Abstract
Background:
The aim of this study was survey of the effect of Vitamin D supplementation on the incidence of gestational diabetes (GDM) in pregnant women.
Materials and Methods:
This randomized clinical trial was conducted at Alzahra and Shahid Beheshti Hospital in Isfahan, Iran, from January, 2013 to January, 2014 on 210 pregnant women referred to gynecology clinics. Serum levels of Vitamin D were measured, and those with lower serum levels of 10 nmol/L randomly divided into two groups of A and B. Pregnant women with normal Vitamin D level assigned as Group C. Group A was given 50,000 IU Vitamin D supplement every 2 weeks for 10 weeks, and Group B were given the omega-3 pearl as placebo. Then, the incidence of GDM was measured in 24–26 weeks of pregnancy with glucose tolerance test and compared in three groups. Data were analyzed using SPSS version 20 by descriptive statistics, Chi-square and Logistic regression.
Results:
The mean age of participants was 24.76 years (8.02 standard deviation, range 16–36 years). The incidence of GDM at 24–26 weeks gestational age were 8.57% in normal Vitamin D group, 10.00% in Vitamin D deficiency with treatment group, and 11.43% in Vitamin D deficiency without treatment group. The difference between groups in terms of incidence of GDM was not statistically significant (P = 0.112).
Conclusion:
Vitamin D supplementation had not effect on incidence of GDM during pregnancy.
Keywords: Gestational diabetes mellitus, Vitamin D deficiency, Vitamin D insufficiency, Vitamin D supplement
Introduction
Vitamin D deficiency may be a common health problem worldwide both in children and adults.[1] Vitamin D insufficiency is characterized by 25-hydroxyvitamin D (25(OH)D) concentration <75 nmol/L (or 30 ng/mL).[2] Low concentrations of Vitamin D have been found in all age groups in various countries including in the Middle East.[3] It has been estimated that about 40–100% of elderly men and women living in the United States and Europe are deficient in Vitamin D.[3] Vitamin D plays an important role in glucose metabolism and insulin, and it may improve insulin secretion by the effect on receptors of Vitamin D in the pancreatic islet cells. However, the increase in parathyroid hormone in Vitamin D deficiency reduces insulin sensitivity of cells. Moreover, Vitamin D has anti-inflammatory and immune modulating effects and reduces insulin resistance and increased insulin secretion through modulation of the immune system.[4,5] Vitamin D deficiency is associated with an increased risk of diabetes and metabolic syndrome and insulin resistance.[6,7]
In pregnancy, Vitamin D deficiency and Vitamin D insufficiency are also thought to be common. A study in dark- and light-skinned pregnant women residing in the Northern United States found that approximately 29% of dark-skinned pregnant women and 5% of light-skinned pregnant women had Vitamin D deficiency, whereas 54% of dark-skinned participants and 47% of light-skinned participants had Vitamin D insufficiency.[8] Similar results have been found in Iranian pregnant women.[9] Differences in latitude have also been shown to influence the concentration of Vitamin D in a majority of pregnant women.[10]
On the other hand, pregnancy is characterized by insulin resistance and hyperinsulinemia. Thus, it may predispose some women to develop diabetes. The resistance stems from the placental secretion of diabetogenic hormones including growth hormone, corticotropin-releasing hormone, placental lactogen, and progesterone, as well as increased maternal adipose deposition, decreased exercise, and increased caloric intake. Gestational diabetes occurs when the pancreatic function is not sufficient to overcome the insulin resistance created by changes in diabetogenic hormones during pregnancy.[11]
Vitamin D deficiency can be associated with gestational diabetes mellitus (GDM) and insulin tolerance. Results of two systematic reviews showed that Vitamin D deficiency is associated with a higher risk of GDM and concluded that Vitamin D administration can improve insulin sensitivity and glucose tolerance.[12]
Vitamin D deficiency is still a serious health problem in pregnant women in Iran, despite Iran being located in a sunny region, pregnant women, and their infants are faced to the risk of Vitamin D deficiency, especially among the low socioeconomic status of Iranian population.
The aim of this study was survey of the effect of Vitamin D supplementation on the incidence of gestational diabetes in pregnant women referred to gynecology clinics in Isfahan University of Medical Sciences.
Materials and Methods
This study was a randomized clinical trial study with Iranian registry of clinical trials code of IRCT201309277513N4, which was carried out on pregnant women referred to obstetric clinics of Alzahra Hospital and Shahid Beheshti Hospital in Isfahan, Iran. The study was conducted from January 2013 for 1 year serum levels of Vitamin D were measured for the participants at the age of 14–16 weeks of pregnancy and those with lower serum levels of 10 nmol/L were randomly divided into two groups of A and B using random table. Pregnant women with normal Vitamin D level assigned as Group C. In the table of random numbers for each participant in the study were given a random number and participants were randomly divided into two groups using these numbers. Researcher, the distributors of the drug and the patients, did not know which group was taken the Vitamin D or placebo. After completion of the study, using the label of drug boxes, it was found which patients received the drug and which the placebo. Placebo was omega-3 pearl with the same shape as Vitamin D pearls.
The pregnant women that referred to gynecology clinic were examined by a gynecologist. Eligible women were informed about the study and intervention, and informed consent was obtained from the participants.
Inclusion criteria were patients who are willing to participate in the study and signed informed consent, normal body mass index (BMI) that BMI was calculated by measuring height and weight, gestational age (GA) between 14 and 16 weeks that was based on the evaluation of the gynecologist (last menstrual period, or sonography or clinical examination), the absence of a history of Type 2 diabetes and gestational diabetes, and no family history of diabetes in first-degree relatives. Exclusion criteria were discourage patients from continuing to participate in the study, taking Vitamin D supplements incorrect, and unable to follow-up the patients.
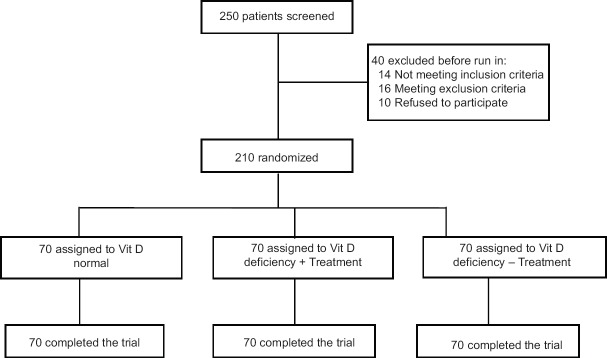
All participants were under glucose tolerance test (GTT), and they had positive GTT were also excluded from the study. GTT was performed in the morning, and the participants were instructed to fast (water is allowed) for 8–12 h before the test. At zero time (baseline), blood sample was drawn; then, the participants were given 75 g of glucose in solution to drink within a 5 min time frame. A diagnosis of gestational diabetes can be made in women who meet either of the following criteria: fasting plasma glucose ≥92 mg/dL, but <126 mg/dL at any GA (fasting plasma glucose ≥126 mg/dL is consistent with overt diabetes) and at 24–28 weeks of gestation: 75 g 2 h oral GTT with at least one abnormal result: fasting plasma glucose ≥92 mg/dL or 1 h >140 mg/dL or 2 h between 140 and 200 mg/dL.[13,14] Flow diagram of study shown in Figure 1.
Figure 1.
Flow diagram of the trial
Group A was given a Vitamin D supplement of Iranian Drug Corporation of Zahravi dose of 50,000 IU every 2 weeks for 10 weeks, and Group B was not given the supplement and was given placebo. From those participants with higher serum levels from 25 nmol/L (10 ng/mL) of 25(OH)D, normal individuals were selected randomly as control group (Group C with seventy pregnant women).
Given that Vitamin D deficiency has no effect on the outcome, and so far it has not been studied in a population of Iranian pregnant women, it is morally permissible do not treat pregnant women with Vitamin D deficiency according to the unproven efficacy of treatment in this group as it has not been treated. Participants who received Vitamin D had not reported any complications and continued the study to the end.
At the end of the study at 24–26 weeks of pregnancy, oral GTT was performed for the three groups and compared the incidence of gestational diabetes (glucose intolerance that occurs during pregnancy) in these groups together, and the effect of Vitamin D supplementation was concluded. GTT was performed in the following way: blood glucose was measured at baseline, and then participants were given a 75 g oral glucose and measurement of blood glucose levels 1 and 2 h later was done. Normal result for the glucose screening test was fasting blood sugar between 100 and 120 mg/dL. if 1 h after drinking, the glucose solution equal to or <140 mg/dL or blood glucose after 2 h was between 140 and 200 it was considered to be impaired GTT, and two impaired oral GTTs were considered as positive test.[13,14] Gestational diabetes subjects were diagnosed at 24–26 weeks and taken the standard treatment.
Data were analyzed using the Statistical Package for the Social Sciences version 20.0 (SPSS Inc., Chicago, IL, USA). Chi-square test was used for comparison difference between groups and logistic regression was used to predict the effect of variables related to gestational diabetes. P < 0.05 was considered statistically significant.
Results
At first, 250 participants entered the study. Forty of them excluded from the study: 14 due to not meeting inclusion criteria, 16 meeting exclusion, and 10 refused to participate. A total of 210 pregnant women were included in the study. The mean age of participants was 24.76 years (8.02 standard deviation, range 16–36 years). Patients divided into three groups in terms of Vitamin d deficiency and with or without take supplement. Three groups of patients were matched in term of age. The incidence rate of gestational diabetes was achieved through the percentage of patients with positive GTT.
The results of comparisons between the three groups (patients with normal Vitamin D, patients with Vitamin D deficiency that take supplement and patients with Vitamin D deficiency without treatment) in terms of percent of patients with positive GTT are shown in Table 1.
Table 1.
Comparisons between the three groups of patients in terms of the incidence of gestational diabetes
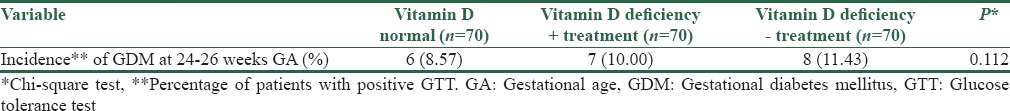
The results of this study showed that Vitamin D supplementation in pregnant women with low levels of Vitamin D cannot prevent the incidence of gestational diabetes.
The results of the prognostic value of Vitamin D level for gestational diabetes prediction are shown in Table 2.
Table 2.
Prognostic value of Vitamin D level for gestational diabetes prediction
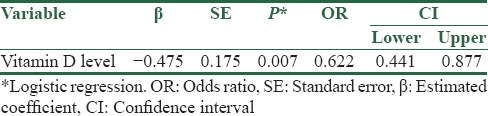
The prognostic value of Vitamin D level for gestational diabetes prediction was evaluated using regression analysis. Vitamin D deficiency was not a possible risk factor for gestational diabetes in pregnant women.
Discussion
The results of our study showed that Vitamin D supplementation in pregnant women with low levels of Vitamin D cannot prevent the incidence of gestational diabetes and due to the lack of a program for screening potential cases of Vitamin D deficiency, it is important to diagnosis Vitamin D deficiency and its complications in pregnancy prognosis.
Timms et al. have demonstrated in a study when used supplements of Vitamin D for patients with Vitamin D deficiency, the mean serum levels of fetal bovine serum significantly decreased after treatment.[15]
Some studies investigating the relationship between Vitamin D levels and GDM and have shown that Vitamin D supplements is associated with decrease risk of GDM, but have not declare Vitamin D supplements can be used in pregnant women or not. Three recent case–control studies from India, the UK and North Carolina aimed to determine whether early pregnancy 25(OH)D levels were associated with a later diagnosis of GDM.[16,17,18] Results were mixed. In one, women with GDM had 2.7 times the odds (confidence interval [CI] 1.0–7.0) of Vitamin D deficiency in the first trimester as those without.[16] The second showed no association between low Vitamin D levels and a GDM diagnosis but did find increased fasting glucose and hemoglobin a1c at 28 weeks.[17] The third found no association between diagnosis of GDM and first trimester Vitamin D deficiency but had very wide CIs.[18] None of the studies were adjusted for dietary factors or sun exposure.
Senti et al. in their review article surveyed the association of maternal Vitamin D deficiency and risk of GDM in the previous studies. Results of their review showed that the majority of studies reported an inverse relationship between circulating Vitamin D levels and markers of glucose homeostasis associated with gestational diabetes or an increased risk for GDM associated with reduced maternal levels of Vitamin D between 24 and 30 weeks of gestation. Results of their study also showed an association between higher Vitamin D levels and lower fasting glucose and insulin levels.[19]
Some societies consider it unnecessary, and others recommend up to 2000 UI/day. Yu et al. suggested that single oral dose of 200,000 IU Vitamin D, a daily supplement of 800 IU Vitamin D from 27 weeks until delivery improved 25(OH)D levels significantly. However, even with supplementation, only a small percentage of women and babies were Vitamin D sufficient.[20]
Some previous cohort studies showed that Vitamin D supplementation likely increases 25(OH)D levels. Supplemented women had less Vitamin D deficiency in three large well-controlled cohorts (n = 1539), a similar trend in one poorer quality study (n = 201), and no difference in one study with an overall low rate of supplementation (n = 559).[21,22,23,24,25] Randomized controlled trials of Vitamin D supplementation have consistently shown success in raising 25(OH)D levels in pregnant women and neonates albeit with varying doses of 25(OH)D.[26] Despite increases with supplementation, 25(OH)D levels remained low in most studies. A recent randomized, double-blinded placebo controlled trial occurred in pregnant South Carolina women. The treatment arms were 2000 IU Vitamin D daily plus standard prenatal vitamins and 4000 IU Vitamin D daily plus standard prenatal vitamins compared with a placebo arm consisting of a placebo pill plus standard prenatal vitamins. The mean Vitamin D level measured at 36 weeks was 79 nmol/L for the control group, 105 for the 2000 IU group, and 119 for the 4000 IU group. This difference was statistically significant (P < 0.0001); however, the levels were higher than most other trials even in the placebo group. In its 2011 report, the Institute of Medicine recommended 600 IU/day of 25(OH)D for pregnant women specifically to support bone metabolism and no more than 4000 IU/day to avoid hypercalcemia.[27] The American Congress of Obstetricians and Gynecologists endorses these recommendations and proposes 1000–2000 IU/day of 25(OH)D when deficiency is identified (<20 ng/mL).[28]
The results cannot be generalized to all patients, because of genetic and environmental factors may play a role in glucose metabolism. Nonetheless, it is important that Vitamin D deficiency in pregnant women should be considered further than before. Because of Vitamin D deficiency can be associated with outcomes such as gestational diabetes.
The results of this study showed no significant difference between the two groups; however, it still cannot say whether Vitamin D supplementation for the prevention of gestational diabetes can be effective or not? And is it a cost-effective prescription?
Limitations of our study were not measuring Vitamin D in the end of the study and sample size selection from two referral Hospitals in one city.
Conclusion
According to the results mentioned Vitamin D deficiency in pregnancy due to several complications for mother and fetus is very important and prevention of it is necessary. However, the use of Vitamin D supplements for pregnant women is not universally agreed. Therefore, recommended that future studies on the cost-effectiveness of the use of these supplements during pregnancy be conducted.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bandeira F, Griz L, Dreyer P, Eufrazino C, Bandeira C, Freese E. Vitamin D deficiency: A global perspective. Arq Bras Endocrinol Metabol. 2006;50:640–6. doi: 10.1590/s0004-27302006000400009. [DOI] [PubMed] [Google Scholar]
- 2.Benachi A, Cordier AG, Courbebaisse M, Souberbielle JC. Vitamin D and pregnancy. Presse Med. 2013;42:1377–82. doi: 10.1016/j.lpm.2013.07.007. [DOI] [PubMed] [Google Scholar]
- 3.Holick MF, Chen TC, Lu Z, Sauter E. Vitamin D and skin physiology: A D-lightful story. J Bone Miner Res. 2007;22(Suppl 2):28–33. doi: 10.1359/jbmr.07s211. [DOI] [PubMed] [Google Scholar]
- 4.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2008;31(Suppl 1):S55–60. doi: 10.2337/dc08-S055. [DOI] [PubMed] [Google Scholar]
- 5.Ryan EA. Diagnosing gestational diabetes. Diabetologia. 2011;54:480–6. doi: 10.1007/s00125-010-2005-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.American Diabetes Association. Gestational diabetes mellitus. Diabetes Care. 2004;27:88–90. [Google Scholar]
- 7.Alvarez JA, Ashraf A. Role of vitamin d in insulin secretion and insulin sensitivity for glucose homeostasis. Int J Endocrinol. 2010;2010:351385. doi: 10.1155/2010/351385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bodnar LM, Catov JM, Simhan HN, Holick MF, Powers RW, Roberts JM. Maternal Vitamin D deficiency increases the risk of preeclampsia. J Clin Endocrinol Metab. 2007;92:3517–22. doi: 10.1210/jc.2007-0718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kazemi A, Sharifi F, Jafari N, Mousavinasab N. High prevalence of Vitamin D deficiency among pregnant women and their newborns in an Iranian population. J Womens Health (Larchmt) 2009;18:835–9. doi: 10.1089/jwh.2008.0954. [DOI] [PubMed] [Google Scholar]
- 10.Sloka S, Stokes J, Randell E, Newhook LA. Seasonal variation of maternal serum Vitamin D in newfoundland and Labrador. J Obstet Gynaecol Can. 2009;31:313–21. doi: 10.1016/S1701-2163(16)34148-2. [DOI] [PubMed] [Google Scholar]
- 11.Committee Opinion No. 504: Screening and diagnosis of gestational diabetes mellitus. Obstet Gynecol. 2011;118:751–3. doi: 10.1097/AOG.0b013e3182310cc3. [DOI] [PubMed] [Google Scholar]
- 12.Burris HH, Camargo CA., Jr Vitamin D and gestational diabetes mellitus. Curr Diab Rep. 2014;14:451. doi: 10.1007/s11892-013-0451-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Committee on Practice Bulletins-Obstetrics. Gestational Diabetes Mellitus. Practice Bulletin No. 137. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2013;122:406–16. [Google Scholar]
- 14.London MB, Catalano PM, Gabbe SG. Diabetes Mellitus Complicating Pregnancy. In: Gabbe SG, Niebyl JR, Galan HL, Jauniaux ERM, Landon M, Simpson JL, et al., editors. Obstetrics: Normal and Problem Pregnancies. 6th ed. Ch. 39. Philadelphia, PA: Saunders Elsevier; 2012. [Google Scholar]
- 15.Timms PM, Mannan N, Hitman GA, Noonan K, Mills PG, Syndercombe-Court D, et al. Circulating MMP9, Vitamin D and variation in the TIMP-1 response with VDR genotype: Mechanisms for inflammatory damage in chronic disorders? QJM. 2002;95:787–96. doi: 10.1093/qjmed/95.12.787. [DOI] [PubMed] [Google Scholar]
- 16.Zhang C, Qiu C, Hu FB, David RM, van Dam RM, Bralley A, et al. Maternal plasma 25-hydroxyvitamin D concentrations and the risk for gestational diabetes mellitus. PLoS One. 2008;3:e3753. doi: 10.1371/journal.pone.0003753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baker AM, Haeri S, Camargo CA, Stuebe AM, Boggess KA. First-trimester maternal vitamin D status and risk for gestational diabetes (GDM) a nested case-control study. Diabetes/Metab Res Rev. 2012;28:164–8. doi: 10.1002/dmrr.1282. doi:10.1002/dmrr.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Makgoba M, Nelson SM, Savvidou M, Messow CM, Nicolaides K, Sattar N. First-trimester circulating 25-hydroxyvitamin D levels and development of gestational diabetes mellitus. Diabetes Care. 2011;34:1091–3. doi: 10.2337/dc10-2264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Senti J, Thiele DK, Anderson CM. Maternal Vitamin D status as a critical determinant in gestational diabetes. J Obstet Gynecol Neonatal Nurs. 2012;41:328–38. doi: 10.1111/j.1552-6909.2012.01366.x. [DOI] [PubMed] [Google Scholar]
- 20.Yu CK, Sykes L, Sethi M, Teoh TG, Robinson S. Vitamin D deficiency and supplementation during pregnancy. Clin Endocrinol (Oxf) 2009;70:685–90. doi: 10.1111/j.1365-2265.2008.03403.x. [DOI] [PubMed] [Google Scholar]
- 21.Ginde AA, Sullivan AF, Mansbach JM, Camargo CA., Jr Vitamin D insufficiency in pregnant and nonpregnant women of childbearing age in the United States. Am J Obstet Gynecol. 2010;202:436.e1–8. doi: 10.1016/j.ajog.2009.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hamilton SA, McNeil R, Hollis BW, Davis DJ, Winkler J, Cook C, et al. Profound Vitamin D Deficiency in a diverse group of women during pregnancy living in a sun-rich environment at latitude 32 degrees N. Int J Endocrinol. 2010;2010:917428. doi: 10.1155/2010/917428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perampalam S, Ganda K, Chow KA, Opie N, Hickman PE, Shadbolt B, et al. Vitamin D status and its predictive factors in pregnancy in 2 Australian populations. Aust N Z J Obstet Gynaecol. 2011;51:353–9. doi: 10.1111/j.1479-828X.2011.01313.x. [DOI] [PubMed] [Google Scholar]
- 24.Li W, Green TJ, Innis SM, Barr SI, Whiting SJ, Shand A, et al. Suboptimal Vitamin D levels in pregnant women despite supplement use. Can J Public Health. 2011;102:308–12. doi: 10.1007/BF03404056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dror DK, King JC, Durand DJ, Allen LH. Association of modifiable and nonmodifiable factors with Vitamin D status in pregnant women and neonates in Oakland, CA. J Am Diet Assoc. 2011;111:111–6. doi: 10.1016/j.jada.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 26.Roth DE. Vitamin D supplementation during pregnancy: Safety considerations in the design and interpretation of clinical trials. J Perinatol. 2011;31:449–59. doi: 10.1038/jp.2010.203. [DOI] [PubMed] [Google Scholar]
- 27.IOM (Institute of Medicine). Dietary Reference Intakes for Calcium and Vitamin D. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 28.ACOG Committee on Obstetric Practice. ACOG Committee Opinion No 495: Vitamin D: Screening and supplementation during pregnancy. Obstet Gynecol. 2011;118:197–8. doi: 10.1097/AOG.0b013e318227f06b. [DOI] [PubMed] [Google Scholar]