Abstract
Myoglobin is dark red colour heme containing protein, stored in muscle. Change in permeability of myolemma causes myoglobin leak in plasma, which is cleared by kidney swiftly. Differentiating myoglobinuria from hemoglobinuria is important. Clinicians concern over myoglobinuria is to protect the patient from acute renal disease. We present a case of primary myoglobinuria, its clinical symptoms, diagnosis and treatment.
Keywords: Myoglobin, Myoglobinuria, Hemoglobin, Hemoglobinuria, Myocyte
Introduction
Myoglobin is dark red colour heme containing monomeric protein having 17–18 kD molecular weight and stored in Skeletal muscle. It functions as an oxygen-storage unit, providing oxygen to the working muscles. Alteration in the permeability of myocyte membrane or necrosis of myocyte leads to myoglobinemia [1]. Myoglobinuria is usually the result of rhabdomyolysis or muscle destruction. The cause can be either hereditary or acquired. A typical myoglobinuria presents classical triad of symptoms like myalgia, muscle weakness and tea red colour urine [2, 3]. Though this triad is seen in less than 10 % of cases, fatigue, fever, tachycardia, nausea and vomiting may be seen in many cases [4].
Prevalence of myoglobinuria is 1 in 2000 lives. Primary myoglobinuria is rare and diagnosed once causes of secondary myoglobinuria like crush or burn injury, Flu, high voltage accidents, convulsion, arterial occlusion, strenuous exercise, alcoholism and drug abuse are ruled out.
Usually myoglobin is filtered through glomerulus and rapidly excreted in urine. Increased amount of myoglobin reaching distal convoluted tubule gets precipitated in acidic urine causing distal tubular toxicity. This is the primary cause of acute renal injury. Clinicians interest in recognizing severity of myoglobinuria is to prevent and protect Acute renal injury [7].
We present a rare case of idiopathic/primary myoglobinuria.
Case
A 13 year old boy was brought to the emergency Department at about 6.00 pm with chief complaint of Pain in lower limb, difficulty in walking for last one month, mild fever with 10–12 episode of vomiting in last 24 h. The patient was almost bedridden from last week because unable to sit or stand.
History of Patient (HOP)-I: Boy was apparently normal 2 months ago when he developed pain in left thigh, insidious onset gradually progressed to spasmodic pain in the left thigh with a feeling of tightness around the limb, initially on exertion but later even at rest. Severity of pain was such that the boy found difficulty in walking and this hampered his daily routine activity also. After 12–13 days following the first symptom, pain progressed to the opposite limb and took a similar course. Eventually the patient was unable to walk without support, his movements were restricted. Weakness has progressed to such an extent that the patient was unable to fold legs completely.
On observation, the patient had difficulty in climbing and getting down stairs (+), unable to balance while walking (+), difficulty in getting up from squatting (+), had severe low back ache (++).
The patient has no history of (H/O) loss of bowel and bladder control, dropping of eyelids, difficulty chewing and swallowing. No sign of drooling, breathlessness, excess sweating or flushing redness of face. No recent history of fever or any medication.
Detailed history revealed, a boy was Full term normal vaginaly delivered (FTNVD) with adequate birth weight from 2° Conseguneous Marriage couple, studying in 6th standard having good academic record. He is second child, first sibling is normal. There is no other significant family history.
A nerve conduction study was done to rule out neuropathy. Except 10–12 episode of non-projectile vomiting, loss of appetite and mild fever for 1 day no other significant findings were noted.
With above complaints, patient was admitted to the pediatric ward. As a routine diagnostic check up, blood and urine samples were sent to clinical Biochemistry for investigations.
Due to brown–red colour of urine, fresh sample of urine was sent to the Department of Biochemistry for Inborn Error of Metabolism and metabolic disease investigation.
Report from Department of Biochemistry reads, Tea red colour urine (Fig. 1), Specific gravity within normal range, No inborn error of amino acid metabolism.
Fig. 1.
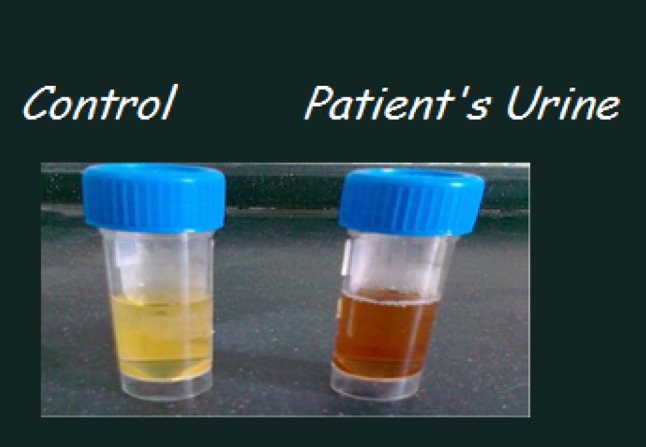
Tea coloured urine of myoglobinuria
Laboratory findings
Chemical examination of urine sample revealed Reducing sugar, ketone bodies and Bile Salt Bile Pigment—negative but, presence of +2 protein (by 30 % Sulphosalicylic acid), Dipstick test for hemoprotein and Benzidine test for hemoglobin were Positive (+1). To rule out hemoglobin from myoglobin, Benzidine test was performed after 40 fold dilution of urine. The result was positive indicating the presence of myoglobin. Further, to confirm myoglobin following tests were performed on fresh urine sample.
Urine was centrifuged at 5000 rpm for 30 min—Supernatant obtained was subjected for Benzidine reagent test. Positive result obtained indicated presence of Myoglobin in supernatant.
Benzidine reagent test remained negative on Sediment obtained after centrifugation. Microscopic examination reveals few leucocytes but no red blood cell, again indicating myoglobinuria.
Rapid Ammonium sulfate precipitation test [5] for Differentiating Myoglobin from Hemoglobin. To 5 ml urine sample 2.8 g ammonium sulfate was added slowly with thorough mixing to obtain 80 % saturation of ammonium sulphate in urine. Pprecipite obtained at 80 % saturation is of haemoglobin which was removed by centrifugation for 10 min at 3000 rpm. Red brown colour persisted in the supernatant indicates myoglobin. It was tested with the Benzidine reagent test. The result was compared with a control urine sample with added blood. Positive result in patient’s urine indicated myoglobin.
Precipitation of myoglobin at different concentration of Ammonium sulphate suggested by Hamilton RW [6]. (Table 1).
Table 1.
Results of Precipitation with Ammonium sulfate at various concentrations
| % Ammonium sulfate saturation | 50 % | 60 % | 70 % | 80 % | 90 % | 100 % |
|---|---|---|---|---|---|---|
| Control urine with added hemoglobin | No ppt | No ppt | Mild ppt | Thick ppt | Mild ppt | No ppt |
| Fresh patient’s urine | No ppt | No ppt | No ppt | No ppt | Mild ppt | Thick ppt |
Precipitation with Ammonium sulfate at different concentrations indicates hemoglobin is precipitated at 80 % saturation of Ammonium sulfate, whereas, myoglobin gets precipitated only on full saturation.
The result obtained in Serum sample from day one to 3 weeks (Table 2) was supportive of myoglobinuria. The patient was treated with predneson along with Urocit. Colour of urine returned to normal on day three. The patient was discharged on day five as he felt relieved of pain but, he was kept under observation for three weeks on OPD clinics. No recurrence of symptoms were noted.
Table 2.
Three week results of serum and urine parameters
| Biochemical parameter | Result on 4/2/16 |
Result on 18/2/16 |
Result on 3/3/16 |
Normal ref. range |
|---|---|---|---|---|
| Serum sodium | 98 | 91 | 93 | 20–110 mmol/L |
| Serum potassium | 43 | 42 | 4 | 12–62 mmol/L |
| Serum chloride | 68 | 92 | 93 | 65–125 mmol/L |
| Serum urea | 18 | 22 | 25 | 15–40 mg/dl |
| Serum creatinine | 0.9 | 1.2 | 0.8 | 0.7 to 1.3 mg/dl |
| Serum AST | 730 | 552 | 192 | 05–40 U/L |
| Serum ALT | 110 | 93 | 76 | 0–65 U/L |
| Serum LDH | 1142 | 329 | 101 | 82–234 U/L |
| Serum CPK | 27,310 | 1228 | 196 | 26–308 U/L |
| Colour of urine | Dark red | Yellow | Pale yellow | Pale yellow to yellow |
| Urine hemoglobin | Absent | Absent | Absent | Nil (Benzidine test) |
| Urine protein | Present (++) | + | Absent | (30 % SSA) |
| Urine myoglobin [5] | Present (+++) | Present (+) | Absent | Nil |
Discussion
Myoglobinuria is usually the result of muscle destruction or any process that interferes with storage by muscle cells. Change in membrane permeability causes imbalance in membrane bound Na+–K+ ATPase pump which affect Na+–Ca+2channel. Thus, high intracellular Ca+2 activates many Calcium dependent enzymes and adds to membrane damage. This results in increased activity of LDH, CK, AST, ALT, Aldolase enzymes in plasma along with myoglobin [2]. Alkalinization of urine help excretion of myoglobin through urine and protects from renal damage.
The diagnosis of myoglobinemia and myoglobinuria can be confirmed by immune assay techniques. Although not widely available, offer the possibility of the specificity and sensitivity needed for clinical use. Due to unavailability of procedure it was not performed on our patient [8].
Conclusion
With reference to clinical examination, symptoms and Laboratory results, patient was diagnosed as a case of primary myoglobinuria.
Acknowledgments
We thank management for providing support in research activity. We thank our technical staff for their technical support. We thank the patient and his relative for their cooperation.
Copliance with Ethical Standards
Conflict of interest
No author has expressed any conflict of interest.
Contributor Information
Dhiraj J. Trivedi, Email: dhiraj99trivedi@gmail.com
Shrirang P. Kulkarni, Email: drsrirang@gmail.com
Rakesh Mudaraddi, Email: drrakesh_raddi@yahoo.co.in.
References
- 1.Luck RP, Sandi V. Rhabdomyolysis: a review of clinical presentation, etiology, diagnosis and management. Pediatr Emerg Care. 2008;24(4):262–268. doi: 10.1097/PEC.0b013e31816bc7b7. [DOI] [PubMed] [Google Scholar]
- 2.Davis WS. Myoglobinuria. Neurol Clin. 2000;18(1):215–243. doi: 10.1016/S0733-8619(05)70187-0. [DOI] [PubMed] [Google Scholar]
- 3.Barca E, Valentina E, Salvatore DM. Metabolic myoglobinuria. Curr Neurol Neurosci Rep. 2015;15(10):69. doi: 10.1007/s11910-015-0590-9. [DOI] [PubMed] [Google Scholar]
- 4.Dalakas MC. Toxic drug induced myopathies. J Neurol Neurosurg Psychiatry. 2009;80(8):832–838. doi: 10.1136/jnnp.2008.168294. [DOI] [PubMed] [Google Scholar]
- 5.Blondheim SH, Margoliash E, Shafrir E. A Simple test for myohemoglobinuria (myoglobinuria) JAMA. 1958;167(4):453–454. doi: 10.1001/jama.1958.72990210001009. [DOI] [PubMed] [Google Scholar]
- 6.Hamilton RW, Hopkins MB, Shihabi ZK. Myoglobinuria, hemoglobinuria and acute renal failure. Clin Chem. 1989;35(8):1713–1720. [PubMed] [Google Scholar]
- 7.Ahsan SK, Washington RJ, Ahsan N. Myoglobinuria: evaluation of methods in the clinical diagnosis acute renal failure. Indian J Med Sci. 2001;55(8):443–452. [PubMed] [Google Scholar]
- 8.Duma RJ, Trigg JW, Hammack WJ. Primary myoglobinuria: a case report emphasizing recent diagnostic techniques. Ann Intern Med. 1962;56:97–104. doi: 10.7326/0003-4819-56-1-97. [DOI] [PubMed] [Google Scholar]


