobilization and β-oxidation are enhanced to provide more energy in schizophrenia patients.
The activities of the delta-9 and delta-5 desaturases were also estimated using the product to precursor fatty acid ratios. Delta-9 activity was estimated from the ratios of 16:1/16:0 and 18:1/18:0.15, 16 In the present study, delta-9 activity was significantly enhanced in SCZ compared with its activity in HC, with P-values of 1.2684E−07 and 0.0037 for 16:1/16:0 and 18:1/18:0, respectively (Figure 2a). Delta-5 desaturase activity is reflected by the 20:4/20:3 ratio.13, 15, 17 The desaturation progress catalyzed by delta-5 (20:4/20:3(ω-6) and 20:5/20:4(ω-6)) did not differ appreciably between SCZ and HC in the present study (Figures 2b and c).
Since using metabolite ratios to estimate biochemical equilibrium status or metabolic enzyme activity is numerical and indirect, direct measurement of the characteristics of related enzymes participating in lipid metabolism in schizophrenia patients is highly encouraged in future studies.
Higher levels of oxidative stress
The increased production of ROS and/or decreased occurrence of antioxidant protection indicates that oxidative stress is involved in the pathophysiology of schizophrenia.18 Increased oxidative stress in schizophrenia patients has been observed in the central nervous system3, 18, 19 and peripheral blood.20, 21 Many factors can cause an imbalance of ROS and antioxidants.
Enhanced β-oxidation can increase ROS and oxidative stress significantly.14 As mentioned above, our findings suggest increased lipid mobilization and β-oxidation. The elevated levels of FFAs may be a factor causing oxidative stress.
PUFAs, the main material of membranes, are vulnerable to damage by free radicals due to their double-bond structure. This process is called lipid peroxidation and damages cell membrane fluidity and permeability, signal transduction and mitochondrial function.22, 23
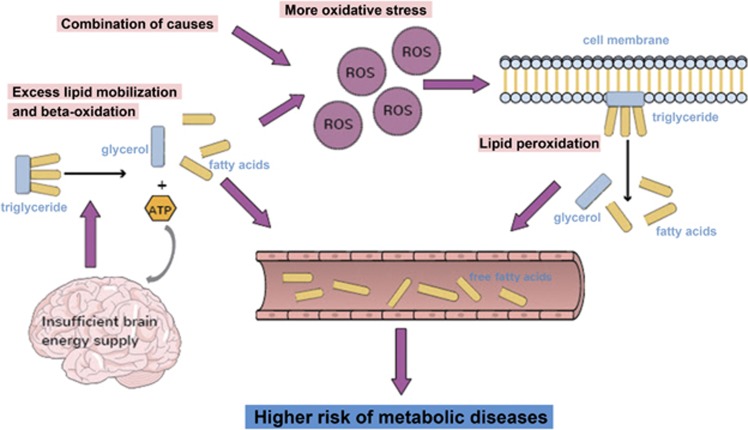
Membrane PUFAs are significantly decreased in both the central nervous system and RBCs of patients with schizophrenia.24, 25 There may be some links between plasma or serum FFA abnormalities and changes in membrane fatty acids in schizophrenia patients. Therefore, we hypothesize that in schizophrenia patients, the brain energy supply is insufficient for certain reasons, such as mitochondrial dysfunction. Hence, body lipids and fatty acids are mobilized to compensate for the brain energy shortage, resulting in elevated serum FFAs. Lipid peroxidation damages the membrane lipids, releasing free PUFAs into the plasma and further elevating plasma free PUFA levels. Simultaneously, enhanced β-oxidation during the process of energy production of fatty acids increases ROS in the body, aggravating the oxidative stress in schizophrenia patients.14 Consequently, more free FFAs, such as PUFAs, are derived from the lipid peroxidation progress, further increasing the FFA levels in the blood of patients (Figure 3). Further research is needed to verify this hypothesis.
Figure 3.
The systemic alterations resulting in the changes in free fatty acids (FFA) patterns in schizophrenia patients. Insufficient energy supply in the brains of schizophrenia patients causes excess lipolysis and β-oxidation, accompanied by FFA and ROS accumulation. Additional oxidative stress caused by active β-oxidation and other factors results in lipid peroxidation, causing loss of polyunsaturated fatty acids (PUFAs) from the lipid membrane. The increased FFAs increase the risk of metabolic diseases such as cardiovascular diseases and type II diabetes in schizophrenia patients.
Adverse FFA patterns for health
Schizophrenia is a complex multi-pathogenic disease closely related to metabolic disorders. The morbidities of metabolic syndrome, obesity, type II diabetes and cardiovascular disease are higher in subjects with schizophrenia than in healthy controls.26 Although no metabolic disorders were observed in either SCZ or HC in our samples, the FFA pattern suggests a high risk of metabolic disorders in SCZ.
Cardiovascular disease is the main cause of increased mortality in patients with schizophrenia.27, 28 ω-3 and ω-6 PUFAs share the same desaturases and elongases. Many studies have indicated that ω-3 PUFAs play an important role in the nervous and cardiovascular systems.29, 30 The ratio of ω-6/ω-3 PUFAs can be used as a health balance index, and the lower ratio the better, especially for cardiovascular disease.31
It is noteworthy that the ω-3 PUFAs in the present study were less elevated (geometric mean of the FCs=1.16) than the ω-6 PUFAs (geometric mean of the FCs=1.46) in the discovery set. The geometric means of the FCs in the validation set were 1.34 and 1.51, respectively. The higher ratio of ω-6/ω-3 in the schizophrenia group can be deduced from the results, which indicates the higher risk of cardiovascular disease.
The link between schizophrenia and diabetes has been known for over a century.32 The prevalence of diabetes in schizophrenia patients ranges from 10 to 15%, 2- to 3-fold higher than in the general population.33 Antipsychotics increase metabolic risks, but antipsychotic-naïve patients also have a higher risk of developing diabetes. Impaired glucose tolerance, hyperglycemia, and insulin resistance has been reported in first-episode drug-free schizophrenia patients.34, 35, 36, 37, 38 Although several factors including genetic susceptibility, unhealthy lifestyles and neuroendocrine dysregulation are involved in the association between schizophrenia and diabetes, the etiology of the high comorbidity rate remains obscure.32 Numerous studies have reported that high plasma (or serum) FFAs are involved in the etiology of type II diabetes mellitus. Elevated plasma FFAs in humans result in reduced insulin sensitivity throughout the entire body, increased insulin secretion and β-cell compensation.39 Glucose transport (GLUT-4) is inhibited by elevated plasma FFAs, and this inhibition is followed by a reduction in the rate of glucose oxidation.40, 41 Among major human FFA, palmitic acid (C16:0) is particularly notable as a major culprit of type II diabetes.42, 43, 44, 45 Palmitate inhibits the insulin-stimulated phosphorylation of key insulin signaling molecules and facilitates their ubiquitination.46
We observed that 13 even-carbon FFAs were increased in SCZ, including palmitic acid (C16:0). In SCZ serum, the concentrations of C16:0 were much higher, 276.41 μg/ml and 266.24 μg/ml in the discovery and validation sets, respectively, than in HC serum, which exhibited values of 117.80 μg/ml and 115.48 μg/ml, respectively (Supplementary Table 4). The considerable difference in C16:0 between SCZ and HC may indicate a high risk of type II diabetes in the SCZ group.
Obesity is closely correlated with diabetes. High levels of FFAs are a characteristic of obesity.47 A significant and positive correlation between delta-9 desaturase and markers of obesity has been reported.15 The estimated elevated delta-9 desaturase activity implies that schizophrenia patients are more likely to be obese.
Thus, a vicious cycle appears to occur: energy metabolic dysfunction in schizophrenia patients and oxidative stress cause elevated FFAs, which in turn, induce high risks of cardiovascular disease, diabetes and other metabolic diseases. Drugs that can alleviate the vicious FFA pattern in schizophrenia patients would be beneficial and could be used as auxiliary treatment for schizophrenia.
TFCs, BCFAs and OCFAs in serum
Trans-fatty acids and BCFAs cannot be synthesized in humans and are obtained from food. We did not observe differences in TFAs or BCFAs between SCZ and HC, implying that there is no considerable difference in diet between the two groups.
Twelve odd-numbered carbon fatty acids were detected in this study, and two of them, C17:1 and C19:1, were significantly increased in patients. Odd-numbered carbon fatty acids have received little attention due to their indigestibility in humans and technique limitations.
Odd-numbered carbon fatty acids usually exist in bacteria, fungi, poriferans, plants and animals, with various types in different species. Bacteria usually contain odd-numbered fatty acids in general, most often C15, C17 or C19.48 Many recent studies have suggested that microorganisms in the human body can affect the mental state. The relationship between gut microbiota and brain disease is attracting increasing attention.49, 50 The differences in the odd-numbered carbon FFA contents in serum observed in this study may imply the disturbance of gut microbiota in schizophrenia patients. To further investigate the potential association, research at the genome and metabolome levels is needed.
Strengths and limitations
In this study, we tried to mediate medication effects on our results by recruiting first-onset drug-naïve patients and patients without any antipsychotic drugs for at least 1 month. UPLC-QTOF-MS platform was employed to achieve a comprehensive scan of serum free fatty acids of our samples. As many as 47 fatty acids were relatively quantified and 39 were absolutely quantified. This quantitative scale is impressive and provides considerable information on FFA profiles. Alterations of FFA levels in schizophrenia reflect the abnormalities of energy metabolism in patients. Analysis of FFA patterns and products-precursors ratios helped to draw our attention to the lipolysis, β-oxidation and desaturation process, and guide our follow-up researches on other molecular levels, such as related proteins or genes.
This study also has limitations. Generally speaking, there are two sources of free fatty acids in human body: dietary intake and lipolysis from triglyceride. Since no survey has been conducted on detailed eating habits of participants, we can’t remove possible confounding effects of food intake when interpreting our results. However, whether schizophrenia patients have dietary bias remains controversial. A series of literature on schizophrenic eating habits describes that patients have preference in unhealthy diet.51, 52, 53 Another work discovers that individuals with schizophrenia and healthy controls seem to apply preference ratings to food in a similar manner.54 In addition, we have tried to mediate the impact of eating habit on our results in the following ways: (1) The residence of our participants were limited to Wuhu, Anhui to minimize regional differences in diet structure. (2) BMIs were matched between schizophrenia patients and healthy controls, and none of the participants had metabolic disorders. (3) Fasting blood was collected to avoid the disturbance of short-term food intake. Another limitation in this study is that we estimated biochemical equilibrium status or metabolic enzyme activity by using indices based on product to precursor fatty acid ratios. Direct measurement of the characteristics of related enzymes especially in lipolysis, desaturation and β-oxidation progress is necessary in the future.
Metabonomics reflects a resultant status of the body from a combined influence of genes and environment. Different genetic background in other populations may modify individual metabonomics and there is no systematic study of free fatty acids in other population till now. Thus, genetic factors should be considered when exploring such signatures in other population.
We used UPLC-QTOF-MS to characterize the serum fatty acid pattern in schizophrenia patients. Forty-seven FFAs were detected and relatively quantitatively analyzed, and 39 of these FFAs were absolutely quantitated by establishing standard curves. Sixteen of the 47 detected FFAs were significantly different in patients with schizophrenia and healthy controls. With the exception of the very long-chain fatty acid C24:0, these significantly different FFAs were all increased in schizophrenia serum. Desaturation from SFAs to MUFAs and β-oxidation, particularly in the endoplasmic reticulum, were enhanced, as estimated by the ratios of products to precursors. These results suggest upregulated lipolysis and β-oxidation in SCZ, presumably resulting from insufficient brain energy supply. Drugs that can alleviate the vicious FFA pattern in schizophrenia patients would be beneficial and could be used as auxiliary treatment for schizophrenia.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (81271486, 81421061), Ministry of Science and Technology of China (2016YFC1306802, 2016YFC1306900), the Program for NSFC International (Regional) Cooperation and Exchange (81361120389), Grants of Shanghai Brain-Intelligence Project from STCSM(16JC1420500).
Footnotes
Supplementary Information accompanies the paper on the Translational Psychiatry website (http://www.nature.com/tp)
The authors declare no conflict of interest.
Supplementary Material
References
- Ross CA, Margolis RL, Reading SA, Pletnikov M, Coyle JT. Neurobiology of schizophrenia. Neuron 2006; 52: 139–153. [DOI] [PubMed] [Google Scholar]
- Freedman R. Schizophrenia. N Engl J Med 2003; 349: 1738–1749. [DOI] [PubMed] [Google Scholar]
- Prabakaran S, Swatton JE, Ryan MM, Huffaker SJ, Huang JT, Griffin JL et al. Mitochondrial dysfunction in schizophrenia: evidence for compromised brain metabolism and oxidative stress. Mol Psychiatry 2004; 9: 643. [DOI] [PubMed] [Google Scholar]
- Schwarz E, Prabakaran S, Whitfield P, Major H, Leweke FM, Koethe D et al. High throughput lipidomic profiling of schizophrenia and bipolar disorder brain tissue reveals alterations of free fatty acids, phosphatidylcholines, and ceramides. J Proteome Res 2008; 7: 4266–4277. [DOI] [PubMed] [Google Scholar]
- Taha AY, Cheon Y, Ma K, Rapoport SI, Rao JS. Altered fatty acid concentrations in prefrontal cortex of schizophrenic patients. J Psychiatr Res 2013; 47: 636–643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Misiak B, Stanczykiewicz B, Laczmanski L, Frydecka D. Lipid profile disturbances in antipsychotic-naive patients with first-episode non-affective psychosis: a systematic review and meta-analysis. Schizophr Res 2017. (e-pub ahead of print). [DOI] [PubMed]
- Solberg DK, Bentsen H, Refsum H, Andreassen OA. Association between serum lipids and membrane fatty acids and clinical characteristics in patients with schizophrenia. Acta Psychiatr Scand 2015; 132: 293–300. [DOI] [PubMed] [Google Scholar]
- Yang J, Chen T, Sun L, Zhao Z, Qi X, Zhou K et al. Potential metabolite markers of schizophrenia. Mol Psychiatry 2013; 18: 67–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodson L, Skeaff CM, Fielding BA. Fatty acid composition of adipose tissue and blood in humans and its use as a biomarker of dietary intake. Prog Lipid Res 2008; 47: 348–380. [DOI] [PubMed] [Google Scholar]
- Ni Y, Zhao L, Yu H, Ma X, Bao Y, Rajani C et al. Circulating Unsaturated Fatty Acids Delineate the Metabolic Status of Obese Individuals. EBioMedicine 2015; 2: 1513–1522, (2352-3964 (Electronic)). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trufelli H, Famiglini G, Termopoli V, Cappiello A. Profiling of non-esterified fatty acids in human plasma using liquid chromatography-electron ionization mass spectrometry. Anal Bioanal Chem 2011; 400: 2933–2941. [DOI] [PubMed] [Google Scholar]
- Ni Y, Zhao L, Yu H, Ma X, Bao Y, Rajani C et al. Circulating Unsaturated Fatty Acids Delineate the Metabolic Status of Obese Individuals. EBioMedicine 2015; 2: 1513–1522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assies J, Pouwer F, Lok A, Mocking RJ, Bockting CL, Visser I et al. Plasma and erythrocyte fatty acid patterns in patients with recurrent depression: a matched case-control study. PloS one 2010; 5: e10635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koerkamp MG, Rep M, Bussemaker HJ, Hardy GP, Mul A, Piekarska K et al. Dissection of transient oxidative stress response in Saccharomyces cerevisiae by using DNA microarrays. Mol Biol Cell 2002; 13: 2783–2794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warensjo E, Ohrvall M, Vessby B. Fatty acid composition and estimated desaturase activities are associated with obesity and lifestyle variables in men and women. Nutr Metab Cardiovasc Dis 2006; 16: 128–136. [DOI] [PubMed] [Google Scholar]
- Chong MF, Hodson L, Bickerton AS, Roberts R, Neville M, Karpe F et al. Parallel activation of de novo lipogenesis and stearoyl-CoA desaturase activity after 3 d of high-carbohydrate feeding. Am J Clin Nutr 2008; 87: 817–823. [DOI] [PubMed] [Google Scholar]
- Riserus U, Tan GD, Fielding BA, Neville MJ, Currie J, Savage DB et al. Rosiglitazone increases indexes of stearoyl-CoA desaturase activity in humans: link to insulin sensitization and the role of dominant-negative mutation in peroxisome proliferator-activated receptor-gamma. Diabetes 2005; 54: 1379–1384. [DOI] [PubMed] [Google Scholar]
- Salim S. Oxidative stress and psychological disorders. Curr Neuropharmacol 2014; 12: 140–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao JK, Leonard S, Reddy R. Altered glutathione redox state in schizophrenia. Dis Markers 2006; 22: 83–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedrini M, Massuda R, Fries GR, de Bittencourt Pasquali MA, Schnorr CE, Moreira JC et al. Similarities in serum oxidative stress markers and inflammatory cytokines in patients with overt schizophrenia at early and late stages of chronicity. J Psychiatr Res 2012; 46: 819–824. [DOI] [PubMed] [Google Scholar]
- Yao JK, Reddy R, McElhinny LG, van Kammen DP. Reduced status of plasma total antioxidant capacity in schizophrenia. Schizophr Res 1998; 32: 1–8. [DOI] [PubMed] [Google Scholar]
- Tsaluchidu S, Cocchi M, Tonello L, Puri BK. Fatty acids and oxidative stress in psychiatric disorders. BMC Psychiatry 2008; 8(Suppl 1): S5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adibhatla RM, Hatcher JF. Lipid oxidation and peroxidation in CNS health and disease: from molecular mechanisms to therapeutic opportunities. Antioxid Redox Signal 2010; 12: 125–169. [DOI] [PubMed] [Google Scholar]
- Bentsen H, Solberg DK, Refsum H, Gran JM, Bohmer T, Torjesen PA et al. Bimodal distribution of polyunsaturated fatty acids in schizophrenia suggests two endophenotypes of the disorder. Biol Psychiatry 2011; 70: 97–105. [DOI] [PubMed] [Google Scholar]
- Hoen WP, Lijmer JG, Duran M, Wanders RJ, van Beveren NJ, de Haan L. Red blood cell polyunsaturated fatty acids measured in red blood cells and schizophrenia: a meta-analysis. Psychiatry Res 2013; 207: 1–12. [DOI] [PubMed] [Google Scholar]
- Subashini R, Deepa M, Padmavati R, Thara R, Mohan V. Prevalence of diabetes, obesity, and metabolic syndrome in subjects with and without schizophrenia (CURES-104). J Postgrad Med 2011; 57: 272–277. [DOI] [PubMed] [Google Scholar]
- Tandon R, Nasrallah HA, Keshavan MS. Schizophrenia, "just the facts" 4. Clinical features and conceptualization. Schizophr Res 2009; 110: 1–23. [DOI] [PubMed] [Google Scholar]
- Azad MC, Shoesmith WD, Al Mamun M, Abdullah AF, Naing DK, Phanindranath M et al. Cardiovascular diseases among patients with schizophrenia. Asian J Psychiatr 2016; 19: 28–36. [DOI] [PubMed] [Google Scholar]
- Crupi R, Marino A, Cuzzocrea S. n-3 fatty acids: role in neurogenesis and neuroplasticity. Curr Med Chem 2013; 20: 2953–2963. [DOI] [PubMed] [Google Scholar]
- Zugno AI, Chipindo HL, Volpato AM, Budni J, Steckert AV, de Oliveira MB et al. Omega-3 prevents behavior response and brain oxidative damage in the ketamine model of schizophrenia. Neuroscience 2014; 259: 223–231. [DOI] [PubMed] [Google Scholar]
- Harris WS, Poston WC, Haddock CK. Tissue n-3 and n-6 fatty acids and risk for coronary heart disease events. Atherosclerosis 2007; 193: 1–10. [DOI] [PubMed] [Google Scholar]
- Annamalai A, Tek C. An overview of diabetes management in schizophrenia patients: office based strategies for primary care practitioners and endocrinologists. Int J Endocrinol 2015; 2015: 969182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schreurs M DEH, Vancampfort V, D, VANW R. Metabolic syndrome in people with schizophrenia: a review. World Psychiatry 2009; 8: 15–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Egea E, Bernardo M, Donner T, Conget I, Parellada E, Justicia A et al. Metabolic profile of antipsychotic-naive individuals with non-affective psychosis. Br J Psychiatry 2009; 194: 434–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandez-Egea E, Bernardo M, Parellada E, Justicia A, Garcia-Rizo C, Esmatjes E et al. Glucose abnormalities in the siblings of people with schizophrenia. Schizophr Res 2008; 103: 110–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guest PC, Wang L, Harris LW, Burling K, Levin Y, Ernst A et al. Increased levels of circulating insulin-related peptides in first-onset, antipsychotic naive schizophrenia patients. Mol Psychiatry 2010; 15: 118–119. [DOI] [PubMed] [Google Scholar]
- Spelman LM, Walsh PI, Sharifi N, Collins P, Thakore JH. Impaired glucose tolerance in first-episode drug-naive patients with schizophrenia. Diabet Med 2007; 24: 481–485. [DOI] [PubMed] [Google Scholar]
- Ryan MC, Collins P, Thakore JH. Impaired fasting glucose tolerance in first-episode, drug-naive patients with schizophrenia. Am J Psychiatry 2003; 160: 284–289. [DOI] [PubMed] [Google Scholar]
- Carpentier A, Mittelman SD, Lamarche B, Bergman RN, Giacca A, Lewis GF. Acute enhancement of insulin secretion by FFA in humans is lost with prolonged FFA elevation. Am J Physiol 1999; 276(6 Pt 1): E1055–E1066. [DOI] [PubMed] [Google Scholar]
- Roden M, Price TB, Perseghin G, Petersen KF, Rothman DL, Cline GW et al. Mechanism of free fatty acid-induced insulin resistance in humans. J Clin Invest 1996; 97: 2859–2865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tremblay F, Lavigne C, Jacques H, Marette A. Defective insulin-induced GLUT4 translocation in skeletal muscle of high fat-fed rats is associated with alterations in both Akt/protein kinase B and atypical protein kinase C (zeta/lambda) activities. Diabetes 2001; 50: 1901–1910. [DOI] [PubMed] [Google Scholar]
- Mordier S, Iynedjian PB. Activation of mammalian target of rapamycin complex 1 and insulin resistance induced by palmitate in hepatocytes. Biochem Biophys Res Commun 2007; 362: 206–211. [DOI] [PubMed] [Google Scholar]
- Patel PS, Sharp SJ, Jansen E, Luben RN, Khaw KT, Wareham NJ et al. Fatty acids measured in plasma and erythrocyte-membrane phospholipids and derived by food-frequency questionnaire and the risk of new-onset type 2 diabetes: a pilot study in the European Prospective Investigation into Cancer and Nutrition (EPIC)-Norfolk cohort. Am J Clin Nutr 2010; 92: 1214–1222. [DOI] [PubMed] [Google Scholar]
- Gustavo Vazquez-Jimenez J, Chavez-Reyes J, Romero-Garcia T, Zarain-Herzberg A, Valdes-Flores J, Manuel Galindo-Rosales J et al. Palmitic acid but not palmitoleic acid induces insulin resistance in a human endothelial cell line by decreasing SERCA pump expression. Cell Signal 2015; 28: 53–59. [DOI] [PubMed] [Google Scholar]
- Hirabara SM, Curi R, Maechler P. Saturated fatty acid-induced insulin resistance is associated with mitochondrial dysfunction in skeletal muscle cells. J Cell Physiol 2010; 222: 187–194. [DOI] [PubMed] [Google Scholar]
- Ishii M, Maeda A, Tani S, Akagawa M. Palmitate induces insulin resistance in human HepG2 hepatocytes by enhancing ubiquitination and proteasomal degradation of key insulin signaling molecules. Arch Biochem Biophys 2015; 566: 26–35. [DOI] [PubMed] [Google Scholar]
- Koutsari C, Jensen MD. Thematic review series: patient-oriented research. Free fatty acid metabolism in human obesity. J Lipid Res 2006; 47: 1643–1650. [DOI] [PubMed] [Google Scholar]
- Rezanka T, Sigler K. Odd-numbered very-long-chain fatty acids from the microbial, animal and plant kingdoms. Prog Lipid Res 2009; 48: 206–238. [DOI] [PubMed] [Google Scholar]
- Borre YE, O'Keeffe GW, Clarke G, Stanton C, Dinan TG, Cryan JF. Microbiota and neurodevelopmental windows: implications for brain disorders. Trends Mol Med 2014; 20: 509–518. [DOI] [PubMed] [Google Scholar]
- Clarke G, O'Mahony SM, Dinan TG, Cryan JF. Priming for health: gut microbiota acquired in early life regulates physiology, brain and behaviour. Acta Paediatr 2014; 103: 812–819. [DOI] [PubMed] [Google Scholar]
- Elman I, Borsook D, Lukas SE. Food intake and reward mechanisms in patients with schizophrenia: implications for metabolic disturbances and treatment with second-generation antipsychotic agents. Neuropsychopharmacology 2006; 31: 2091–2120. [DOI] [PubMed] [Google Scholar]
- Heald A, Pendlebury J, Anderson S, Narayan V, Guy M, Gibson M et al. Lifestyle factors and the metabolic syndrome in Schizophrenia: a cross-sectional study. Ann Gen Psychiatry 201716: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahn LA, Galletly CA, Foley DL, Mackinnon A, Watts GF, Castle DJ et al. Inadequate fruit and vegetable intake in people with psychosis. Aust N Z J Psychiatry 2014; 48: 1025–1035, (1440-1614 (Electronic)). [DOI] [PubMed] [Google Scholar]
- Folley BS, Park S. Relative food preference and hedonic judgments in schizophrenia. Psychiatry Res 2010; 175: 33–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.