Abstract
Objectives
A growing empirical literature indicates that emotion-related impulsivity (compared to impulsivity that is unrelated to emotion) is particularly relevant for understanding a broad range of psychopathologies. Recent work, however, has differentiated two forms of emotion-related impulsivity: A factor termed Pervasive Influence of Feelings captures tendencies for emotions (mostly negative emotions) to quickly shape thoughts. A factor termed Feelings Trigger Action captures tendencies for positive and negative emotions to quickly and reflexively shape behavior and speech. The current study used path modeling to consider links from emotion-related and non-emotion-related impulsivity to a broad range of psychopathologies.
Design and Methods
Undergraduates completed self-report measures of impulsivity, depression, anxiety, aggression, and substance use symptoms.
Results
A path model (N = 261) indicated specificity of these forms of impulsivity. Pervasive Influence of Feelings was related to anxiety and depression, whereas Feelings Trigger Action and non-emotion-related impulsivity were related to aggression and substance use.
Conclusions
The findings of this study suggest that emotion-relevant impulsivity could be a potentially important treatment target for a set of psychopathologies.
Keywords: impulsivity, urgency, psychopathology, aggression, anxiety, depression
Considerable research indicates that impulsivity is a transdiagnostic risk factor for a broad range of psychopathologies. Indeed, it has been suggested that impulsivity might be the most frequently occurring diagnostic criterion within the DSM (Whiteside & Lynam, 2001). Impulsivity, however, is a broad umbrella term (Depue & Collins, 1999), and research suggests that different forms of impulsivity, such as difficulties with sensation-seeking, ability to delay gratification, to persevere toward difficult to attain goals, and to think before acting, are only modestly correlated (Whiteside & Lynam, 2003). More importantly, these different forms of impulsivity have been shown to have only modest overlap in their ties to behavioral or psychopathology outcomes (Sharma, Markon, & Clark, 2014).
In one major factor analysis of impulsivity measures, Whiteside and Lynam (2003) found that tendencies to respond to emotion states in a highly impulsive manner could be differentiated from other forms of impulsivity. A growing body of work suggests that this form of impulsivity may be particularly important for understanding daily behavioral problems (Sharma, Markon, & Clark, 2014), neurocognitive correlates of impulsivity (Johnson, Tharp et al., 2016), and psychopathology (Cyders & Smith, 2008; Johnson, Carver et al., 2013; Whiteside & Lynam, 2003). For example, impulsive reactivity to emotions has been found to be uniquely related to a broad range of externalizing and internalizing problems such as aggression, alcohol use problems, anxiety, depression, eating disorder symptoms, and borderline personality disorder (Berg, Latzman et al., 2015; Carver, Johnson et al., 2013; Dick, Smith et al., 2010; Johnson et al., 2013; Magid & Colder, 2007; Miller, Flory et al., 2003; Pawluk & Koerner, 2013; Peters, Upton et al., 2013; Whiteside, Lynam et al., 2005). A tendency to overreact to positive feelings in particular—called positive urgency—has also been related to vandalism, risky sexual behavior, gambling, and drug use (Cyders, Smith et al., 2007; Zapolski, Cyders et al., 2009), and bipolar disorder (Muhtadie, Johnson et al., 2013).
Despite these associations, several gaps exist in our understanding of the tie between this form of impulsivity and psychopathology. An important issue is that psychopathologies are highly comorbid. Little research has considered whether links of impulsivity with some psychopathologies might be secondary to the links of impulsivity with other syndromes. To address this, we construct a multivariate model to conjointly consider multiple outcomes.
A second gap is in the understanding of the nature of emotion-related impulsivity. In recent work on this topic, two factor-analytically distinct forms of emotion-related impulsivity have been identified and distinguished from impulsivity for which emotions do not play an obvious role (Carver, Johnson et al., 2011). One emotion-related factor was termed Pervasive Influence of Feelings. It centers on the extent to which (mostly negative) emotions influence the person’s orientation to the world, mostly in automatic cognitive responses. Another factor was termed Feelings Trigger Action. This one centers on impulsive reactivity that is mostly behavioral and is affected by both positive and negative emotions (Carver et al., 2011).
Both of these factors have also been found to be correlated more robustly with key outcomes than non-emotion-related forms of impulsivity were, including aggression, borderline personality traits, depression, suicidality, and manic symptoms (Auerbach, Stewart et al., 2016; Carver et al., 2013; Johnson et al., 2013). Despite overlap in the validity of the emotion-related impulsivity factors, early studies suggest that it may be important to distinguish between these two factors in understanding psychopathology. That is, there is some evidence that Pervasive Influence of Feelings is more relevant for internalizing conditions such as depressive symptoms, whereas Feelings Trigger Action is more robustly related to externalizing conditions and hypomanic symptoms (Johnson, Carver, & Joormann, 2013). In another study, Pervasive Influence of Feelings was tied to suicidal ideation, whereas Feelings Trigger Action was tied to suicidal actions (Auerbach, Stewart, & Johnson, 2016). These findings validate the idea that the two forms of impulsivity differentially guide difficulties with thoughts versus actions in the face of emotion. As that evidence comes from only two datasets, however, there is a need for further evidence pertaining to the differential associations of these forms of impulsivity with psychopathologies.
In sum, the goal of this study was to re-consider how two aspects of emotion-related impulsivity, as well as non-emotion-related impulsivity, relate to a set of psychopathological syndromes. To do so, we assessed internalizing syndromes of anxiety and depression, along with externalizing syndromes of aggression and substance use. Participants completed measures of emotion-related and emotion-unrelated impulsivity, and we used path modeling to test unique associations between impulsivity factors and psychopathology symptoms. We predicted that all types of psychopathology symptoms would show closer associations with emotion-related impulsivity than with emotion-unrelated impulsivity, and that links of Pervasive Influence of Feelings, with its emphasis on poor constraint over emotion, would be stronger for problems that more directly involve moods (anxiety, depression), whereas links of Feelings Trigger Action, with its emphasis on poor constraint over behavior and motivation, would be more strongly related to problems that involve behavior, such as aggression and substance use. We examined these hypotheses in a large undergraduate sample, given evidence that rates of psychopathology, substance abuse, and impulsivity are particularly elevated during early adulthood (Hasin et al., 2005; Grant, Hasin, et al., 2005; Hunt & Eisenberg, 2010; Roberts, Walton, & Viechtbauer, 2006).
Method
Participants
The sample consisted of undergraduate students at a large public university in the US. Analyses presented here were based on participants (N =261) who had completed most the questionnaires and responded correctly to catch items (e.g. “Please answer “Agree” for this question”). Six participants failed to complete most of the questionnaires, and another four participants were excluding for answering four or more of the seven “catch items” incorrectly. When we repeated the analyses including participants with missing data, results remained essentially the same, with no changes in the significance or general magnitude of results. Participants in the final sample (69.3% female, age M = 20.77, SD = 2.65) described their ethnicities as follows: 33% Asian-American, 23% Caucasian, 12% Hispanic/Latino, and 19% as other; ethnicity responses were missing from 3% of the sample.
Participants earned partial credit toward a requirement in psychology courses for taking part in the study. All procedures were approved by the university’s Institutional Review Board.
Measures
Table 1 shows descriptive statistics and sample items for all measures. Multiple indices of anxiety, depression, and aggression were gathered, and then used in constructing composite variables for these three dimensions.
Table 1.
Descriptive Statistics and Sample Items of Individual Impulsivity and Psychopathology Measures
| Measure | Number of items | Mean (SD) | Alpha | Sample Item |
|---|---|---|---|---|
| Impulsivity | ||||
| Pervasive Influence of Feelings | 46 | 0.138 (2.69) | .82 | “My feelings greatly affect how I see the world.” |
| Lack of Follow Through | 64 | 0.057 (2.54) | .70 | “Unfinished tasks really bother me.” (reverse coded) |
| Feelings Trigger Action | 25 | 0.004 (1.22) | .68 | “When I am upset I often act without thinking” |
|
| ||||
| Anxiety | ||||
| MASQ General Distress Anxiety | 11 | 24.48 (7.43) | .85 | “Felt afraid” |
| MASQ Somatic Arousal | 17 | 25.55 (9.35) | .90 | “Startled easy” |
|
| ||||
| Depression | ||||
| MASQ General Distress Depression | 12 | 26.16 (10.89) | .94 | “Blamed myself for a lot of things” |
| MASQ Anhedonia | 22 | 62.40 (13.96) | .91 | “Felt like nothing was very enjoyable” |
| 7-Up 7-Down Depression | 7 | 12.77 (5.13) | .94 | “Have there been periods lasting several days or more when you were so down in the dumps that you thought you might never snap out of it?” |
| IDD | 22 | 2.66 (2.86) | .89 | “My appetite was not greater than normal” |
|
| ||||
| Aggression | ||||
| AQ Anger | 3 | 6.13 (2.76) | .73 | “I have trouble controlling my temper” |
| AQ Physical Aggression | 3 | 4.82 (2.36) | .67 | “I have threatened people I know” |
| AQ Verbal Aggression | 3 | 7.34 (3.02) | .82 | “I often find myself disagreeing with people” |
| STAB Physical Aggression | 9 | 15.02 (5.27) | .86 | “Felt like hitting people” |
| STAB Social Aggression | 11 | 21.79 (6.75) | .89 | “Tried to hurt someone’s feelings” |
|
| ||||
| Substance Use | ||||
| Substance Use Frequency | 40 | 1.38 (.41) | .68 | “In the past year, how many times have you used each of these [types of drugs] per month?” |
| Substance Use Problems | 11 | 0.53 (1.58) | .90 | “During the previous 12-month period, I have experienced a persistent desire or unsuccessful effort to cut down or control my use of a substance.” |
Note. AQ = Aggression Questionnaire; IDD = Inventory to Diagnose Depression; MASQ = Mood and Anxiety Symptom Questionnaire; STAB = Subscales of Antisocial Behaviors.
The AQ was only available for 239 persons due to experimenter error.
Impulsiveness
Participants were administered a broad range of measures of impulsivity that had been previously found to represent three underlying factors, two of which pertain to impulsive reactivity to emotions, and one of which does not. These scales were derived from previously developed impulsivity scales, supplemented with new item sets (see Carver et al., 2011 for scale development). The first factor (labeled Pervasive Influence of Feelings) centers on the extent to which (mostly negative) emotions influence the person’s orientation to the world. Scales loading primarily on this factor were Negative Generalization (Carver, 1998), and items reflecting tendencies to become immobilized by sadness, to have Emotions Color One’s Worldview, and to have an Inability to Overcome Lethargy (Carver et al., 2011); other scales that cross-loaded on this factor include Negative Urgency (Whiteside & Lynam, 2001) and Laziness (Jackson, Wood et al., 2010).
Factor 2 (labeled Lack of Follow-Through) is composed of scales that do not reference emotion. Scales loading primarily on this factor were Lack of Perseverance (Whiteside & Lynam, 2001), (Lack of) Self-control (Tangney, Baumeister et al., 2004), Laziness (Jackson et al., 2010), and Distractibility (Carver et al., 2011), though Inability to Overcome Lethargy and Positive Urgency (Cyders et al., 2007) also cross-loaded onto this factor.
Factor 3 (labeled Feelings Trigger Action) centers on impulsive behavioral actions and speech to both positive and negative emotions. Scales loading primarily on this factor were Reflexive Reaction to Feelings (Carver et al., 2011), an abbreviated version of the Positive Urgency Measure (Cyders et al., 2007), and an abbreviated version of the Negative Urgency scale (Whiteside & Lynam, 2001). Previous work has replicated the factor structure of scales (Auerbach, Stewart, & Johnson, 2016).
Responses on most scales were made from options ranging from 1 = I agree a lot to 5 = I disagree a lot; response options for the Laziness scale were 1 = Never to 5 = Very often. Scales were standardized, and factor scores were constructed using the previously published factor loadings to weight the contributing scales (Carver et al., 2011).
Anxiety
Anxiety was measured by two anxiety subscales from the Mood and Anxiety Symptoms Questionnaire (MASQ): General Distress Anxiety Symptoms, designed to assess indicators of anxious mood such as inability to relax; and Somatic Arousal, which covers symptoms that are related to anxiety and physiological arousal, such as dizziness, trembling, and being easily startled. The MASQ was developed to help differentiate symptoms that are specific to anxiety and depression from those that are common to both syndromes, such as insomnia and poor concentration, and was constructed based on the tripartite model (Clark & Watson, 1991). We used the 62-item short version (Watson, Weber et al., 1995). Participants were asked to rate the severity of each symptom during the past week on a scale of 1 = not at all to 5 = extremely, and items were summed within each subscale. The MASQ subscales have been validated against other measures of anxiety, depression, and psychopathology (Watson, Weber, et al., 1995). A composite score was calculated by standardizing the two scales and then averaging them (α = .86).
Depression
Depression was measured by the MASQ General Distress Depression and the MASQ Anhedonia subscales, the Inventory to Diagnose Depression (IDD), and the 7-Up 7-Down Depression subscale. The MASQ General Distress Depression subscale covers symptoms related to depressed mood, including self-blame and pessimism; and the MASQ Anhedonia subscale covers symptoms such as loss of interest and decreased positive affect. Both the MASQ depression subscales have been shown to differentiate patients and non-patients (Watson, Clark, et al., 1995).
The IDD is a self-report measure designed to assess symptoms of lifetime depression (Zimmerman & Coryell, 1987). Items cover 9 major symptoms of major depressive disorder that are included in the DSM criteria for major depressive disorder (e.g., guilt, hopelessness, decreased energy, loss of interest, and suicidality). Symptoms were rated on a 5-point scale, ranging from no endorsement (i.e. “My appetite was not greater than normal” = 0) to complete endorsement (i.e. “I felt hungry all the time” = 4). For each item endorsed, participants were asked whether the symptom was present for at least two weeks. IDD scores were a sum of the number of symptoms endorsed out of 10. The scale has been found to correlate highly with interview-based and other self-report measures of depression (Hodgins, Dufour et al., 2000) and to differentiate those who do and do not meet diagnostic criteria for major depressive disorder according to structured clinical interviews (Uehara, Sato et al., 1997).
The 7-Up 7-Down scale is a self-report scale that was designed to assess current manic (7 items) and depressive symptoms (7 items). In this study, we used the 7-Down subscale. Items were drawn from the General Behavior Inventory (Depue, 1987) using factor analysis and were validated against diagnoses and a set of personality and other correlates of mood disorders (Youngstrom, Murray et al., 2013). Respondents answered on a scale of 1 = never or hardly ever to 4 = very often or almost constantly. The total score is the sum of depression items (possible range 7 to 28).
A mean of the standardized scores was used as a composite index of depression. Depression subscales correlated as expected with the total depression composite score (α based on subscale totals = .73).
Aggression
Aggression was measured by three subscales of the Aggression Questionnaire – Short Form (AQ) and by two subscales from Subscales of Antisocial Behavior (STAB). The AQ – Short Form was developed by Bryant and Smith (2001) by removing items with reverse wording and low loadings or multiple loadings from the AQ (Buss & Perry, 1992). We used subscales (with 3 items each) of Anger, Physical Aggression, and Verbal Aggression, and omitted Hostility, which is conceptually distinct and showed only moderate correlations with the other subscales. The AQ subscales have been shown to elevated in individuals with severe psychopathology diagnoses, as well as suicide and narcissism (Barnett & Powell, 2016; Johnson & Carver, 2016; Menon, Sarkar, et al., 2015). Respondents answered on a scale ranging from 1 = extremely uncharacteristic of me to 5 = extremely characteristic of me. Items for each subscale were averaged. Because it was inadvertently not included for initial participants, n = 239 for the AQ.
The STAB is a self-report questionnaire that includes factor-analytically distinct subscales; of these, we used Physical Aggression (9 items) and Social Aggression (11 items) subscales and omitted Rule-breaking (11 items) behaviors (Burt & Donnellan, 2009). Participants responded on a scale ranging from 1 = never to 5 = nearly all the time. Scores for each subscale were created by summing the items. Each of the STAB subscales predict characteristic acting-out behaviors, such as gossip (Social Aggression) or feeling like hitting someone (Physical Aggression; Burt & Donnellan, 2010), and effectively differentiates offenders of violent crimes and substance users from normative groups (Burt & Donnellan, 2009). STAB Physical Aggression subscale is correlated with high impulsivity and negative affectivity (Burt & Donnellan, 2009).
A composite score was calculated by taking the mean of the five standardized scales. Subscales correlated adequately with this composite score (α based on subscale totals=.78).
Substance Use
Substance use was measured by the Substance Use Questionnaire, which was designed to measure the types of substances used, as well as problems due to that substance use (e.g., missing work or school, social or legal problems, and physical withdrawal) during the past year. The Frequency subscale includes items (derived from two-item conjoint screen (TICS) by Brown, Leonard et al. (2001)) which is focused on the frequency of use of 10 specific classes of substances (e.g., alcohol, stimulants, dissociatives, opioids, etc.; 1 = never, 2 = 1–2 times, 3 = 2–3 times, 4 = 3–4 times to 5 = greater than 5 times). The Substance problems subscale includes 11 items based on the Rapid Alcohol Problems Screen (RAPS; Cherpitel, 2000). Both substance use scales are well-validated and show high sensitivity in identifying problem drinking across gender and race (Brown et al., 2001; Cherpitel, 1998). A composite score comprising the average of the two z-transformed subscales was used, α = .62. Substance use problems have been found to correlate with emotion-related impulsivity (Latzman, Chan et al., 2013), but comparable correlations have been observed with non-emotionally relevant forms of impulsivity (Berg et al., 2015; de Wit, 2009; Latzman et al., 2013).
Procedure
After informed consent procedures, participants completed the questionnaires just described. A subset of these participated in individual laboratory-based assessments after completing questionnaires, which have been reported previously (References to be filled in after blind review).
Data Analysis
Data were analyzed using AMOS in a structural equation modeling (SEM) framework (e.g., Kline, 2005). As indicators of model fit, we inspected the χ2 statistic (known to be affected by sample size and therefore not of primary interest), the Comparative Fit Index (CFI; using a cut-off value of > .90 following Hu & Bentler, 1999), and the Root Mean Square Error of Approximation (RMSEA; using < .08 as an indicator of fit following Browne & Cudeck, 1993). Alpha was set to .05, and all analyses were two-tailed. All variables were z-standardized.
Data reduction
To test the viability of our psychopathology measurement model, we first conducted an exploratory factor analysis using principal component analysis (PCA) with Varimax rotation. Results provided initial support for the measurement model. Specifically (see Table 2), the PCA yielded four factors with anxiety subscales loading on factor 3, depression subscales loading on factor 2, substance use subscales loading on factor 4, and aggression subscales loading on factor 1. Factor cross-loadings were generally low, except for the MASQ general distress depressive symptoms subscale, which showed a substantial cross-loading on factor 3, reflecting shared method variance with the MASQ anxiety subscales. Somewhat lower cross-loadings were shown for MASQ General Distress Anxiety, which loaded dominantly on factor 3 and modestly on factor 2, and for STAB Social Aggression, which loaded dominantly on factor 1 and modestly on factor 3.
Table 2.
Psychopathology Measures: Results from Principal Components Analysis
| Factor 1 | Factor 2 | Factor 3 | Factor 4 | |
|---|---|---|---|---|
| MASQ General Distress Anxiety | .130 | .355 | .850 | .097 |
| MASQ Somatic Arousal | .109 | .159 | .863 | .138 |
| MASQ General Distress Depression | .099 | .615 | .640 | .074 |
| MASQ Anhedonia | .084 | .812 | .112 | −.022 |
| IDD | .073 | .783 | .153 | .111 |
| 7-Up 7-Down Depression | .155 | .837 | .250 | .073 |
| AQ Anger | .814 | .256 | −.048 | .066 |
| AQ Physical Aggression | .784 | .060 | .111 | .137 |
| AQ Verbal Aggression | .777 | .108 | −.075 | .095 |
| STAB Physical Aggression | .809 | .007 | .259 | .101 |
| STAB Social Aggression | .639 | .010 | .392 | .132 |
| Substance Use Problems | .106 | .141 | .098 | .813 |
| Substance Use Frequency | .205 | −.012 | .111 | .783 |
Note. Rotated component matrix (Rotation method: Varimax with Kaiser Normalization).
AQ = Aggression Questionnaire; IDD = Inventory to Diagnose Depression; MASQ = Mood and Anxiety Symptom Questionnaire; STAB = Subscales of Antisocial Behaviors.
We then conducted a confirmatory factor analysis using SEM with four correlated factors (i.e., anxiety, depression, substance use, aggression) and accounting for shared method variance within the MASQ, AQ, and STAB subscales. The resulting model showed acceptable fit, χ2(55) = 105.82, p < .001, CFI = .96, RMSEA = .064, with high factor loadings (i.e., anxiety subscales: .63–.85; depression subscales: 63–.95; substance use subscales: 54–.67; aggression subscales: .53–.84).
Hypothesis tests
Hypothesis tests were conducted in an SEM framework using path modeling (Kline, 2005). This analysis included only observed variables (no latent variables, to maintain a reasonable parameter-to-case ratio) and allows for including multiple explanatory and outcome variables in the same model. In this path model, the three impulsivity factors were included as (correlated) explanatory variables and the four psychopathology syndromes were included as outcome variables (with significantly correlated error terms included in the model). Regression paths were included between the explanatory and outcome variables.
First, we examined associations between the impulsivity factors and psychopathology syndromes by inspecting all regression paths in the path model. Second, where links of emotion-related impulsivity with psychopathology were significant, we tested whether associations were significantly larger than those for the emotion-unrelated impulsivity factor with psychopathology, using Δχ2 tests.
Follow-up analyses
In follow-up analyses we examined whether results (1) remained stable when controlling for gender (i.e., by including gender as a correlated predictor in the path model and examining stability of the regression paths) and (2) generalized across gender (i.e., by using multi-group modeling following Byrne, 2010 and examining whether a model in which a regression path was constrained to be equal across men and women showed significantly worse fit, Δχ2, p < .05, than a model in which this regression path was unconstrained across men and women). When a significant difference in model fit emerged, we examined this regression path separately for men and women. We conducted multi-group modeling for each regression path separately to allow for targeted tests.
Results
Preliminary Analyses
Descriptive statistics of key variables are shown in Table 1. For all variables, skewness and kurtosis were below the recommended thresholds (skewness > 3, kurtosis > 10; Kline, 2005). As shown in Table 3, all impulsivity and psychopathology variables were correlated with each other, ps <= .001. Depression was highly related to anxiety. Each of the three impulsivity scores was significantly related to each psychopathology syndromes in bivariate correlations, with particularly strong correlations of Pervasive Influence of Feelings with Anxiety, Depression, and Aggression, as well as (Lack of) Follow Through with Depression, and Feelings Trigger Action with Aggression.
Table 3.
Intercorrelations of Impulsivity and Composite Psychopathology Measures (N = 261)
| 1. | 2. | 3. | 4. | 5. | 6. | |
|---|---|---|---|---|---|---|
|
|
||||||
| 1. Pervasive Influence of Feelings | - | |||||
| 2. Lack of Follow Through | .70 | - | ||||
| 3. Feelings Trigger Action | .46 | .30 | - | |||
| 4. Anxiety | .50 | .36 | .21 | - | ||
| 5. Depression | .72 | .55 | .23 | .58 | - | |
| 6. Aggression | .40 | .36 | .42 | .30 | .27 | - |
| 7. Substance use | .24 | .27 | .25 | .23 | .21 | .33 |
Note. All correlations are significant at the level of p ≤ .001
Impulsivity Factors as Predictors of Psychopathology Syndromes
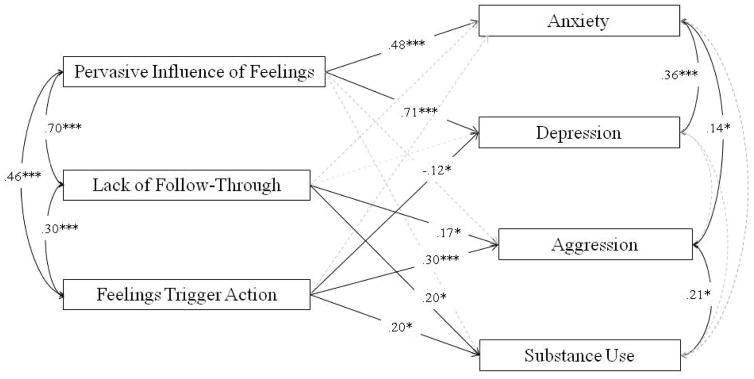
We used SEM to examine the unique associations between the impulsivity factors and psychopathology syndromes (see Table 4 and Figure 1). The final path model fit the data well, χ2(2) = 1.49, p = .474, CFI = 1.00, RMSEA = .000. Results revealed substantial specificity: Impulsivity Factor 1 (Pervasive Influence of Feelings) was positively related to anxiety and depression composite scores. Impulsivity Factor 2 (Lack of Follow-Through) and Factor 3 (Feelings Trigger Action) both positively predicted the aggression and substance abuse composite scores. In contrast with bivariate analyses, Factor 3 (Feelings Trigger Action) related to modestly lower depression composite scores. The remaining associations were nonsignificant, ps > .05.
Table 4.
Impulsivity and Psychopathology: Results from Path Model (N = 261)
| Impulsivity | Psychopathology | B | SE(B) | p |
|---|---|---|---|---|
| Pervasive Influence of Feelings (Factor 1) | Anxiety | .48 | .08 | < .001 |
| Depression | .71 | .06 | < .001 | |
| Aggression | .15 | .08 | .064 | |
| Substance Use | .01 | .09 | .933 | |
|
| ||||
| Lack of Follow Through (Factor 2) | Anxiety | .03 | .08 | .707 |
| Depression | .09 | .06 | .141 | |
| Aggression | .17 | .08 | .028 | |
| Substance Use | .21 | .08 | .012 | |
|
| ||||
| Feelings Trigger Action (Factor 3) | Anxiety | −.01 | .06 | .768 |
| Depression | −.12 | .05 | .015 | |
| Aggression | .30 | .06 | < .001 | |
| Substance Use | .19 | .07 | .004 | |
Note. Unstandardized regression coefficients.
Figure 1.
Impulsivity and psychopathology symptoms.
Note. Standardized regression coefficients (β) shown. Bold lines indicate significant associations (ps ≤ .05). Dashed lines indicate nonsignificant associations (ps > .05).
*p < .05. ***p ≤ .001.
Comparing Emotion-Related and Emotion-Unrelated Impulsivity as Predictors of Psychopathology Syndromes
We examined whether the unique associations between emotion-related vs. emotion-unrelated impulsivity factors and psychopathology syndromes significantly differed from each other using Δχ2 tests. In these analyses, Factor 1 Pervasive Influence of Feelings showed a significantly stronger association than (the nonsignificant) Factor 2 Lack of Follow-Through in relation to both anxiety, χ2(1) = 10.05, p = .002 and depression, χ2(1) = 28.78, p = .001. The Factor 2 Lack of Follow-Through and Factor 3 Feelings Trigger Action did not differ significantly from each other for either aggression, χ2(1) = 2.02, p = .155, or for substance abuse, χ2(1) = .03, p = .853.
Analyses of Gender
First, we examined whether results remained stable when controlling for gender. Results indicated that associations between impulsivity factors and psychopathology syndromes remained stable when controlling for gender, with two minor changes: The association between Factor 1 Pervasive Influence of Feelings and aggression became significant rather than a nonsigificant trend, B = .19, SE(B) = .08, p = .019, and the association between Factor 2 Lack of Follow-Through and aggression was reduced to a nonsignificant trend, B = .14, SE(B) = .08, p = .071).
Second, we examined whether findings generalized across gender using multi-group modeling. Most associations between impulsivity factors and psychopathology syndromes were not moderated by gender, Δχ2, ps > .05, with two exceptions. The association between Pervasive Influence of Feelings and depression was moderated by gender, χ2(1) = 4.60, p = .032, such that the association was stronger for women, B = .79, SE(B) = .08, p < .001, than men, B = .46, SE(B) = .12, p < .001. The association between Feelings Trigger Action and anxiety was also moderated by gender, χ2(1) = 5.03, p = .025, such that the association was significant for women, B = −.18, SE(B) = .06, p = .002, but not for men, B = .03, SE(B) = .08, p = .693.
Discussion
Previous work had suggested that tendencies toward impulsive thoughts in response to emotion were particularly relevant to depression and suicidal ideation, whereas impulsive actions in response to emotion were particularly relevant to psychopathologies involving behavioral concerns, such as externalizing syndromes. Here, we tested whether we could observe this differentiation for internalizing and externalizing syndromes (i.e., anxiety, depression, aggression, and substance use) using a multivariate path model. Multivariate findings showed that one emotion-related impulsivity factor, Pervasive Influence of Feelings, was uniquely related to depression and anxiety syndromes, whereas the other emotion-related factor, Feelings Trigger Action, was uniquely tied to substance use problems and aggression.
We hypothesized that the non-emotion impulsivity factor, Lack of Follow-Through, would be less robustly related to psychopathology than emotion-related impulsivity, but this was only partially supported. The associations of Pervasive Influence of Feelings with anxiety and depression were significantly stronger than those for Lack of Follow-Through. The effect of Lack of Follow-Through, however, did not differ significantly from the magnitude of the Feelings Trigger Action effect on either substance abuse or aggression scores. Although Feelings Trigger Action was positively correlated with depression at the bivariate level, consistent with previous results (Carver et al., 2013; Ceschi, Billieux et al., 2014; d’Acremont & Van der Linden, 2007; Gonzalez, Reynolds et al., 2011; Miller et al., 2003), once the other forms of impulsivity were controlled for, it instead was related to modestly lower depression. Apparently the variance the three impulsivity factors shared with one another acted as a suppressor of that unique effect.
A substantial body of research has shown that impulsivity is a transdiagnostic risk factor for a wide range of psychopathological syndromes and disorders (Berg et al., 2015; Johnson et al., 2013; MacKillop, Amlung et al., 2011; Moeller, Barratt et al., 2001). Our results fit well with prior findings and add considerable specificity in two ways. First, converging with previous theoretical and empirical work (Berg et al., 2015; Carver et al., 2013; Cyders & Smith, 2008; Johnson et al., 2013; Smith, Fischer et al., 2007; Smith, Guller et al., 2013; Whiteside et al., 2005), we found that the emotion-related impulsivity factors contributed more strongly to predicting symptoms of depression and anxiety than did the non-emotion-related impulsivity factor. This converges with theoretical propositions and empirical work suggesting that emotional dysfunction constitutes one of the building blocks of psychopathology (Johnson et al., 2013; Kring & Sloan, 2010; Levenson, Sturm et al., 2014; Rottenberg & Johnson, 2007), as reflected in the prominence of emotion dysfunction in the Research Domain Criteria framework (RDoC; Morris & Cuthbert, 2012). The current work highlights emotion-related impulsivity as an important feature of this emotional dysfunction (Carver et al., 2013).
Second, our findings show important specificity between the two emotion-related impulsivity factors. Specifically, Pervasive Influence of Feelings (Factor 1) showed a unique significant positive relationship to internalizing symptoms (although a link with aggression emerged as well, when controlling for gender); in contrast, Feelings Trigger Action (Factor 3) showed significant positive relationships to externalizing symptoms, as did Lack of Follow Through (Factor 2). This finding supports the common distinction between internalizing and externalizing syndromes and suggests considerable specificity at the level of impulsivity-related antecedents. Factor 1 includes tendencies toward overly general cognitive responses to negative emotions, as well as behavioral responses such as lethargy. Factor 3 covers a tendency for both positive and negative emotions to quickly and reflexively shape action and speech. Factor 2 concerns impulsivity without reference to emotion states. These findings suggest that depression and anxiety symptoms appear more distinctly related to difficulties in constraining how emotion influences thought, whereas externalizing symptoms appear related to difficulties in constraining how emotion influences behavior and to problems with impulsivity that occur without regard to emotion.
It should be noted that poor constraint appears to be the critical issue here, rather than intensity of emotional response. That is, previous work has shown that persons with emotion-related impulsivity do not have elevated emotional responses per se to standardized stimuli (Johnson, Tharp, et al., 2016). There is also evidence that impulsive responses to emotion are more predictive of psychopathology than are tendencies to be emotional per se (Kaiser, Milich, et al., 2012).
One more thing should be noted about the present results. We have emphasized the differentiation between the two emotion-related impulsivity factors and their differential unique associations with internalizing versus externalizing symptoms. Although this is important, we should also note that the SEM results do not place focus on the variance that is shared among the predictors. It is clear from the correlations in Table 3 that shared variance among the predictors plays a large role in accounting for variance in symptoms. The SEM results reveal what remains after that shared effect has been removed. We would highlight that shared effects are not trivial.
Limitations
Before considering implications, it is important to note several limitations. First, people may consider their previous experiences of symptoms experiences when evaluating their sense of control over their emotion responses. This problem may be amplified by our reliance entirely on self-report scales, with the possibility that common method variance exaggerates the strengths of effects. The relatively modest internal consistency of our psychopathology scales should also be noted, as unreliability would constrain the magnitude of effects. It will be important to assess the profile of findings using behavioral measures of impulsivity, administered during periods of high emotion. Although current findings dovetail with prior findings linking emotion-triggered impulsivity to diagnoses of anxiety and depression (Johnson et al., 2013; Miller et al., 2003), it will be important to assess the generalizability of these transdiagnostic effects in a patient sample and to validate that they predict related deficits in functioning. Previous work suggests that the neurocognitive correlates of emotion-related impulsivity may be more pronounced in clinical samples (Johnson, Tharp et al., 2016), and so generalizability to clinical samples should not be assumed. Despite the importance of testing generalizability across samples, however, it is worth noting that recent work suggests that prevalence of psychopathology in undergraduate samples approximates that in the general population (Burt & Donnellan 2009; Hunt & Eisenberg, 2010; Ibrahim, Kelly, et al., 2013). Finally, the cross-sectional design limits ability to comment on whether impulsivity operates as a vulnerability factor.
Conclusions
Despite limitations, the current findings highlight that emotion-related impulsivity may be a key facet of psychopathology. Given the large literature suggesting that impulsivity is an important risk factor that can prospectively predict the onset and progression of disorders (Alloy, Bender, et al., 2009; Bauer, Meyer, et al., 2015), it is hoped that more specific understanding of which facets of impulsivity are particularly important for different syndromes could be applied in developing predictive models of psychopathology.
Understanding the importance of emotion-related impulsivity in these symptom clusters also helps form a bridge to other risk factors in psychopathology. A growing body of research links emotion-relevant impulsivity with genetic, neural, developmental, and neurocognitive processes, which have implications for treatment. That is, emotion-relevant impulsivity has been related to the serotonin transporter gene (Carver et al., 2011; Carver, LeMoult et al., 2014; Haase et al., 2015), to cortical thinning (Hoptman, Antonius et al., 2014), reduced right-frontal activity (Gable, Mechin et al., 2015), to early adversity (Carver et al., 2011), and to response inhibition (Bagge, Littlefield et al., 2013; Gay, Rochat et al., 2008; Roberts, Fillmore et al., 2011; Rochat, Beni et al., 2013; Wilbertz, Deserno et al., 2014). To the extent that early life experiences coupled with neurobiologically-based deficits drive these traits, this could be considered in treatment planning.
If these findings generalize to patient samples, it will be important for clinicians to consider assessing more specifically whether patients have particular problems with impulse control during periods of high emotion and whether those problems take the form of poor constraint over cognitive, motivational, or behavioral domains. Persons with these difficulties could receive tailored interventions to focus on strategies that can be easily used during those specific moments. Considerable research suggests that emotion regulation depends on the same neurobiological pathways that are engaged during other kinds of cognitive control (Ochsner, Silvers, & Buhle, 2012); thus, interventions that enhance control, such as cognitive remediation strategies, may be helpful. Behavioral strategies that promote tolerance of emotion before acting, as well as emotion regulation (Linehan, 2014), warrant further testing for this form of impulsivity as well.
Practitioner Points.
Recent work has differentiated two forms of emotion-related impulsivity.
This study tests a multivariate path model linking emotion-related and non-emotion-related impulsivity with multiple forms of psychopathology.
Impulsive thoughts in response to negative emotions were related to anxiety and depression.
Impulsive actions in response to emotions were related to aggression and substance use, as did non-emotion-related impulsivity.
The study was limited by the reliance on self-report measures of impulsivity and psychopathology.
There is a need for longitudinal work on how these forms of impulsivity predict the onset and course of psychopathology.
Acknowledgments
Our thanks to Anna Feiss, Aly DiRocco, Andrea Elser, Steven Wandery, and Chris Bruce for their assistance in data collection.
Andrew Peckham was supported by National Institute of Mental Health Grant T32 MH089919 during the preparation of this manuscript.
References
- Allen PA, Hall RJ, Druley JA, et al. How shared are age-related influences on cognitive and noncognitive variables? Psychology and Aging. 2001;16:532–549. doi: 10.1037//0882-7974.16.3.532. [DOI] [PubMed] [Google Scholar]
- Alloy LB, Bender RE, Wagner CA, Whitehouse WG, Abramson LY, Hogan ME, … Harmon-Jones E. Bipolar spectrum-substance use co-occurrence: Behavioral approach system (BAS) sensitivity and impulsiveness as shared personality vulnerabilities. Journal of Personality and Social Psychology. 2009;97:549–565. doi: 10.1037/a0016061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auerbach RP, Stewart JG, Johnson SL. Impulsivity and suicidality in adolescent inpatients. Journal of Abnormal Child Psychology, Epub ahead of print. 2016 doi: 10.1007/s10802-016-0146-8.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bagge CL, Littlefield AK, Rosellini AJ, et al. Relations among behavioral and questionnaire measures of impulsivity in a sample of suicide attempters. Suicide & Life-Threatening Behavior. 2013;43:460–467. doi: 10.1111/sltb.12030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett MD, Powell HA. Self-esteem mediates narcissism and aggression among women, but not men: A comparison of two theoretical models of narcissism among college students. Personality and Individual Differences. 2016;89:100–104. doi: 10.1016/j.paid.2015.09.042. [DOI] [Google Scholar]
- Bauer IE, Meyer TD, Sanches M, Zunta-Soares G, Soares JC. Does a history of substance abuse and illness chronicity predict increased impulsivity in bipolar disorder? Journal of Affective Disorders. 2015;179:142–147. doi: 10.1016/j.jad.2015.03.010. [DOI] [PubMed] [Google Scholar]
- Berg JM, Latzman RD, Bliwise NG, et al. Parsing the heterogeneity of impulsivity: A meta-analytic review of the behavioral implications of the UPPS for psychopathology. Psychological Assessment. 2015;27:1129–1146. doi: 10.1037/pas0000111. [DOI] [PubMed] [Google Scholar]
- Brown RL, Leonard T, Saunders LA, et al. A two-item conjoint screen for alcohol and other drug problems. Journal of the American Board of Family Medicine. 2001;14:95–106. [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- Burt SA, Donnellan MB. Development and validation of the Subtypes of Antisocial Behavior Questionnaire. Aggressive Behavior. 2009;35:376–398. doi: 10.1002/ab.20314. [DOI] [PubMed] [Google Scholar]
- Burt SA, Donnellan MB. Evidence that the Subtypes of Antisocial Behavior questionnaire (STAB) predicts momentary reports of acting-out behaviors. Personality and Individual Differences. 2010;48:917–920. doi: 10.1016/j.paid.2010.02.021. [DOI] [Google Scholar]
- Buss AH, Perry M. The aggression questionnaire. Journal of Personality and Social Psychology. 1992;63:452–459. doi: 10.1037//0022-3514.63.3.452. [DOI] [PubMed] [Google Scholar]
- Byrne BM. Structural equation modeling with AMOS: Basic concepts, applications, and programming. 2. New York, NY: Routledge/Taylor & Francis Group; 2010. [Google Scholar]
- Carver CS. Generalization, adverse events, and development of depressive symptoms. Journal of Personality. 1998;66:607–619. doi: 10.1111/1467-6494.00026. [DOI] [PubMed] [Google Scholar]
- Carver CS, Johnson SL, Joormann J, et al. Serotonin transporter polymorphism interacts with childhood adversity to predict aspects of impulsivity. Psychological Science. 2011;22:589–595. doi: 10.1177/0956797611404085. [DOI] [PubMed] [Google Scholar]
- Carver CS, Johnson SL, Joormann J. Major depressive disorder and impulsive reactivity to emotion: Toward a dual-process view of depression. British Journal of Clinical Psychology. 2013;52:285–299. doi: 10.1111/bjc.12014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, LeMoult J, Johnson SL, et al. Gene effects and G x E interactions in the differential prediction of three aspects of impulsiveness. Social Psychological and Personality Science. 2014;5:730–739. [Google Scholar]
- Ceschi G, Billieux J, Hearn M, et al. Trauma exposure interacts with impulsivity in predicting emotion regulation and depressive mood. European Journal of Psychotraumatology. 2014;5 doi: 10.3402/ejpt.v5.24104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cherpitel CJ. Differences in performance of screening instruments for problem drinking among blacks, whites and Hispanics in an emergency room population. Journal of Studies on Alcohol. 1998;59:420–426. doi: 10.15288/jsa.1998.59.420. [DOI] [PubMed] [Google Scholar]
- Cherpitel CJ. A brief screening instrument for problem drinking in the emergency room: the RAPS4. Rapid Alcohol Problems Screen. Journal of Studies on Alcohol and Drugs. 2000;61:447–449. doi: 10.15288/jsa.2000.61.447. [DOI] [PubMed] [Google Scholar]
- Clark LA, Watson D. Tripartite model of anxiety and depression: Psychometric evidence and taxonomic implications. Journal of Abnormal Psychology. 1991;100:316–36. doi: 10.1037//0021-843x.100.3.316. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Smith GT, Spillane NS, et al. Integration of impulsivity and positive mood to predict risky behavior: Development and validation of a measure of positive urgency. Psychological Assessment. 2007;19:107–118. doi: 10.1037/1040-3590.19.1.107. [DOI] [PubMed] [Google Scholar]
- Cyders MA, Smith GT. Emotion-based dispositions to rash action: Positive and negative urgency. Psychological Bulletin. 2008;134:807–828. doi: 10.1037/a0013341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- d’Acremont M, Van der Linden M. How is impulsivity related to depression in adolescence? Evidence from a French validation of the cognitive emotion regulation questionnaire. Journal of Adolescence. 2007;30:271–282. doi: 10.1016/j.adolescence.2006.02.007. [DOI] [PubMed] [Google Scholar]
- de Wit H. Impulsivity as a determinant and consequence of drug use: A review of underlying processes. Addiction Biology. 2009;14:22–31. doi: 10.1111/j.1369-1600.2008.00129.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Depue RA. General Behavior Inventory Manual. Minneapolis: University of Minnesota; 1987. [Google Scholar]
- Depue RA, Collins PF. Neurobiology of the structure of personality: Dopamine, facilitation of incentive motivation, and extraversion. The Behavior and Brain Sciences. 1999;22:491–569. doi: 10.1017/s0140525x99002046. [DOI] [PubMed] [Google Scholar]
- Dick DM, Smith G, Olausson P, et al. Understanding the construct of impulsivity and its relationship to alcohol use disorders. Addiction Biology. 2010;15:217–226. doi: 10.1111/j.1369-1600.2009.00190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gable PA, Mechin NC, Hicks JA, et al. Supervisory control system and frontal asymmetry: Neurophysiological traits of emotion-based impulsivity. Social Cognitive & Affective Neuroscience. 2015;10:1310–1315. doi: 10.1093/scan/nsv017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gay P, Rochat L, Billieux J, et al. Heterogeneous inhibition processes involved in different facets of self-reported impulsivity: Evidence from a community sample. Acta Psychologica. 2008;129:332–339. doi: 10.1016/j.actpsy.2008.08.010. [DOI] [PubMed] [Google Scholar]
- Gonzalez VM, Reynolds B, Skewes MC. Role of impulsivity in the relationship between depression and alcohol problems among emerging adult college drinkers. Experimental and Clinical Psychopharmacology. 2011;19:303–313. doi: 10.1037/a0022720. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Ruan WJ, Goldstein RB, … Huang B. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: Results from the national epidemiologic survey on alcohol and related conditions. Psychological Medicine. 2005;35:1747–1759. doi: 10.1017/S0033291705006069. [DOI] [PubMed] [Google Scholar]
- Haase CM, Beermann U, Saslow LR, Shiota MN, Saturn SR, Lwi SJ, Casey JJ, Nguyen NK, Whalen PK, Keltner D, Levenson RW. Short alleles, bigger smiles? The effect of 5-HTTLPR on positive emotional expressions. Emotion. 2015;15:438–448. doi: 10.1037/emo0000074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodgins DC, Dufour M, Armstrong S. The reliability and validity of the inventory to diagnose depression in alcohol-dependent men and women. Journal of Substance Abuse. 2000;11:369–378. doi: 10.1016/S0899-3289(00)00033-X. [DOI] [PubMed] [Google Scholar]
- Hoptman MJ, Antonius D, Mauro CJ, et al. Cortical thinning, functional connectivity, and mood-related impulsivity in schizophrenia: Relationship to aggressive attitudes and behavior. American Journal of Psychiatry. 2014;171:939–948. doi: 10.1176/appi.ajp.2014.13111553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- Hunt J, Eisenberg D. Mental health problems and help-seeking behavior among college students. Journal of Adolescent Health. 2010;46:3–10. doi: 10.1016/j.jadohealth.2009.08.008. [DOI] [PubMed] [Google Scholar]
- Ibrahim AK, Kelly SJ, Adams CE, Glazebrook C. A systematic review of studies of depression prevalence in university students. Journal of Psychiatric Research. 2013;47:391–400. doi: 10.1016/j.jpsychires.2012.11.015. [DOI] [PubMed] [Google Scholar]
- Jackson JJ, Wood D, Bogg T, et al. What do conscientious people do? Development and validation of the Behavioral Indicators of Conscientiousness (BIC) Journal of Research in Personality. 2010;44:501–511. doi: 10.1016/j.jrp.2010.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SL, Carver CS, Joormann J. Impulsive responses to emotion as a transdiagnostic vulnerability to internalizing and externalizing symptoms. Journal of Affective Disorders. 2013;150:872–878. doi: 10.1016/j.jad.2013.05.004. [DOI] [PubMed] [Google Scholar]
- Johnson SL, Tharp JA, Peckham AD, et al. Positive urgency is related to difficulty inhibiting prepotent responses. Emotion. 2016;16:750–9. doi: 10.1037/emo0000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaiser AJ, Milich R, Lynam DR, Charnigo RJ. Negative Urgency, Distress Tolerance, and substance abuse among college students. Addictive Behaviors. 2012;37:1075–1083. doi: 10.1016/j.addbeh.2012.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2. New York: Guilford Press; 2005. [Google Scholar]
- Kring AM, Sloan DM. Emotion regulation and psychopathology. New York, NY: Guilford Press; 2010. [Google Scholar]
- Latzman RD, Chan WY, Shishido Y. Impulsivity moderates the association between racial discrimination and alcohol problems. Addictive Behaviors. 2013;38:2898–2904. doi: 10.1016/j.addbeh.2013.08.020. [DOI] [PubMed] [Google Scholar]
- Levenson RW, Sturm VE, Haase CM. Emotional and behavioral symptoms in neurodegenerative disease: A model for studying the neural bases of psychopathology. Annual Review of Clinical Psychology. 2014;10:581–606. doi: 10.1146/annurev-clinpsy-032813-153653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan MM. DBT Skills Training Manual. 2. New York, New York: Guilford Publications; 2014. [Google Scholar]
- Littlefield AK, Sher KJ, Steinley D. Developmental trajectories of impulsivity and their association with alcohol use and related outcomes during emerging and young adulthood I. Alcoholism: Clinical and Experimental Research. 2010;34:1409–1416. doi: 10.1111/j.1530-0277.2010.01224.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, Amlung MT, Few LR, et al. Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology. 2011;216:305–321. doi: 10.1007/s00213-011-2229-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magid V, Colder CR. The UPPS Impulsive Behavior Scale: Factor structure and associations with college drinking. Personality and Individual Differences. 2007;43:1927–1937. doi: 10.1016/j.paid.2007.06.013. [DOI] [Google Scholar]
- Menon V, Sarkar S, Kattimani S, Mathan K. Do personality traits such as impulsivity and hostility-aggressiveness predict severity of intent in attempted suicide? Findings from a record based study in South India. Indian Journal of Psychological Medicine. 2015;37:393–8. doi: 10.4103/0253-7176.168563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JD, Flory K, Lynam DR, et al. A test of the four-factor model of impulsivity-related traits. Personality and Individual Differences. 2003;34:1403–1418. A test of the four-factor model of impulsivity-related traits. [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, et al. Psychiatric aspects of impulsivity. American Journal of Psychiatry. 2001;158:1783–1793. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Morris SE, Cuthbert BN. Research Domain Criteria: Cognitive systems, neural circuits, and dimensions of behavior. Dialogues in Clinical Neuroscience. 2012;14:29–37. doi: 10.31887/DCNS.2012.14.1/smorris. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muhtadie L, Johnson SL, Carver CS, et al. A profile approach to impulsivity in bipolar disorder: The key role of strong emotions. Acta Psychiatrica Scandinavica. 2013;129:100–108. doi: 10.1111/acps.12136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ochsner KN, Silvers JA, Buhle JT. Functional imaging studies of emotion regulation: A synthetic review and evolving model of the cognitive control of emotion. Annals of the New York Academy of Sciences. 2012;125:E1–24. doi: 10.1111/j.1749-6632.2012.06751.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pawluk EJ, Koerner N. A preliminary investigation of impulsivity in generalized anxiety disorder. Personality and Individual Differences. 2013;54:732–737. doi: 10.1016/j.paid.2012.11.027. [DOI] [Google Scholar]
- Peters JR, Upton BT, Baer RA. Brief report: relationships between facets of impulsivity and borderline personality features. Journal of Personality Disorders. 2013;27:547–552. doi: 10.1521/pedi_2012_26_044. [DOI] [PubMed] [Google Scholar]
- Roberts W, Fillmore MT, Milich R. Separating automatic and intentional inhibitory mechanisms of attention in adults with attention-deficit/hyperactivity disorder. Journal of Abnormal Psychology. 2011;120:223–233. doi: 10.1037/a0021408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin. 2006;132:1–25. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Rochat L, Beni C, Annoni JM, et al. How inhibition relates to impulsivity after moderate to severe traumatic brain injury. Journal of the International Neuropsychological Society. 2013;19:890–898. doi: 10.1017/S1355617713000672. [DOI] [PubMed] [Google Scholar]
- Rottenberg J, Johnson SL. Emotion and Psychopathology. Washington, DC: American Psychological Association; 2007. [Google Scholar]
- Sharma L, Markon KE, Clark LA. Toward a theory of distinct types of “impulsive” behaviors: A meta-analysis of self-report and behavioral measures. Psychological Bulletin. 2014;140:374–408. doi: 10.1037/a0034418. [DOI] [PubMed] [Google Scholar]
- Smith GT, Fischer S, Cyders MA, et al. On the validity and utility of discriminating among impulsivity-like traits. Assessment. 2007;14:155–170. doi: 10.1177/1073191106295527. On the validity and utility of discriminating among impulsivity-like traits. [DOI] [PubMed] [Google Scholar]
- Smith GT, Guller L, Zapolski TC. A comparison of two models of Urgency: Urgency predicts both rash action and depression in youth. Clinical Psychological Science. 2013;1:266–275. doi: 10.1177/2167702612470647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tangney JP, Baumeister RF, Boone AL. High self-control predicts good adjustment, less pathology, better grades, and interpersonal success. Journal of Personality. 2004;72:271–324. doi: 10.1111/j.0022-3506.2004.00263.x. [DOI] [PubMed] [Google Scholar]
- Uehara T, Sato T, Sakado K, et al. Discriminant validity of the Inventory to Diagnose Depression between patients with major depression and pure anxiety disorders. Psychiatry Research. 1997;71:57–61. doi: 10.1016/s0165-1781(97)00040-1. [DOI] [PubMed] [Google Scholar]
- Watson D, Clark LA, Weber K, et al. Testing a tripartite model: II. Exploring the symptom structure of anxiety and depression in student, adult, and patient samples. Journal of Abnormal Psychology. 1995;104:3–14. doi: 10.1037//0021-843x.104.1.15. [DOI] [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, et al. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of Abnormal Psychology. 1995;104:3–14. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR. The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences. 2001;30:669–689. doi: 10.1016/S0191-8869(00)00064-7. [DOI] [Google Scholar]
- Whiteside SP, Lynam DR. Understanding the role of impulsivity and externalizing psychopathology in alcohol abuse: Application of the UPPS impulsive behavior scale. Experimental and Clinical Psychopharmacology. 2003;10:210–217. doi: 10.1037/1064-1297.11.3.210. [DOI] [PubMed] [Google Scholar]
- Whiteside SP, Lynam DR, Miller JD, et al. Validation of the UPPS impulsive behavior scale: A four-factor model of impulsivity. European Journal of Personality. 2005;19:559–574. doi: 10.1002/per.556. [DOI] [Google Scholar]
- Wilbertz T, Deserno L, Horstmann A, et al. Response inhibition and its relation to multidimensional impulsivity. NeuroImage. 2014;103:241–248. doi: 10.1016/j.neuroimage.2014.09.021. [DOI] [PubMed] [Google Scholar]
- Youngstrom EA, Murray G, Johnson SL, et al. The 7 up 7 down inventory: A 14-item measure of manic and depressive tendencies carved from the General Behavior Inventory. Psychological Assessment. 2013;25:1377–1383. doi: 10.1037/a0033975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zapolski TC, Cyders MA, Smith GT. Positive urgency predicts illegal drug use and risky sexual behavior. Psychology of Addictive Behaviors. 2009;23:348–354. doi: 10.1037/a0014684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmerman M, Coryell W. The inventory to diagnose depression, lifetime version. Acta Psychiatrica Scandinavica. 1987;75:495–499. doi: 10.1111/j.1600-0447.1987.tb02824.x. [DOI] [PubMed] [Google Scholar]