Abstract
Objectives
The aim of this study was to compare potential differences between the perception that COPD patients have of their disease and the perception that physicians have of how the disease affects their patients.
Methods
Surveys in COPD patients and physicians caring for COPD patients were conducted in Spain, Italy, and Germany. Online questionnaires mirrored to explore the same domains, were administered to patients and physicians. Physicians were asked to respond to the questionnaire taking a recently seen patient who represents the majority of COPD patients usually managed, as a reference. Patients with COPD completed a survey containing the same questions offered to the physicians (Medical Investigation of Respiratory COPD Perception [MIRROR] survey). Comparisons between the responses of patients and general practitioners (GPs) and between patients and pulmonologists (PULs) were run separately using the chi-square, Fisher’s exact, or Student’s t-tests.
Results
A total of 334 COPD patients, 333 GPs, and 333 PULs participated in the surveys. The typical perception that PULs have of the COPD patient was that of an older man with more severe disease and less likely to be a smoker, than the included COPD patients. COPD was regarded as a major health problem by patients and physicians, but its impact on overall quality of life among more severe patients was less strongly perceived by physicians than by patients. Instead, physicians paid more attention to domains related to clinical features (cough, phlegm, and dyspnea), while underestimating COPD impact on leisure and social activities. The majority of patients stated not being completely frank with their doctors during visits. Both GPs and PULs seemed to recognize this issue but underestimated its extent.
Conclusion
To improve the doctor–patient communication, a more frank reporting by the patients of their symptoms and feelings and an increased awareness of physicians about the impact on nonconventional domains that patients perceive as importantly affected by COPD should be encouraged.
Keywords: COPD, perception, QoL
Introduction
COPD is a major public health problem because of its high prevalence, adverse impact on quality of life (QoL),1 and large social and economic costs.2 The recent 2017 update of the Global Strategy for Diagnosis and Management of COPD (GOLD) states that the disease is characterized by “persistent respiratory symptoms and airflow limitation”.3 Yet, the severity of symptoms and the impairment of QoL are weakly associated with the degree of airflow limitation.4
The Confronting COPD International Survey conducted in Europe and North America showed that many patients underestimated their symptoms and the severity of disease.5 Similarly, the hidden depths of COPD online survey also identified a significant impact of COPD on daily activities with frequent health care resource use, despite the fact that the majority of patients regarded their disease as “under control”.6 Psychological and behavioral factors may influence individual perceptions of symptom severity, and strategies used by patients to cope with the burden of symptoms and disability are still incompletely understood.7 Several studies1,10,13 have conducted surveys pairing patients with the doctors taking care of them and have observed differences in the way the disease is perceived. However, a limiting factor is that different questionnaires have been used for the two groups. To our knowledge, no previous study has attempted to identify, quantify, characterize, and understand the communication gaps in the perception of disease and QoL between patients and physicians using a tool that contains identical questions.
We hypothesized that there are important differences (gaps) between the perceptions that COPD patients have of their disease and physicians have of how the disease affects their COPD patients. In addition, we hypothesized that there were problems in the frankness of COPD patients during their interaction with physicians in clinic visits. The Medical Investigation of Respiratory COPD Perception (MIRROR) survey was conducted to determine the presence and magnitude of perception gaps that exist between patients with COPD and physicians who care for COPD patients.
Methods
Study design
Surveys in patients with COPD and physicians caring for patients with COPD, both in general practitioners (GPs) and pulmonologists (PULs) in specialized care, were conducted between July and August 2016 in Spain, Italy, and Germany. The survey was conducted by QuintilesIMS. QuintilesIMS is a member of the European Pharmaceutical Market Research Association (EphMRA), and this survey was conducted in compliance with the EphMRA code of conduct. All the subjects participating in the survey provided voluntary, informed consent to data collection and use, based upon a clear understanding of the purpose of the data collection. In addition, the present survey met the definition of market research, and thus did not require Clinical Research Ethics Committee or Independent Review Board approval.8
Patient survey
Patients were identified from national panels collaborating with QuintilesIMS (refer Supplementary materials for a full description of the panels) who met the following criteria: >45 years old, with a diagnosis of COPD and receiving maintenance therapy provided by their physicians on a continuous basis for at least 12 months and including at least one of the following drugs: long-acting beta-2 agonists, inhaled corticosteroids, long-acting muscarinic antagonists, or their combinations. Patients receiving supplemental oxygen were excluded. An invitation was sent through email to all COPD patients (n=13,108) who were panel members. A total of 1,164 (9%) patients accepted to participate, and 334 subjects met the inclusion criteria and returned a completed questionnaire. Participating patients were not being followed by the GPs and PULs taking part in the survey.
Physician survey
Participating physicians were recruited from panels of professionals collaborating with QuintilesIMS (refer Supplementary materials for a full description of the panels) who agreed to take part in the survey and had experience treating COPD patients. Participating GPs were required to be regular prescribers of >20 maintenance therapy prescriptions per month for COPD patients, whereas PULs had to spend >30% of their professional time managing COPD patients in the outpatient setting. Both GPs and PULs were asked to answer the questionnaire (refer Supplementary materials) taking one recently seen patient as a reference, who was representative of the majority of COPD patients seen in their clinical practice. An invitation was sent by email to 13,836 physicians: 1,192 (9%) accepted to participate and 666 physicians met the inclusion criteria and returned a completed questionnaire.
Survey questionnaire
The questionnaire was developed by a group of physicians and psychologists and then subjected to a review and approval process by physicians experienced in COPD research. The questions were administered through a Computer-Aided Web Interview (CAWI) lasting for ~30 minutes. A full description of the questionnaire, which was similar for patients and physicians, is explained in the Supplementary materials. In brief, questions included a mix of single and multiple responses as well as scalar items. Both patient’s and physician’s questionnaires explored the following domains: patient’s sociodemographics and COPD severity, symptoms and impact of disease on overall health-related QoL, and its individual domains (daily symptoms, working and leisure time activities, sleep, and physician/patient relationship). In addition, sub-domains of daily activities, such as self-care and household chores, were investigated. Participants were asked to assign a score using a scale ranging from 1 (not impact at all) to 5 (maximal impact). To investigate the openness of the physician/patient relationship, physicians were asked how frank (ie, whether the patient freely disclosed all relevant information) they felt the patient was during the visit, and patients were asked how frank they actually were while communicating with physicians. Finally, the survey also assessed the degree of disease severity (mild, moderate, severe, and very severe) as perceived by patients and physicians, the perceived degree of satisfaction with the overall treatment, and the handling of the inhalers.
Statistical analysis
Since results in the three participating countries (Spain, Italy, and Germany) were not significantly different, only the aggregated results are presented. To compare the responses of patients, GPs and PULs, we used chi-square, Fisher’s exact, or Student’s t-tests for independent groups, as appropriate. Comparisons between patients and GPs and between patients and PULs were performed separately. P-value <0.05 was considered statistically significant. Analyses were performed using SPSS, Version 22.
Results
Patients’ characteristics
The survey included 334 COPD patients, 333 GPs, and 333 PULs (Table 1). Compared to the actual responses by the patients, on average, the PULs thought that their patients were older, primarily men, with lower educational level, more severe disease, more likely to live with the family, and less likely to be actively smoking. For most of the variables, the patients described by GPs had characteristics that fell between patients reported by PULs and the patients participating in the survey.
Table 1.
Characteristics of patients directly answering the questionnaire (patients) and those reported by GPs or PULs
| Patients, n=334 | GPs, n=333 | PULs, n=333 | P-valuea (patients vs GPs) | P-valuea (patients vs PULs) | |
|---|---|---|---|---|---|
| Age strata (years), n (%) | |||||
| 45–54 | 98 (29.3) | 87 (26.1) | 42 (12.6) | 0.002 | <0.001 |
| 55–64 | 153 (45.8) | 121 (36.3) | 136 (40.8) | ||
| 65+ | 83 (24.9) | 125 (37.5) | 155 (46.5) | ||
| Gender, female, N (%) | 139 (41.6) | 37 (11.1) | 28 (8.4) | <0.001 | <0.001 |
| Education level, N (%) | |||||
| Elementary/middle school | 150 (44.9) | 227 (68.2) | 213 (64.0) | <0.001 | <0.001 |
| High school/university | 184 (55.1) | 73 (21.9) | 90 (27.0) | ||
| Working status, N (%) | |||||
| Employed | 148 (44.3) | 169 (50.8) | 137 (41.1) | <0.001 | <0.001 |
| Retired | 121 (36.2) | 133 (40.0) | 168 (50.5) | ||
| Unemployed | 28 (8.4) | 19 (5.7) | 16 (4.8) | ||
| Occupational disability | 34 (10.2) | 6 (1.8) | 9 (2.7) | ||
| Living status, N (%) | |||||
| Alone | 75 (22.5) | 33 (9.9) | 14 (4.2) | ||
| With the family | 251 (75.1) | 293 (88.0) | 314 (94.3) | <0.001 | <0.001 |
| Others | 8 (2.4) | 7 (2.1) | 5 (1.5) | ||
| Smoker, N (%) | 129 (38.6) | 112 (33.6) | 77 (23.1) | 0.18 | <0.001 |
| COPD severity, N (%) | |||||
| Mild | 46 (13.8) | 139 (41.7) | 31 (9.3) | <0.001 | 0.04 |
| Moderate | 188 (56.3) | 173 (52.0) | 183 (55.0) | ||
| Severe | 93 (27.8) | 19 (5.7) | 101 (30.3) | ||
| Very severe | 7 (2.1) | 2 (0.6) | 18 (5.4) | ||
Notes:
P-value resulting from chi-square test or Fisher’s exact test, as appropriate. Comparisons between patients and GPs and between patients and PULs were performed separately.
Abbreviations: GPs, general practitioners; PULs, pulmonologists.
Perception differences
Table 2 provides a visual representation (heatmap like) of the magnitude and direction of perception differences between patients (reference) and GPs or PULs. COPD was regarded as a major health problem by patients and physicians. The overall impact of COPD on QoL was similarly regarded by patients, GPs, and PULs in the cases considered having mild/moderate disease. However, for the severe/very severe cases, the patients perceived a greater impact than that perceived by PULs. For all symptoms, the perception differed between the patients and physicians. Interestingly, the misalignment direction of the perception varied depending on the symptoms considered. Cough was more frequently highlighted as being important by GPs and PULs than perceived by patients. Dyspnea or shortness of breath was perceived to be more important by PULs than perceived by the patients. In contrast, chest tightness, wheezing, and tiredness/fatigue were more frequently reported as being important by patients than perceived by GPs and PULs regardless of disease severity. No significant differences were observed for phlegm or sputum. Overall, physicians perceived most symptoms to be less bothersome to the patients compared to patients’ own perceptions (refer Graph 4S in the Supplementary materials).
Table 2.
Heat map expression of the magnitude of differences between patients’ perceptions reported by GPs and PULs vs those directly reported by the patients
| Disease severity | Patientsa (%) | GPs (%) | PULs (%) | ||
|---|---|---|---|---|---|
| COPD perception | MM | A major health problem or somewhat of a health problem | 88 | 89 | 93 |
| A minor health problem or not a problem at all | 12 | 11 | 7 | ||
| SVS | A major health problem or somewhat of a health problem | 99 | 91b | 95 | |
| A minor health problem or not a problem at all | 1 | 10b | 5 | ||
| Overall impact of COPD on QoL | MM | Not at all limited or slightly limited or somewhat limited | 62 | 69 | 65 |
| Very limited or completely limited | 38 | 31 | 35 | ||
| SVS | Not at all limited or slightly limited or somewhat limited | 26 | 76b | 49c | |
| Very limited or completely limited | 74 | 24b | 51c | ||
| Symptoms perception | MM | Presence of cough | 62 | 79c | 77c |
| SVS | 62 | 91b | 80c | ||
| MM | Presence of dyspnea/shortness of breath | 65 | 69c | 85c | |
| SVS | 83 | 71b | 94c | ||
| MM | Presence of phlegm/sputum | 53 | 65c | 57 | |
| SVS | 59 | 76b | 62 | ||
| MM | Presence of chest tightness | 28 | 13c | 20c | |
| SVS | 40 | 19b | 20c | ||
| MM | Presence of wheezing | 49 | 30c | 28c | |
| SVS | 56 | 29b | 34c | ||
| MM | Presence of tiredness/fatigue | 42 | 31c | 22c | |
| SVS | 54 | 38b | 34c |
Notes:
Reference group.
Test for statistical significance not performed due to the low number of SVS patients reported by GPs.
The comparison is statistically significant (P<0.05) compared to the reference group. The color green represents domains in which the values were statistically significantly higher in the patients. The color red represents those domains where the perceptions were higher in the physicians than in the patients.
Abbreviations: GPs, general practitioners; MM, mild/moderate; PULs, pulmonologists; QoL, quality of life; SVS, severe/very severe.
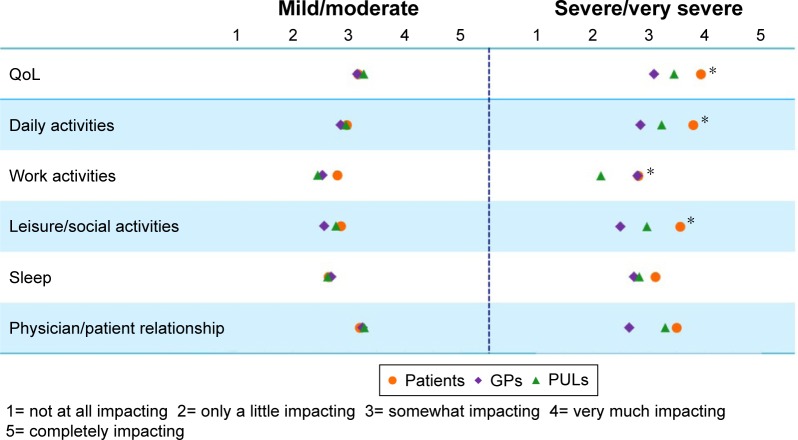
Perceptions related to QoL domains
The results about the impact of COPD on overall QoL and its domains are presented in Figure 1. There were no differences between the three groups for mild/moderate cases. However, in the severe/very severe cases, the patients assigned significantly higher scores than physicians to the impact of COPD on daily activities, work activities, leisure time activities, and overall QoL.
Figure 1.
COPD impact on QoL and its domains as perceived by the patients and by GPs and PULs answering about patients’ perception.
Notes: Mean values of the scores assigned to QoL and its domains stratified by disease severity. *Student’s t-test for the comparison between scores directly assigned by patients and those reported by PULs is statistically significant. t-tests for the comparisons between scores directly assigned by patients and those reported by GPs for the severe/very severe class were not performed due to the low number of GPs describing a patient with severe or very severe COPD.
Abbreviations: GPs, general practitioners; PULs, pulmonologists; QoL, quality of life.
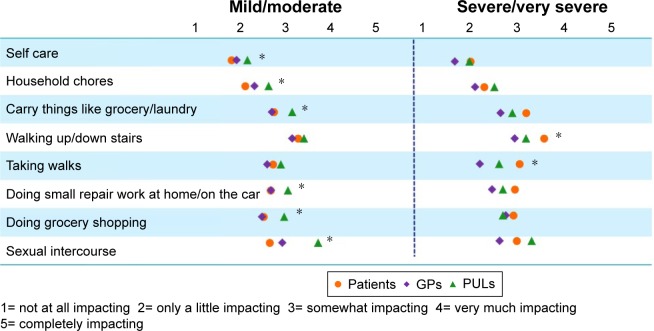
Results about the perception of daily activities subdomains are shown in Figure 2. There were minimal differences in the magnitude of the perception of the effect of COPD between patients and the physicians except for sexual intercourse. In fact, PULs assigned a statistically significantly higher score to the impact of COPD on sexual intercourse compared to the score reported by patients, particularly in mild/moderate COPD patients.
Figure 2.
COPD impact on daily activities subdomains as perceived by the patients and by GPs and PULs answering about patients’ perception.
Notes: Mean values of the scores assigned stratified by disease severity. *Student’s t-test for the comparison between scores directly assigned by patients and those reported by PULs is statistically significant. t-tests for the comparisons between scores directly assigned by patients and those reported by GPs for the severe/very severe class were not performed due to the low number of GPs describing a patient with severe or very severe COPD.
Abbreviations: GPs, general practitioners; PULs, pulmonologists.
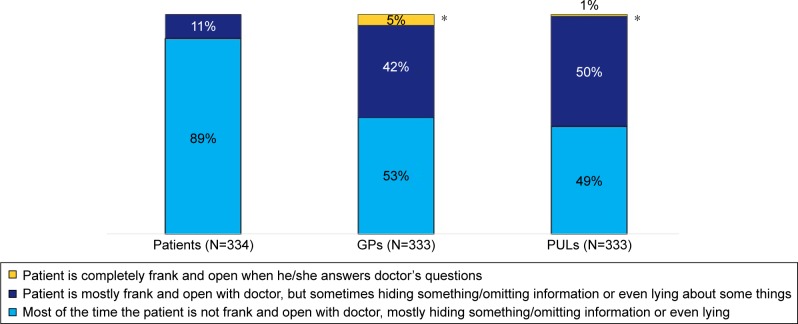
Perception toward the health care professional
Figure 3 presents the patients’ attitude during clinical visits. Almost 90% of the patients declared that most of the time they are not completely frank and open during interactions with physicians. Both GPs and PULs seemed to be aware of this issue but underestimated the extent, with 53% and 49% of GPs and PULs, respectively, declaring that most of the time patients are not frank and open during visits.
Figure 3.
Patients’ attitude during the visit with the health care professional of reference as perceived by patients, GPs, and PULs.
Note: *The comparison with patients directly answering the questionnaire is statistically significant based on the results from chi-square test.
Abbreviations: GPs, general practitioners; PULs, pulmonologists.
Discussion
This survey shows important differences between how COPD patients perceive various domains of their disease and the understanding that physicians, both GPs and PULs, have on the same domains. Furthermore, patients are frequently not frank during communications with physicians, a fact that is underestimated by doctors caring for COPD patients.
Participating patients
There have been several surveys of patients with COPD aimed at identifying their perception of different aspects of the disease.5,6,9–11 In general, these studies have found that patients have little knowledge on COPD itself, underestimate the severity of the disease and the importance of their symptoms, and tend to be undertreated compared to other diseases, such as hypertension.
The characteristics of the patients who participated in the present survey were quite similar to those from previous surveys in COPD patients.5,6,9–11 These surveys included a relatively high proportion of females and older nonworking exsmokers, who considered their disease to be of moderate severity. The similarity of the clinical characteristics of the patients in this survey compared to previous studies lends support to our findings and allows us to make informative comparisons. All previous surveys evaluated the perception of dyspnea, primarily during exertion. However, as we did in this study, only Molimard and Colthorpe11 evaluated “dyspnea” and “chest tightness” as separate symptoms. Interestingly, the two surveys found that the number of patients experiencing chest tightness was different from those patients experiencing dyspnea, suggesting that chest tightness is a symptom perceived differently from dyspnea. The clinical significance of “tightness” is unclear, and there was no way to find an explanation in a survey, but the results from these two studies indicate a need to explain the nature and significance of its presence.
Concordance and gaps between patients and doctors
To our knowledge, no previous studies or surveys have investigated and compared patients’ and physicians’ perception on COPD symptoms and QoL, simultaneously using “mirrored” questionnaires developed to explore exactly the same domains. Previous studies comparing doctors’ and patients’ perceptions were more focused on the management of disease, the preference of treatments and the utilization of resources and relied on instruments that included different questions.1,10–13
Miravitlles et al surveyed 450 patients paired with 77 PULs caring for them. The patients and their PULs agreed on the ranking of the first three impacting symptoms: breathlessness, fatigue, and cough. However, the scores assigned by the PULs were significantly higher for breathlessness and lower for fatigue and cough.1 Results from the present survey extend those findings by showing that PULs perceived the symptoms of fatigue and tiredness that have less impact on the patients than that directly perceived by the patients. Both PULs and GPs assigned more importance to the symptoms of breathlessness, cough, and phlegm than patients themselves did. In the present survey, physicians considered the domains related to leisure and social time activities were less impacted than patients did.
A telephone survey of ~1,000 patients with COPD and 1,000 GPs and PULs was conducted by Barr et al.10 The nature and number of questions were limited to the general perception of dyspnea, functional capacity, utilization of resources, and knowledge of the disease. The results showed that patients had limited knowledge on their disease and had functional limitation but underperceived the severity of their symptoms. The physicians had a relatively nihilistic approach to therapy and failed to adhere to guidelines. The current survey is more comprehensive and provides more information about specific domains of importance to the patients and the caregivers. Thus, whereas physicians believe that their patients’ perception of classical symptoms of COPD is very important to them, the patients assign more importance to activities related to leisure and social interaction.
An important new gap that deserves particular attention relates to the patients’ attitude toward the physicians during clinic visits. The vast majority of the patients (89%) stated that they “lied” or at least were “not honest” when interacting with their physician. Both GPs and PULs seemed to be aware of this issue, but they underestimated its magnitude. This occurred, even though patients and physicians regarded the impact of the patient–physician relationship as an important factor when evaluating the impact of COPD on QoL. We believe this existing gap is extremely important, because a lack of frankness between patients and their caregivers is a recipe for poor outcomes.
The picture emerging from the present survey reflects the differences that exist in how patients and physicians perceive the actual impact of COPD itself. Physicians overestimate the importance of dyspnea, cough, and sputum on their patients, perhaps because these are symptoms that are thought to be directly related to the disease. However, chest tightness and fatigue are symptoms not well appreciated by physicians, even though they are perceived as being very important by patients. Physicians understand that COPD affects certain domains of daily life such as work and exercise, but they have difficulties in understanding the impact that disease has on leisure time and social life. For physicians, it is easy to imagine that a patient affected by COPD could have difficulties in climbing up and down stairs, but it is less intuitive to imagine how much a patient can be impacted when he/she is not able to push his/her grandchildren on the swings. The fact that such symptoms are not frequently perceived to be as important by physicians reflects the existence of a communication gap between patients and their physicians.
Strength and weaknesses of the study
The main strength of the present survey is the use of questionnaires exploring exactly the same domains in patients and physicians, thus allowing effective comparisons between perceptions of a wide range of items. Also, the high number of subjects involved in the survey provides confidence to the generalizability of the study results. There also were some limitations. First, the online recruitment had the disadvantage of only assessing individuals with access to the internet. However, the patients’ characteristics are quite similar to those from previous surveys using different methods, suggesting that online surveys provide a similar type of sample population compared to personal or telephone interviews.5,10 Second, there was a relatively high proportion of women participating in the survey. However, real-world data obtained from GP and PUL medical records from IMS Health14 and a recent review of epidemiological and clinical data concluded that the paradigm of COPD is changing from a male-predominant disease to a disorder with a growing female prevalence.15 Third, another limitation is the patients’ self-reported diagnosis of COPD. However, most surveys previously conducted also selected COPD patients with a self-reported diagnosis.5,10,16,17 In addition, self-reporting information about chronic respiratory disease has a very good grade of agreement with information reported in the medical records.18 Fourth, it could be argued that the questionnaire has not been validated, but all of the surveys of COPD until now reported have used questionnaire developed ad hoc, using many questions similar to those included in the present survey. Finally, it could be said that patients and health care professionals were not paired. However, involving paired patients and physicians could have resulted in a selection bias itself, with physicians potentially selecting patients more frequently seeking care or with a more severe stage of the disease. Also, previous questionnaires have used similar unpaired methodology with validated results.10
Further research should center on the ways in which the perception gaps between patients and doctors could be decreased. Perhaps, group discussions involving all parties with frank interactions among all of the stake holders can provide the field with practical ways to address this problem.
Conclusion
This study shows that there are significant gaps between the perception of different domains of disease in patients with COPD and the understanding that the doctors caring for COPD patients have of their patients’ perception. This is particularly important in the areas of QoL and symptoms. Physicians must become aware of the impact on nonconventional domains that patients perceive as being importantly affected by COPD, so that they can be integrated into management plans. There is also insufficient frankness between patients and doctors that may be hindering the constructive interaction needed to maintain a healthy patient–doctor relationship. More open discussions between patients and physicians are needed in order to achieve better provision of health care.
Acknowledgments
This study was funded by Menarini. All authors meet the International Committee for Medical Journal Editors criteria for authorship.
Footnotes
Disclosure
BC, FB, MG, DS, CV, and AA served on the Scientific Advisory Board for the MIRROR survey. The Scientific Advisory Board members were not paid for authorship services. The authors report no other conflicts of interest in this work.
References
- 1.Miravitlles M, Ferrer J, Baró E, Lleonart M, Galera J. Differences between physician and patient in the perception of symptoms and their severity in COPD. Respir Med. 2013;107(12):1977–1985. doi: 10.1016/j.rmed.2013.06.019. [DOI] [PubMed] [Google Scholar]
- 2.Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 3.Vogelmeier C, Agusti A, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of Chronic Obstructive Pulmonary Disease (2017 Report) 2017. [Accessed March 20, 2017]. webpage on the Internet. Available from: http://goldcopd.org/gold-2017-global-strategy-diagnosis-management-prevention-copd/
- 4.Agusti A, Calverley PM, Celli B, et al. Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) investigators Characterisation of COPD heterogeneity in the ECLIPSE cohort. Respir Res. 2010;11:122. [Google Scholar]
- 5.Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2000: subjects’ perspective of Confronting COPD International Survey. Eur Respir J. 2002;20(4):799–805. doi: 10.1183/09031936.02.03242002. [DOI] [PubMed] [Google Scholar]
- 6.Barnes N, Calverley PM, Kaplan A, Rabe KF. Chronic obstructive pulmonary disease and exacerbations: patient insights from the global Hidden Depths of COPD survey. BMC Pulm Med. 2013;13:54. doi: 10.1186/1471-2466-13-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brien SB, Lewith GT, Thomas M. Patient coping strategies in COPD across disease severity and quality of life: a qualitative study. NPJ Prim Care Respir Med. 2016;26:16051. doi: 10.1038/npjpcrm.2016.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.European Pharmaceutical Market Research Association [webpage on the Internet] Code of Conduct 2017. [Accessed June 22, 2017]. Available from: http://www.ephmra.org/Code-of-Conduct-Support.
- 9.Barr RG, Celli BR, Mannino DM, et al. Comorbidities, patient knowledge, and disease management in a national sample of patients with COPD. Am J Med. 2009;122(4):348–355. doi: 10.1016/j.amjmed.2008.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barr RG, Celli BR, Martinez FJ, et al. Physician and patient perceptions in COPD: the COPD Resource Network Needs Assessment Survey. Am J Med. 2005;118(12):1415. doi: 10.1016/j.amjmed.2005.07.059. [DOI] [PubMed] [Google Scholar]
- 11.Molimard M, Colthorpe P. Inhaler devices for chronic obstructive pulmonary disease: insights from patients and healthcare practitioners. J Aerosol Med Pulm Drug Deliv. 2015;28(3):219–228. doi: 10.1089/jamp.2014.1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Menezes AM, Landis SH, Han MK, et al. Continuing to Confront COPD International Surveys: comparison of patient and physician perceptions about COPD risk and management. Int J Chron Obstruct Pulmon Dis. 2015;10:159–172. doi: 10.2147/COPD.S74315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hernandez P, Balter MS, Bourbeau J, Chan CK, Marciniuk DD, Walker SL. Canadian practice assessment in chronic obstructive pulmonary disease: respiratory specialist physician perception versus patient reality. Can Respir J. 2013;20(2):97–105. doi: 10.1155/2013/369019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Visentin E, Nieri D, Vagaggini B, Peruzzi E, Paggiaro P. An observation of prescription behaviors and adherence to guidelines in patients with COPD: real world data from October 2012 to September 2014. Curr Med Res Opin. 2016;32(9):1493–1502. doi: 10.1080/03007995.2016.1182900. [DOI] [PubMed] [Google Scholar]
- 15.Ohar J, Fromer L, Donohue JF. Reconsidering sex-based stereotypes of COPD. Prim Care Respir J. 2011;20(4):370–378. doi: 10.4104/pcrj.2011.00070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yin P, Ma Q, Wang L, et al. Chronic obstructive pulmonary disease and cognitive impairment in the Chinese elderly population: a large national survey. Int J Chron Obstruct Pulmon Dis. 2016;11:399–406. doi: 10.2147/COPD.S96237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vaske I, Kenn K, Keil DC, Rief W, Stenzel NM. Illness perceptions and coping with disease in chronic obstructive pulmonary disease: effects on health-related quality of life. J Health Psychol. 2016 Feb 29; doi: 10.1177/1359105316631197. Epub. [DOI] [PubMed] [Google Scholar]
- 18.Iversen L, Hannaford PC, Godden DJ, Price D. Do people self-reporting information about chronic respiratory disease have corroborative evidence in their general practice medical records? A study of intermethod reliability. Prim Care Respir J. 2007;16(3):162–168. doi: 10.3132/pcrj.2007.00013. [DOI] [PMC free article] [PubMed] [Google Scholar]