Abstract
Objective
Pressures for men to conform to a lean, muscular ideal have, in part, contributed to eating disorder and muscle dysmorphia symptoms, yet few programs have been developed and empirically evaluated to help men. The present study investigated the acceptability and efficacy of a cognitive dissonance-based (DB) intervention in reducing eating disorder and muscle dysmorphia risk factors in men with body dissatisfaction.
Method
Men were randomized to a 2-session DB intervention (n=52) or a waitlist control condition (n=60). Participants completed validated measures assessing eating disorder risk factors pre-intervention, post-intervention, and at 1-month follow-up.
Results
Program ratings indicated high acceptability. The DB condition demonstrated greater decreases in body-ideal internalization, dietary restraint, bulimic symptoms, drive for muscularity, and muscle dysmorphia symptoms compared to controls (p-values < .02; between-condition Cohen’s d = .30–1.11) from pre- to post-intervention. At one-month follow-up, the DB condition demonstrated significantly lower scores for all variables (p-values < .03; between-condition d = .29–1.16). Body-ideal internalization mediated intervention outcomes on bulimic and muscle dysmorphia symptoms.
Discussion
Results support the acceptability and efficacy of The Body Project: More Than Muscles up to one-month post-intervention and should be examined against active control conditions.
Keywords: eating disorder, muscle dysmorphia, men, dissonance, peer-led, intervention, body dissatisfaction
Although males represent up to 33% of all eating disorder (ED) cases (Hudson, Hiripi, Pope, & Kessler, 2007), men have traditionally been underrepresented in ED research (Strother, Lemberg, Stanford, & Turberville, 2012). Over recent decades, men have faced increasing social pressures to obtain an unrealistically lean and muscular physique (Jones & Morgan, 2010; Rodgers, Ganchou, Franko, & Chabrol, 2012). These pressures have, in part, contributed to body dissatisfaction and unhealthy eating and weight control behaviors among men, including both ED and muscle dysmorphia (MD) symptoms (Cafri et al., 2005; Leit, Gray, & Pope, 2002; Litt & Dodge, 2008; Tylka, 2011). Despite the impairment and distress associated with body dissatisfaction, EDs, and MD (Bramon-Bosch, Troop, & Treasure, 2000; Griffiths et al., 2016; Olivardia, Pope, & Hudson, 2000; Pope, Gruber, Choi, Olivardia, & Phillips, 1997), males are less likely to seek treatment than females, partially due to stigma (Griffiths et al., 2015; Striegel-Moore, Leslie, Petrill, Garvin, & Rosenheck, 2000). When men seek treatment, few programs have been developed to address their concerns. Therefore, well-accepted programs that target male-specific ED symptoms prior to disorder onset may be particularly beneficial to help reduce health disparities for this group.
Although eating and appearance-based disorders have complex etiologies, research supports the role that media depictions and pressures to pursue a lean and muscular (or mesomorphic) body have on eating and MD-related psychopathology. Media depictions of the masculine body ideal have become more muscular over time, illustrated by the unreasonably increasing muscle mass of boys’ action figures (Pope, Olivardia, Gruber, & Borowiecki, 1999) and by analyses of media images of males (Leit, Pope, & Gray, 2001). Importantly, these images of extremely low body fat and extreme muscle mass are rarely achievable without unhealthy approaches (Pope, Phillips, & Olivardia, 2000). Indeed, viewing mesomorphic media images is associated with greater drive for thinness and dieting frequency (Harrison & Cantor, 1997), and greater muscularity dissatisfaction in men (Leit et al., 2001).
Tylka’s (2011) expanded tripartite model posits that sociocultural influences contribute to both ED and muscularity psychopathology. This model suggests that pressures from media, along with pressures from friends, partners, and family to be mesomorphic lead to internalization of the mesomorphic ideal among men. The internalization of this mesomorphic ideal then contributes to dual pathways of dissatisfaction with muscularity and dissatisfaction with body fat, which then contribute to muscularity enhancement behaviors and disordered eating behaviors, respectively. Within the tripartite model, targeting body-ideal internalization within body-dissatisfied males would be important for reducing both ED symptoms and symptoms related to MD.
The Body Project (TBP) directly targets body-ideal internalization in young body-dissatisfied females using cognitive dissonance (Stice, Marti, Spoor, Presnell, & Shaw, 2008). The program was based on the dual pathway model of bulimic symptoms (Stice, 2001; Stice, Ziemba, Margolis, & Flick, 1996) and cognitive dissonance theory (Festinger & Carlsmith, 1959). Dissonance theory, applied to EDs, proposes that engaging in a series of activities arguing against the thin ideal helps increase dissonance or discomfort, which in turn promotes a reduction in internalization of the thin ideal and a reduction in ED risk factors. The Body Project has garnered impressive empirical support, with several independent labs replicating efficacious results in improving ED risk factors for young women post-intervention (Becker, Smith, & Ciao, 2005; Becker et al., 2010; Stice et al., 2008; Stice, Rohde, Gau, & Shaw, 2009; Stice, Shaw, Burton, & Wade, 2006) through 3 year follow-up (Stice et al., 2008; Stice, Rohde, Butryn, Shaw, & Marti, 2015). Reductions in the proposed intervention mechanism, thin-ideal internalization, partially mediate treatment effects among women (Seidel, Presnell, & Rosenfield, 2009; Stice, Marti, Rohde, & Shaw, 2011; Stice, Presnell, Gau, & Shaw, 2007).
Recently, our group developed and evaluated The PRIDE Body Project to target ED risk factors in sexual minority males (Brown & Keel, 2015). Results demonstrated significant and large effect-size reductions across ED risk factors compared to a waitlist control, post-treatment and 4-weeks post-treatment (Brown & Keel, 2015). Additionally, body-ideal internalization mediated the relationship between intervention condition and eating pathology (Brown & Keel, 2015). While these initial results were impressive, it is unclear whether these effects would generalize to men, regardless of sexual orientation.
To our knowledge, only one recently published study has examined TBP for men, regardless of sexual orientation. The Body Project 4 All (Kilpela et al., 2016), a mixed-gender version of TBP, found significant improvements in body fat, muscle, and overall body dissatisfaction for men compared to waitlist control at post-intervention, with effects largely maintained at 2- and 6-month follow-up. The authors did not find significant differences for body-ideal internalization or overall eating pathology. While these results support the adaptability and utility of TBP in a broader group of men, the authors did not examine MD symptoms. Thus, it is unknown if the program generalizes to these concerns.
Thus, the aim of the present study was to determine the acceptability and efficacy of adapting TBP for college-aged men with body dissatisfaction to target both ED symptoms and muscularity-related symptoms. Based on previous research, regarding acceptability, we hypothesized that we would observe: (1) at least 85% retention across the program and favorable acceptability ratings. Regarding efficacy, we hypothesized that: (2a) men in the DB condition would show significantly greater reductions in all ED-related outcome measures and muscularity-related outcomes over time compared to men in the waitlist control (WL) condition; and (2b) differences between conditions would be maintained at 4-week follow-up. We also hypothesized that: (3) the dissonance-based program’s impact on bulimic and MD symptoms would be mediated by reductions in mesomorphic body-ideal internalization.
METHODS
Participants and Procedures
Participants (N=112) were recruited from a large, public southern university and the local community. Our design represented a targeted prevention in which participants met the following inclusion criteria: (a) male, (b) 18–30 years old, (c) endorsed body image concerns (overvaluation of weight and/or shape or dissatisfaction with body weight, shape, or muscularity), and (d) did not meet criteria for a DSM-5 ED. The Institutional Review Board approved all study procedures. The majority of participants were currently pursuing an undergraduate (86.0%) or graduate degree (9.7%), with a minority (4.3%) coming from the surrounding community.
Eligibility phone screen
Interested participants completed an eligibility phone screen, which included the ED module of the Structured Clinical Interview for Axis-I Disorders (SCID-I; Spitzer, Williams, Gibbon, & First, 1995), modified for DSM-5. Participants also rated (1) how much body shape or weight influenced how they felt about themselves as a person and (2) how dissatisfied they were with their body shape, weight, or muscularity on a 1–10 scale. Scores ≥ 6 on either question met criteria. Participants could not have a current DSM-5 ED but could have ED symptoms (Becker, Bull, Schaumberg, Cauble, & Franco, 2008; Brown & Keel, 2015).
Overview and Study Flow
After providing informed consent, participants were randomly assigned to either the dissonance-based (DB) group intervention (n=52) or a waitlist (WL) condition (n=60) (see Figure 1). Participants who accepted randomization to condition completed baseline questionnaires after randomization (immediately prior to Session 1 in the DB condition and after being randomized in the WL condition). Questionnaires were repeated immediately post-intervention (DB condition)/after a one-week interval (WL) and 4-weeks post-intervention (DB condition)/after a 5-week interval (WL; see Figure 1).
Figure 1.
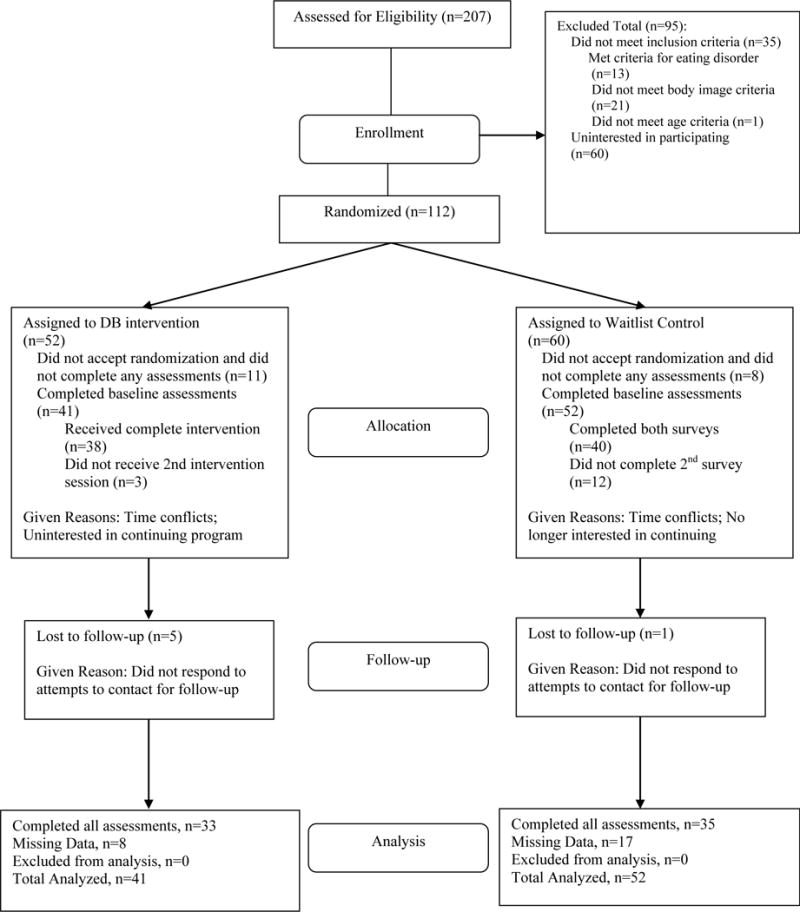
CONSORT chart detailing participant flow through the study.
The two 2-hour group sessions were separated by one week. Intervention groups included between 4–10 members each and were led by the investigator (TAB), a masters level clinician with previous experience co-facilitating DB group interventions (Brown & Keel, 2015), and 1–2 undergraduate peer male co-leaders (dependent on group size). Four different peer co-leaders facilitated 8 different intervention groups. Participants chose between receiving $20 compensation for completing all assessments or receiving course credit for participation. Compensation method did not differ between conditions (χ2(1)=0.60, p=.44).
Dissonance-Based Intervention
The Body Project: More than Muscles, was adapted from The PRIDE Body Project (Brown & Keel, 2015). Based on a community participatory research approach and our previous methods, drafts of the adapted program were submitted to members of the target population of males (n = 9) for feedback on relevance and wording, and materials were refined based on this information and findings from one pilot test group. Consistent with this approach, men enrolled in the pilot group developed the name for the program, “More than Muscles,” during an intervention body activism activity.
In Session 1, participants: (a) defined the “cultural ideal” male body type, (b) discussed the origin and perpetuation of the “cultural ideal,” including viewing images illustrating how TV/movie superheroes have changed over time, (c) brainstormed the costs of pursuing the “cultural ideal,” (d) participated in verbal challenges countering the mesomorphic ideal message, and (e) completed homework assignments (an email to a high school guy, two behavioral challenges, and a mirror exposure assignment). In Session 2, participants: (a) reviewed homework, (b) completed role plays to counter/discourage pursuit of the mesomorphic ideal, (c) listed ways to resist pressure to pursue this “cultural ideal” individually, as a group, and within the greater community (termed “body activism”), (d) brainstormed ways to resist future pressures to conform to the ideal, (e) discussed ways to challenge/avoid negative “body talk” statements, and (f) selected an exit exercise to continue challenging the cultural-ideal.
Intervention Adherence and Leader Competence
Peer co-leaders were trained using previously described methods (Brown & Keel, 2015). Intervention sessions were audiotaped, and five of the eight tapes were randomly selected for adherence and facilitator competence ratings (one group randomly selected for each co-leader). Competence ratings were completed by TAB, KJF, and DP, all of whom were trained on DB interventions by either Dr. Carolyn Becker or the first author. Adherence ratings were above 87% for all sessions (average rating=95%). Leader competence ratings fell in the above average/excellent range (graduate student clinician rating: 8.60/10; co-leaders M=7.25/10, range=5.60–8.20).
Measures
Treatment Acceptability
Treatment acceptability was assessed using four items on a 7-point Likert-type scale: (1) helpfulness in promoting a positive body image, (2) helpfulness in improving the participant’s own body image, (3) overall program satisfaction, and (4) likelihood of recommending the program to a friend (Brown & Keel, 2015). Cronbach’s alpha was .87.
Traditional ED Variables
Body-Ideal Internalization
Body-ideal internalization was measured through the Sociocultural Attitudes Towards Appearance Questionnaire-3 Internalization General subscale (SATAQ-3; Thompson, van den Berg, Roehrig, Guarda, & Heinberg, 2004). The SATAQ-3 has demonstrated strong psychometric properties among males (Karazsia & Crowther, 2008), and internal consistency within the present study ranged from α=.95–.97. Stability for the control group was r=.90.
Dietary Restraint
Dietary restraint was measured through the Restraint subscale of the Eating Disorder Examination-Questionnaire (EDE-Q; Fairburn & Beglin, 1994). Items were reframed to the past 7 days, reflecting the time course in the present study. Internal consistency for the EDE-Q Restraint subscale in the present study ranged from α=.81–.85 and the stability within the control group was r=.93.
Bulimic Symptoms
Bulimic symptoms were assessed through summing the diagnostic items from the EDE-Q over the past seven days (e.g., binge eating, compensatory behaviors, and overvaluation of weight and shape (Becker et al., 2008; Becker et al., 2006; Stice et al., 2006)). This composite has demonstrated strong psychometric properties in females (Stice et al., 2006) and adequate internal consistency (α=.72–.86) and 1-week test-retest reliability (r=.94) in sexual minority males (Brown & Keel, 2015). Internal consistency for the EDE-Q bulimic composite in the present study ranged from α=.62–.67 and stability within the control group was r=.67.
Muscularity-Oriented Variables
Muscle & Body Fat Dissatisfaction
The Male Body Attitudes Scale (MBAS; Tylka, Bergeron, & Schwartz, 2005) comprises 24 items assessed on a 6-point scale and includes Dissatisfaction with Body Fat and Dissatisfaction with Muscularity subscales. Previous research supports strong psychometric properties for the measure (Smith, Hawkeswood, Bodell, & Joiner, 2011; Tylka et al., 2005). Internal consistency for the MBAS in the present study ranged from α=.90–.92 for the Body Fat subscale and from α=.92–.95 for the Muscularity subscale. Stability in the control group was high for both subscales (r=.96 and r=.89).
Drive for Muscularity
Drive for muscularity was assessed through the Drive for Muscularity Scale (DMS; McCreary & Sasse, 2000). The DMS comprises 15 items, with higher scores indicating a stronger drive to be more muscular. The DMS has demonstrated good psychometric properties in males (McCreary & Sasse, 2000). Internal consistency for the DMS in the present study ranged from α=.89–.94, and stability for the control group was r=.90.
MD Symptoms
Symptoms of MD were assessed through the 13-item Muscle Dysmorphia Disorder Inventory (MDDI; Hildebrandt, Langenbucher, & Schlundt, 2004), which includes Drive for Size (DFS), Appearance Intolerance (AI) and Functional Impairment (FI) subscales. Notably, the MDDI was added after study initiation; thus, data are available for n=22 in the DB condition and n=34 in the WL condition. The MDDI has demonstrated strong psychometric properties among college men (Hildebrandt et al., 2004). Internal consistency in the present study was strong (total α=.84–.92, DFS α=.90–.94, AI α= .90–.93, FI α=.81–.85), and stability for the control group was high (total r=.88, DFS r=.91, AI r=.86, FI r=.84).
Analyses
Model Overview & Fitting
Intent-to-treat analyses were run using the Mixed Models module of the Statistical Package for the Social Sciences (SPSS, Version 23). All individuals who completed any assessments were included in analyses (see Figure 1); no data were available for participants who did not accept randomization. Level 1 modeled repeated measurements of the dependent variable nested within participants. Intervention condition and the interaction between condition and time were modeled at Level 2. Group was initially included in all models as a Level 2 covariate to adjust for non-independence1, but was removed if it was not a significant predictor of outcome (Singer & Willett, 2003). Full information maximum likelihood estimation was used to account for missing data (Schafer & Graham, 2002). Model fitting resulted in a random intercept fixed slope model with a nonlinear effect of time.
Mediation Analyses
Mediation models were conducted using bias-corrected bootstrapped confidence intervals (CIs) for indirect effects (Preacher & Hayes, 2008) to maximize power over traditional tests of indirect effects (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). This is consistent with our previous methodology and recommendations for examining mediation of treatment effects (Kraemer, Wilson, Fairburn, & Agras, 2002; Kaufman, Rohde, Seeley, Clarke, & Stice, 2005). One thousand bootstrap resamples tested the indirect effects of condition via the posited mediating variables (i.e., change in body-ideal internalization, baseline to post-intervention) on the dependent variables of interest (i.e., change in bulimic/MD symptoms from baseline to 4-week follow-up).
RESULTS
Baseline Characteristics
Table 1 describes demographic characteristics. Participants in the DB and WL conditions did not differ on age, ethnicity, sexual orientation identity, educational status, or current treatment for emotional problems (p-values >.14). Participants were approximately 20 years old (M(SD)=20.37(2.37), range=18–27) and the racial and ethnic breakdown was as follows: Caucasian (55.9%), Hispanic/Latino (17.2%), African American (9.7%), Asian (7.5%), and Other (9.7%). The majority of the sample identified as mostly or exclusively heterosexual (88.1%).
Table 1.
Demographic Characteristics
| Intervention (n=41) |
Control (n=52) |
Total (n=93) |
|
|---|---|---|---|
| Age | |||
| M (SD) | 20.20 (2.32) | 20.51 (2.42) | 20.37 (2.37) |
| Sexual Orientation Identity | n (%) | n (%) | n (%) |
| Exclusively Heterosexual | 31 (77.5) | 39 (75.0) | 70 (76.1) |
| Mostly Heterosexual | 6 (15.0) | 5 (9.6) | 11 (12.0) |
| More Heterosexual | 1 (2.5) | 2 (3.8) | 3 (3.3) |
| Equally Heterosexual and Gay | 0 (0) | 0 (0) | 0 (0) |
| More Gay | 0 (0) | 1 (1.9) | 1 (1.1) |
| Mostly Gay | 0 (0) | 3 (5.8) | 3 (3.3) |
| Exclusively Gay | 1 (2.5) | 1 (1.9) | 2 (2.2) |
| Does Not Identify with any Orientation | 1 (2.5) | 1 (1.9) | 2 (2.2) |
| Education Status | |||
| Enrolled in undergraduate | 38 (92.7) | 42 (80.8) | 80 (86.0) |
| Enrolled in graduate school | 2 (4.9) | 7 (13.5) | 9 (9.7) |
| Not in school | 1 (2.4) | 3 (5.8) | 4 (4.3) |
| In Current Psychological Treatment | |||
| Yes | 2 (4.9) | 6 (11.5) | 8 (8.6) |
| No | 39 (95.1) | 46 (88.5) | 85 (91.4) |
Acceptability and Homework Completion
Regarding participant flow, 207 men completed the eligibility phone screen for the study (see Figure 1). Of these, 83% were eligible (n=172). Of those eligible, 65% (n=112) consented and were randomized. Seventy-nine percent of participants in the DB condition (n=41) attended the first session and completed baseline assessments, while 87% (n=52) of WL participants completed baseline assessments.
Regarding acceptability, retention in the DB intervention from baseline to post-intervention was 93% (n=38) and was significantly better than retention over assessments in the WL condition (77%, n=40) (χ2(1)=4.33, p=.04). Compared to individuals who dropped out of the intervention (n=3/41), treatment completers (n=38/41) did not differ significantly on age, sexual orientation, or most baseline dependent variables (p-values >.15); however, those who dropped out of treatment were more likely to identify as African American (66.7% dropouts; p=.07, φ=.50) and have higher MBAS muscularity dissatisfaction (p=.06, d=1.12) at a trend level. The acceptability ratings for the program were highly favorable for all items (overall M=6.29/7.00; range=6.03–6.49). All participants completed at least two of the between-session activities, and 95% completed all activities.
Intervention Effects
Table 2 presents estimated marginal means for each outcome variable across time by condition. Table 3 presents HLM estimates for fixed effects and variance components for primary outcome variables.
Table 2.
Estimated Marginal Means for Outcome Variables at Each Time Point by Condition
| Baseline M (SE) |
Post-Intervention M (SE) |
4-week Follow-up M (SE) |
Between-Condition Cohen’s d (95 % CI) |
|||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Measure | DB n=41 |
WL n=52 |
DB n=41 |
WL n=52 |
DB n=41 |
WL n=52 |
Post | Follow-up |
| Eating Disorder Specific Outcomes | ||||||||
| SATAQ-General | 22.00 (1.52) |
23.04 (1.36) |
17.81** (1.54) |
23.51 (1.43) |
19.06* (1.58) |
23.63 (1.44) |
.61 (.16–1.06) |
.48 (.03–.93) |
| EDE-Q Restraint | 1.27 (0.31) |
2.07 (0.27) |
0.64** (0.31) |
2.05 (0.28) |
0.38** (0.31) |
2.10 (0.28) |
.76 (.30–1.22) |
.93 (.46–1.39) |
| EDE-Q Bulimic sxs | 5.53* (0.92) |
9.30 (0.83) |
3.55*** (0.93) |
9.80 (0.86) |
2.97*** (0.95) |
9.57 (0.86) |
1.11 (.63–1.59) |
1.16 (.68–1.64) |
| Muscularity Specific Outcomes | ||||||||
| MBAS – Body Fat | 3.56 (0.20) |
3.64 (0.18) |
3.08 (0.20) | 3.60 (0.18) |
3.00* (0.20) |
3.64 (0.18) |
.43 (.01–.88) |
.53 (.08–.99) |
| MBAS – Musc | 3.92 (0.18) |
3.85 (0.16) |
3.36 (0.19) |
3.80 (0.17) |
3.27** (0.19) |
3.98 (0.17) |
.39 (.06–.84) |
.66 (.20–1.12) |
| DMS | 3.58 (0.16) |
3.66 (0.14) |
2.96* (0.16) |
3.54 (0.15) |
2.86** (0.17) |
3.65 (0.15) |
.59 (.14–1.05) |
.78 (.32–1.24) |
| MDDI Total | 32.66 (2.20) |
33.03 (1.84) |
26.60* (2.21) |
34.10 (1.91) |
27.24* (2.24) |
34.76 (1.91) |
.58 (.12–1.03) |
.55 (.10–1.01) |
| MDDI - DFS | 13.34 (1.25) |
14.00 (1.05) |
11.68 (1.26) |
14.42 (1.09) |
11.70 (1.28) |
14.48 (1.09) |
.37 (.08–.82) |
.37 (.08–.82) |
| MDDI - AI | 8.49 (0.88) |
8.56 (0.74) |
5.73** (0.89) |
8.90 (0.77) |
5.96** (0.90) |
9.20 (0.77) |
.61 (.15–1.06) |
.62 (.16–1.07) |
| MDDI - FI | 10.83 (0.90) |
10.47 (0.75) |
9.22 (0.90) |
10.82 (0.78) |
9.61 (0.91) |
11.13 (0.78) |
.30 (.14–.75) |
.29 (.16–.73) |
Note. The number of participants for the MDDI was reduced from the full sample (DB n= 22, WL n=34). BSQ = DMS = Drive for Muscularity; EDE-Q Bulimic sxs = Eating Disorder Examination Questionnaire - Bulimic Composite; MBAS Body Fat = Male Body Attitudes Scale – Body Fat Subscale; MBAS Musc = Male Body Attitudes Scale – Muscularity Subscale; MDDI = Muscle Dysmorphia Disorder Inventory; SATAQ-General = Sociocultural Attitudes Towards Appearance Questionnaire – Internalization General subscale. Between group effects:
p<.05,
p<.01,
p<.001
Table 3.
HLM Estimates for Fixed Effects and Variance Components for Primary Outcome Variables
| Parameter | Fixed Effects | Variance | |||||||
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Intercept | Time | Condition | Group |
Time* Condition |
Time* Time |
Time* Time* Condition |
Within Person | Intercept | |
| γ (SE) |
γ (SE) |
γ (SE) |
γ (SE) |
γ (SE) |
γ (SE) |
γ (SE) |
γ (SE) |
γ (SE) |
|
| Eating Disorder Specific Outcomes | |||||||||
| SATAQ-General | 22.85*** (1.58) |
−0.87*** (0.20) |
0.09 (2.13) |
− | 0.96** (0.28) |
0.02*** (0.01) |
−0.02** (0.01) |
16.86*** (1.99) |
77.35*** (12.54) |
| EDE-Q Restraint | 1.03* (0.44) |
−0.13*** (0.03) |
0.69 (0.49) |
0.22* (0.11) |
0.12** (0.04) |
0.00*** (0.00) |
0.00* (0.00) |
0.34*** (0.04) |
1.91*** (0.31) |
| EDE-Q Bulimic sxs | 4.45** (1.32) |
−0.40** (0.12) |
3.29* (1.50) |
0.93** (0.32) |
0.50** (0.16) |
0.01** (0.00) |
−0.01** (0.00) |
5.73*** (0.68) |
15.33*** (2.70) |
| Muscularity-Oriented Outcomes | |||||||||
| MBAS – Body Fat | 3.65*** (0.20) |
−0.10*** (0.02) |
−0.01 (0.27) |
− | 0.09** (0.03) |
0.00*** (0.00) |
0.00** (0.00) |
0.18*** (0.02) |
1.43*** (0.22) |
| MBAS – Musc | 4.03*** (0.19) |
−0.11*** (0.02) |
−0.17 (0.26) |
− | 0.10** (0.03) |
0.00*** (0.00) |
−0.00* (0.00) |
0.24*** (0.03) |
1.14*** (0.18) |
| DMS | 3.71*** (0.17) | −0.13*** (0.02) | −0.03 (0.22) |
− | 0.10** (0.03) |
0.00*** (0.00) | 0.00** (0.00) |
0.22*** (0.25) | 0.81*** (0.13) |
| MDDI Total | 33.88*** (2.28) |
−1.25*** (0.27) |
−1.06 (2.97) |
− | 1.47*** (0.36) |
0.03*** (0.01) |
−0.03*** (0.01) |
17.39*** (2.55) |
97.24*** (19.47) |
| MDDI - DFS | 13.67*** (1.30) |
−0.34* (0.16) |
0.24 (1.69) |
− | 0.43* (0.21) |
0.01┼ (0.00) |
−0.01 (0.01) |
5.91*** (0.87) |
31.20*** (6.29) |
| MDDI - AI | 9.05*** (0.93) |
−0.57*** (0.12) |
−0.56 (1.20) |
− | 0.64*** (0.16) |
0.01*** (0.00) |
−0.02** (0.00) |
3.65*** (0.53) |
14.75*** (3.02) |
| MDDI - FI | 11.15*** (0.93) |
−0.33** (0.10) |
−0.75 (1.21) |
− | 0.40** (0.14) |
0.01** (0.00) |
−0.01** (0.00) |
2.48*** (0.36) |
16.64*** (3.31) |
Note. DMS = Drive for Muscularity; EDE-Q Bulimic sxs = Eating Disorder Examination Questionnaire - Bulimic Composite; MBAS Body Fat = Male Body Attitudes Scale – Body Fat Subscale; MBAS Musc = Male Body Attitudes Scale – Muscularity Subscale; MDDI = Muscle Dysmorphia Disorder Inventory; SATAQ-General = Sociocultural Attitudes Towards Appearance Questionnaire – Internalization General subscale.
= .05,
p<.05,
p<.01,
p<.001.
Traditional ED Variables
Body-Ideal Internalization
Results for the SATAQ demonstrated a significant effect of time (b=−0.87, t=−4.36, p<.001), indicating that body-ideal internalization decreased over time across conditions. A significant Condition X Time interaction (b=0.97, t=3.47, p=.001; see Table 3), indicated differences in the trajectory of body-ideal internalization over time between intervention conditions. Consistent with hypotheses, the DB condition demonstrated significantly lower SATAQ scores compared to WL post-intervention (p=.008, between-condition d=0.61; see Table 2) and these effects were maintained at 4-week follow-up (p=.04, between-condition d=0.48).
Dietary Restraint
Results for the EDE-Q Restraint subscale revealed a significant reduction over time for all participants (b=−0.12, t=−4.37, p<.001) and group (b=0.22, t=2.06, p=.04). As predicted, the Condition X Time interaction was significant (b=0.12 t=2.99, p=.003; see Table 3). The DB group demonstrated significantly lower EDE-Q Restraint scores compared to WL post-intervention (p=.005, between-condition d=0.76; see Table 2), and these gains were maintained at 4-week follow-up (p=.001, between-condition d=0.93). Demonstrating a meaningful reduction, the DB group’s scores were reduced from the 65th percentile for undergraduate men at baseline to the 50th percentile post-intervention and the 35th–40th percentile at follow-up (Lavender, De Young, & Anderson, 2010).
Bulimic Symptoms
Results for the EDE-Q bulimic symptoms composite revealed a significant effect of time (b=−0.40, t=−3.42, p=.001) and group (b=0.93, t=2.92, p=.004). A significant Condition X Time interaction (b=0.51, t=3.08, p=.003; see Table 3) indicated differences in the trajectory of bulimic symptoms across conditions over time. There were condition differences at baseline, with the DB group having lower levels of bulimic symptoms (p=.01). The DB condition demonstrated significantly lower EDE-Q bulimic symptoms compared to WL post-intervention (p<.001, between-condition d=1.11; see Table 2) and at 4-week follow-up (p<.001, between-condition d=1.16). There was a 40–50% reduction in the DB group’s bulimic symptom score from baseline to post-intervention and follow-up (see Table 2).
Muscularity-Oriented Variables
Dissatisfaction with Body Fat and Muscularity
Results from the MBAS – Body Fat subscale model demonstrated a significant reduction in body fat dissatisfaction for all participants (b=−0.10, t=−4.76, p<.001). A significant Condition X Time interaction (b=0.09, t=3.14, p=.002) indicated a steeper decline in scores over time for the DB condition compared to WL (see Table 3). Comparison of means demonstrated that conditions did not statistically differ post-intervention (p=.06, between-condition d=0.43; see Table 2); however, at 4-week follow-up, the DB condition demonstrated significantly lower MBAS – Body Fat scores than WL (p=.02, between-condition d=0.53). Results for the MBAS – Muscularity subscale mirrored those for the MBAS – Body Fat subscale (see Tables 2 & 3).
Drive for Muscularity
Results for the DMS demonstrated a significant reduction in drive for muscularity over time (b=−0.13, t=−5.58, p<.001). As hypothesized, a significant Condition X Time interaction (b=0.10, t=3.23, p=.002; see Table 3) reflected that the DB condition demonstrated significantly lower DMS scores compared to WL post-intervention (p=.01, between-condition d=0.59; see Table 2). These effects were maintained 4-weeks later, with the DB condition reporting lower DMS scores compared to WL (p=.001, between-condition d=0.78). Scores for the DB condition were one standard deviation (SD) above the mean for a community sample of males at baseline (M(SD) = 2.69(.85); McCreary, Sasse, Saucier, & Dorsch, 2004) and were reduced to just above the mean at post-intervention and follow-up.
MD Symptoms
Results for the MDDI demonstrated a significant effect of time (b=−1.25, t=−4.68, p<.001) and a significant Condition X Time interaction (b=1.47, t=4.08, p<.001; see Table 3). Post-intervention, the DB condition demonstrated significant decreases in MD symptoms compared to WL (p=.01, between-condition d=0.58; see Table 2), with these differences maintained at 4-week follow-up (p=.01, between-condition d=0.55).
Models were also run for the subscales of the MDDI (see Tables 2–3). While all models demonstrated significant Condition X Time interactions, only MDDI-AI scores were significantly reduced in the DB condition compared to WL at post-intervention (p=.009, between-condition d=0.61) and follow-up (p=.008, between-condition d=0.62). Notably, MDDI-AI scores for the DB condition were one SD above the mean for gym-going males at baseline (M(SD) = 6.12(2.50); Hildebrandt, Langenbucher, Schlundt, 2004) and were reduced to the mean of gym-going males at post-intervention and follow-up.
Mediation Analyses
Table 4 presents mediation analyses, including indirect effects, bias-corrected confidence intervals, and the significance of direct paths. Body-ideal internalization partially mediated the effect of condition on both bulimic symptoms and MD symptoms.
Table 4.
Tests of Mediation: Examination of Indirect Effects, Bias-Corrected 95% Confidence Intervals (CIs), and Direct Paths
| Path
|
||||||
|---|---|---|---|---|---|---|
| Indirect effect | 95% CI | a | b | c | c’ | |
|
|
||||||
| Indirect path | β | β(SD) | β(SD) | β(SD) | β(SD) | |
| Condition → Body-Ideal Internalization → Bulimic Symptoms | −0.87 | −1.92 to −0.27 | −4.51(1.57)** | 0.19(0.07)* | −2.99(0.97)** | −2.12(0.99)* |
| Condition → Body-Ideal Internalization → Muscle Dysmorphia Symptoms | −2.09 | −4.68 to −0.37 | −4.90(1.99)* | 0.43(0.16)** | −7.20 (2.17)** | −5.12(2.17)* |
Note. Body-Ideal Internalization (mediator) = change in Sociocultural Attitudes Towards Appearance Questionnaire – Internalization General subscale from baseline to post-intervention; Bulimic Symptoms (dependent variable) = change in Eating Disorder Examination – Questionnaire Bulimic Symptom Composite from baseline to 4-week follow-up; Muscle Dysmorphia Symptoms (dependent variable) = change in Muscle Dysmorphia Disorder Inventory - Total score from baseline to 4-week follow-up.
a = independent variable (condition) to mediator (body-ideal internalization); b = direct effect of mediator (internalization) on dependent variable (bulimic/muscle dysmorphia symptoms); c = total effect of independent variable (condition) on dependent variable (bulimic/muscle dysmorphia symptoms); c′= direct effect of independent variable (condition) on dependent variable (bulimic/muscle dysmorphia symptoms).
p < .05,
p < .01,
p < .001.
DISCUSSION
The present study examined the acceptability and efficacy of an adapted dissonance-based program, The Body Project: More than Muscles, for men with elevated body dissatisfaction. We observed a high retention rate and favorable acceptability ratings. Consistent with evaluations of similar interventions (Becker et al., 2005; Becker et al., 2010; Brown & Keel, 2015; Stice et al., 2008; Stice et al., 2009; Stice et al., 2006), participants randomized to the DB condition reported significant reductions in ED risk factors and symptoms and maintained these reductions at 4-week follow-up relative to waitlist. Novel to this study, we also observed reductions in some MD risk factors and symptoms across time. Importantly, mediation analyses suggest that the observed reductions in ED and MD symptoms were at least partially due to changes in body-ideal internalization, extending prior cross-sectional findings that body-ideal internalization is associated with increased ED and MD symptoms (Tylka, 2011) in an experimental design.
Our high intervention retention rate suggests the intervention had high relevance for men enrolled. Acceptability ratings and homework completion were also high, potentially reflecting the relevance of muscularity concerns for male body image (Murray, Griffiths, & Mond, 2016). However, approximately a third of those eligible chose not to not enroll in the study, suggesting that the intervention may not be relevant for all men high in body dissatisfaction. Reluctance to participate may be partly due to stigma around body image and eating concerns for men (Raisanen & Hunt, 2014). African American men tended to be more likely to drop out, raising concerns that our adaptation of materials does not address concerns that may be unique to African American men. Replication of this effect is needed.
We observed clinically meaningful reductions in ED risk factors and bulimic symptoms, consistent with previous work in college-aged men and women (Becker et al., 2005; Becker et al., 2010; Brown & Keel, 2015; Kilpela et al., 2016; Stice et al., 2008; Stice et al., 2009; Stice et al., 2006). Effect sizes for the present study were comparable to those in the Body Project 4 All (Kilpela et al., 2016); of note, our study produced slightly lower effects for muscularity and body fat dissatisfaction (current study: d=.44–.66; Kilpela et al., 2016: d =.55–.79), and slightly higher effects for the EDE-Q (current study: d=.76–1.16; Kilpela et al., 2016: d=.31–.62). Effect sizes for the current study were somewhat smaller than our intervention adapted for sexual minority men (Brown & Keel, 2015); potentially, our prior trial was more successful in establishing a sense of community and addressing concerns specific to sexual minority men than the current trial in men more broadly. However, this interpretation is inconsistent with our acceptability ratings and retention rate. Future iterations of this program may benefit from continued feedback from stakeholders, particularly those with high muscularity dissatisfaction, given the tendency for these men to drop out of the program. Finally, our smaller effect sizes may represent floor effects as we observed lower baseline scores than our previous study (Brown & Keel, 2015).
Results extend previous research on DB ED interventions for men to variables related to MD symptoms. This is particularly promising as there are currently no empirically-supported interventions for MD. Although participants were not recruited based on MDDI scores, baseline subscale scores fell within the range of muscle-concerned and muscle dysmorphic weightlifters (Hildebrandt et al., 2006). While the program did not improve symptoms of functional impairment associated with MD, the program did improve appearance intolerance, an indicator of body-related anxiety and exposure avoidance. These improvements may be a result of the behavioral experiment activities. The lack of improvement on Drive for Size and Functional Impairment subscales imply that future iterations of the program could better target these symptoms. Importantly, between-condition effect sizes for several MD variables were comparable to those observed for ED variables, with the largest effect size observed for drive for muscularity. While MD is not currently categorized as an ED, both conditions share similar symptoms, including excessive exercise and body checking/avoidance (Murray et al., 2012; Olivardia, 2001). Findings provide preliminary experimental evidence that similar risk processes, including internalization of the mesomorphic ideal, are involved in disordered eating and MD symptoms, consistent with the expanded tripartite model for men (Tylka, 2011). Replications using more comprehensive tests of mediation in larger-scale trials are needed. Future research in body-dissatisfied males should consider both outcomes in order to continue to elucidate shared and divergent risk pathways.
The present study benefited from the use of a randomized controlled trial design and a 4-week follow-up to evaluate the short-term maintenance of effects. Additional strengths include sophisticated handling of missing and non-independent data and the use of measures with solid psychometric properties. Despite these strengths, there are some notable limitations. First, given the lack of an active control condition, we cannot rule out placebo effects. Future studies should examine the program compared to an alternative treatment. Further, it is unknown if the efficacy of the program extends beyond one month post-intervention. While our use of peer co-leaders capitalized on healthy peer modeling, increasing the relevance to our target group, we observed significant heterogeneity in peer co-leader competence. While this likely models “real world” effects, future effectiveness studies should employ strategies to bolster competence and prevent facilitator drift. We had reduced power in examining MD symptoms; however, we were still able to detect some changes.
In sum, results provide initial support for the acceptability and efficacy of The Body Project: More Than Muscles for men with body image concerns. Results and engagement within the present study are particularly encouraging given that men are less likely to seek treatment for ED and MD problems (Griffiths et al., 2015; Striegel-Moore et al., 2000) despite the clinical significance of EDs and MD in men (Griffiths et al., 2016; Olivardia et al., 2000). Results from the present study bolster empirical support for the efficacy of DB ED prevention programs and extend previous research by focusing on ED and muscularity-related outcome variables within an underrepresented group. Findings also support the importance of body-ideal internalization in models of risk among body-dissatisfied males and contribute to the growing literature on risk for EDs and MD in men. The Body Project: More Than Muscles represents a viable alternative to the Body Project 4 All for universities and programs that wish to offer efficacious programs for men and women separately. Future research would benefit from a head to head comparison between mixed-gender and single sex groups. Findings from this research have the potential to help reduce stigma around body image concerns for males and help improve care for a group that has been overlooked for far too long.
Acknowledgments
Data collection and manuscript preparation were supported by the Global Foundation for Eating Disorders and the P.E.O. Scholar Award, and funding from the National Institute of Mental Health (F31MH105082, PI: Forney). We are incredibly grateful to Scott Boatwright, Kevin Isserman, Matthew McCarthy, Jared Mugfor, Alosha Parfyonov, Krishan Patel, and Ilyssa Rosenzweig for their assistance on the project. We would also like to thank everyone involved with The Body Project, including Eric Stice and Carolyn Becker for their support in our adaptation of this program.
Footnotes
Parts of this manuscript were presented at the International Conference on Eating Disorders, San Francisco, California, May 2016.
Peer co-leader did not significantly predict any outcome variables, with the exception of bulimic symptoms (p=.01). For bulimic symptoms, two co-leaders were associated with higher baseline scores and significantly greater decreases in bulimic symptoms over time compared to the other co-leaders (p-values <.03). Fit statistics favored models with group (AICC: 1362.6) versus leader (AICC: 1364.7) as a covariate. Thus, effects may be more attributable to group membership.
References
- Becker CB, Bull S, Schaumberg K, Cauble A, Franco A. Effectiveness of peer-led eating disorders prevention: a replication trial. Journal of Consulting and Clinical Psychology. 2008;76:347. doi: 10.1037/0022-006X.76.2.347. [DOI] [PubMed] [Google Scholar]
- Becker CB, Smith LM, Ciao AC. Reducing eating disorder risk factors in sorority members: A randomized trial. Behavior Therapy. 2005;36:245–253. doi: 10.1016/S0005-7894(05)80073-5. [DOI] [Google Scholar]
- Becker CB, Smith LM, Ciao AC. Peer-facilitated eating disorder prevention: A randomized effectiveness trial of cognitive dissonance and media advocacy. Journal of Counseling Psychology. 2006;53:550. doi: 10.1037/0022-0167.53.4.550. [DOI] [Google Scholar]
- Becker CB, Wilson C, Williams A, Kelly M, McDaniel L, Elmquist J. Peer-facilitated cognitive dissonance versus healthy weight eating disorders prevention: A randomized comparison. Body Image. 2010;7:280–288. doi: 10.1016/j.bodyim.2010.06.004. [DOI] [PubMed] [Google Scholar]
- Bramon-Bosch E, Troop NA, Treasure JL. Eating disorders in males: a comparison with female patients. European Eating Disorders Review. 2000;8:321–328. 10.1002/1099-0968/(200008)8:4<321::AID-ERV355>3.0.CO;2-G. [Google Scholar]
- Brown TA, Keel PK. A randomized controlled trial of a peer co-led dissonance-based eating disorder prevention program for gay men. Behaviour Research and Therapy. 2015;74:1–10. doi: 10.1016/j.brat.2015.08.008. [DOI] [PubMed] [Google Scholar]
- Cafri G, Thompson JK, Ricciardelli L, McCabe M, Smolak L, Yesalis C. Pursuit of the muscular ideal: Physical and psychological consequences and putative risk factors. Clinical Psychology Review. 2005;25:215–239. doi: 10.1016/j.cpr.2004.09.003. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16:363–370. [PubMed] [Google Scholar]
- Festinger L, Carlsmith JM. Cognitive consequences of forced compliance. The Journal of Abnormal and Social Psychology. 1959;58:203. doi: 10.1037/h0041593. [DOI] [PubMed] [Google Scholar]
- Griffiths S, Hay P, Mitchison D, Mond JM, McLean SA, Rodgers B, Paxton SJ. Sex differences in the relationships between body dissatisfaction, quality of life and psychological distress. Australian and New Zealand Journal of Public Health. 2016;40:518–522. doi: 10.1111/1753-6405.12538. [DOI] [PubMed] [Google Scholar]
- Griffiths S, Mond JM, Li Z, Gunatilake S, Murray SB, Sheffield J, Touyz S. Self-stigma of seeking treatment and being male predict an increased likelihood of having an undiagnosed eating disorder. International Journal of Eating Disorders. 2015;48:775–778. doi: 10.1002/eat.22413. [DOI] [PubMed] [Google Scholar]
- Harrison K, Cantor J. The relationship between media consumption and eating disorders. Journal of Communication. 1997;47:40–67. doi: 10.1111/j.1460-2466.1997.tb02692.x. [DOI] [Google Scholar]
- Hildebrandt T, Langenbucher J, Schlundt DG. Muscularity concerns among men: development of attitudinal and perceptual measures. Body Image. 2004;1:169–181. doi: 10.1016/j.bodyim.2004.01.001. [DOI] [PubMed] [Google Scholar]
- Hildebrandt T, Schlundt D, Langenbucher J, Chung T. Presence of muscle dysmorphia symptomology among male weightlifters. Comprehensive Psychiatry. 2006;47:127–135. doi: 10.1016/j.comppsych.2005.06.001. [DOI] [PubMed] [Google Scholar]
- Hudson JI, Hiripi E, Pope HG, Jr, Kessler RC. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biological Psychiatry. 2007;61:348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones W, Morgan J. Eating disorders in men: A review of the literature. Journal of Public Mental Health. 2010;9:23–31. doi: 10.5042/jpmh.2010.0326. [DOI] [Google Scholar]
- Karazsia BT, Crowther JH. Psychological and behavioral correlates of the SATAQ-3 with males. Body Image. 2008;5:109–115. doi: 10.1016/j.bodyim.2007.08.004. [DOI] [PubMed] [Google Scholar]
- Kaufman NK, Rohde P, Seeley JR, Clarke GN, Stice E. Potential mediators of cognitive-behavioral therapy for adolescents with comorbid major depression and conduct disorder. Journal of Consulting and Clinical Psychology. 2005;73:38. doi: 10.1037/0022-006X.73.1.38. [DOI] [PubMed] [Google Scholar]
- Kilpela LS, Blomquist K, Verzijl C, Wilfred S, Beyl R, Becker CB. The body project 4 all: A pilot randomized controlled trial of a mixed-gender dissonance-based body image program. International Journal of Eating Disorders. 2016;49:591–602. doi: 10.1002/eat.22562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Lavender JM, De Young KP, Anderson DA. Eating Disorder Examination Questionnaire (EDE-Q): norms for undergraduate men. Eating Behaviors. 2010;11:119–121. doi: 10.1016/j.eatbeh.2009.09.005. [DOI] [PubMed] [Google Scholar]
- Leit RA, Gray JJ, Pope HG., Jr The media’s representation of the ideal male body: a cause for muscle dysmorphia? International Journal of Eating Disorders. 2002;31:334–338. doi: 10.1002/eat.10019. [DOI] [PubMed] [Google Scholar]
- Leit RA, Pope HG, Jr, Gray JJ. Cultural expectations of muscularity in men: the evolution of playgirl centerfolds. International Journal of Eating Disorders. 2001;29:90–93. doi: 10.1002/1098-108x(200101)29:1<90::aid-eat15>3.0.co;2-f. 10.1002/1098-108X(200101)29:1<90::AID-EAT15>3.0.CO;2-F. [DOI] [PubMed] [Google Scholar]
- Litt D, Dodge T. A longitudinal investigation of the Drive for Muscularity Scale: predicting use of performance enhancing substances and weightlifting among males. Body Image. 2008;5:346–351. doi: 10.1016/j.bodyim.2008.04.002. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7:83–104. doi: 10.1037/1082-989X.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCreary DR, Sasse DK. An exploration of the drive for muscularity in adolescent boys and girls. Journal of American College Health. 2000;48:297–304. doi: 10.1080/07448480009596271. [DOI] [PubMed] [Google Scholar]
- McCreary DR, Sasse DK, Saucier DM, Dorsch KD. Measuring the Drive for Muscularity: Factorial Validity of the Drive for Muscularity Scale in Men and Women. Psychology of Men & Masculinity. 2004;5:49. doi: 10.1037/1524-9220.5.1.49. [DOI] [Google Scholar]
- Murray SB, Griffiths S, Mond JM. Evolving eating disorder psychopathology: conceptualising muscularity-oriented disordered eating. The British Journal of Psychiatry. 2016;208:414–415. doi: 10.1192/bjp.bp.115.168427. [DOI] [PubMed] [Google Scholar]
- Murray SB, Rieger E, Hildebrandt T, Karlov L, Russell J, Boon E, Touyz SW. A comparison of eating, exercise, shape, and weight related symptomatology in males with muscle dysmorphia and anorexia nervosa. Body Image. 2012;9:193–200. doi: 10.1016/j.bodyim.2012.01.008. [DOI] [PubMed] [Google Scholar]
- Olivardia R. Mirror, mirror on the wall, who’s the largest of them all? The features and phenomenology of muscle dysmorphia. Harvard Review of Psychiatry. 2001;9:254–259. doi: 10.1080/10673220127900. [DOI] [PubMed] [Google Scholar]
- Olivardia R, Pope HG, Jr, Hudson JI. Muscle dysmorphia in male weightlifters: a case-control study. American Journal of Psychiatry. 2000;157:1291–1296. doi: 10.1176/appi.ajp.157.8.1291. [DOI] [PubMed] [Google Scholar]
- Pope H, Phillips KA, Olivardia R. The Adonis complex: The secret crisis of male body obsession. Simon and Schuster; 2000. [Google Scholar]
- Pope HG, Jr, Gruber AJ, Choi P, Olivardia R, Phillips KA. Muscle dysmorphia. An underrecognized form of body dysmorphic disorder. Psychosomatics. 1997;38:548–557. doi: 10.1016/S0033-3182(97)71400-2. [DOI] [PubMed] [Google Scholar]
- Pope HG, Jr, Olivardia R, Gruber A, Borowiecki J. Evolving ideals of male body image as seen through action toys. International Journal of Eating Disorders. 1999;26:65–72. doi: 10.1002/(SICI)1098-108X(199907)26:1<65::AID-EAT8>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:879–891. doi: 10.3758/BRM.40.3.879. [DOI] [PubMed] [Google Scholar]
- Raisanen U, Hunt K. The role of gendered constructions of eating disorders in delayed help-seeking in men: a qualitative interview study. BMJ Open. 2014;4:e004342. doi: 10.1136/bmjopen-2013-004342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers RF, Ganchou C, Franko DL, Chabrol H. Drive for muscularity and disordered eating among French adolescent boys: a sociocultural model. Body Image. 2012;9:318–323. doi: 10.1016/j.bodyim.2012.03.002. [DOI] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological Methods. 2002;7:147. doi: 10.1037/1082-989X.7.2.147. [DOI] [PubMed] [Google Scholar]
- Seidel A, Presnell K, Rosenfield D. Mediators in the dissonance eating disorder prevention program. Behaviour Research and Therapy. 2009;47:645–653. doi: 10.1016/j.brat.2009.04.007. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. Oxford university press; 2003. [DOI] [Google Scholar]
- Smith AR, Hawkeswood SE, Bodell LP, Joiner TE. Muscularity versus leanness: an examination of body ideals and predictors of disordered eating in heterosexual and gay college students. Body Image. 2011;8:232–236. doi: 10.1016/j.bodyim.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer RL, Williams JB, Gibbon M, First MB. Structured clinical interview for DSM-IV (SCID) New York: Biometrics Research. 1995 doi: 10.1001/archpsyc.1992.01820080032005. [DOI] [PubMed] [Google Scholar]
- Stice E. A prospective test of the dual-pathway model of bulimic pathology: mediating effects of dieting and negative affect. Journal of Abnormal Psychology. 2001;110:124. doi: 10.1037/0021-843X.110.1.124. [DOI] [PubMed] [Google Scholar]
- Stice E, Marti CN, Rohde P, Shaw H. Testing mediators hypothesized to account for the effects of a dissonance-based eating disorder prevention program over longer term follow-up. Journal of Consulting and Clinical Psychology. 2011;79:398–405. doi: 10.1037/a0023321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Marti CN, Spoor S, Presnell K, Shaw H. Dissonance and healthy weight eating disorder prevention programs: long-term effects from a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2008;76:329–340. doi: 10.1037/0022-006X.76.2.329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Presnell K, Gau J, Shaw H. Testing mediators of intervention effects in randomized controlled trials: An evaluation of two eating disorder prevention programs. Journal of Consulting and Clinical Psychology. 2007;75:20–32. doi: 10.1037/0022-006X.75.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Butryn ML, Shaw H, Marti CN. Effectiveness trial of a selective dissonance-based eating disorder prevention program with female college students: Effects at 2-and 3-year follow-up. Behaviour Research and Therapy. 2015;71:20–26. doi: 10.1016/j.brat.2015.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Rohde P, Gau J, Shaw H. An effectiveness trial of a dissonance-based eating disorder prevention program for high-risk adolescent girls. Journal of Consulting and Clinical Psychology. 2009;77:825–834. doi: 10.1037/a0016132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Shaw H, Burton E, Wade E. Dissonance and healthy weight eating disorder prevention programs: a randomized efficacy trial. Journal of Consulting and Clinical Psychology. 2006;74:263–275. doi: 10.1037/0022-006X.74.2.263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Ziemba C, Margolis J, Flick P. The dual pathway model differentiates bulimics, subclinical bulimics, and controls: Testing the continuity hypothesis. Behavior Therapy. 1996;27:531–549. doi: 10.1016/S0005-7894(96)80042-6. [DOI] [Google Scholar]
- Striegel-Moore RH, Leslie D, Petrill SA, Garvin V, Rosenheck RA. One-year use and cost of inpatient and outpatient services among female and male patients with an eating disorder: evidence from a national database of health insurance claims. International Journal of Eating Disorders. 2000;27:381–389. doi: 10.1002/(SICI)1098-108X(200005)27:4<381::AID-EAT2>3.0.CO;2-U. [DOI] [PubMed] [Google Scholar]
- Strother E, Lemberg R, Stanford SC, Turberville D. Eating disorders in men: underdiagnosed, undertreated, and misunderstood. Eating Disorders. 2012;20:346–355. doi: 10.1080/10640266.2012.715512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson JK, van den Berg P, Roehrig M, Guarda AS, Heinberg LJ. The sociocultural attitudes towards appearance scale-3 (SATAQ-3): Development and validation. International Journal of Eating Disorders. 2004;35:293–304. doi: 10.1002/eat.10257. [DOI] [PubMed] [Google Scholar]
- Tylka TL. Refinement of the tripartite influence model for men: dual body image pathways to body change behaviors. Body Image. 2011;8:199–207. doi: 10.1016/j.bodyim.2011.04.008. [DOI] [PubMed] [Google Scholar]
- Tylka TL, Bergeron D, Schwartz JP. Development and psychometric evaluation of the Male Body Attitudes Scale (MBAS) Body Image. 2005;2:161–175. doi: 10.1016/j.bodyim.2005.03.001. [DOI] [PubMed] [Google Scholar]


