Abstract
Alanine aminotransferase (ALT) is the most common and cost effective screening test for asymptomatic liver disease. There is paucity of data on normal ALT among healthy individuals in India. An observational cross sectional study was conducted from January to July 2013 to estimate the upper limit of normal for ALT in healthy south Indian population. Adults undergoing voluntary or pre-employment health screening were included. Those with current and past alcoholism or smoking, acute illness or hospitalization during preceding 12 months, non-steroidal anti-inflammatory or over the counter medication use within a month, current or past intake of herbal medications, any chronic medical illness, abnormal body mass index (BMI), fatty liver in ultrasound, abnormality in haemoglobin, platelet count, blood sugar, creatinine, lipid profile and thyroid function test and positive serology (Hepatitis B, C or HIV) were excluded. A total of 2600 subjects were screened. 344 were included for analysis. Mean age was 35 years in men and 34.83 years in women, with a mean BMI of 22.2 kg/m2 in men and 21.8 kg/m2 in women. The mean ALT in men and women were 21.87 ± 2.9 (97.5th percentile 28 U/L) and 19.35 ± 3.3 (97.5th percentile 24 U/L) respectively. In conclusion, mean and upper limit of ALT (97.5th percentile) in south Indian men was 21.87 and 28 IU/L and women were 19.35 and 24 IU/L respectively. There is a need to re-consider ALT levels in our population for better detection of individuals at risk for liver disease.
Keywords: Alanine aminotransferase (ALT), Liver function test, Liver disease, Threshold, Healthy population
Introduction
Serum alanine aminotransferase (ALT) is the most common and economical screening test for assessment of asymptomatic liver disease. Most laboratories in India mention the upper limit of normal for ALT as 30–40 IU/L. The decision to initiate antiviral treatment and the need for liver biopsies in chronic hepatitis B depend on the level of ALT [1, 2]. Serum ALT also plays an important role in the definition and management of anti-tuberculous drug induced liver injury [3]. American association for study of liver disease (AASLD) has mentioned the need to decrease upper limit of ALT to 30 IU/L in men and 19 IU/L in women based on an Italian study on young healthy population [1, 4]. The challenge in the study design addressing the query on normal ALT in healthy population is the robustness of the defined exclusion criteria. While the definition of healthy population has improved from papers published in 2006–2013, the fact that numerous factors can transiently alter ALT makes the exclusion list complex [5–8]. These could include short duration inter current illness, few doses of over the counter medications (especially non-steroidal anti-inflammatory drugs, multi-vitamins and synthetic food supplements) and intake of alcohol <20 g per day. The most well designed study on the research question is by Lee and colleagues on a liver donor population, which had histologically normal liver. However, the mean age of participants was 27.2 years, which is not representative of the entire spectrum of adult population [5]. The present study aimed to estimate upper limit of normal for ALT in healthy population from south India incorporating all possible confounders of mild ALT elevations in the exclusion criteria, like alcohol even in small quantities, recent illness in an other wise healthy person, all over the counter medication intake and fatty liver diagnosed by ultrasound.
Materials and Methods
It was an observational study of adults (defined as aged ≥18 years) undergoing voluntary preventive screening or pre-employment health screening through 4 private outpatient clinics in Chennai city (located in South India) headed by physicians with an experience of at least 10 years of clinical practice. The study period was from January to July 2013. All testing were done at laboratories approved by National Accredited Board for Laboratories (NABL), India. Exclusion criteria included: (a) current or past alcoholism of any quantity (b) current or past smoking (c) acute illness during the preceding 2 months of any severity (d) hospitalization during the preceding 12 months (e) non-steroidal anti-inflammatory drugs or over the counter medication use within a month prior to current visit (f) current or past intake of herbal medications (g) any chronic medical illness (h) Body Mass Index (BMI) <18 and ≥25 kg/m2 (included normal and overweight participants as per Asian standards) (i) dyslipidemia defined as total cholesterol ≥200 mg/dl, triglycerides ≥150 mg/dl or low density lipoprotein ≥100 mg/dl (j) any grade of fatty liver in ultrasound assessed using either 2- to 4-MHz vector transducer or 2- to 5-MHz convex transducer (k) abnormal blood counts (Hb% < 12 g/dl, total count <4000 per mm3 or more than 11,000 mm3, platelet count <1.5 lakhs or more than 4 lakhs per mm3) (l) serum creatinine > 1 mg/dl m) abnormal thyroid function tests (n) Total Bilirubin >1.1 mg/dl (o) albumin <3.5 g/dl p) HbA1C > 5.5 or fasting blood sugar >100 mg/dl (p) Positive HBsAg, anti-HCV or HIV test. We included overweight (BMI-23 to 24.9 kg/m2) patients without ultrasound features of fatty liver so that the study inclusion is not too narrow and prevent application in clinical practice. Figure 1 shows outline of study methods.
Fig. 1.
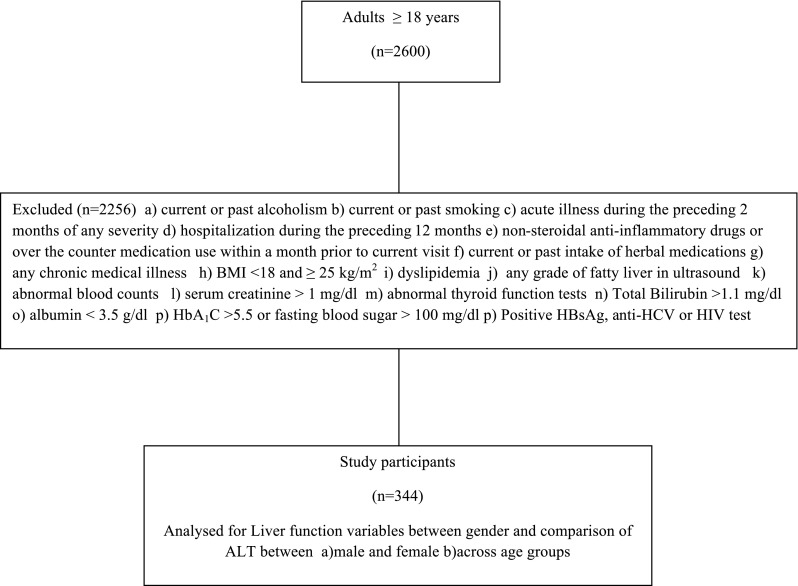
Flow of study participants
The health screening method included a clinical evaluation by a physician, which included questioning regarding alcohol intake, smoking, recent and past medical illness, intake of over the counter medications, synthetic food supplements and herbal preparations. This was followed by evaluation with a battery of laboratory test which included complete blood count, fasting blood sugar, lipid profile, serum creatinine, electrolytes, liver function test, thyroid function test, electrocardiogram, chest x-ray and ultrasound abdomen.
Hematological tests were done using Sysmex XN 3120 7 Part cell Counter (Kobe, Japan). Serum Biochemistry and endocrinology tests were done using COBOS c 6000 integrated analyzer (blood sugar-hexokinase, creatinine-Jaffe’s kinetic, electrolytes-ion specific electrodes, UV-phosphomolybdate, Lipids-enzymatic calorimetry, bilirubin-colorimetric endpoint diazo, AST and ALT-Kinetic, alkaline phosphatase-kinetic, thyroid stimulating hormone-CLIA and FT4-CLIA). Serum hepatitis B surface antigen (HBsAg) was tested using radio-immunoassay (Abbott Laboratories, USA) whereas antibody to hepatitis C virus (anti-HCV) and HIV was measured with enzyme immunoassay (Abbott Laboratories, USA). The study protocol was approved by the community research network ethics committee.
Statistical Methods
Variables were expressed as number (%) or mean ± SD. Difference between liver function variables between men and women as well, differences within same gender across different age groups were analysed using a paired ‘t’ test. A p value of <0.05 was considered as statistically significant. 50th, 75th, 90th, 95th, 97.5th percentile of ALT was calculated by standard methods. Analysis was done with SPSS version 21.0
Results
A total of 2600 subjects were screened during the study period. 2256 were excluded due to presence of one or more exclusion criteria. 1210 had at least two exclusion criteria. Distribution of exclusion criteria were alcoholism (n = 582), smoking (n = 436), recent acute illness (n = 340), hospitalization within a year (n = 128), medication intake (n = 620), elevated blood sugar (n = 310) chronic medical illness (n = 196), elevated BMI (n = 510), dyslipidemia (n = 462), hematological or thyroid abnormality (n = 121), HBsAg positivity (n = 18), Anti-HCV positivity (n = 3) and HIV (n = 2). After exclusion, 344 subjects satisfied the inclusion criteria and were included for analysis.
The mean age of the study participants was 35 years in men and 34.83 years in women, with a mean BMI of 22.2 kg/m2 in men and 21.8 kg/m2 in women. The mean ALT levels (IU/L) in men and women were 21.87 ± 2.9 and 19.35 ± 3.3 respectively (Table 1). The 50th, 75th, 95th and 97.5th percentile for ALT among men was 22, 24, 27 and 28 IU/L, while for women it was 21, 22, 23 and 24 IU/L. The study observed a statistically significant difference (p < 0.001) between ALT levels among men (mean 21.87 ± 2.9 IU/L) and women (mean 19.35 ± 3.3 IU/L). Comparison of ALT levels between different age groups among men (Table 2) observed significant difference (p = 0.025) between men aged 20–35 years (mean ALT 22.23 ± 2.83 IU/L) and men aged >50 years (mean ALT 20.71 ± 3.33 IU/L), while there was no significant difference (p = 0.052) between men aged 20–35 years and 36–50 years or men aged 36–50 years and >50 years (p = 0.637). Similar comparison of ALT among women (Table 2) did not identify any significant differences between different age groups, 20–35 and 36–50 years (p = 0.411), 20–35 and >50 years (p = 0.914) and 36–50 and >50 years (p = 0.610).
Table 1.
Gender difference of liver function parameters
| Function | Male (n = 183) | Female (n = 161) | p value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| T. Bilirubin (mg/dl) | 0.936 | 0.1267 | 0.983 | 0.1329 | 0.001 |
| D. Bilirubin (mg/dl) | 0.256 | 0.057 | 0.255 | 0.0661 | 0.872 |
| AST (IU/L) | 21.13 | 3.006 | 17.59 | 3.274 | <0.001 |
| ALT (IU/L) | 21.87 | 2.909 | 19.35 | 3.321 | <0.001 |
| SAP (IU/L) | 83.97 | 11.324 | 85.22 | 13.411 | 0.350 |
| Albumin (g/dl) | 4.25 | 0.208 | 4.122 | 0.2139 | <0.001 |
| Globulin (g/dl) | 3.18 | 0.183 | 2.98 | 0.269 | <0.001 |
AST aspartate transaminase, ALT alanine transaminase, SAP serum alkaline phosphatase
Table 2.
Comparison of liver function parameters among men and women of different age groups
| Function | Male: 20–35 (n = 132) |
Male: 36–50 (n = 30) |
Male: >50 (n = 21) |
|||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| T. Bilirubin (mg/dl) | 0.921 | 0.1272 | 0.953 | 0.1196 | 1.005 | 0.1117 |
| D. Bilirubin (mg/dl) | 0.247 | 0.0545 | 0.280 | 0.0610 | 0.276 | 0.0539 |
| AST (IU/L) | 21.47 | 3.000 | 20.40 | 3.069 | 20.05 | 2.617 |
| ALT (IU/L) | 22.23 | 2.831 | 21.10 | 2.675 | 20.71 | 3.334 |
| SAP (IU/L) | 83.43 | 11.598 | 86.13 | 10.497 | 84.24 | 10.816 |
| Albumin (g/dl) | 4.258 | 0.2165 | 4.257 | 0.1524 | 4.190 | 0.2211 |
| Globulin (g/dl) | 3.18 | 0.182 | 3.21 | 0.176 | 3.17 | 0.203 |
| Female: 20–35 (n = 104) | Female: 36–50 (n = 34) | Female: >50 (n = 23) | ||||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | |
| T. Bilirubin (mg/dl) | 0.968 | 0.1381 | 1.015 | 0.1258 | 1.004 | 0.1107 |
| D. Bilirubin (mg/dl) | 0.247 | 0.0638 | 0.274 | 0.0666 | 0.261 | 0.0722 |
| AST (IU/L) | 17.64 | 3.165 | 17.47 | 3.510 | 17.52 | 3.540 |
| ALT (IU/L) | 19.22 | 3.297 | 19.76 | 3.220 | 19.30 | 3.661 |
| SAP (IU/L) | 83.25 | 14.452 | 89.74 | 9.937 | 87.43 | 11.269 |
| Albumin (g/dl) | 4.108 | 0.1904 | 4.135 | 0.2533 | 4.170 | 0.2512 |
| Globulin (g/dl) | 2.92 | 0.252 | 3.03 | 0.254 | 3.19 | 0.257 |
AST aspartate transaminase, ALT alanine transaminase, SAP serum alkaline phosphatase
Discussion
The mean ALT level observed in the present study for men (21.8 ± 2.9 IU/L) and women (19.3 ± 3.3 IU/L) is consistent with levels suggested by earlier Asian (non-Indian) studies [5, 6]. Of the 12 studies done on the topic from Asia outside of India, three studies warrant further mention on account of their superior methodology and (or) sample size. A study of 1105 potential liver donors in South Korea observed a mean ALT level of 17.9 ± 6.8 (97.5th percentile-35 IU/L) in men and 13.5 ± 5.2 (97.5th percentile-26 IU/L) in women [5]. The study excluded participants with abnormal liver histology defined as >5 % fatty changes, significant fibrosis or inflammatory cell infiltration [5]. A national health survey in South Korea with a large sample size (n = 27,913) which excluded history of cirrhosis, dyslipidemia, malignancy, stroke, myocardial infarction, chronic kidney disease, diabetes mellitus, alcohol intake >20 g/day for men and >10 g/day for women and risk for non-alcoholic fatty liver disease observed the ALT in men and women as 18.1 ± 9.2 (95th percentile-34 IU/L) and 13.6 ± 7 (95th percentile-25 IU/L) respectively [6]. It may be observed that the standard deviation in our study population is more narrow compared to other studies indicating that ALT level fall closely around a mean when additional possible reasons for elevated LFT like recent acute illness, intake of all over the counter medication and alcohol intake irrespective of quantity are added to the exclusion criteria. The study involving healthy Chinese Han population (n = 13,637) which excluded fatty liver by ultrasound, intake of hepatotoxic medications or herbs, chronic liver disease, chronic alcohol intake, abnormal other biochemical values, and HBV, HCV or HIV infection showed a ALT level (95th percentile) of 35 IU/L in men and 23 IU/L in women [7]. It may be observed that the upper limit of ALT among men observed in our study (97.5th percentile-28 IU/L) is lesser than similar observation in men of above mentioned studies which show a value of around 35 IU/L. Whether, the difference is attributable to the exclusion of all alcoholics irrespective of intake volume need further systematic exploration in future studies.
Table 3 shows the comparison between Indian studies on upper limit of normal for ALT [8–11]. Variation in the methods (mean ± SD, median with range, median with inter-quartile range and percentiles) adopted by Indian studies to describe and analyze ALT, makes comparison of ALT in present study with other studies in the region less comprehensive. The 97.5th percentile for ALT observed in our study appears to be the lowest in literature published from India, especially among men. This raises the importance of a design, which excludes even likely causes of transient ALT elevation. Though the study population from western India included individuals with increased BMI (61.5 % had BMI > 23 kg/m2), mean values of ALT (20.5 IU/L in males and 15.0 IU/L in female) among participants with normal BMI is similar to our observation. The observation of 97.5th percentile for ALT among men (28 IU/L) and women (24 IU/L) should be interpreted clinically as an ALT value above which the probability of abnormality is high. Furthermore, the degree of elevation in ALT (often described as twofold, etc.) is conventionally calculated from this value.
Table 3.
Comparison of Indian studies on ALT among healthy population
| Authors with region and year | Study population and sample size | Exclusion criteria | ALT in men IU/L Mean ± SD, median (or) percentile |
ALT in women IU/L Mean ± SD, median (or) percentile |
|---|---|---|---|---|
| Furruqh et al. [9] Southern India 2004 |
Visitors of Health plan clinic (n = 464) | History of acute inflammatory condition, diabetes mellitus, tuberculosis, malignancy, dyslipidemia, liver dysfunction, contact with jaundiced patients, cardiac disease, renal disease, medications, and exposure to carbon tetrachloride, beryllium, and vinyl chloride. Presence of factors which includes excessive body weight, smoking, alcohol abuse, pregnancy and strenuous exercise | Age dependent median-38 to 43 Overall value for 97.5th percentile not mentioned |
Age dependent median-33 to 38 Overall value for 97.5th percentile not mentioned |
| Yadhav et al. [10] Northern India 2013 |
Healthy individuals (n = 2021) | Diabetes, Coronary artery disease, obesity (Body Mass Index [BMI] > 30), hypertension, risks from occupation and environment, genetically determined risks, drug treatment for disease or suffering, oral contraceptives, drug abuse, alcohol, tobacco, pregnancy, stress, & excessive exercise | Median-28 (range 11–70) 97.5th percentile-70 |
Median-22 (range 9–63) 97.5th percentile-63 |
| Kumar et al. [8] Western India 2014 |
Blood donors (n = 4917) | Hepatitis B, C, Human Immunodeficiency Virus (HIV) I and II infection, Leprosy, Malignancy, Heart disease, Chronic nephritis, Allergic disorders, Schizophrenia, Polycythemia vera, Abnormal bleeding tendencies, Unexplained weight loss, Individuals on anticonvulsant, antiarrhythmic, Immunosuppressive, anticoagulant, vasodilator, sedative in high doses, antithyroid & lipid lowering drugs, asparaginase, tetracycline, warfarin, amiodarone, tamoxifen, oestrogens, bleomycin, diltiazem, nifedipine, methotrexate, corticosteroids, salicylates Chronic alcoholic (consumed >20g/day), those who were found to be seropositive after blood donation for hepatitis B surface antigen, anti HCV antibody, HIV 1 and 2, and malarial parasite, and serum bilirubin level more than 1.5 mg/dl |
27.0 ± 17.3 97.5th percentile not mentioned |
17.7 ± 11.2 97.5th percentile not mentioned |
| Maksane et al. [11] Western India 2015 |
Blood donors (n = 1059) | Any concurrent acute or chronic illness (including acute febrile illness, thyroid disease, hypertension, diabetes, renal failure, congestive heart disease, chronic respiratory diseases, liver diseases, malabsorption syndromes, and nutritional anemia), Acute viral hepatitis in last 6 months, Intake of tobacco, oral contraceptives, replacement or supplementation therapy such as Insulin intake, Family history of jaundice, H/o hepatotoxic drugs like aspirin, acetaminophen, ibuprofen etc., any other concurrent alternative medications (ayurvedic, homeopathic anticoagulant drugs etc.), Blood transfusion in 6 months, Obese (BMI >30 kg/m2) and pregnancy, severe stress and depression, exercise or physical training in previous days | Median 16 97.5th percentile-36 |
Median 13 97.5th percentile-23 |
| Present study Southern India 2016 |
Healthy people undergoing voluntary health screening (n = 344) | Mentioned under methods | 21.87 ± 2.9 97.5th percentile-28 |
19.35 ± 3.3 97.5th percentile-24 |
The hormonal differences may be attributed for the higher levels of ALT in men. ALT increases with age until fourth decade only to decrease subsequently [12, 13]. In the present study, mean ALT in men aged 50 years and above was less than the younger subjects while no such age distribution was observed in women.
The benefits of lowering upper limit of ALT include (a) early evaluation for liver disease leading to timely treatment and better clinical outcome (b) early detection of drug induced liver injury (c) preventing sub-optimal therapy in chronic hepatic inflammation by targeting a newer lower limit of ALT. However, the disadvantages of lowering upper limit of ALT are (a) over diagnosis leading to unwanted and unnecessary evaluation and treatment (b) increase in patient anxiety (c) rejection of potential blood donors and (d) increase in the use of medical resources.
It has been evident from studies, that individuals with normal ALT by earlier criteria had increased liver-related mortality [14]. Chronic hepatitis B and C patients with persistently normal ALT had significant necro-inflammation or fibrosis ranging from 16 to 37 % [15–17]. Therefore, it seems reasonable to lower the upper limit of normal for ALT, as it increases the sensitivity of screening of asymptomatic individuals for liver disease.
The limitations of our study include estimation of ALT at a single point of time, which may potentially miss the intra-individual variability and small sample size. The later was a result of robust exclusion criteria. The observations of the present study should be applied only to healthy individuals who satisfy our study methods and exclusion criteria. For individuals who are apparently normal but have risk for asymptomatic pathological elevation of ALT (obesity, dyslipidemia, drug intake, etc.), a balance between watchful monitoring and testing for alternate pathologies may be required.
Conclusion
In conclusion, serum ALT (mean and 97.5th percentile) in healthy south Indian population is much lower than the current threshold. The 97.5th percentile for ALT in men and women were 28 and 24 IU/L. There is a need for further large well-designed prospective studies from different regions within the country using uniform entry criteria to establish reproducibility of the present observation.
Compliance with Ethical Standards
Conflict of Interest
None.
References
- 1.Lok AS, McMahon BJ. Chronic hepatitis B: update 2009. Hepatology. 2009;50(3):661–662. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 2.Liaw YF, Kao JH, Piratvisuth T, Chan HL, Chien RN, Liu CJ, et al. Asian-Pacific consensus statement on the management of chronic hepatitis B: a 2012 update. Hepatol Int. 2012;6(3):531–561. doi: 10.1007/s12072-012-9365-4. [DOI] [PubMed] [Google Scholar]
- 3.Tostmann A, Boeree MJ, Aarnoutse RE, de Lange WC, van der Ven AJ, Dekhuijzen R. Antituberculosis drug-induced hepatotoxicity: concise up-to-date review. J Gastroenterol Hepatol. 2008;23(2):192–202. doi: 10.1111/j.1440-1746.2007.05207.x. [DOI] [PubMed] [Google Scholar]
- 4.Prati D, Taioli E, Zanella A, Della Torre E, Butelli S, Del Vecchio E, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002;137(1):1–10. doi: 10.7326/0003-4819-137-1-200207020-00006. [DOI] [PubMed] [Google Scholar]
- 5.Lee JK, Shim JH, Lee HC, Lee SH, Kim KM, Lim YS, et al. Estimation of the healthy upper limits for serum alanine aminotransferase in Asian populations with normal liver histology. Hepatology. 2010;51(5):1577–1583. doi: 10.1002/hep.23505. [DOI] [PubMed] [Google Scholar]
- 6.Park HN, Sinn DH, Gwak GY, Kim JE, Rhee SY, Eo SJ, et al. Upper normal threshold of serum alanine aminotransferase in identifying individuals at risk for chronic liver disease. Liver Int. 2012;32(6):937–944. doi: 10.1111/j.1478-3231.2011.02749.x. [DOI] [PubMed] [Google Scholar]
- 7.Zheng MH, Shi KQ, Fan YC, Liu WY, Lin XF, Li LF, et al. Upper limits of normal for serum alanine aminotransferase levels in Chinese Han population. PLoS One. 2012;7(9):e43736. doi: 10.1371/journal.pone.0043736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kumar S, Amarapurkar A, Amarapurkar D. Serum aminotransferase levels in healthy population from western India. Indian J Med Res. 2013;138(6):894–899. [PMC free article] [PubMed] [Google Scholar]
- 9.Furruqh S, Anitha D, Venkatesh T. Estimation of reference values in liver function test in health plan individuals of an urban south Indian population. Indian J Clin Biochem. 2004;19(2):72–79. doi: 10.1007/BF02894260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yadav D, Mishra S, Gupta M, John PJ, Sharma P. Establishment of reference interval for liver specific biochemical parameters in apparently healthy north Indian population. Indian J Clin Biochem. 2013;28(1):30–37. doi: 10.1007/s12291-012-0281-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Maksane SN, Dandekar SP, Shukla A, Bhatia S. Hepatic enzyme’s reference intervals and their modulating factors in Western Indian population. Indian J Clin Biochem. 2016;31(1):108–116. doi: 10.1007/s12291-015-0508-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Piton A, Poynard T, Imbert Bismut F, Khalil L, Delattre J, Pelissier E, et al. Factors associated with serum alanine transaminase activity in healthy subjects: consequences for the definition of normal values for selection of blood donors and for patients with chronic hepatitis C. MULTIVIRC Group. Hepatology. 1998;27:1213–1219. doi: 10.1002/hep.510270505. [DOI] [PubMed] [Google Scholar]
- 13.Dong MH, Bettencourt R, Barrett-Connor E, Loomba R. Alanine aminotransferase decreases with age: the Rancho Bernardo Study. PLoS One. 2010;5(12):e14254. doi: 10.1371/journal.pone.0014254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim HC, Nam CM, Jee SH, Han KH, Oh DK, Suh I. Normal serum aminotransferase concentration and risk of mortality from liver diseases: prospective cohort study. BMJ. 2004;328:983. doi: 10.1136/bmj.38050.593634.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lai M, Hyatt BJ, Nasser I, Curry M, Afdhal NH. The clinical significance of persistently normal ALT in chronic hepatitis B infection. J Hepatol. 2007;47:760–767. doi: 10.1016/j.jhep.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 16.Kyrlagkitsis I, Portmann B, Smith H, O’Grady J, Cramp ME. Liver histology and progression of fibrosis in individuals with chronic hepatitis C and persistently normal ALT. Am J Gastroenterol. 2003;98(7):1588–1593. doi: 10.1111/j.1572-0241.2003.07539.x. [DOI] [PubMed] [Google Scholar]
- 17.Boccato S, Pistis R, Noventa F, Guido M, Benvegnu L, Alberti A. Fibrosis progression in initially mild chronic hepatitis C. J Viral Hepat. 2006;13:297–302. doi: 10.1111/j.1365-2893.2005.00683.x. [DOI] [PubMed] [Google Scholar]


