Key Clinical Message
Popliteal artery occlusion after total knee arthroplasty is rare (0.03–0.17%) but can lead to amputation if overlooked. We should carefully assess vascular patency by Doppler ultrasound and ankle brachial pressure index (ABPI) measurement before and after total knee arthroplasty (TKA) operation.
Keywords: popliteal artery, thrombosis, Total knee arthroplasty
Introduction
Individuals indicated for total knee arthroplasty (TKA) are most often elderly, among whom limb arterial diseases are not uncommon 1. In fact, chronic lower extremity arterial insufficiency is estimated to exist in 2% of patients undergoing total knee arthroplasty 2. Popliteal artery occlusion after total knee arthroplasty occurs at a low incidence (0.03–0.17%) 3, 4, 5 but can be a grave complication if not found and treated promptly. We experienced a case of acute arterial occlusion at the right popliteal artery after simultaneous bilateral total knee arthroplasty. Fortunately, we found acute arterial thrombosis just after the operation and managed well without any complications. We report the case in detail here.
Case Presentation
The patient was an 80‐year‐old Asian female. She had been suffering from intractable right knee pain for 20 years and left knee pain for 10 years due to osteoarthritis. Conservative treatment failed, and she consulted us for surgical treatment. She was a nonsmoker and had hypertension and history of surgical treatment for left breast cancer 15 years ago with additional hormonal therapy (tamoxifen) for several years. Her hypertension was well controlled with medications. There were no signs of metastasis of her breast cancer.
Physical examination revealed limited range of motion in both knees (−5° extension lag and 125° passive flexion limit). Preoperative X‐rays showed disappearance of medial knee joint spaces, rigorous osteophyte formations and moderate varus deformity (Fig. 1). Femorotibial angles (FTA) were measured as 182° for both knees.
Figure 1.

Preoperative radiographs of both knees. Varus deformity with disappearance of joint spaces at medial compartment and osteophyte formations at patellofemoral joint are shown. Calcified‐free bodies located in the left knee. Vascular calcification is not obvious.
We performed simultaneous bilateral total knee arthroplasties under lumber spinal anesthesia. ACTIYAS implants (Kyocera Medical Corporation, Osaka, Japan) were used. Total ischemic time by tourniquet with 290 mmHg was 94 min for the right knee and 85 min for the left knee. The total operation times were almost the same bilaterally, that is, about 2 h. The whole procedure was completed without any complications. The postoperative radiograph showed successful implantation for both knees (Fig. 2).
Figure 2.
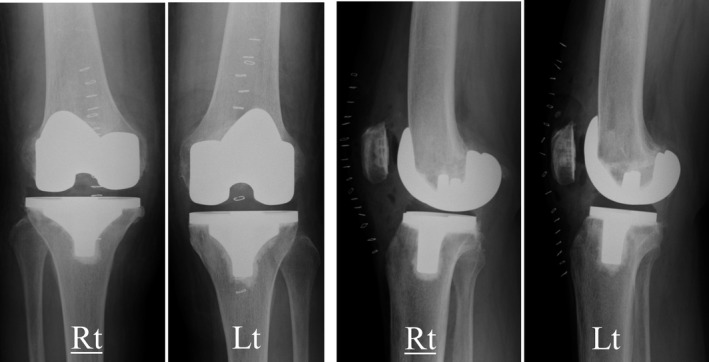
Postoperative radiographs of both knees. Each implant was installed in the proper position.
However, immediately after the operation was finished, we found that the right foot was cold and that the right dorsalis pedis artery and the right tibialis posterior artery were impalpable in the operating room. Although both feet appeared to be normal,the pulse oximeter displayed as low as 80% oxygen saturation and flat pulse wave in the right second toe. Acute arterial occlusion at the right lower extremity was suspected, and we immediately consulted vascular surgeons at our hospital. They diagnosed occlusion of the right popliteal artery with a Doppler ultrasound, and emergent angiography was performed in the operating room under general anesthesia. An arterial catheter was inserted into the right femoral artery, and angiography demonstrated that the right distal popliteal artery just proximal to the right peroneal‐tibia trunk was occluded (Fig. 3A). Vascular surgeons aspirated one fibrin clot longer than 2 cm and three blood clots (Fig. 4).
Figure 3.
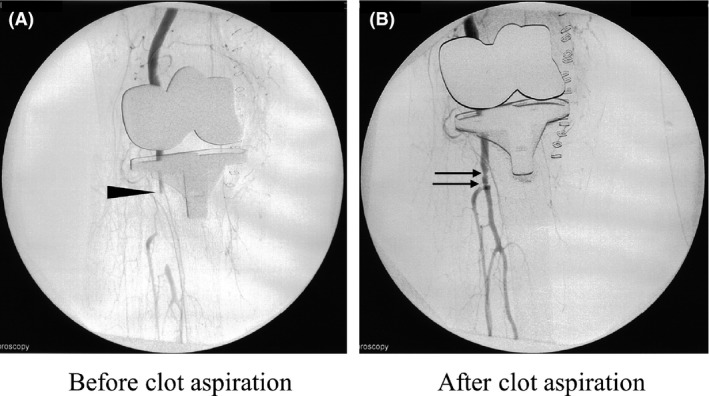
Angiographies of the right knee. (A) Before clot aspiration, the right distal popliteal artery just proximal to the right peroneal‐tibia trunk was occluded (arrow head). (B) After clot aspiration, the peroneal and tibia artery can be confirmed. Stenosis at the distal popliteal artery is still observed at the two portions (arrows).
Figure 4.
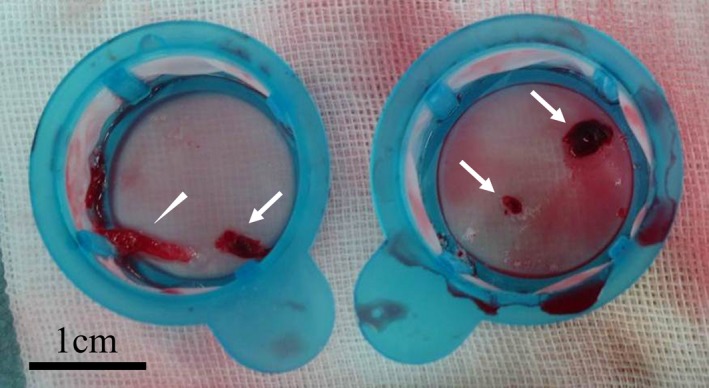
Aspirates. One fibrin clot (arrow head) and three blood clots (arrows) were obtained after aspiration.
After clot aspiration, the dorsalis pedis artery became palpable, oxygen saturation of the right second toe rose up to 100% on the pulse oximeter, and the peroneal and tibia artery were confirmed by angiography (Fig. 3B), although vascular stenosis was still observed in two portions at the distal popliteal artery. For anticoagulation treatment, a combination of heparin, alprostadil, cilostazol, and fondaparinux sodium was carefully used. The patient underwent the regular rehabilitation course, started early postoperative ambulation the next day, and left the hospital without recurrence of ischemic event 17 days after the operation. Four years have passed since the operation, and her knees function quite well without any problems.
Discussion
As the occurrence rate of acute arterial thrombosis after TKA, three cases of 9022 TKA patients were reported at Mayo Clinic, and the rate was as low as 0.03% 6. At Pennsylvania Hospital, seven of 4097 TKA patients were reported and the rate was 0.17% 5. Matziolis et al. 7 reviewed six reports and in a total of 31 cases of popliteal artery occlusions after TKA, amputations were performed in 11 cases. Chokesy et al. also reviewed that in 29 knees complicated with thrombosis after TKA, 11 cases required amputation 8. Arterial complications after TKA are relatively uncommon 9 but cause a catastrophic result if not managed properly.
As the commonly accepted Virchow's triad 10 indicates, the presumable risk factors of acute arterial thrombosis after TKA are intravascular stasis (no motion under lumbar anesthesia, tourniquet, an elastic bandage soon after the operation), damage of arterial endothelium (hypertension, compression by tibial anterior dislocation during operation, fragile arteriosclerotic plaque in vascular endothelium), and hypercoagulopathy (history of cancer and hormonal therapy) 11. In this case, all three risk factors did exist; therefore, a preoperative vascular study should be performed for the index patient.
For other risk factors, surgical correction of fixed knee deformities can bring about subsequent traction on the popliteal artery and cause intimal tears, which may lead to the formation of occlusive thrombus and ischemia 1. In addition, compression of the artery against the newly displaced bony or musculotendinous component also causes blood stasis and clot formation 12. Varus deformities and extension contractures of both knees are confirmed in this case, although the magnitude of deformity was moderate.
Ischemic time by tourniquet inflation is considered as a risk factor for thrombosis, but Matziolis et al. 7 reported a case of arterial occlusion caused by even limited use of a tourniquet for about 10 min during only the cementing phase. Most patients suffering from osteoarthritis are elderly and have associated atherosclerosis. A calcified plaque is fragile and easily fractured by even single, short‐term use of a tourniquet. Patients with a highly calcified femoropopliteal artery on plane radiographs should be encouraged to seek preoperative vascular surgery consultation, because the chronic lower extremity ischemic (CLEI) subgroup with no femoropopliteal calcification survived TKA with tourniquet use and without complications, compared with 25% ischemic complications with all CLEI populations 13. Prompt recognition and intervention are critical for limb salvage once artery occlusion occurs. Furthermore, orthopedic surgeons must be aware that, in some cases, acute arterial occlusion developed even after 9 days postoperatively 14. Latent popliteal artery injury during total knee arthroplasty has also been reported 15. Total knee arthroplasty is the orthopedic surgical procedure most commonly associated with vascular injuries, followed by hip arthroplasty 16, spinal surgery, and knee arthroscopy 17. This fact prompts us to pay further attention to preventing arterial injury and thrombosis after TKA.
The artifacts caused by the prostheses make computed tomography (CT) and magnetic resonance angiography (MRA) insufficient for an early and precise diagnosis. A Doppler ultrasound should be performed first, but thereafter angiography gives us the precise location of the lesion and can work as a less invasive approach for endovascular therapy 8.
Surgical procedure is of vital importance in preventing vascular injury. During TKA operation, insertion of the retractor into the posterolateral corner of the tibia should be avoided because it is the most vulnerable area of the popliteal artery 18, 19. The popliteal artery, vein, and posterior tibial nerve usually run through the posteromedial to the lateral corner of tibia, and more than one centimeter insertion of the retractor on this site poses a great risk of direct injury to the popliteal artery 20.
Several preoperative assessments have been proposed to minimize the arterial complications during knee arthroplasty. In the manifestation of a preexisting arterial disease, it is of primary importance to keep records during the physical examination. Smoking history, hypertension, diabetes mellitus, intermittent claudication, and previous history of transient ischemic attack or stroke should be addressed. Inspection of lower extremity circulation (popliteal artery, dorsalis pedis artery, and posterior tibial artery), skin ulceration, intolerance for cold, skin discoloration, and previous history of surgery should be focused on. Careful preoperative selection and vascular surgery consultation are thought to be warranted in doubtful cases 4.
Measuring ankle brachial pressure index (ABPI) can be an easy, objective preoperative vascular study for atherosclerosis. The problem is that inelastic blood vessels of patient with diabetes sometimes disfigure the diagnostic value of ABPI 12. In one report, seven chronic lower extremity patients with ischemia (ABPI < 0.9) and 33 normal patients (ABPI ≥ 0.9) were categorized by measuring ABPI before TKA 1. However, no arterial or venous injuries were found in either group, and low ABPI, correction of minor knee deformity, and a tourniquet time of 2 hours did not alter arterial blood pressure before and after TKA 1. This study indicates that simple criterion by measuring ABPI preoperatively is not good enough to screen out high‐risk patients with ischemia.
Palpation of the dorsalis pedis artery after TKA is thought to be imperative and should be conducted and recorded in all cases because other typical signs of ischemia, such as pain, paresthesia, and paralysis, are often masked by spinal or epidural anesthesia and this fact often hampers early diagnosis. Furthermore, false‐negative Doppler sonographical studies failed to detect vascular emergencies until the dorsalis pedis artery was found to be impalpable in one case 3. In another case, even though the posterior tibialis artery was palpated, the dorsalis pedis artery was not palpated after TKA, which led to prompt diagnosis and treatment 7. In addition to our case, these studies demonstrate the clinical value of palpation of the dorsalis pedis artery after TKA.
Conclusion
We reported a case of acute arterial thrombosis after bilateral total knee arthroplasties. We recommend the pre‐ and postoperative assessment for low‐extremity blood flow, such as Doppler ultrasound, ABPI measurement, and severity of vascular calcification seen by knee lateral radiograph before and after TKA surgery, especially in patients with a risk of thrombosis.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editor‐in‐chief of this journal. The director of the local ethical committee of our institute also confirmed the patient's written consent for her case to be published and officially allowed us to submit this paper as an exempt from the approval of the committee.
Authorship
All the authors substantially contributed to this report. KI: worked as a major contributor in writing the manuscript. IS, KO, TN, MH, HK, TW, and TM: committed to the diagnosis and treatment of this case, critically revised the manuscript, and provided approval for the final version to be published.
Conflict of Interest
The authors declare that they have no competing interests.
Acknowledgments
We greatly appreciate the emergency response by the vascular surgery team at Tokyo Medical and Dental University Hospital. All the authors declare no conflict of interests to disclose. This study was supported by a grant‐in‐aid for Research on Regenerative Medicine for Clinical Application from the Ministry of Health, Labor and Welfare.
References
- 1. Patil, S. , Allan D. B., and Quin R.. 2002. Effect of total knee arthroplasty on blood flow to the lower limb ‐ a prospective clinical study and review of literature. J. Arthroplasty 17:882–886. [DOI] [PubMed] [Google Scholar]
- 2. Turner, N. S. , Pagnano M. W., and Sim F. H.. 2001. Total knee arthroplasty after ipsilateral peripheral arterial bypass graft ‐ acute arterial occlusion is a risk with or without tourniquet use. J. Arthroplasty 16:317–321. [DOI] [PubMed] [Google Scholar]
- 3. Bayne, C. O. , Bayne O., Peterson M., and Cain E.. 2008. Acute arterial thrombosis after bilateral total knee arthroplasty. J. Arthroplasty 23:e1231–e1236. [DOI] [PubMed] [Google Scholar]
- 4. Langkamer, V. G. 2001. Local vascular complications after knee replacement: a review with illustrative case reports. Knee 8:259–264. [DOI] [PubMed] [Google Scholar]
- 5. Calligaro, K. D. , Delaurentis D. A., Booth R. E., Rothman R. H., Savarese R. P., Dougherty M. J., et al. 1994. Acute arterial thrombosis associated with total knee arthroplasty. J. Vasc. Surg. 20:927–932. [DOI] [PubMed] [Google Scholar]
- 6. Rand, J. A. 1987. Vascular complications of total knee arthroplasty. Report of three cases. J. Arthroplasty 2:89–93. [DOI] [PubMed] [Google Scholar]
- 7. Matziolis, G. , Perka C., and Labs K.. 2004. Acute arterial occlusion after total knee arthroplasty. Arch. Orthop. Traum. Surg. 124:134–136. [DOI] [PubMed] [Google Scholar]
- 8. Choksey, A. , Noble J., Brown J. J. K., and Marcuson R. W.. 1998. Angiography in vascular problems with total knee replacement: a report of three cases. Knee 5:63–67. [Google Scholar]
- 9. Abularrage, C. J. , Weiswasser J. M., Dezee K. J., Slidell M. B., Henderson W. G., and Sidawy A. N.. 2008. Predictors of lower extremity arterial injury after total knee or total hip arthroplasty. J. Vasc. Surg. 47:803–807; discussion 807–808. [DOI] [PubMed] [Google Scholar]
- 10. Brotman, D. J. , Deitcher S. R., Lip G. Y. H., and Matzdorff A. C.. 2004. Virchow's triad revisited. South. Med. J. 97:213–214. [DOI] [PubMed] [Google Scholar]
- 11. Ko, L. J. , DeHart M. L., Yoo J. U., and Huff T. W.. 2014. Popliteal artery injury associated with total knee arthroplasty: trends, costs and risk factors. J. Arthroplasty 29:1181–1184. [DOI] [PubMed] [Google Scholar]
- 12. Butt, U. , Samuel R., Sahu A., Butt I. S., Johnson D. S., and Turner P. G.. 2010. Arterial injury in total knee arthroplasty. J. Arthroplasty 25:1311–1318. [DOI] [PubMed] [Google Scholar]
- 13. Delaurentis, D. A. , Levitsky K. A., Booth R. E., Rothman R. H., Calligaro K. D., Raviola C. A., et al. 1992. Arterial and ischemic aspects of total knee arthroplasty. Am. J. Surg. 164:237–240. [DOI] [PubMed] [Google Scholar]
- 14. Gregory, P. C. , Rogic R., and Eddington C.. 2006. Acute arterial occlusion after total knee arthroplasty. Am. J. Phys. Med. Rehab. 85:924–926. [DOI] [PubMed] [Google Scholar]
- 15. De Santis, F. , Martini G., Haglmuller T., Mani G., Conati C., and Bonatti G.. 2013. Anticoagulation therapy for postoperative deep vein thrombosis coupled with pulmonary embolism: a potential trigger for delayed popliteal artery injury presentation after total knee arthroplasty. Phlebology 28:275–277. [DOI] [PubMed] [Google Scholar]
- 16. Simon, J. P. , Van Raebroeckx A., and Bellemans J.. 2007. Intraoperative arterial occlusion in total hip arthroplasty ‐ a report of two cases. Acta Orthop. Belg. 73:533–535. [PubMed] [Google Scholar]
- 17. Wu, R. W. , Hsu C. C., and Wang C. J.. 2003. Acute popliteal artery occlusion after arthroscopic posterior cruciate ligament reconstruction. Arthroscopy 19:889–893. [DOI] [PubMed] [Google Scholar]
- 18. Ninomiya, J. T. , Dean J. C., and Goldberg V. M.. 1999. Injury to the popliteal artery and its anatomic location in total knee arthroplasty. J. Arthroplasty 14:803–809. [DOI] [PubMed] [Google Scholar]
- 19. Tindall, A. J. , Shetty A. A., James K. D., Middleton A., and Fernando K. W.. 2006. Prevalence and surgical significance of a high‐origin anterior tibial artery. J. Orthop. Surg. (Hong Kong). 14:13–16. [DOI] [PubMed] [Google Scholar]
- 20. Farrington, W. J. , and Charnley G. J.. 2003. The effect of knee flexion on the popliteal artery and its surgical significance. J. Bone Joint Surg. Br. 85:1208; author reply 1208. [PubMed] [Google Scholar]


