Abstract
Utilization and perceived benefits of hospice may vary across populations. In a population-based survey, we examined the prevalence of hospice utilization; caregiver socio-demographic characteristics; and quality and complexity of end-of-life (EOL) care, as reported by community caregivers to people who died in the prior year.
The 2009–2010 Allegheny County, PA BRFSS Health Survey, a population-based telephone survey of 5442 adult residents, included an 8-item EOL caregiver module.
Overall 7.8% (95% CI=7.0, 8.6) of respondents reported having arranged or provided care for a close friend/family member who died in the previous 12 months. Caregivers of decedents who utilized hospice reported positive quality outcomes and greater involvement in care.
Utilization of hospice services was associated with beneficial outcomes at EOL, but with increased involvement of EOL caregivers.
Keywords: Hospice, End of Life Care, Caregivers, Community Surveys, Health Care Quality, Access, Evaluation, Behavioral Risk Factor Surveillance System
Introduction
Dying in America has changed markedly in the past quarter century and continues to change as the population ages, advances are made in the treatment of chronic disease, and opinion and practice around end-of-life (EOL) care evolve. There is an ever-increasing array of treatment choices available to those with life-limiting illness and their caregivers as well as a broadening of the possible settings in which an individual might choose to receive care at EOL.
Hospice is a multidisciplinary approach to EOL care that provides both pain and symptom management for individuals with life-limiting illness and psychological, spiritual, and practical support for the patient and family.1Hospice care is available in a variety of settings including the home, freestanding hospice facilities, and skilled care facilities, with the cost of services covered by both federal and private insurance programs.1Use of hospice services is associated with consistent benefits including: improved pain and symptom management; fewer hospital admissions; decreased incidence of curative treatment in the 48 hours prior to death; increased likelihood of dying in the location of choice; and improved patient and family satisfaction with care.2–7 Hospice may also be directly beneficial to those acting as caregivers at EOL. Providing care to a dying friend or family member can be highly stressful and may lead to poor physical and mental health outcomes.8 Research suggests that hospice utilization may buffer poor mental health outcomes for caregivers.2,5However, these studies are few and primarily involved retrospective designs or cohorts and/or samples limited to a single patient diagnosis.
While the benefits of hospice care are well demonstrated, a number of barriers to hospice utilization have been identified. Prior studies show that the availability of hospice services and patterns of hospice utilization are highly variable and depend on a variety of factors, including geographic region and locale (rural vs. urban), community demographics (race/ethnicity and wealth), and state hospice regulations, leading to disparities in hospice service availability, quality and uptake.1, 9–13 Regions with greater proportions of low-income and minority members typically have fewer hospice options.9, 10 African Americans are also less likely than whites to utilize hospice services, with cultural and historical factors being most often cited as a rationale for this difference.12
Nonetheless, use of hospice services in the U.S. has expanded exponentially in the forty years since the inception of the Medicare Hospice Benefit, from approximately 100,000 patients receiving services in 1984 to fully 1.58 million in 2010.1 As hospice becomes the predominant model in EOL care, it is important to monitor the prevalence and benefits of hospice for individuals at EOL and their caregivers. To this end we analyzed data from the Allegheny County Health Survey (ACHS) to determine 1) the prevalence of hospice use in a population-based survey; 2) socio-demographic differences between hospice users and non-users; and 3) differences in the quality and complexity of EOL care between hospice users and non-hospice users.
Methods
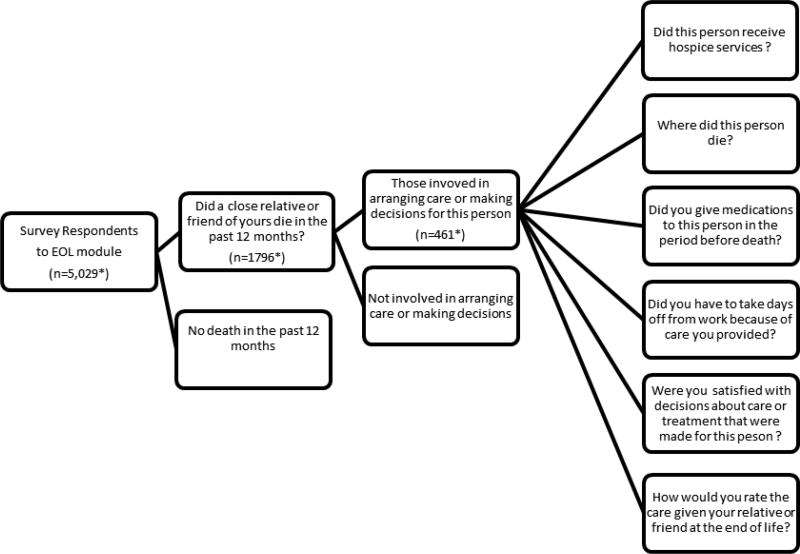
Data were drawn from the 2009–2010 Allegheny County Health Survey (ACHS), conducted by the Evaluation Institute of the University of Pittsburgh’s Graduate School of Public Health on behalf of the Allegheny County Health Department.14This county-wide, population-based telephone survey was modeled after the Center for Disease Control (CDC) Behavioral Risk Factor Surveillance System (BRFSS) and included an EOL module (Figure 1). The EOL module consisted of 8 items focused on EOL caregiving; services utilized; satisfaction with decision-makingand quality of dying. Items used in the module were based on a CDC inventory of questions used in the EOL module currently under development for the BRFSS. The module was administered in a step-wise fashion such that all 8 items were only administered to those reporting care at EOL (Figure 1). The collection of EOL care data via population-based surveys is based on recommendations from the Institute of Medicine, National Institutes of Health, and other stakeholders.15, 16
Figure 1.
End of Life Module Survey Structure
*excludes missing, “don’t know” and “refused” responses
In addition to EOL measures, two measures of mental health were collected as part of main survey. While we were unable to collect information on the time elapsed between the interview and death of the close friend/family member or the duration of hospice service delivery, we chose to include the mental health measures to capture associations between mental health and caregiving at EOL. The Kessler-6 scale is a reliable and valid measure used to screen for serious mental illness,17,18 and the number days in the prior month where mental health is reported as “not good” is currently included in the annual BRFSS and other national surveys.19 Scores were dichotomized. Serious mental illness was coded as a Kessler-6 score of 13 or greater18and poor mental health-related quality of life was coded as greater or equal to 4 “not good” mental health days in past 30 days. Four or more “not good” mental health days indicates the uppermost quartile in the distribution. Demographic data included age, gender, race, household income, and education. Race was dichotomized into white and African American, reflective of the demographic profile of the region. (Non-African American minority respondents made up only 2.3% the sample.)
In total 5,442 phone interviews were conducted between August, 2009 and September, 2010. The sample, which was limited to individuals aged 18 or older, was enrolled using a Random Digit Dialing (RDD) protocol. A disproportionate stratified sampling design was employed and included oversampling productive telephone numbers and telephone exchanges corresponding to census tracts with 50% or more African Americans residents and census tracts with household incomes below the county’s median household income. The cooperation rate, defined as the proportion of all cases interviewed of all those contacted, was 66%.
Post-stratification weighting was conducted to reflect the known population totals for Allegheny County adults. Additional weighting was performed to adjust for probability of selection and included weighting for oversampling of African Americans and low income households, selection of one adult per household, and selection of households with more than one landline telephone number. The results reported here are based on analyses of the weighted data and were conducted using survey procedures in SAS 9.2 (SAS Institute, Inc., Cary, NC). Differences between caregiver groups and between hospice and non-hospice caregiver groups were assessed using Rao Scott chi-square tests, which account for design effects in complex sample surveys. Differences were considered significant at p < .05.
The research was approved by the Institutional Review Board of the University of Pittsburgh.
Results
Comparisons between those who completed the EOL module (n=5029) and those who terminated the survey prior to the EOL module (n=413) indicated that those who terminated the survey had lower household incomes (OR = 1.7, 95%CI = 1.3–2.2) and were more likely to be African American (OR = 1.5, 95%CI = 1.12–1.95) than those completing the EOL module. No differences in gender or age were observed. Of the 5029 Allegheny County residents completing the EOL module, 33.8% (95% CI=32.1%–35.5%) reported that a close relative or friend had died in the past 12 months; and among those reporting a death, 23.2% (95% CI = 20.9%,–25.5%) reported they had arranged care or made decisions on behalf of the individual who had died. This yielded a sub-sample of 461 respondents, which we termed “EOL caregivers,” who were primary caregivers to someone who had died. The EOL caregivers account for 7.8% (95% CI = 7.0%–8.6%) of the county’s adult population and indicate the overall prevalence of EOL caregiving in the previous 12 months.
Compared to those reporting a death but not involved in EOL care, EOL caregivers were more likely to be older (age 50+years) and female (OR = 1.4, 95% CI = 1.1–1.9 and OR = 1.4, 95% CI = 1.1–1.8, respectively). The two groups did not differ by race, educational attainment, or household income.
As shown in Table 1, over half of EOL caregivers reported use of hospice (n=238, or 53.7%). Compared to EOL caregivers not using hospice, EOL caregivers using hospice were more likely to have annual household incomes above $25,000 (OR = 1.5, 95% CI = 1.0–2.4). No other demographic differences were observed.
Table 1.
Caregiver Demographics and Outcomes among EOL Caregivers, by Hospice Status
| Measure | EOL Caregivers, non- Hospice (n=214)a |
EOL Caregivers With Hospice (n=238)a |
P Valueb |
|---|---|---|---|
| Age, frequency (weighted percent) | |||
| 18–49 | 58 (36.9%) | 71 (39.3%) | .67 |
| 50+ | 156 (63.1%) | 167 (60.7%) | |
| Race, frequency (weighted percent) | |||
| White | 146 (79.0%) | 180 (84.2%) | .15 |
| African-American | 68 (21.0%) | 58 (15.8%) | |
| Gender, frequency (weighted percent) | |||
| Male | 60 (39.2%) | 71 (39.2%) | .99 |
| Female | 154 (60.8%) | 167 (60.8%) | |
| Level of Education, frequency (weighted percent) | |||
| ≤High School | 80 (39.3%) | 90 (41.1%) | .74 |
| >High School | 134 (60.7%) | 148 (58.9%) | |
| Income, frequency (weighted percent) | |||
| <$25,000 | 95 (40.0%) | 81 (30.2%) | .05 |
| ≥$25,000 | 119 (60.0%) | 157 (69.8%) | |
| Kessler-6 Score, frequency (weighted percent) | |||
| ≥13 | 18 (8.5%) | 17 (8.7%) | .95 |
| <13 | 193 (91.5%) | 221 (91.3%) | |
| Days in month where mental health was not good, frequency (weighted percent) | |||
| > 4 days | 71 (34.4%) | 77 (34.1%) | .96 |
| ≤ 4 days | 143 (65.6%) | 161 (65.9%) | |
| Administered Medications in the Period before Death, frequency (weighted percent) | 56 (33.3%) | 85 (46.4%) | .03 |
| Rated Care at End-of-Life as Excellent, frequency (weighted percent) | 52 (26.1%) | 117 (51.2%) | <.0001 |
| Satisfied with Decisions about Care or Treatment, frequency (weighted percent) | 161 (71.2%) | 204 (86.4%) | .03 |
| Non-Hospital Location of Death, frequency (weighted percent) | 96 (45.3%) | 181 (74.1%) | <.0001 |
Excluding missing, “don’t know”, and “refused” responses
Based on the Rao-Scott χ2 test.
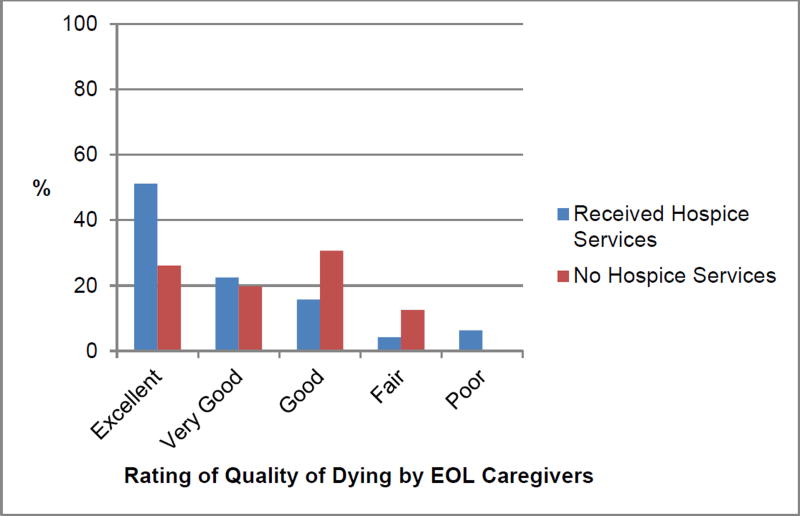
Use of hospice services was associated with a significantly higher likelihood of death occurring outside the hospital setting, either at home or at an alternative location such as skilled nursing or free-standing hospice facility (OR = 3.5, 95% CI = 2.2–5.4). The use of hospice services was also associated with overwhelmingly greater satisfaction with quality of dying, as shown in Figure 2. EOL caregivers who used hospice were three times as likely to rate the quality of care at EOL as excellent (OR = 3.0, 95% CI = 1.8–4.8). In addition, EOL caregivers using hospice were twice as likely to report satisfaction with decisions about care or treatment (OR = 2.0, 95% CI = 1.1–3.6).
Figure 2.
Quality of Dying with and without Hospice Services Utilization
EOL caregiving required considerable investment of time and effort on the part of family members, as evidenced by the higher proportion of caregivers who administered medications and took time off from work. Thirty-five percent of EOL caregivers administered medicine in the period before death, and 58.3% reported a need to take off days of work during this time. Caregivers using hospice were more likely to report taking time off from work (OR= 1.9; 95% CI=1.0, 3.6) and administering medications (OR=1.7; 95% CI=1.1, 2.9) compared to EOL caregivers who did not make use of hospice.
Despite the increased investment in caregiving tasks among EOL caregivers who used hospice services (and hence likely greater caregiving burden), outcomes on measures related to mental health did not differ according to hospice use, Table 1.
Discussion
Findings from the ACHS indicate Allegheny County, PA residents have a relatively high rate of hospice usage (53.7%), even among minority members of the community (46.6%). These rates are above the national average of 41.9% deaths involving hospice1 and may be related to the high percentage of older adults in the community, the robust healthcare infrastructure, and the number and breadth of hospice agencies and facilities in the area. The benefits of hospice involvement at EOL included increased satisfaction with care and a lower likelihood of death occurring in the hospital, where the chances of receiving aggressive, costly, and often unwanted treatment are high.20By the same token, hospice was also was associated with increased complexity of care and involvement in caregiving tasks on the part of EOL caregivers.
With the aging of the U.S. population, an increasing number of individuals will spend at least some time in the EOL caregiving role. Pittsburgh ranks in the top 15 U. S. cities with the highest proportion of residents over 65 years of age, so this is a particular concern for Allegheny County. Indeed, the survey found EOL caregivers in all age categories, although the majority of EOL caregivers were older. In addition, the responsibilities of caregiving fell disproportionately on women. Many of these are likely to be older women caring for a spouse, and those ≤ 50 years may be daughters simultaneously working, caring for younger children, and providing supportive care to an aging relative.
Although there was no difference in the mental health outcomes between EOL caregivers with and without hospice, these finding must be interpreted cautiously. Caregivers in deaths with hospice involvement experienced greater potential burden, as indicated by higher likelihood of hands-on care (administering medications) and greater need to take time off from work. The higher level of caregiver involvement seen among those utilizing hospice services is likely reflective of those caregiving situations where home hospice services are used. In the home hospice care model, agency staff provides support and some direct care services, but the family members or informal caregivers remain primary caregivers to the patient. Hospice utilization was associated with higher household incomes, so it is possible that despite the increased involvement, greater financial resources may offset stress due to caregiver burden.
Strengths of this research include a population-based assessment of EOL circumstances for both individuals and their caregivers, including EOL care options chosen. With recent expansion of EOL services, such as hospice and palliative care, and great variation in state regulation concerning delivery of EOL services, it is important to describe EOL care utilization patterns, the level of the satisfaction caregivers have with EOL care services, and the quality of care being provided. In addition, with increasing options for where these services can be delivered, it is valuable to assess patterns of use within the community.
Results should be interpreted in light of the study design. Although we had a robust picture of caregivers, data on decedents are limited. The cause of death, demographic characteristics of the deceased, and relationship to the caregiver were not elicited in the EOL module. We did not obtain information on the duration of hospice service or whether hospitalized patients received hospital-based palliative care consultation services. Among EOL caregivers, the duration of time that elapsed between the death and telephone interview was not elicited. Finally, the cross-sectional nature of the survey precluded any understanding of the temporal ordering of care events, death, and mental health status.
Overall, this population-based study provides insight into EOL care in a community, direction for ongoing research, and identification of areas for increased community awareness and public health focus. Public health is increasingly concerned with quality of life at the end-of-life. Given current population trends, the number and age of those providing informal EOL caregiving will steadily increase. If the current model of home hospice care is to remain successful, these caregivers will likely require higher levels of support. Determining EOL caregiving patterns, place of death, and the impact of EOL caregiving on families can expand the public health knowledge base in this area. Future studies might also explore differences in demographics and caregiver involvement among the different settings in which hospice services are delivered.
Acknowledgments
University of Pittsburgh-School of Nursing & Graduate School of Public Health; Institute for Evaluation Science in Community Health; National Hartford Centers of Gerontological Nursing Excellence; Allegheny County Health Department and Community Supporters
Footnotes
Presented: Gerontological Society of America, Annual Scientific Meeting, New Orleans, LA, November 21, 2013
Contributor Information
Jennifer B. Seaman, University of Pittsburgh, School of Nursing.
Todd M. Bear, University of Pittsburgh, Graduate School of Public Health.
Patricia I. Documet, University of Pittsburgh, Graduate School of Public Health.
Susan M. Sereika, University of Pittsburgh, School of Nursing.
Steven M. Albert, University of Pittsburgh, Graduate School of Public Health.
References
- 1.NHPCO Facts and Figures. Hospice Care in America. Alexandria, VA: National Hospice and Palliative Care Organization; 2012. http://www.nhpco.org/sites/default/files/public/Statistics_Research/2012_Facts_Figures.pdf. [Google Scholar]
- 2.Christakis NA, Iwashyna TJ. The health impact of health care on families: a matched cohort study of hospice use by decedents and mortality outcomes in surviving, widowed spouses. Soc Sci Med. 2003;57:465–475. doi: 10.1016/s0277-9536(02)00370-2. [DOI] [PubMed] [Google Scholar]
- 3.Teno JM, Clarridge BR, Casey V, Welch LC, Wetle T, Shield R, Mor V. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 4.Solloway M, LaFrance S, Bakitas M, Gerken M. A chart review of seven hundred eighty-two deaths in hospitals, nursing homes, and hospice/home care. J Palliat Med. 2005;8:789–796. doi: 10.1089/jpm.2005.8.789. [DOI] [PubMed] [Google Scholar]
- 5.Wright AA, Keating NL, Balboni TA, Matulonis UA, Block SD, Prigerson HG. Place of death: Correlations with quality of life of patients with cancer and predictors of bereaved caregivers' mental health. J Clin Oncol. 2010;28:4457–4464. doi: 10.1200/JCO.2009.26.3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brumley R, Enguidanos S, Jamison P, Seitz R, Morgenstern N, Saito S, McIlwane J, Hillary K, Gonzales J. Increased satisfaction with care and lower costs: Results of a randomized trial of in-home palliative care. J Am Geriatr Soc. 2007;55:993–1000. doi: 10.1111/j.1532-5415.2007.01234.x. [DOI] [PubMed] [Google Scholar]
- 7.Shega JW, Hougham GW, Stocking CB, Cox-Hayley D, Sachs GA. Patients dying with dementia: Experience at the end of life and impact of hospice care. J Pain Symptom Manage. 2008;35:499–507. doi: 10.1016/j.jpainsymman.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 8.Schultz R, Hebert R, Boerner K. Bereavement after caregiving. Geriatrics. 2008;63:20–22. [PMC free article] [PubMed] [Google Scholar]
- 9.O’Mahony S, McHenry J, Snow D, Cassin C, Schumacher D, Selwyn PA. A review of barriers to utilization of the medicare hospice benefits in urban populations and strategies for enhanced access. J Urban Health. 2008;85:281–290. doi: 10.1007/s11524-008-9258-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Silveira MJ, Connor SR, Goold SD, McMahon LF, Feudtner C. Community supply of hospice: Does wealth play a role? J Pain Symptom Manage. 2011;42:76–82. doi: 10.1016/j.jpainsymman.2010.09.016. [DOI] [PubMed] [Google Scholar]
- 11.Johnson KS, Kuchibhatla M, Tanis D, Tulsky JA. Racial differences in hospice revocation to pursue aggressive care. Arch Intern Med. 2008;168:218–224. doi: 10.1001/archinternmed.2007.36. [DOI] [PubMed] [Google Scholar]
- 12.Mazanec PM, Daly BJ, Townsend A. Hospice utilization and end-of-life care decision making of African Americans. Am J Hosp Palliat Care. 2010;27:560–566. doi: 10.1177/1049909110372087. [DOI] [PubMed] [Google Scholar]
- 13.Carlson MD, Morrison RS, Holford TR, Bradley EH. Hospice care: What services do patients and their families receive? Health Serv Res. 2007;42:1672–1690. doi: 10.1111/j.1475-6773.2006.00685.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Documet PI, Bear TM, Green HH. Results from the 2009–2010 Allegheny county health survey (ACHS): Measuring the health of adult residents. Pittsburgh: The Evaluation Institute; 2012. [Google Scholar]
- 15.Lunney JR, Foley KM, Smith TJ, Gelband H, editors. Describing Death in America: What We Need to Know. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 16.Rao JK, Alongi J, Anderson LA, Jenkins L, Stokes G-A, Kane M. Development of public health priorities for end-of-life initiatives. Am J Prev Med. 2005;29:453–460. doi: 10.1016/j.amepre.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 17.Kessler R, Andrews G, Colpe L, Hiripi E, Mrocek DK, Normand SL, Walters EE, Zaslavsky AM. Short screening scales to monitor population prevalances and trends in nonspecific psychological distress. Psychol Med. 2002;32:959–979. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- 18.Kessler RC, Barker PR, Colpe LJ, Epstein JF, Gfroerer JC, Hiripi E, Howes MJ, Normand SL, Manderscheid RW, Walters EE, Zaslavaky AM. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60:184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 19.Hagerty MR, Cummins RA, Ferriss AL, Land K, Michalos AC, Peterson M, Sharpe A, Sirgy J, Vogel J. Quality of life indexes for national policy: Review and agenda for research. Soc Ind Res. 2001;55:1–96. [Google Scholar]
- 20.Field MJ Cassel CK, editor. Approaching Death: Improving Care at the End of Life. Washington, DC: The National Academies Press; 1997. [PubMed] [Google Scholar]