Abstract
Objectives
Few studies have assessed outcomes following non-metal-on-metal hip arthroplasty (non-MoMHA) revision surgery performed for adverse reactions to metal debris (ARMD). We assessed outcomes following non-MoMHA revision surgery performed for ARMD, and identified predictors of re-revision.
Methods
We performed a retrospective observational study using data from the National Joint Registry for England and Wales. All non-MoMHAs undergoing revision surgery for ARMD between 2008 and 2014 were included (185 hips in 185 patients). Outcome measures following ARMD revision were intra-operative complications, mortality and re-revision surgery. Predictors of re-revision were identified using Cox regression.
Results
Intra-operative complications occurred in 6.0% (n = 11) of the 185 cases. The cumulative four-year patient survival rate was 98.2% (95% CI 92.9 to 99.5). Re-revision surgery was performed in 13.5% (n = 25) of hips at a mean time of 1.2 years (0.1 to 3.1 years) following ARMD revision. Infection (32%; n = 8), dislocation/subluxation (24%; n = 6), and aseptic loosening (24%; n = 6) were the most common re-revision indications. The cumulative four-year implant survival rate was 83.8% (95% CI 76.7 to 88.9). Multivariable analysis identified three predictors of re-revision: multiple revision indications (hazard ratio (HR) = 2.78; 95% CI 1.03 to 7.49; p = 0.043); selective component revisions (HR = 5.76; 95% CI 1.28 to 25.9; p = 0.022); and ceramic-on-polyethylene revision bearings (HR = 3.08; 95% CI 1.01 to 9.36; p = 0.047).
Conclusions
Non-MoMHAs revised for ARMD have a high short-term risk of re-revision, with important predictors of future re-revision including selective component revision, multiple revision indications, and ceramic-on-polyethylene revision bearings. Our findings may help counsel patients about the risks of ARMD revision, and guide reconstructive decisions. Future studies attempting to validate the predictors identified should also assess the effects of implant design (metallurgy and modularity), given that this was an important study limitation potentially influencing the reported prognostic factors.
Cite this article: G. S. Matharu, A. Judge, D. W. Murray, H. G. Pandit. Outcomes following revision surgery performed for adverse reactions to metal debris in non-metal-on-metal hip arthroplasty patients: Analysis of 185 revisions from the National Joint Registry for England and Wales. Bone Joint Res 2017;6:405–413. DOI: 10.1302/2046-3758.67.BJR-2017-0017.R2.
Keywords: Adverse reactions to metal debris, Complications, Mortality, Non-metal-on-metal hip arthroplasty, Revision surgery
Article focus
Few studies have assessed the outcomes following non-metal-on-metal hip arthroplasty (non-MoMHA) revision surgery performed for adverse reactions to metal debris (ARMD), despite this clinical problem being increasingly reported worldwide.
This study aimed to determine the outcomes following non-MoMHA revision surgery performed for ARMD using National Joint Registry data from England and Wales.
Predictors of future re-revision surgery were also investigated.
Key messages
Non-MoMHA patients undergoing ARMD revision surgery have a high risk of re-revision within four years, with infection, dislocation/subluxation, and aseptic loosening representing the most common re-revision indications.
Predictors of future re-revision risk were revision indications in addition to ARMD, selective component revision procedures, and ceramic-on-polyethylene revision bearings, with the last two representing potentially modifiable factors.
The study findings may be used to counsel non-MoMHA patients about the risks associated with ARMD revision, and to guide decisions about the type of reconstructive procedure to perform.
Strengths and limitations
Study strengths include using linked data from the world’s largest arthroplasty registry, and reporting on the entire population, which decreases the risk of sampling bias.
A major limitation was not having specific implant design information available, such as manufacturer, metallurgy, and details regarding implant modularity. The lack of such data has the potential to influence the reported prognostic factors (such as the importance of the revision bearing surface), and must be considered in future studies attempting to validate the present findings.
An important limitation is that surgeons may have either incorrectly coded ARMD revisions using other indications (such as infection), or alternatively made a diagnosis of ARMD that was subsequently not confirmed histopathologically.
Introduction
Metal-on-metal hip arthroplasty (MoMHA) has resulted in high short-term rates of failure.1,2 Many MoMHA revisions have been performed for adverse reactions to metal debris (ARMD),3,4 with poor short-term outcomes reported following ARMD revision.5,6 Dislocation, recurrence of ARMD, and acetabular loosening represent the most common modes of failure following MoMHA revision for ARMD.7
Recent studies have reported on non-MoMHAs requiring revision surgery for ARMD, with failures generally occurring in newer implant designs with large femoral head sizes.8-14 In the absence of metal-on-metal bearings, ARMD in non-MoMHAs has been attributed to wear and mechanically assisted crevice corrosion occurring at modular implant junctions (head-taper and taper-stem).8-14 In light of these problems, patients with certain non-MoMHA designs now require regular follow-up, with a low threshold recommended for performing a systematic evaluation.15
Although a number of studies have observed ARMD failures after non-MoMHA,8-11,14 few have detailed the outcomes following revision surgery.16 Three studies have reported short-term outcomes following ARMD revision surgery performed in non-MoMHAs (mean follow-up 18 to 25 months), with two studies involving small cohorts.12,13,17 Complications (19% to 29%) and re-revisions (8% to 29%) were frequently observed following ARMD revision, with failures most commonly due to ARMD recurrence, dislocation and infection.12,13,17
At present, the true risk of ARMD failure in non-MoMHAs remains unknown. One recent study has estimated the risk of ARMD revision in non-MoMHAs to be 0.25%.12 Although this is lower than the current 3.7% risk of ARMD revision in MoMHAs, it is worth acknowledging that the risk in MoMHA patients was 0.15% in 2009, which represents a time when little was known about ARMD in MoMHAs.3 Given the widespread use of newer non-MoMHA designs with large femoral head sizes and modular junctions,3,4 it is expected that the risk of ARMD revision surgery in non-MoMHA patients will increase with time. Therefore, it is important that surgeons have information about the expected outcomes following ARMD revision so that patients can be appropriately counselled about the risks of further intervention. In addition, identifying prognostic factors of outcome following ARMD revision may assist decision-making about the reconstructive procedure and post-operative follow-up regimen. Large cohort studies would help answer these important clinical questions.
The National Joint Registry (NJR) for England and Wales was established in April 2003 to identify poorly performing implants early, and is the world’s largest arthroplasty registry.3 We used NJR data to: (1) determine the outcomes following non-MoMHA revision surgery performed for ARMD; (2) establish the indications for re-revision surgery; and (3) identify predictors of re-revision surgery.
Patients and Methods
A retrospective observational study was performed using data from the NJR for England and Wales. Data were obtained on 07 December 2015. This dataset included details of all primary stemmed non-MoMHAs which subsequently underwent revision surgery for adverse soft-tissue reaction to particulate debris as recorded in the NJR between 01 June 2008 and 07 December 2014 (n = 194). We have elected to classify this revision indication as ARMD throughout, which is currently the most commonly used term.18 The former date is when the NJR introduced ARMD as a formal indication for revision surgery. The latter date ensured outcomes after ARMD revision were reported at a minimum of one-year follow-up. Before obtaining the dataset, the NJR database was linked with the Office for National Statistics database (provides data on all-cause patient mortality and time to death) using unique patient identifiers.
Hips undergoing staged (two or more) revision procedures for ARMD were subsequently excluded (n = 9). As registries do not record the results of microbiological and histopathological analysis of tissues excised at revision, it is possible that these staged procedures may have been performed for undiagnosed infection. The final cohort for analysis therefore included 185 primary non-MoMHAs in 185 patients undergoing single-stage revision surgery for ARMD. Revision procedures were performed by 140 surgeons (surgeons performed between one and five cases) at 109 centres (between one and nine cases were carried out at each centre). These 185 revisions were either complete revision procedures (all components from the primary arthroplasty were revised at revision) or selective component revision procedures. Selective component revision procedures included cases where at least one component from the primary arthroplasty procedure was retained at revision. This included either the femoral or acetabular component being retained at revision, or both the femoral and acetabular components being retained, with revision of the femoral head and liner (with or without the use of a taper adapter).
Unique patient identifiers allowed linkage of all ARMD revision procedures to the primary non-MoMHA surgery as well as to any re-revisions. For all procedures, the NJR collects data on patient demographics (age, gender, body mass index (BMI), American Society of Anesthesiologists grade19) and the surgical procedure (indication, venous thromboembolism prophylaxis, surgeon grade, approach, and the components implanted). NJR data for revision operations also include details of intra-operative findings. Patient and surgical factors relating to the ARMD revision were used as covariates when assessing predictors of re-revision surgery. For the components implanted at primary and revision surgery, the NJR provided data on the bearing surface, femoral head size, and implant fixation. Although the NJR does collect data on the specific implant design and manufacturer of all arthroplasty components, this information was not approved for release due to ongoing negotiations between the NJR and the various manufacturers. Therefore, for the current study it was not possible to identify the specific implants used; the metallurgy and nature of any modular junctions were not known.
Study outcome measures were: intra-operative complications during ARMD revision; all-cause mortality following ARMD revision; and all-cause re-revision surgery following ARMD revision. Intra-operative complications recorded by the NJR include calcar crack, pelvic and/or femoral shaft penetration, trochanteric and/or femoral shaft fracture, and other complications.
Statistical analysis
All data analyses were performed using Stata Version 13.1 (StataCorp, College Station, Texas). Differences in patient and surgical factors between re-revised and non-re-revised hips were assessed using either unpaired t-tests or the Wilcoxon rank-sum test (numerical data), and either the chi-squared test or Fisher’s exact test (categorical data). Cumulative patient and implant survival rates following ARMD revision were determined using the Kaplan-Meier method. Re-revision surgery (removal or exchange of any component, which included isolated revisions of the femoral head and acetabular liner) was the endpoint for implant survival. Patients who had not died and who were not undergoing re-revision were censored on the study end date (07 December 2015).
Cox proportional hazards models (univariable and multivariable) were used to identify predictors of re-revision surgery. Linearity of continuous predictors with outcome (re-revision) was assessed using fractional polynomials, with data grouped if effects were non-linear. The proportional hazards assumption was examined and satisfied for all predictors. Covariates were included in the final multivariable model if p < 0.20 in the univariable analysis. The significance level for all analyses was p < 0.05, with 95% confidence intervals (CI) also used.
Results
Revision surgery for ARMD was performed in 185 patients with 185 non-MoMHAs (Table I). During the study period, 10 496 non-MoMHA revisions (with a linked primary non-MoMHA within the NJR) were performed for all causes.3 Therefore, the risk of ARMD revision surgery in all revised non-MoMHAs with a linked primary was 1.8%. During the study period, 451 664 primary non-MoMHAs were implanted.3 Therefore, the risk of ARMD revision surgery in all primary non-MoMHAs was 0.041%.
Table I.
Patient and surgical factors for all non-metal-on-metal hip arthroplasties revised for adverse reactions to metal debris (ARMD), and in hips not undergoing re-revision surgery compared with those undergoing re-revision surgery
| Covariate | All ARMD hip revisions (n = 185) (100%) | ARMD hip revisions not undergoing re-revision surgery (n = 160) (86.5%) | ARMD hip revisions undergoing re-revision surgery (n = 25) (13.5%) | p-value |
|---|---|---|---|---|
| Female | 119 (64.3) | 101 (63.1) | 18 (72.0) | 0.389 |
| Age at revision (yrs), mean (sd) | 66.4 (10.6) | 67.0 (10.8) | 62.8 (9.0) | 0.046 |
| BMI (kg/m2)*, mean (sd) | 28.2 (5.0) | 28.1 (4.9) | 29.3 (6.5) | 0.589 |
| Time from primary to revision (yrs), mean (sd) | 3.1 (2.6) | 3.2 (2.7) | 2.8 (2.0) | 0.363 |
| Yr revision performed | ||||
| 2008 to 2011 | 56 (30.3) | 45 (28.1) | 11 (44.0) | 0.108 |
| 2012 to 2014 | 129 (69.7) | 115 (71.9) | 14 (56.0) | |
| ASA grade at revision | ||||
| 1 | 33 (17.8) | 30 (18.8) | ‡ | 0.234 |
| 2 | 128 (69.2) | 107 (66.9) | 21 (84.0) | |
| 3 | 24 (13.0) | 23 (14.4) | ‡ | |
| VTE – chemical | ||||
| LMWH (+/-other) | 114 (61.6) | 98 (61.3) | 16 (64.0) | 0.270 |
| Aspirin only | 10 (5.4) | 9 (5.6) | ‡ | |
| Other | 52 (28.1) | 47 (29.4) | ‡ | |
| None | 9 (4.9) | 6 (3.8) | ‡ | |
| VTE – mechanical (any versus none) | 180 (97.3) | 155 (96.9) | 25 (100) | 1.00 |
| Revision surgeon grade (consultant versus other) | 176 (95.1) | 152 (95.0) | 24 (96.0) | 1.00 |
| Surgical approach (posterior versus other) | 127 (68.7) | 108 (67.5) | 19 (76.0) | 0.394 |
| Revision indications/intra-operative findings | ||||
| ARMD (+/-pain) only | 82 (44.3) | 74 (46.3) | 8 (32.0) | 0.182 |
| Additional indications | 103 (55.7) | 86 (53.8) | 17 (68.0) | |
| ARMD | 185 (100) | § | § | § |
| Pain | 41 (22.2) | § | § | § |
| Aseptic loosening (any) | 45 (24.3) | § | § | § |
| Acetabular | 27 (14.6) | |||
| Femoral | 23 (12.4) | |||
| Osteolysis (any) | 21 (11.4) | § | § | § |
| Acetabular | 13 (7.0) | |||
| Femoral | 13 (7.0) | |||
| Other abnormal findings | ‡ | § | § | § |
| Implant malalignment | 18 (9.7) | § | § | § |
| Acetabular liner wear | 23 (12.4) | § | § | § |
| Fracture | 9 (4.9) | § | § | § |
| Dislocation/subluxation | 17 (9.2) | § | § | § |
| Infection | ‡ | § | § | § |
| Incorrect implant size | ‡ | § | § | § |
| Liner dissociation | 8 (4.3) | § | § | § |
| Implant fracture | 9 (4.9) | § | § | § |
| Revision procedure | ||||
| Selective component† | 134 (72.4) | 111 (69.4) | 23 (92.0) | 0.017 |
| All component | 51 (27.6) | 49 (30.6) | ‡ | |
| Revision femoral head size (mm)* | ||||
| Mean (sd) | 33.1 (3.7) | 33.1 (3.6) | 33.1 (4.3) | 0.969 |
| Range | 22.25 to 40 | 22.25 to 40 | 22.25 to 40 | |
| ≤ 28 | 42 (23.5) | 37 (23.7) | ‡ | 0.975 |
| 32 | 52 (29.1) | 45 (28.9) | 7 (30.4) | |
| ≥ 36 | 85 (47.5) | 74 (47.4) | 11 (47.8) | |
| Revision bearing* (n, %) | ||||
| MoP | 87 (51.5) | 81 (54.7) | 6 (28.6) | 0.072 |
| CoC | 45 (26.6) | 37 (25.0) | 8 (38.1) | |
| CoP | 37 (21.9) | 30 (20.3) | 7 (33.3) | |
| Revision component fixation | ||||
| Uncemented | 90 (81.8) | 81 (81.8) | 9 (81.8) | 1.00 |
| Cemented | 20 (18.2) | 18 (18.2) | ‡ | |
| Revision stem fixation | ||||
| Uncemented | 43 (51.2) | 39 (50.0) | ‡ | 0.676 |
| Cemented | 41 (48.8) | 39 (50.0) | ‡ | |
| Bone graft (femoral) | 7 (3.8) | 7 (4.4) | 0 (0) | 0.596 |
| Bone graft (acetabular) | 27 (14.6) | 22 (13.8) | ‡ | 0.375 |
missing data for stated number of hips: BMI (n = 72); revision femoral head size (n = 6); revision bearing surface (n = 16)
selective component revision procedures included cases where at least one component from the primary arthroplasty procedure was retained at revision. This included either the femoral or acetabular component being retained at revision, or both the femoral and acetabular components being retained, with revision of the femoral head and liner (with or without the use of a taper adapter)
data suppressed due to small count within the cell. The actual number was between one and five
due to small numbers, statistical comparisons between hips re-revised and hips not re-revised have not been performed for the individual revision indications
ASA, American Society of Anesthesiologists; BMI, body mass index; CoC, ceramic-on-ceramic; CoP, ceramic-on-polyethylene; LMWH, low-molecular weight heparin; MoP, metal-on-polyethylene; VTE, venous thromboembolism
All values in the table are number, with the percentages in brackets, unless otherwise indicated
Statistically significant differences between the re-revised and non re-revised hips (p < 0.05) are highlighted in bold text
The non-MoMHA bearing surfaces most frequently revised for ARMD were metal-on-polyethylene (44.9%; n = 83), followed by ceramic-on-ceramic (35.7%; n = 66), and ceramic-on-polyethylene (11.4%; n = 21). The femoral head size of the primary arthroplasty was most commonly 28 mm or less (38.9%; n = 72), followed by 36 mm (35.1%; n = 65) and 32 mm (20.0%; n = 37). Primary acetabular (86.5%; n = 160) and femoral (71.8%; n = 130) components were predominantly uncemented.
Intra-operative complications
Intra-operative complications occurred in 6.0% (n = 11) of hips. The most common complications were calcar fracture (n = 3) and greater trochanteric fracture (n = 3).
Patient mortality
Overall mortality following revision surgery was 1.1% (n = 2). Deaths occurred at 2.1 years and 2.4 years following ARMD revision; neither patient underwent re-revision surgery before death. The cumulative four-year patient survival rate following ARMD revision was 98.2% (95% CI 92.9 to 99.5).
Re-revision surgery
Re-revision surgery was performed in 13.5% (n = 25) of hips at a mean time of 1.2 years (0.1 to 3.1 years) following ARMD revision. In hips undergoing re-revision, 32% (n = 8) had more than one indication for failure. Infection (32%; n = 8), dislocation or subluxation (24%; n = 6), and aseptic loosening (24%; n = 6) were the most common re-revision indications (Table II). The mean follow-up time for hips not undergoing re-revision surgery was 3.1 years (1.0 to 7.2 years). The cumulative four-year implant survival rate following ARMD revision was 83.8% (95% CI 76.7 to 88.9) (Fig. 1). The risk of re-revision surgery by type of initial revision procedure performed was as follows: 36% (9/25) acetabular component only revision; 36% (9/25) femoral head and liner exchange alone; 20% (5/25) femoral component only revision; 8% (2/25) all component revision.
Table II.
Indications for hips undergoing re-revision surgery following revision surgery performed for adverse reactions to metal debris (n = 25)
| Re-revision indications and intra-operative findings | Number of events (%) |
|---|---|
| All indications | |
| Overall | 37 in 25 re-revised hips |
| Hips with one re-revision indication | 17 (68) |
| Hips with two to four re-revision indications | 8 (32) |
| Deep infection | 8 (32) |
| Dislocation/subluxation | 6 (24) |
| Aseptic loosening (acetabular or femoral) | 6 (24) |
| Adverse reactions to metal debris | 3 (12) |
| Osteolysis (acetabular or femoral) | 3 (12) |
| Pain | 3 (12) |
| Liner dissociation | 3 (12) |
| Other (including femoral malalignment, periprosthetic fracture, and implant fracture) | 5 (20) |
Fig. 1.
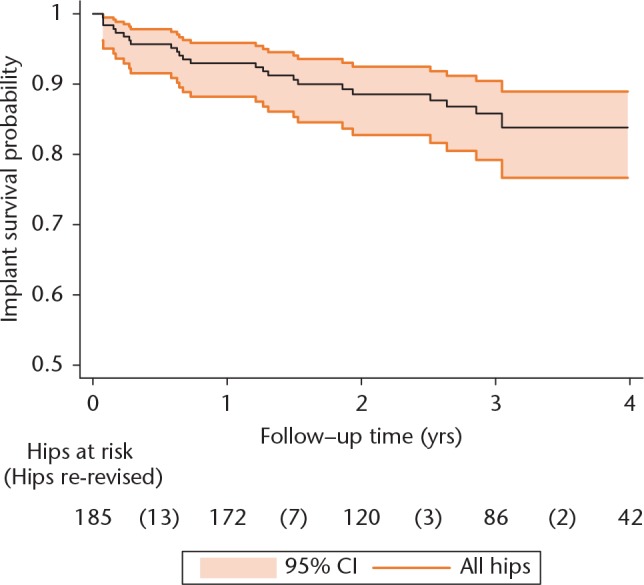
Implant survival rate following revision surgery performed for adverse reactions to metal debris at up to four years. Shaded area represents the respective upper and lower limits of the 95% confidence intervals (CIs). Risk table indicates the number of hips at risk at one-year intervals, with the corresponding number in brackets detailing the number of hips undergoing re-revision surgery during each one-year interval. The cumulative four-year implant survival rate was 83.8% (95% CI 76.7 to 88.9).
Predictors of re-revision surgery
Univariable analysis identified the type of revision procedure performed as the only significant predictor of re-revision surgery (Table III). Selective component revision procedures were associated with an increased risk of re-revision compared with all component revisions (hazard ratio (HR) = 5.01; 95% CI 1.18 to 21.3; p = 0.029).
Table III.
Univariable and multivariable Cox regression analysis to identify predictors of re-revision surgery following revision surgery performed for adverse reactions to metal debris (ARMD)
| Covariate | Univariable hazard ratio (95% CI) | p-value | Multivariable hazard ratio (95% CI) | p-value |
|---|---|---|---|---|
| Gender (female versus male) | 1.41 (0.59 to 3.37) | 0.443 | * | * |
| Age at revision (per yr) | 0.97 (0.94 to 1.00) | 0.072 | 0.97 (0.93 to 1.01) | 0.165 |
| BMI (per kg/m2) | 1.04 (0.93 to 1.17) | 0.464 | * | * |
| Time from primary to revision (per yr) | 0.96 (0.82 to 1.13) | 0.659 | * | * |
| ASA grade at revision | ||||
| 1 | 1.00 | Ref | * | * |
| 2 | 1.95 (0.58 to 6.54) | 0.280 | ||
| ⩾ 3 | 0.46 (0.05 to 4.44) | 0.504 | ||
| VTE – chemical | ||||
| None | 1.00 | Ref | 1.00 | Ref |
| LMWH (+/-other) | 0.47 (0.14 to 1.60) | 0.227 | 0.26 (0.07 to 1.02) | 0.053 |
| Aspirin only | 0.28 (0.03 to 2.70) | 0.271 | 0.35 (0.03 to 3.65) | 0.378 |
| Other | 0.31 (0.07 to 1.31) | 0.111 | 0.21 (0.04 to 1.05) | 0.057 |
| VTE – mechanical (any versus none) | † | † | * | * |
| Revision surgeon grade (consultant versus other) | 1.23 (0.17 to 9.06) | 0.842 | * | * |
| Surgical approach (posterior versus other) | 1.48 (0.59 to 3.70) | 0.407 | * | * |
| Revision indications | ||||
| ARMD (+/-pain) only | 1.00 | Ref | 1.00 | Ref |
| Additional indications | 1.76 (0.76 to 4.09) | 0.186 | 2.78 (1.03 to 7.49) | 0.043 |
| Revision procedure‡ | ||||
| All components revised | 1.00 | Ref | 1.00 | Ref |
| Selective component revision | 5.01 (1.18 to 21.3) | 0.029 | 5.76 (1.28 to 25.9) | 0.022 |
| Revision femoral head size (in mm) | ||||
| ⩽ 28 | 1.00 | Ref | * | * |
| 32 | 1.09 (0.35 to 3.44) | 0.882 | ||
| ⩾ 36 | 1.11 (0.39 to 3.20) | 0.845 | ||
| Revision bearing | ||||
| MoP | 1.00 | Ref | 1.00 | Ref |
| CoC | 2.84 (0.98 to 8.18) | 0.054 | 1.79 (0.54 to 5.89) | 0.339 |
| CoP | 2.96 (1.00 to 8.83) | 0.051 | 3.08 (1.01 to 9.36) | 0.047 |
| Revision cup fixation | ||||
| Uncemented | 1.00 | Ref | * | * |
| Cemented | 0.99 (0.21 to 4.60) | 0.993 | ||
| Revision stem fixation | ||||
| Uncemented | 1.00 | Ref | * | * |
| Cemented | 0.51 (0.09 to 2.80) | 0.440 | ||
| Bone graft (femoral) | † | † | * | * |
| Bone graft (acetabular) | 1.31 (0.49 to 3.50) | 0.590 | * | * |
covariate was not eligible for inclusion in the final multivariable model
unable to calculate value as no hips in this subgroup underwent re-revision surgery
selective component revision procedures included cases where at least one component from the primary arthroplasty procedure was retained at revision. This included either the femoral or acetabular component being retained at revision, or both the femoral and acetabular components being retained, with revision of the femoral head and liner (with or without the use of a taper adapter)
ASA, American Society of Anesthesiologists; BMI, body mass index; CI, confidence interval; CoC, ceramic-on-ceramic; CoP, ceramic-on-polyethylene; LMWH, low-molecular weight heparin; Ref, reference group; MoP, metal-on-polyethylene; VTE, venous thromboembolism
Statistically significant differences (p < 0.05) have been highlighted in bold text
Due to missing BMI data, the univariable analysis for BMI was based on a cohort of 113 hip revisions with ten hips undergoing re-revision surgery
Multivariable analysis was based on a cohort of 167 hip revisions with 21 hips undergoing re-revision surgery
In an adjusted multivariable model, three significant predictors of re-revision surgery were identified. Hips with revision indications in addition to ARMD (+/-pain) had a higher risk of re-revision compared with hips revised for ARMD (+/-pain) alone (HR = 2.78; 95% CI 1.03 to 7.49; p = 0.043). Selective component revision procedures were associated with an increased risk of re-revision compared with all component revisions (HR = 5.76; 95% CI 1.28 to 25.9; p = 0.022). Ceramic-on-polyethylene revision bearings had an increased risk of re-revision compared with hips revised with metal-on-polyethylene bearings (HR = 3.08; 95% CI 1.01 to 9.36; p = 0.047).
Discussion
Failure of non-MoMHA designs due to ARMD represents an emerging clinical problem.8-14 Early outcomes following ARMD revision surgery performed in MoMHA patients have largely been poor.5-7 However, little is known about the outcomes following ARMD revision performed in non-MoMHA patients, with previous studies involving small cohorts.12,13 Analysis of a large cohort of ARMD revision procedures performed in non-MoMHAs has demonstrated that patients have a high risk of re-revision surgery within four years. Predictors of future re-revision were revision indications in addition to ARMD, selective component revision procedures, and ceramic-on-polyethylene revision bearings.
Outcomes: intra-operative complications and patient mortality
The frequency of intra-operative complications in hips undergoing ARMD revision observed in this study was similar to that found in previous non-MoMHA revision cohorts.20,21 Fractures of the proximal femur were the most common intra-operative complication in all studies, which illustrates the potential difficulty associated with removing well-fixed stemmed components.20,21 In addition, the risk of mortality following ARMD revision was observed to be low in our series, which is in line with previous work.3,22
Outcomes: re-revision surgery
The short-term risk of re-revision following ARMD revision surgery in non-MoMHA patients was high. The proportion of re-revisions in our series (13.5%) was comparable with that observed following ARMD revision in non-MoMHA patients (8% to 29%),12,13,17 though these previous reports had shorter follow-up periods compared with the current study. The implant survival rate following ARMD revision of 83.8% at four years was similar to that reported in the only other large cohort of non-MoMHA ARMD revisions (86% at 2.5 years).17 However, our reported implant survival following ARMD revision represents the best-case scenario because registries may underreport arthroplasty failures.23,24 If the early observations of outcomes following ARMD revision in MoMHA patients are excluded,5 implant survival following non-MoMHA revision for ARMD appears inferior to both that reported following MoMHA revision for ARMD25-27 and following revision of non-MoMHAs for conventional indications.28,29 Even when compared with data from the same registry, the re-revision rates following ARMD revision surgery in non-MoMHAs reported in this study are high. The five-year implant survival rates following all-cause non-MoMHA revision surgery recorded in the NJR are 87.8% to 89.1% for primary metal-on-polyethylene arthroplasties (depending on fixation), and 88.2% for primary uncemented ceramic-on-ceramic arthroplasties.3 This high short-term re-revision rate following ARMD revision in non-MoMHA patients is concerning. We therefore recommend careful surveillance of these patients following ARMD revision surgery.
Re-revisions following ARMD revision surgery were performed early (mean 1.2 years), with the most common re-revision indications similar to previous reports in both non-MoMHAs and MoMHAs revised for ARMD.7,12,13,17 Multiple surgeries, incomplete excision of metal debris/necrotic tissue, and retained components from the primary arthroplasty may contribute to deep infection following ARMD revision.7 Risk factors for hip instability include destructive ARMD lesions requiring extensive soft-tissue debridement, reduction of the femoral head diameter, and cases where suboptimal primary component positioning may be accepted because of the potential risks associated with removing well-fixed acetabular and femoral components.6,25 Aseptic loosening of revision components may occur because of ARMD-induced osteolysis.6,7 Although ARMD recurrence has frequently been reported following ARMD revision in both non-MoMHA and MoMHA patients,7,12,13,17 it was not commonly observed in the present study. This variance may be due to multiple factors, such as the different types of primary and revision implants used in each study, the severity of ARMD, and the completeness of ARMD excision performed. Further work is needed to understand why ARMD recurs following revision and how recurrence can be minimised.
Predictors of re-revision surgery
Our final multivariable model identified three predictors of future re-revision risk, all with large effect sizes. However, the lack of implant design data available for the revised arthroplasty (including manufacturer, metallurgy, and details about modularity) limits the clinical significance of the three predictors given that these implant design details may represent confounding factors that were truly responsible for the associations identified in the present study.
Hips with revision indications in addition to ARMD were almost three times more likely to be re-revised compared with hips revised for ARMD alone. Aseptic loosening, acetabular liner wear, osteolysis, implant malalignment, and dislocation/subluxation were the most common additional indications for revision (Table I). Adverse intra-operative findings in addition to ARMD have frequently been reported in MoMHA patients.25,26,30 Although ARMD complicated by other adverse features would be expected to be associated with inferior outcomes following revision, such a relationship has yet to be established in MoMHA revisions.25,26,30 We have identified multiple revision indications as a poor prognostic factor following ARMD revision in non-MoMHA patients. If these additional abnormalities reflect more advanced ARMD, the regular follow-up currently recommended for certain non-MoMHA designs may assist detection of ARMD at an earlier stage with the potential for improved post-revision outcomes. There is evidence that such an approach can improve outcomes in MoMHA patients revised for ARMD.25
The risk of re-revision was six times higher in hips undergoing selective component revision procedures compared with all component revisions, with 92% of re-revisions in our series initially undergoing selective component revisions. This mirrors observations following MoMHA revision.25,31 When performing ARMD revision surgery in patients with stemmed implants, well-fixed and adequately positioned components are frequently retained, with adapters used if tapers are not severely damaged or corroded.6,12,13,32 Selective component revisions reduce the perceived morbidity associated with removing well-fixed components.20,33 However, there is limited data to support this strategy in non-MoMHAs with ARMD. Selective component revision was the strongest risk factor for re-revision in the present study. Given the most common indications for re-revision (infection, instability and aseptic loosening), it is possible that these failures occurred due to occult or unrecognised infection or component loosening at the ARMD revision procedure. Furthermore, there can be difficulties optimising soft-tissue tension and component positioning (namely combined version) when performing selective revisions, which increases the risk of subsequent hip instability.6,12,13 Therefore, our findings do not support selective component revision procedures as a universal approach for managing non-MoMHAs with ARMD. If surgeons do perform such revisions, it is important to counsel patients pre-revision about the increased risk of future procedures. These patients should also undergo regular follow-up post-revision given the increased risk of short-term failure.
Presently, there is no consensus on which bearing surface to implant when revising non-MoMHAs for ARMD. Ceramic bearings and metal-on-polyethylene articulations have most commonly been used at revision, with a preference for ceramic heads in order to avoid further taper corrosion which can occur with metal femoral heads.12,13,17 We observed ceramic-on-polyethylene revision bearings to have a three-fold increased risk of re-revision compared with hips revised with metal-on-polyethylene bearings. Registries have reported ceramic-on-polyethylene bearings to have the lowest rates of failure when used in primary arthroplasty,3,4 therefore it is unclear why ceramic-on-polyethylene bearings had an increased risk of re-revision when used at ARMD revision. Given that this finding reached borderline significance in the multivariable model, and that there was no prior belief that ceramic-on-polyethylene revision bearings would be associated with a higher re-revision risk, we cannot exclude a type I error. As data were not available on implant design, metallurgy and the nature of any modular junctions, the study findings may have been confounded by factors that were not assessed. As a result, rates of failure may not truly be influenced by the revision bearing surface, but instead by factors which are associated with implantation of ceramic-on-polyethylene bearings at revision, such as stem design or other unrecognised confounding factors. We recommend other large independent datasets be assessed to determine the significance of this particular result, with such analyses adjusting for any potential implant-related confounding factors.
Strengths and limitations
Study strengths include using linked data from the world’s largest arthroplasty registry, which contains details of the primary surgery and any subsequent procedures. Furthermore, reporting on the entire population decreases the risk of sampling bias. It is therefore likely that our findings have good external validity and generalisability, however, this requires validation in future studies.
This study has a number of limitations. A major limitation was not having specific implant design information available for the revised arthroplasty, such as the manufacturer, metallurgy, and details regarding implant modularity. The lack of such data has the potential to influence the reported prognostic factors (such as the importance of the revision bearing surface), which must be considered and adjusted for in future studies attempting to validate the present findings. A further substantial limitation was that the absolute number of ARMD revisions and subsequent re-revisions was small, a fact which is suspected to be largely responsible for the broad confidence intervals observed for the three significant predictors of re-revision surgery. Although this study can conclude that the three predictors of re-revision surgery were statistically significant, the true magnitude of the effect sizes for each predictor is less certain given the broad confidence intervals. Therefore, this study cannot definitively establish whether the predictors of re-revision identified were truly clinically significant. It is therefore important for further research to be performed in this area using larger cohorts of non-MoMHA patients undergoing ARMD revision, though this may be difficult given that only small cohorts have currently been reported.8-13 A further limitation is using observational data which makes it difficult to infer causality. Our patient cohort was also subject to sampling bias. Given ARMD associated with non-MoMHAs was only described recently,8-11 surgeons may have incorrectly coded ARMD revisions using other indications, namely infection. The NJR would not have captured such cases. By contrast, some surgeons may have made a diagnosis of ARMD that was subsequently not confirmed following histopathological and microbiological analysis of intra-operative samples. Such cases may therefore have been inappropriately included in the present study cohort. Furthermore, although we have classified these revisions as performed for ARMD, the aetiology and pathogenesis of this condition remains unknown;8-14 we cannot be certain that the reaction is specifically to metal debris.
Given the relatively small cohort size, it is possible that missing data for some variables, such as BMI and revision bearing surface, may have affected our analyses and subsequent interpretation of the data. Although the multivariable models used to identify predictors of re-revision surgery were adjusted for other relevant clinical factors, the comparisons presented in Table I were not adjusted statistically for multiple comparisons, which is acknowledged as a limitation. As ARMD became a revision indication in the NJR in 2008,3 only short-term outcomes following revision were available. Despite using linked data, it is feasible that some re-revision procedures were not captured by the NJR.23,24 Registries do not record non-revision procedures (washouts or closed hip reductions) or patient-reported outcomes following revision.3,4 Consequently, these endpoints could not be assessed but are acknowledged to be important when determining clinical outcomes following reconstructive procedures. Finally, our findings may not be applicable to non- MoMHA patients following staged ARMD revision procedures.
In conclusion, non-MoMHA patients undergoing ARMD revision surgery have a high risk of re-revision within four years. Infection, dislocation/subluxation, and aseptic loosening were the most common re-revision indications. Predictors of future re-revision risk were revision indications in addition to ARMD, selective component revision procedures, and ceramic-on-polyethylene revision bearings. Our findings may be used to: (1) counsel non-MoMHA patients about the risks associated with ARMD revision; and (2) guide decisions about the type of reconstructive procedure to perform. However, future studies are needed to assess the predictors identified. These should also assess the effects of implant design (manufacturer, metallurgy, and nature of the modular junctions), given that this was a significant study limitation potentially influencing the reported prognostic factors (such as the importance of the revision bearing surface).
Footnotes
Author Contribution: G. S. Matharu: Study design, Data analysis and interpretation, Manuscript draft, Revision and approval.
A. Judge: Study design, Data analysis and interpretation, Manuscript revision and approval.
D. W. Murray: Study design, Data interpretation, Manuscript revision and approval.
H. G. Pandit: Study design, Data interpretation, Manuscript revision and approval.
Conflicts of Interest Statement: One of the authors provides expert testimony to Kennedys Law, which includes work relating to metal-on-metal hip replacements.
Funding Statement
One author received funding from Arthritis Research UK (Grant reference number 21006) and The Orthopaedics Trust to undertake the work contained within this manuscript. These funders had no role in the study design, data collection, analysis and interpretation, decision to publish, or preparation of the manuscript. The authors would like to thank the patients and staff of all of the hospitals in England, Wales and Northern Ireland which have contributed data to the National Joint Registry. We are grateful to the Healthcare Quality Improvement Partnership (HQIP), the NJR Research Sub-committee and staff at the NJR Centre for facilitating this work. The authors have conformed to the NJR’s standard protocol for data access and publication. The views expressed represent those of the authors and do not necessarily reflect those of the NJR Steering Committee or HQIP who do not vouch for how the information is presented. The Healthcare Quality Improvement Partnership (“HQIP”) and/or the National Joint Registry (“NJR”) take no responsibility for the accuracy, currency, reliability and correctness of any data used or referred to in this report, nor for the accuracy, currency, reliability and correctness of links or references to other information sources and disclaim all warranties in relation to such data, links and references to the maximum extent permitted by legislation
References
- 1. Smith AJ, Dieppe P, Vernon K, Porter M, Blom AW; National Joint Registry of England and Wales. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry for England and Wales. Lancet 2012;379:1199–1204. [DOI] [PubMed] [Google Scholar]
- 2. Smith AJ, Dieppe P, Howard PW, Blom AW, National Joint Registry for England and Wales. Failure rates of metal-on-metal hip resurfacings: analysis of data from the National Joint Registry for England and Wales. Lancet 2012;380:1759-1766. [DOI] [PubMed] [Google Scholar]
- 3. National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. 13th Annual Report 2016. http://www.njrcentre.org.uk/njrcentre/Portals/0/Documents/England/Reports/13th%20Annual%20Report/07950%20NJR%20Annual%20Report%202016%20ONLINE%20REPORT.pdf (last accessed 12 May 2017).
- 4. Australian Orthopaedic Association. National Joint Replacement Registry: Hip, Knee & Shoulder Arthroplasty. Annual Report 2016. https://aoanjrr.sahmri.com/documents/10180/275066/Hip%2C%20Knee%20%26%20Shoulder%20Arthroplasty (last accessed 12 May 2017).
- 5. Grammatopoulos G, Pandit H, Kwon YM, et al. Hip resurfacings revised for inflammatory pseudotumour have a poor outcome. J Bone Joint Surg [Br] 2009;91-B:1019-1024. [DOI] [PubMed] [Google Scholar]
- 6. Munro JT, Masri BA, Duncan CP, Garbuz DS. High complication rate after revision of large-head metal-on-metal total hip arthroplasty. Clin Orthop Relat Res 2014;472:523-528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Matharu GS, Pynsent PB, Dunlop DJ. Revision of metal-on-metal hip replacements and resurfacings for adverse reaction to metal debris: a systematic review of outcomes. Hip Int 2014;24:311-320. [DOI] [PubMed] [Google Scholar]
- 8. Cooper HJ, Della Valle CJ, Berger RA, et al. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg [Am] 2012;94-A:1655-1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Cooper HJ, Urban RM, Wixson RL, Meneghini RM, Jacobs JJ. Adverse local tissue reaction arising from corrosion at the femoral neck-body junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg [Am] 2013;95-A:865-872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Molloy DO, Munir S, Jack CM, et al. Fretting and corrosion in modular-neck total hip arthroplasty femoral stems. J Bone Joint Surg [Am] 2014;96-A:488-493. [DOI] [PubMed] [Google Scholar]
- 11. Meftah M, Haleem AM, Burn MB, Smith KM, Incavo SJ. Early corrosion-related failure of the rejuvenate modular total hip replacement. J Bone Joint Surg [Am] 2014;96-A:481-487. [DOI] [PubMed] [Google Scholar]
- 12. Whitehouse MR, Endo M, Zachara S, et al. Adverse local tissue reactions in metal-on-polyethylene total hip arthroplasty due to trunnion corrosion: the risk of misdiagnosis. Bone Joint J 2015;97-B:1024-1030. [DOI] [PubMed] [Google Scholar]
- 13. Plummer DR, Berger RA, Paprosky WG, et al. Diagnosis and management of adverse local tissue reactions secondary to corrosion at the head-neck junction in patients with metal on polyethylene bearings. J Arthroplasty 2016;31:264-268. [DOI] [PubMed] [Google Scholar]
- 14. Nawabi DH, Do HT, Ruel A, et al. Comprehensive analysis of a recalled modular total hip system and recommendations for management. J Bone Joint Surg [Am] 2016;98-A:40-47. [DOI] [PubMed] [Google Scholar]
- 15. Kwon YM, Fehring TK, Lombardi AV, et al. Risk stratification algorithm for management of patients with dual modular taper total hip arthroplasty: consensus statement of the American Association of Hip and Knee Surgeons, the American Academy of Orthopaedic Surgeons and the Hip Society. J Arthroplasty 2014;29:2060-2064. [DOI] [PubMed] [Google Scholar]
- 16. Weiser MC, Chen DD. Revision for taper corrosion at the neck-body junction following total hip arthroplasty: pearls and pitfalls. Curr Rev Musculoskelet Med 2016;9:75-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Dimitriou D, Liow MH, Tsai TY, et al. Early outcomes of revision surgery for taper corrosion of dual taper total hip arthroplasty in 187 patients. J Arthroplasty 2016;31:1549-1554. [DOI] [PubMed] [Google Scholar]
- 18. Langton DJ, Jameson SS, Joyce TJ, et al. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: a consequence of excess wear. J Bone Joint Surg [Br] 2010;92-B:38-46. [DOI] [PubMed] [Google Scholar]
- 19. Dripps RD, Lamont A, Eckenhoff JE. The role of anesthesia in surgical mortality. JAMA 1961;178:261–266. [DOI] [PubMed] [Google Scholar]
- 20. Abdel MP, Houdek MT, Watts CD, Lewallen DG, Berry DJ. Epidemiology of periprosthetic femoral fractures in 5417 revision total hip arthroplasties: a 40-year experience. Bone Joint J 2016;98-B:468-474. [DOI] [PubMed] [Google Scholar]
- 21. Kwon YM, Antoci V, Jr, Eisemon E, et al. “Top-out” removal of well-fixed dual-taper femoral stems: surgical technique and radiographic risk factors. J Arthroplasty 2016;31:2843-2849. [DOI] [PubMed] [Google Scholar]
- 22. Hunt LP, Ben-Shlomo Y, Clark EM, et al. 90-day mortality after 409,096 total hip replacements for osteoarthritis, from the National Joint Registry for England and Wales: a retrospective analysis. Lancet 2013;382:1097-1104. [DOI] [PubMed] [Google Scholar]
- 23. Sabah SA, Henckel J, Cook E, et al. Validation of primary metal-on-metal hip arthroplasties on the National Joint Registry for England, Wales and Northern Ireland using data from the London Implant Retrieval Centre: a study using the NJR dataset. Bone Joint J 2015;97-B:10-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sabah SA, Henckel J, Koutsouris S, et al. Are all metal-on-metal hip revision operations contributing to the National Joint Registry implant survival curves?: a study comparing the London Implant Retrieval Centre and National Joint Registry datasets. Bone Joint J 2016;98-B:33-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. De Smet KA, Van Der Straeten C, Van Orsouw M, et al. Revisions of metal-on-metal hip resurfacing: lessons learned and improved outcome. Orthop Clin North Am 2011;42:259-269. [DOI] [PubMed] [Google Scholar]
- 26. Matharu GS, Pynsent PB, Sumathi VP, et al. Predictors of time to revision and clinical outcomes following revision of metal-on-metal hip replacements for adverse reaction to metal debris. Bone Joint J 2014;96-B:1600-1609. [DOI] [PubMed] [Google Scholar]
- 27. Matharu GS, Judge A, Pandit HG, Murray DW. Which factors influence the rate of failure following metal-on-metal hip arthroplasty revision surgery performed for adverse reactions to metal debris? An analysis from the National Joint Registry for England and Wales. Bone Joint J 2017;99-B:1020-1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Munro JT, Masri BA, Garbuz DS, Duncan CP. Tapered fluted modular titanium stems in the management of Vancouver B2 and B3 peri-prosthetic fractures. Bone Joint J 2013;95-B(Suppl A):17-20. [DOI] [PubMed] [Google Scholar]
- 29. Konan S, Duncan CP, Masri BA, Garbuz DS. Porous tantalum uncemented acetabular components in revision total hip arthroplasty: a minimum ten-year clinical, radiological and quality of life outcome study. Bone Joint J 2016;98-B:767-771. [DOI] [PubMed] [Google Scholar]
- 30. Liddle AD, Satchithananda K, Henckel J, et al. Revision of metal-on-metal hip arthroplasty in a tertiary center: a prospective study of 39 hips with between 1 and 4 years of follow-up. Acta Orthop 2013;84:237-245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. de Steiger RN, Miller LN, Prosser GH, et al. Poor outcome of revised resurfacing hip arthroplasty. Acta Orthop 2010;81:72-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lainiala O, Reito A, Elo P, et al. Revision of metal-on-metal hip prostheses results in marked reduction of blood cobalt and chromium ion concentrations. Clin Orthop Relat Res 2015;473:2305-2313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Stryker LS, Odum SM, Fehring TK, Springer BD. Revisions of monoblock metal-on-metal THAs have high early complication rates. Clin Orthop Relat Res 2015;473:469-474. [DOI] [PMC free article] [PubMed] [Google Scholar]


