Abstract
Objectives
Plantar heel pain is common and can be severely disabling. Unfortunately, a gap in the literature exists regarding the optimal intervention for this painful condition. Consequently, a systematic review of the current literature regarding manual therapy for the treatment of plantar heel pain was performed.
Methods
A computer-assisted literature search for randomized controlled trials in MEDLINE, EMBASE, Cochrane, CINAHL, and Rehabilitation & Sports Medicine Source, was concluded on 7 January 2014. After identification of titles, three independent reviewers selected abstracts and then full-text articles for review.
Results
Eight articles were selected for the final review and underwent PEDro scale assessment for quality. Heterogeneity of the articles did not allow for quantitative analysis. Only two studies scored ≥7/10 on the PEDro scale and included joint, soft tissue, and neural mobilization techniques. These two studies showed statistically greater symptomatic and functional outcomes in the manual therapy group.
Discussion
This review suggests that manual therapy is effective in the treatment of plantar heel pain; however, further research is needed to validate these findings given the preponderance of low quality studies.
Keywords: Heel pain, Foot pain, Plantar fasciitis, Manual therapy
Background
Plantar heel pain is a common complaint of individuals seeking ambulatory care services. Pain in the plantar aspect of the heel may be associated with a number of diagnoses including, but not limited to, plantar fasciopathy, calcaneal stress fractures, fat pad atrophy, tarsal tunnel syndrome, neuromas and/or referred pain from the lumbar spine.1,2 Annually, roughly two million patients spend $284 million on the evaluation and treatment of plantar heel pain in the United States.3,4 Nearly 10% of the population will suffer from plantar heel pain at some time in their life.5
Due to the common nature of plantar heel pain, the risk factors have been well studied over the past decade. Recent literature has found associations between chronic plantar heel pain and limited ankle dorsiflexion, limited first metatarsophalangeal joint extension, increased age, increased weight in a non-athletic population and prolonged standing.6,7 Interestingly, joint mobility restrictions in the foot and ankle complex appear to largely influence the development of plantar fasciopathy, with the limited ankle dorsiflexion as the greatest risk factor identified in a matched case-control study.7 Biomechanically, excessive pronation may potentially be a compensatory response to a lack of ankle dorsiflexion,8 which theoretically could increase stress on the plantar fascia. These findings support evaluating and treating ankle mobility impairments in the management of plantar heel pain.9
Manual therapy is commonly used by physical therapists to improve joint mobility and decrease pain.10 Specific to the ankle complex, in participants status post lateral ankle sprains, manual therapy was shown to have positive effects on ankle dorsiflexion mobility and pain levels.11 Given the association between limited ankle dorsiflexion and plantar heel pain, it seems reasonable to utilize joint and soft tissue mobilization.
Although there appears to be a construct for the inclusion of manual therapy in the treatment of plantar heel pain, the current literature detailing the effects of manual therapy primarily for plantar heel pain is sparse. More commonly used conservative interventions for plantar heel pain may include physical therapy, pharmaceutical interventions, such as nonsteroidal anti-inflammatory medications or injections, heel pads, orthotics, night splints and modalities, such as extra-corporeal shockwave therapy.12,13 To date, a systematic literature review describing the use of manual therapy interventions to manage plantar heel pain has not been performed. The purpose of this systematic review is to evaluate and synthesize the available evidence regarding the reported effects of manual therapy interventions in the treatment of plantar heel pain.
Methods
This systematic review was designed using the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses. The systematic review was conducted using a research question framed by PICOS methodology. The PICOS was as follows: Population (adults with plantar heel pain) Intervention (manual therapy), Comparison (standard care or control), Outcome (self-report outcome measures and/or physiological outcomes) and Study design (randomized control trials).
Identification of studies
A comprehensive and systematic literature search of MEDLINE, EMBASE, Cochrane, CINAHL and Rehabilitation & Sports Medicine Source databases was conducted by one author (JJM). Any randomized control trial that involved human participants and was published as a full text in English through July 2014 was included. The search terms (alone or in combination) included key words and MeSH terms and were: ‘heel’, ‘plantar’, ‘foot’, ‘pain’, ‘manual therapy’, ‘musculoskeletal manipulations’, ‘mobilization’, ‘manipulation’, ‘myofascial’, ‘physical therapy’, ‘conservative treatment’ and ‘humans’, The medline search was performed as follows: ((((manual therapy OR mobilization OR physical therapy OR conservative treatment OR manipulation OR myofascial) AND (heel pain OR plantar OR foot)) AND (Humans[Mesh])) OR ((pain[MeSH Terms]) AND ((musculoskeletal manipulations[MeSH Terms]) AND foot[MeSH Terms] AND (Humans[Mesh])) AND (Humans[Mesh]))). Articles that did not demonstrate any identifiable manual technique, or addressed other foot or ankle diagnoses not specific to heel pain, were not included in this systematic review. A manual technique was identified as an intervention in which the therapist used their hands to perform the treatment. This included soft tissue mobilization, myofascial release, trigger point release, joint mobilization/manipulation, manual stretching and strain–counterstrain. Articles detailing the use of trigger point dry needling as the only form of ‘manual therapy’ were excluded.
Selection of studies
Three authors independently screened the titles for eligibility using the criteria determined a priori (JJM, AEK, DJJ). After the preliminary search of the above databases, any title that included manual therapy in the intervention of plantar heel pain was included for further analysis. Amongst those articles in which disagreement occurred (six articles), the final decision was made by the primary author. Based on the title selection process, abstracts meeting the above inclusion criteria were obtained. The same three authors reviewed the abstracts and a final consensus was made to obtain the full article to be included in this systematic review.
Quality assessment of studies
Three reviewers independently assessed the quality of studies using the PEDro scale.14 As the PEDro scale delineates, one point was assigned whenever the criterion was clearly described in the article. Any disagreement was resolved by consensus discussion.
Results
Selection of Studies
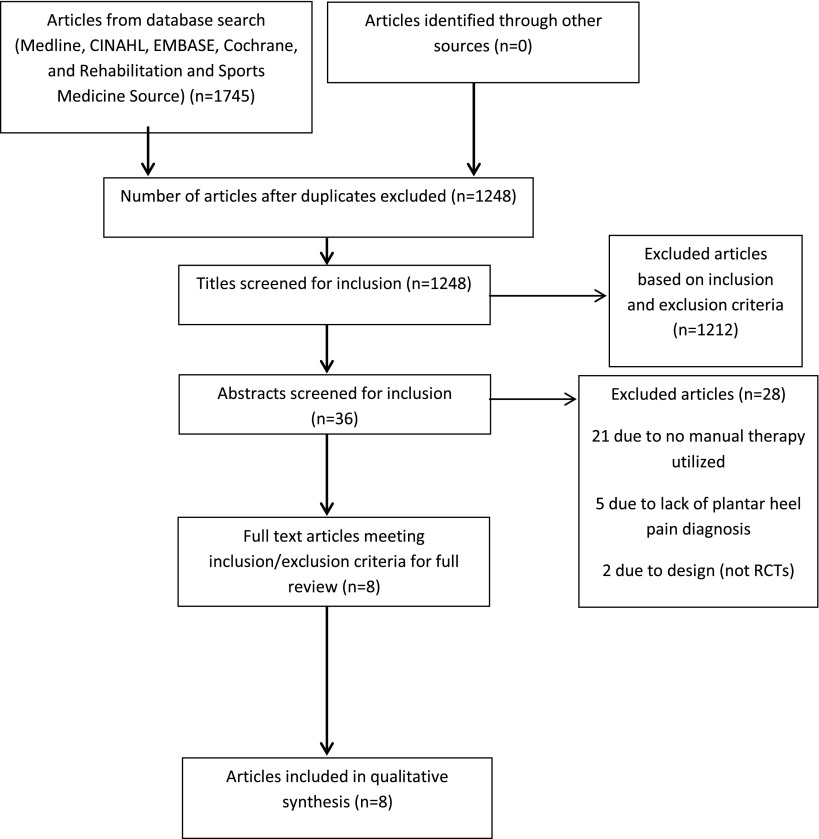
One thousand seven hundred and forty-five articles were identified through database and reference searches. Once duplicates were removed, 1,248 titles remained for assessment of eligibility. Of these, 36 abstracts were chosen to assess for eligibility and, of these, 8 were chosen for the final assessment of full texts (Fig. 1). Due to the heterogeneity of the studies, a quantitative analysis could not be performed. The results of the analysis were dichotomized into the short-term effects of manual therapy (less than or equal to four weeks) and the longer term effects of manual therapy (greater than four weeks on plantar heel pain).
Figure 1.
Flow chart of study selection.
Quality assessment
The PEDro scoring of the articles range between 3–8/10 and is shown in Table 1. The primary limitations on the PEDro scale were allocation concealment (2/8 studies awarded one point), blinding of subjects (2/8 studies awarded one point), blinding of therapists (0/8 studies awarded one point) and obtaining outcomes on more than 85% originally allocated to group assignment (3/8 studies awarded one point). Please refer to Table 2 for a complete summary of study characteristics.
Table 1.
PEDro Scale14
| Pedro | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ajimsha et al.19 | + | + | − | − | + | − | + | + | − | + | + | 6/10 |
| Cleland et al.21 | + | + | + | + | − | − | + | + | + | + | + | 8/10 |
| Dimou et al.20 | + | + | − | + | − | − | + | + | + | + | − | 6/10 |
| Kuhar et al.16 | + | + | − | + | − | − | − | − | − | + | + | 4/10 |
| Renan-Ordine et al.18 | + | + | − | + | − | − | + | − | − | + | + | 5/10 |
| Saban et al.22 | + | + | + | + | − | − | + | − | + | + | + | 7/10 |
| Wynne et al.15 | + | + | − | − | + | − | − | − | − | + | − | 3/10 |
| Yadav and Lakshmiprabha17 | + | − | − | + | − | − | − | − | − | + | + | 3/10 |
Notes: + = Criterion was satisfied; − = Criterion was not satisfied.
1 = Eligibility criteria specified.
2 = Subjects were randomly allocated in groups.
3 = Allocation was concealed.
4 = Groups were similar at baseline.
5 = Subjects were blinded.
6 = Therapists who administered the treatment were blinded.
7 = Assessors were blinded.
8 = Measures of key outcomes were obtained from more than 85% of subjects.
9 = Data were analysed by intention-to-treat.
10 = Statistical comparisons between groups were conducted.
11 = Point measures and measures of variability were provided.
Table 2.
Description of studies reviewed
| Patient characteristics | Interventions | Comparison | Outcome timeline | Outcome measures | |
|---|---|---|---|---|---|
| Ajimsha et al.19 | N = 65; experimental mean age = 42.4; sham US mean age = 40.8 | MFR vs. sham US | Control | Baseline; week 4; week 12 | 1. Function: FFI; 2. PPT |
| Cleland et al.21 | N = 60; experimental mean age = 49.5; exercise mean age = 47.4 | Electrophysical agents and exercise vs. manual therapy and exercise (impairment-based STM and joint mobilization) | Control | Baseline; week 4; 6 months | 1. Pain (NPRS); 2. Function: LEFS, FAAM, GROC |
| Dimou et al.20 | N = 20; experimental mean age = 42.1; orthotic mean age = 40.6 | Chiropractic adjustment and calf stretching vs. custom orthotics | Between group | Baseline, visit 4, visit 9, 1 month follow up | 1. Pain; 2: PPT; 3. Self-reported disability with various tasks |
| Kuhar et al.16 | N = 30; experimental mean age = 42.46; conventional therapy mean age = 43.73 | Conventional therapy vs. conventional therapy + MFR | Between group | Baseline; 10 days | 1. Pain (VAS); 2. Function: FFI |
| Renan-Ordine et al.18 | N = 60; experimental mean age = 44; stretching mean age = 45 | STM + self-stretching vs. self-stretching | Control | Baseline; 1 month | 1. Function: SF-36; 2. PPT |
| Saban et al.22 | N = 69; experimental mean age = 54; ultrasound mean age = 52 | STM, neural mobilization and self-stretching vs. US and self-stretching | Between group | Baseline; 6 weeks | 1. Pain (VAS); 2) Function: Foot & Ankle CAT |
| Wynne et al.15 | N = 19; mean age unknown | Counterstrain vs. placebo pill | Crossover design, 2–4 week washout | Baseline; 3 weeks | 1. Function: PDQ; 2. Stretch reflex; 3. H-reflex |
| Yadav and Lakshmiprabha17 | N = 60; experimental mean age = 40.13; standard care mean age = 42.7 | MFR + standard of care vs. pulsed US + standard of care | Between group | Baseline; 10 days | 1. Pain (VAS); 2. Function: FFI |
Notes: CAT = Computerized Adaptive Test; FAAM = Foot and Ankle Ability Measure; FFI = Foot Function Index; GROC = Global Rating of Change; LEFS = Lower Extremity Functional Scale; MFR = myofascial release; NPRS = Numeric Pain Rating Scale; PDQ = Pain and Dysfunction Questionnaire; PPT = Pressure Pain Threshold; STM = soft tissue mobilization; US = Ultrasound; VAS = Visual Analog Scale.
Short-term effects of manual therapy (less than or equal to four weeks)
Four articles15–18 examined the short-term effects of manual therapy to treat patients with plantar heel pain. Interestingly, these were the articles that scored lower on the PEDro scale having all scored ≤5/10. Only one study15 used a placebo pill for the control group; the other studies16–18 included some form of conservative intervention.
Two studies16,17 examined the effectiveness of manual therapy intervention when compared to ultrasound, plantar intrinsic stretching and strengthening. Both of these studies used baseline and 10-day comparisons of the visual analog scale (VAS) and the foot and function index (FFI). While duration of the manual therapy intervention was 15 min in one study,16 it was not documented in the other.17 Both studies provided treatment for 10 consecutive days and both reported statistically significant differences in pre-test/post-test changes in VAS (p < 0.00116, p = 0.02317) and FFI (p = 0.02416, p = 0.0317) in the manual therapy + exercise group in comparison to ultrasound + exercise group.
A third study18 randomized 60 participants into 2 groups consisting of (1) stretching exercises for the plantar fascia, gastrocnemius and soleus and (2) the same self-stretching exercises along with trigger point pressure release and a neuromuscular release technique to the gastrocnemius. Though the duration of manual therapy was not included, all participants received their respective interventions four times weekly for four weeks. A significant group-by-time interaction was revealed for the physical function (p = 0.001) and bodily pain (p = 0.005) components of the Medical Outcomes Study 36-item Short Form Health Survey (SF-36) and for pressure pain threshold (PPT) (p < 0.001).
The final study15 examined the efficacy of counterstrain manual therapy vs. placebo in a crossover-designed study. Fifty per cent of the 20 participants received a pragmatically designed manual therapy intervention while the other half received a placebo pill. After three weeks of treatment and a two- to four-week washout period, the groups received the opposite intervention. The H-reflex and stretch reflex of the calf muscles were monitored and the participants completed subjective outcome measures. No significant changes in electrically recorded reflexes were noted between the groups, though the participants reported decreased pain over 48 h after manual therapy intervention (p < 0.05).
Long-term effects of manual therapy (greater than four weeks)
The remaining four articles19–22 examined the effects of manual therapy in patients with plantar heel pain with follow-up greater than four weeks. These articles all scored ≥6/10 on the PEDro scale, with the two highest scoring studies on the PEDro scale done by Cleland and colleagues21 and Saban et al.22 (Table 1).
Ajimsha et al.19 examined the effects of myofascial release to the gastrocnemius, soleus and plantar fascia, as compared to sham ultrasound over the gastrocnemius, soleus and plantar fascia. The authors reported statistically significant differences on the FFI between the two groups at week four (p < 0.001) and week twelve (p < 0.001). These authors also found decrease in pain, as measured by the FFI pain subscale, in the myofascial release group vs. the control group at week four and week twelve.
Dimou and colleagues20 randomized 20 participants into 2 groups: (1) chiropractic manipulation/Achilles stretching and (2) custom orthotics. The participants in the intervention group received manipulations to the ankle and foot twice per week for four weeks and again at one-month follow-up, in addition to daily gastrocnemius and soleus stretching 10 times for the entire eight-week period. Although PPT improvement was observed in both groups, there was not a statistically significant difference observed. In addition, no statistically significant differences were found on other self-reported aspects of resting heel pain, heel pain with the first few steps in the morning and heel pain with leisure.
Saban et al.22 randomized 69 patients into 2 groups comparing ultrasound and triceps surae stretching exercises (n = 33) to deep massage, neural mobilizations and the same stretching exercises (n = 36). The Foot and Ankle Computerized Adaptive Test (FACAT) was used. Although improvements were found in both groups over a six-week period, the manual therapy + stretching group improved significantly more (p < 0.05) than the ultrasound + stretching group. The effect size, as calculated by Cohen’s d, of 0.6 is considered medium.
Cleland and colleagues21 randomized 60 participants into 2 groups: (1) ultrasound, dexamethasone and therapeutic exercise, (2) manual therapy (aggressive soft tissue mobilization to the triceps surae and plantar fascia insertion followed by rearfoot eversion mobilization) and therapeutic exercise. Patients in both groups were treated two times per week for two weeks, followed by one time per week for two weeks for a total of six visits. Between group differences demonstrated significant improvement for the manual therapy + exercise group at both the four-week and six-month follow-ups per the Foot and Ankle Ability Measure (FAAM) (p = 0.004, p = 0.012, respectively) and Lower Extremity Functional Scale (LEFS) (p = 0.001, p = 0.027, respectively). The six-month effect sizes, using Cohen’s d, were calculated to be medium (0.6 for the LEFS and 0.7 for the FAAM). The manual therapy + exercise group showed statistically significant improvement on the Numeric Pain Rating Scale (NPRS) at the four-week follow-up (p = 0.008), but not at the six-month follow-up (P = 0.39). The six-month effect size for the NPRS was calculated to be small (−0.2).
Outcome Measures: Psychometric Properties
Given the heterogeneity of the studies, there was a large degree of variability of outcome measurement tools used to assess pain and function. This is of concern when a reader is trying to critically analyse the validity of a study’s findings. The following places the current findings of the specific outcome tool’s psychometric properties in context.
In order to properly interpret this section, several terms must first be defined. Jaeschke et al.23 originally defined minimal clinically important difference (MCID) as ‘the smallest difference in score in the domain of interest which patients perceive as beneficial and which would mandate, in the absence of troublesome side effects and excessive cost, a change in patient’s management’. This definition has since been simplified to ‘the smallest change that is important to patients’.24 The terminology, minimal important difference (MID), is synonymous with MCID and is also used in a number of the studies. Minimal detectable change (MDC) is defined as the smallest amount of change that likely reflects true change rather than measurement error inherent in the score.25
Foot function index
The FFI was utilized in three studies.16,17,19 Originally developed for patients with rheumatoid arthritis,26 it is frequently used in research for a variety of foot conditions and treatments.27 The FFI is reported to have moderate-to-high correlation with the SF-36,28 and demonstrates excellent reliability.27 The MID is 6.5 points [CI: −13.1 to 0.1] in patients with plantar fasciitis.29 All studies included in this systematic review, using the FFI,16,17,19 demonstrated greater than MID change in the FFI in their experimental groups that exceeded the change in the comparison group; however, both control groups from the Kuhar et al.16 and Yadav and Lakshmiprabha17 studies also demonstrated results that exceeded the MID.
SF-36
The SF-36 has not been studied specifically in patients with foot or ankle disorders; however, it does correlate to the FFI.28 In patients with lower extremity osteoarthritis, the MCID is reported as 7.8 points for the bodily pain and 3.3 points for the physical function subscales.30 The one study18 that used the SF-36 demonstrated findings meeting the MCID for these subscales.
Pressure pain thresholds
PPTs have been purported to quantify tissue hyperalgesia and can be used to clinically identify signs of central sensitization. The normative data for the plantar aspect of the heel are not known. Saggini et al.31 found, in a group of control participants, PPT values at the medial calcaneal tubercle were ~7.5 kilograms of force (kgf). Neither Renan-Ordine et al.18 nor Ajimsha et al.19 assessed PPTs on the plantar aspect of the heel, but rather at the posterior calcaneus. Therefore, the interpretations of the true measure of the magnitude of change after manual therapy on plantar heel pain in these studies are limited.
Visual analogue and numeric pain rating scales
The VAS is established as a valid measure of subjective pain, correlates well to other measures of pain (numeric rating scale, faces pain scale), and is highly sensitive to change.32 The VAS demonstrates a MID of −8 mm [95% CI: −12 to −4] in heel pain.33 Kuhar et al.16 Yadav and Lakshmiprabha,17 and Saban et al.22 all demonstrated changes exceeding the MID in both their experimental and control groups.
With regard to the NPRS, a change of two points out of ten has been suggested as clinically meaningful in patients with chronic pain;34 however, its responsiveness in plantar heel pain is not explicitly established. Though Cleland et al.21 reported that both groups exceeded the MCID for the NPRS at six months, only the group receiving manual therapy met the MCID at four weeks. Both groups in the study done by Dimou et al.20 had statistically significant reductions in pain on the NPRS; however, the lack of a true control group may cloud their results.
Foot and ankle ability measure
The FAAM, utilized in one study,21 has a reported MDC and a MCID of 5.7 and 8 out of 84 points and 12.3 and 9 out of 32 points for the activities of daily living (ADL) and sports subscales, respectively.35 Initial validation of this tool included patients with plantar fasciitis, and patients with either chronic or acute plantar heel pain report similar levels of ability on both the ADL and sports subscales.36 While only utilizing the ADL subscale, Cleland et al.21 demonstrated greater than MCID changes in both groups at four-week and six-month follow-up.
Lower extremity functional scale
The LEFS, utilized in one study,21 demonstrates high reliability, validity and sensitivity to change for a variety of lower extremity conditions. While never studied specifically for heel pain; its general MDC and MCID were reported initially to be nine points (out of the best possible 80 points), though Wang et al.37 found it varied considerably based on age, chronicity and severity. As it is specific to the lower extremity, it has been purported to be more sensitive to change than the SF-36 in lower extremity conditions.38 In this systematic review, the results from Cleland et al.21 met the nine point MCID in only the group receiving manual therapy at four weeks; however, both groups exceeded the nine point MCID by the six-month follow-up.
Foot and ankle computerized adaptive test
The FACAT, utilized in one study,22 is a computer administered self-report outcome measure based on the items of the LEFS that were identified to be most indicative of foot and ankle function. The patient continues to answer the computer generated questions until a stopping rule is satisfied and an estimate of function is established.39 With a reported MDC of 6.9 points and a minimally clinically important improvement of 8 points,40 Saban et al.22 demonstrated improvements of 15 points [95% CI: 9–21 points] in the group receiving manual therapy indicating meaningful functional results.
Discussion
The results of this systematic review demonstrate that manual therapy may be effective in treating patients with plantar heel pain. Not surprisingly, this is in concordance with the updated version of the clinical practice guidelines for heel pain.12 The dosing of the manual therapy remains unclear as the studies that did report effectiveness were pragmatically designed.
Of note, only two of the studies21,22 scored ≥7/10 on the PEDro scale, while the other studies selected for the full review were of lesser quality. Of the studies selected, Cleland and colleagues21 had the highest quality study and found superior results in the manual therapy group with validated outcome measures (NPRS in the short term, FAAM, LEFS in the long term) that did meet the MCID. Their experimental group received a multimodal approach (soft tissue mobilization to the triceps surae and plantar fascia and a rearfoot eversion mobilization) and impairment-based manual therapy to the hip, knee and ankle. This is similar to the study design used by Saban et al.22 where the intervention group received neural mobilizations, deep tissue massage and stretching exercises. While these treatment approaches may simulate a pragmatic clinical scenario for intervention selection, they do not allow for extrapolation of the influence of manual therapy treatment technique alone or for identification of the most advantageous technique.
The lack of high quality studies is compounded by the variety and quality of outcome measures selected. For example, the SF-36, while widely used as an indicator of general health, is not specific to the foot and ankle. Renan-Ordine et al.18 used the SF-36 in conjunction with PPT, which may not have captured all the constructs of plantar heel pain.
Specific to improvement in pain, there were a variety of measures used, including the FFI pain subscale, NPRS and VAS. The FFI has been validated and determined to be reliable for patients with non-traumatic foot and ankle problems.41 The NPRS and VAS are well documented for their reliability42,43 and validity for a variety of patient populations.43–45
The FFI, FAAM, LEFS and FACAT all measure function of the foot and ankle to some extent; and, while their specific validity to the diagnostic category of ‘plantar heel pain’ has not been established, each of them has been validated in populations which included a portion of patients with a form of plantar heel pain (most commonly reported plantar fasciitis).29,35,38,39 The ability to compare efficacy is difficult given the diversity of the outcomes monitored and ethical considerations for withholding treatment. The effectiveness of pragmatically designed manual therapy demonstrated superior results in the long term.21,22
The results of this systematic review identify a significant gap in the literature regarding long-term outcomes of physical therapy treatment for plantar heel pain, and even-more-so regarding the long-term effectiveness of manual therapy in the treatment of plantar heel pain. Biomechanical, neurophysiological and psychological mechanisms have been proposed following the use of manual therapy.10 Based on these mechanisms, one would expect the short-term results observed. Unfortunately, due to the methodology and psychometric properties of the outcomes used, it is difficult to state that manual therapy was effective in the short term. Of the studies in this review, the study by Cleland et al.21 had the longest outcomes (six months), suggesting that manual therapy may be effective in the treatment of plantar heel pain in the long term. However, as the Cleland et al.21 study is the only study of high quality to assess long term (greater than three months) outcomes, more studies of higher quality are needed to validate these data. Of note, the PEDro scale involves categories based on the presence of blinding. In manual therapy, blinding in interventional studies can be hard to achieve, making higher PEDro scores more difficult to obtain in these investigations.
Limitations
One limitation of this review is that internal reliability of the reviewers was not assessed on the scoring of the articles on the PEDro scale. Also, due to the heterogeneity of studies, the authors were unable to perform a quantitative analysis of the studies. A variety of outcome measures, some not validated for the plantar heel pain patient population, were used in the studies included in this systematic review, making the validity of treatment effectiveness difficult to determine. The longest follow-up of the articles chosen was six months, with the majority of studies selected for the review assessing the short-term effects of treatment. Therefore, specific recommendations detailing optimal manual therapy prescriptions cannot be made for individuals with plantar heel pain. However, practically speaking, variability within manual therapy prescription is likely to exist in clinical practice based on the degree of impairment and of the clinician’s philosophical treatment bias. Additionally, as only two studies15,19 used only manual therapy in the experimental group, the co-interventions undermine the ability to determine the effectiveness of manual therapy alone for individuals with plantar heel pain. Consequently, the results should be interpreted with caution for long-term improvements in patients with plantar heel pain.
Conclusion
There is recent evidence, including two well-designed studies, to suggest that manual therapy is effective in the long term in the treatment of plantar heel pain. Only two studies21,22 scored ≥7/10 on the PEDro scale and included joint, soft tissue and neural mobilization techniques. These two studies showed statistically greater symptomatic and functional outcomes in the manual therapy group. Results for short-term effects are difficult to interpret given limitations in several studies’ designs. Further research is needed to validate these claims given the preponderance of low quality studies.
Conflict of interest
The authors report no conflicts-of-interest.
References
- 1.Alvarez-Nemegyei J, Canoso JJ. Heel pain: diagnosis and treatment, step by step. Cleveland Clin J Med. 2006;73(5):465–71. 10.3949/ccjm.73.5.465 [DOI] [PubMed] [Google Scholar]
- 2.Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med. 2004;350(21):2159–66. 10.1056/NEJMcp032745 [DOI] [PubMed] [Google Scholar]
- 3.Pfeffer G, Bacchetti P, Deland J, Lewis A, Anderson R, Davis W, et al. Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis. Foot Ankle Int. 1999;20(4):214–21. 10.1177/107110079902000402 [DOI] [PubMed] [Google Scholar]
- 4.Tong KB, Furia J. Economic burden of plantar fasciitis treatment in the United States. Am J Orthop (Belle Mead NJ). 2010;39(5):227–31. [PubMed] [Google Scholar]
- 5.Crawford F, Atkins D, Edwards J. Interventions for treating plantar heel pain. Cochrane Database Syst Rev. 2000;3(3):CD000416. [DOI] [PubMed] [Google Scholar]
- 6.Irving DB, Cook JL, Menz HB. Factors associated with chronic plantar heel pain: a systematic review. J Sci Med Sport. 2006;9(1-2):11–22; discussion 23-4. 10.1016/j.jsams.2006.02.004 [DOI] [PubMed] [Google Scholar]
- 7.Riddle DL, Pulisic M, Pidcoe P, Johnson RE. Risk factors for Plantar fasciitis: a matched case-control study. J Bone Joint Surg Am. 2003;85-A(5):872–7. [DOI] [PubMed] [Google Scholar]
- 8.Cornwall MW, McPoil TG. Effect of ankle dorsiflexion range of motion on rearfoot motion during walking. J Am Podiatr Med Assoc. 1999;89(6):272–7. 10.7547/87507315-89-6-272 [DOI] [PubMed] [Google Scholar]
- 9.Kwong PK, Kay D, Voner RT, White MW. Plantar fasciitis. Mechanics and pathomechanics of treatment. Clin Sports Med. 1988;7(1):119–26. [PubMed] [Google Scholar]
- 10.Bialosky JE, Bishop MD, Price DD, Robinson ME, George SZ. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531–538. 10.1016/j.math.2008.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loudon JK, Reiman MP, Sylvain J. The efficacy of manual joint mobilisation/manipulation in treatment of lateral ankle sprains: a systematic review. Br J Sports Med. 2014;48(5):365–70. 10.1136/bjsports-2013-092763 [DOI] [PubMed] [Google Scholar]
- 12.Martin RL, Davenport TE, Reischl SF, McPoil TG, Matheson JW, Wukich DK, et al. Heel pain – plantar fasciitis: revision 2014. J Orthop Sports Phys Ther. 2014;44(11):A1–A33. 10.2519/jospt.2014.0303 [DOI] [PubMed] [Google Scholar]
- 13.Rosenbaum AJ, DiPreta JA, Misener D. Plantar heel pain. Med Clin North Am. 2014;98(2):339–52. 10.1016/j.mcna.2013.10.009 [DOI] [PubMed] [Google Scholar]
- 14.Physiotherapy Evidence Database. Pedro Scale. [Document on the Internet] The George Institute for Global Health; 2015. [updated 2015 Apr 8; cited 2015 Apr 12]. Available from: http://www.pedro.org.au/english/downloads/pedro-scale
- 15.Wynne MM, Burns JM, Eland DC, Conatser RR, Howell JN. Effect of counterstrain on stretch reflexes, hoffmann reflexes, and clinical outcomes in subjects with plantar fasciitis. J Am Osteopath Assoc. 2006;106(9):547–56. [PubMed] [Google Scholar]
- 16.Kuhar S, Subhash K, Chitra J. Effectiveness of myofascial release in treatment of plantar fasciitis: a RCT. Indian J Physiother Occup Ther. 2007;1(3):3–9. [Google Scholar]
- 17.Yadav AO, Lakshmiprabha R. Comparison of the effects of therapeutic ultrasound v/s myofascial release technique in treatment of plantar fasciitis. Indian J Physiother Occup Ther. 2012;6:13–6. [Google Scholar]
- 18.Renan-Ordine R, Alburquerque-SendÍn F, Rodrigues De Souza DP, Cleland JA, Fernández-de-las-PeÑas C. Effectiveness of myofascial trigger point manual therapy combined with a self-stretching protocol for the management of plantar heel pain: a randomized controlled trial. J Orthop Sports Phys Ther. 2011;41(2):43–50. 10.2519/jospt.2011.3504 [DOI] [PubMed] [Google Scholar]
- 19.Ajimsha MS, Binsu D, Chithra S. Effectiveness of myofascial release in the management of plantar heel pain: a randomized controlled trial. Foot. 2014;24(2):66–71. 10.1016/j.foot.2014.03.005 [DOI] [PubMed] [Google Scholar]
- 20.Dimou ES, Brantingham JW, Wood T. A randomized, controlled trial (with blinded observer) of chiropractic manipulation and Achilles stretching vs. orthotics for the treatment of plantar fasciitis. JACA J Am Chiropract Assoc. 2004;41(9):32–42. [Google Scholar]
- 21.Cleland JA, Abbott JH, Kidd MO, Stockwell S, Cheney S, Gerrard DF, et al. Manual physical therapy and exercise versus electrophysical agents and exercise in the management of plantar heel pain: a multicenter randomized clinical trial. J Orthop Sports Phys Ther. 2009;39(8):573–585. 10.2519/jospt.2009.3036 [DOI] [PubMed] [Google Scholar]
- 22.Saban B, Deutscher D, Ziv T. Deep massage to posterior calf muscles in combination with neural mobilization exercises as a treatment for heel pain: a pilot randomized clinical trial. Man Ther. 2014;19(2):102–108. 10.1016/j.math.2013.08.001 [DOI] [PubMed] [Google Scholar]
- 23.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989;10(4):407–15. 10.1016/0197-2456(89)90005-6 [DOI] [PubMed] [Google Scholar]
- 24.Stratford PW, Binkley JM, Riddle DL, Guyatt GH. Sensitivity to change of the Roland-Morris back pain questionnaire: part 1. Phys Ther. 1998;78(11):1186–96. [DOI] [PubMed] [Google Scholar]
- 25.Portney LG, Watkins MP. Foundations of clinical research: applications to practice, 3rd edn Upper Saddle River, NJ: Pearson/Prentice Hall; 2009. [Google Scholar]
- 26.Budiman-Mak E, Conrad kJ, Roach KE. The foot function index: a measure of foot pain and disability. J Clin Epidemiol. 1991;44(6):561–70. 10.1016/0895-4356(91)90220-4 [DOI] [PubMed] [Google Scholar]
- 27.Budiman-Mak E, Conrad kJ, Mazza J, Stuck RM. A review of the foot function index and the foot function index – revised. J Foot Ankle Res. 2013;6(1):5-1146-6-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.SooHoo NF, Vyas R, Samimi D. Responsiveness of the foot function index, AOFAS clinical rating systems, and SF-36 after foot and ankle surgery. Foot Ankle Int. 2006;27(11):930–934. [DOI] [PubMed] [Google Scholar]
- 29.Landorf KB, Radford JA. Minimal important difference: values for the foot health status questionnaire, foot function index and visual analogue scale. Foot. 2008;18(1):15–9. 10.1016/j.foot.2007.06.006 [DOI] [Google Scholar]
- 30.Angst F, Aeschlimann A, Stucki G. Smallest detectable and minimal clinically important differences of rehabilitation intervention with their implications for required sample sizes using WOMAC and SF-36 quality of life measurement instruments in patients with osteoarthritis of the lower extremities. Arthritis Rheum. 2001;45(4):384–391. 10.1002/(ISSN)1529-0131 [DOI] [PubMed] [Google Scholar]
- 31.Saggini R, Bellomo RG, Affaitati G, Lapenna D, Giamberardino MA. Sensory and biomechanical characterization of two painful syndromes in the heel. J Pain. 2007;8(3):215–222. 10.1016/j.jpain.2006.07.002 [DOI] [PubMed] [Google Scholar]
- 32.Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain. 2011;152(10):2399–2404. 10.1016/j.pain.2011.07.005 [DOI] [PubMed] [Google Scholar]
- 33.Landorf KB, Radford JA, Hudson S. Minimal important difference (MID) of two commonly used outcome measures for foot problems. J Foot Ankle Res. 2010;3:7-1146-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole MR. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain. 2001;94(2):149–58. 10.1016/S0304-3959(01)00349-9 [DOI] [PubMed] [Google Scholar]
- 35.Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the foot and ankle ability measure (FAAM). Foot Ankle Int. 2005;26(11):968–83. [DOI] [PubMed] [Google Scholar]
- 36.Klein SE, Dale AM, Hayes MH, Johnson JE, McCormick JJ, Racette BA. Clinical presentation and self-reported patterns of pain and function in patients with plantar heel pain. Foot Ankle Int. 2012;33(9):693–698. 10.3113/FAI.2012.0693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang YC, Hart DL, Stratford PW, Mioduski JE. Clinical interpretation of a lower-extremity functional scale-derived computerized adaptive test. Phys Ther. 2009;89(9):957–68. 10.2522/ptj.20080359 [DOI] [PubMed] [Google Scholar]
- 38.Binkley JM, Stratford PW, Lott SA, Riddle DL. The lower extremity functional scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999;79(4):371–383. [PubMed] [Google Scholar]
- 39.Hart DL, Mioduski JE, Stratford PW. Simulated computerized adaptive tests for measuring functional status were efficient with good discriminant validity in patients with hip, knee, or foot/ankle impairments. J Clin Epidemiol. 2005;58(6):629–38. 10.1016/j.jclinepi.2004.12.004 [DOI] [PubMed] [Google Scholar]
- 40.Hart DL, Wang YC, Stratford PW, Mioduski JE. Computerized adaptive test for patients with foot or ankle impairments produced valid and responsive measures of function. Qual Life Res. 2008;17(8):1081–91. 10.1007/s11136-008-9381-y [DOI] [PubMed] [Google Scholar]
- 41.Martin RL, Irrgang JJ. A survey of self-reported outcome instruments for the foot and ankle. J Orthop Sports Phys Ther. 2007;37:72–84. 10.2519/jospt.2007.2403 [DOI] [PubMed] [Google Scholar]
- 42.Ferraz MB, Quaresma MR, Aquino LR, Atra E, Tugwell P, Goldsmith CH. Reliability of pain scales in the assessment of literate and illiterate patients with rheumatoid arthritis. J Rheumatol. 1990;17(8):1022–4. [PubMed] [Google Scholar]
- 43.Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011;63(Suppl 11):S240–S252. 10.1002/acr.v63.11s [DOI] [PubMed] [Google Scholar]
- 44.Downie WW, Leatham PA, Rhind VM, Wright V, Branco JA, Anderson JA. Studies with pain rating scales. Ann Rheum Dis. 1978;37(4):378–381. 10.1136/ard.37.4.378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Price DD, McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain. 1983;17(1):45–56. 10.1016/0304-3959(83)90126-4 [DOI] [PubMed] [Google Scholar]